Abstract
Objective
Although generalized convulsive status epilepticus (GCSE) is a life-threatening emergency, evidence-based data to guide initial drug treatment choices are lacking in the Chinese population. We conducted this prospective, randomized, controlled trial to evaluate the relative efficacy and safety of intravenous phenobarbital and valproate in patients with GCSE.
Methods
After the failure of first-line diazepam treatment, Chinese adult patients with GCSE were randomized to receive either intravenous phenobarbital (standard doses, low rate) or valproate (standard). Successful treatment was considered when clinical and electroencephalographic seizure activity ceased. Adverse events following treatment, as well as the neurological outcomes at discharge and 3 months later, were also evaluated.
Results
Overall, 73 cases were enrolled in the study. Intravenous phenobarbital was successful in 81.1% of patients, and intravenous valproate was successful in 44.4% of patients (p < 0.05). The relapse rate of status epilepticus within 24 h of receiving phenobarbital (6.7%) was significantly lower than that in patients receiving valproate (31.3%), and the total number of adverse events did not differ significantly between the two groups (p > 0.05). In the phenobarbital group, two patients (5.4%) required ventilation and two patients (5.4%) developed serious hypotension. The neurological outcomes of the phenobarbital group were generally better than those of the valproate group; however, no significant differences were observed between phenobarbital and valproate with respect to mortality (8.1 vs. 16.6%) at discharge, or mortality (16.2 vs. 30.5%) and post-symptomatic epilepsy (26.3 vs. 42.8%) at 3-month follow-up.
Conclusions
Intravenous phenobarbital appears to be more effective than intravenous valproate for Chinese adult patients with GCSE. The occurrence of serious respiratory depression and hypotension caused by phenobarbital was reduced by decreasing the intravenous infusion rate; however, even at a lower infusion rate than typically used in other institutions, intravenous phenobarbital resulted in more serious adverse events than intravenous valproate. The better outcomes in the phenobarbital group compared with the valproate group suggest that phenobarbital should be considered for the early successful treatment of GCSE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In Chinese adult patients, phenobarbital had a higher clinical termination rate and lower relapse rate compared with valproate. |
The incidence rate of serious adverse events caused by phenobarbital declined with decreasing intravenous speed. |
Patients with early successful treatment are prone to have good outcomes. |
1 Introduction
Status epilepticus (SE) is a life-threatening neurological emergency, with incidence rates of 10.3–17.1/100,000 in Europe and 18.1/100,000 in the US, and represents approximately 6% of emergency department cases of seizures in the US [1–4]. The mortality rates for SE have been reported as 7.6–39% in Europe, 10.7% in California, and 15.8% in Southwestern China [1–3, 5, 6], with generalized convulsive SE (GCSE) being the most common and most dangerous type. SE requires emergent, targeted treatment to reduce irreversible cerebral and systemic injury.
Benzodiazepines have been advocated for the initial treatment of SE. Cardiovascular toxicity and serious reactions at the injection site sometimes limit the application of phenytoin, particularly in patients older than 40 years of age [7]. Moreover, phenytoin and lorazepam are currently not available in mainland China; in the past 10 years, only valproate has been added to the market in China. It has been reported that valproate can terminate SE in 50–90% of study cases, with little respiratory depression or hypotension [8–12]. Our prior study also reported the successful rate of valproate as the initial treatment for GCSE (50%) at rates equal to that seen with diazepam (56%), whereas the rates of respiratory or circulatory complications after valproate treatment (0%) were significantly lower than those seen following diazepam treatment (5.5%); however, these seemingly successful rates for both medications did not result in satisfactory long-term outcomes [12].
Phenobarbital is one of the oldest antiepileptic drugs (AEDs) still in clinical practice, as a result of advantages in its affordability and efficacy, but its value in the treatment of SE is still controversial. Phenobarbital has lost favor in Europe and the US because of anecdotal evidence of adverse events such as hypotension, arrhythmias, and respiratory depression [13–15]; however, there are still limited studies available assessing the efficacy and safety of phenobarbital for the treatment of SE. Direct comparisons of intravenous phenobarbital and valproate have been reported in only one study performed in children with convulsive SE (CSE) and acute prolonged convulsive seizures [11]. High doses and/or fast intravenous rates can result in higher blood–drug levels sooner, which may cause serious adverse events. Malamiri et al. [11] prospectively compared the efficacy of phenobarbital in children at a lower dose than in former studies. Intravenous phenobarbital was successful in seizure termination in 77% of patients compared with 90% of patients receiving intravenous valproate. Adverse events with phenobarbital were few, with a 3.3% rate of hypoventilation and a 0% hypotension rate. Clinically significant adverse effect rates differed between the phenobarbital group and the valproate group; however, the main frequent adverse effects of phenobarbital were lethargy and vomiting.
We therefore undertook this prospective, randomized controlled trial to evaluate the relative efficacy and safety of intravenous phenobarbital (standard doses, low rate) and valproate (standard) for the treatment of GCSE as second-line anticonvulsants in adults.
2 Methods
2.1 Patients
The study period ran from February 2011 to August 2015. All adult patients (aged 18 years or older) with GCSE who were admitted to the emergency room or neurocritical care unit of the Xuanwu Hospital, Capital Medical University, initially received first-line treatment with diazepam (intravenous injection of 0.2 mg/kg, administered twice at a 10-min interval) according to hospital protocol. Patients who did not respond to first-line treatment, and were eligible based on the study inclusion and exclusion criteria, were prospectively and consecutively enrolled into the trial. We applied an operational definition of SE as 5 min or more of continuous clinical and/or electrographic seizure activity or recurrent seizure activity without recovery between seizures, according to guidelines for the evaluation and management of SE [16]. Exclusion criteria included (1) unstable vital signs, such as systolic blood pressure <90 mmHg, pulse <60 beats/min, or arterial blood oxygen saturation <90%; (2) liver dysfunction (alanine transaminase or total bilirubin more than twice the upper limit of normal); (3) neurologic emergency requiring immediate surgical intervention; (4) pregnant or breastfeeding; (5) hypersensitivity to study drugs.
This study was approved by the Ethics Committee of Xuanwu Hospital, Capital Medical University. It adhered to the tenets of the Declaration of Helsinki and was registered in the Cochrane Central Register of Controlled Trials (ChiCTR-TRC-13003339). Written informed consent was obtained from the legal representatives of the patients.
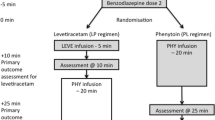
2.2 Drug Treatment
In this study, eligible patients were assigned to treatment according to a table of random digits, which was kept by one particular physician. Other members of the team did not know in advance which group the patients would be assigned to, and the randomization process was strictly supervised. Those who had not responded to first-line anticonvulsants were enrolled in this trial and were randomized to receive either intravenous phenobarbital or valproate. In the phenobarbital group, a loading dose of 20 mg/kg (an additional 5–10 mg/kg may be administered) began at a rate of 50 mg/min, followed by an intravenous dose of 100 mg every 6 h. Once the patient began to show hypopnea or hypotension, phenobarbital was stopped or stepped-down for the time being. In the valproate group, a loading dose of 30 mg/kg (an additional 15 mg/kg may be administered) began at a rate of 3 mg/kg/min, followed by a continuous infusion at a rate of 1–2 mg/kg/h. The infusions were maintained for 24–48 h and then gradually tapered until they were eventually replaced with oral AEDs (24–72 h). The blood–drug level was also tested.
2.3 Electroencephalography Recording
Bedside video electroencephalography (EEG; DAVINCI-SAM, Micromed, Mogliano Veneto, Italy) was performed shortly after initial treatment. Electrodes were placed according to the international 10–20 system, and the EEG monitoring lasted for a minimum of 24 h.
2.4 Evaluation of Efficacy and Safety
The primary study endpoint was the number of patients with effective seizure control, defined as a cessation of clinical and electroencephalographic seizure activity within 10–20 min of administration of the phenobarbital or valproate loading dose. Effective control of GCSE was assessed clinically by a certified neurologist, and was also confirmed by a certified electroencephalographer using EEG. We also recorded the relapse rates of SE and nonconvulsive SE (NCSE)/nonconvulsive seizures (NCS) in each group in the first 24 h.
Adverse events were recorded as follows: systolic blood pressure lower than 90 mmHg, pulse lower than 50 beats/min, arrhythmia (except supraventricular tachycardia), respiratory depression (arterial oxygen saturation below 90%, partial pressure of oxygen below 60 mmHg, or partial pressure of carbon dioxide above 60 mmHg), drug-induced liver disease (alanine aminotransferase or total bilirubin increase of more than twice the upper limit of the normal range), elevation of blood ammonia (more than twice the upper limit of the normal range), gastric motility insufficiency, bone marrow suppression (leukocytopenia, neutrocytopenia, thrombocytopenia or anemia), coagulation disorders, or drug-related sedation. Adverse events were separated as severe and nonsevere, with hypoventilation (FO2 <90%), severe hypotension, and bone marrow depletion defined as a severe adverse event. The time to record adverse events was the time from administration of phenobarbital or valproate to 1 week. We continuously monitored vital signs and recorded hematologic examination on days 1, 3, 5, and 7.
A physician who was unaware of the therapeutic assignment assessed neurologic outcome, both at discharge and at 3 months, through a phone interview or scheduled follow-up clinic visit, and the mortality of each group was recorded at discharge and at 3 months. Moreover, post-SE symptomatic epilepsy at 3 months was analyzed, and was defined as the occurrence of at least one unprovoked epileptic seizure occurring not earlier than 4 weeks after termination of SE in those without pre-existing epilepsy [17].
2.5 Statistical Analysis
All data were analyzed using SPSS version 22.0 (IBM Corporation, Armonk, NY, USA). Categorical variables between the two groups were compared using Chi-squared tests. A Pearson’s Chi-square test was used when no subgroup had an expected count below 5, otherwise a Fisher’s exact test was performed. A two-tailed t test for normally distributed continuous variables was performed, and the Mann–Whitney U test was used in cases where the variable was not normally distributed. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. A p value <0.05 was considered statistically significant.
The sample size was calculated keeping type I error (α) at 0.05 and type II error (β) at 0.1, using a Z-test for proportion (based on a one-sided test). The sample size was calculated to be 70, with the power of the test as 90%. Therefore, a study population of 73 patients was considered sufficient.
3 Results
A total of 134 patients met the GCSE criteria, among whom 56 patients (41.79%) were successfully controlled with diazepam. Five patients were excluded from the study for the following reasons: two were pregnant, one was breastfeeding, and two had a past history of hypersensitivity to valproate. Overall, 73 patients with GCSE and a mean age of 41.72 ± 17.14 years (range 18–80) were successfully enrolled in the study. The leading etiology of GCSE was viral encephalitis (n = 30), followed by pre-existing epilepsy (n = 23), other undetermined causes (n = 14), and cerebrovascular disease (n = 6). No significant differences between the two groups were observed in terms of age, sex, etiology, or duration of GCSE before treatment. The baseline characteristics of both groups are shown in Table 1. Patients may have received nonstandard treatment prior to enrollment in the study, the definition of which was that the method of administration and/or dosage of drugs were not standard, including intramuscular diazepam (5–10 mg; phenobarbital 12 patients vs. valproate 10 patients), intramuscular phenobarbital (0.1–0.2 g; phenobarbital 13 patients vs. valproate 13 patients), and oral AEDs (phenobarbital 4 patients vs. valproate 3 patients). No significant difference in terms of the nonstandard treatments received was observed between the intravenous phenobarbital and intraveous valproate groups, and the time from SE onset to the first (non-standard) treatment outside of the study was 5 or 30 min.
Intravenous phenobarbital was successful in 81.1% (30/37) of patients with GCSE, and intravenous valproate was successful in 44.4% (16/36) of patients with GCSE (Chi-square 10.508, OR 5.357, 95% CI 1.869–15.356; p = 0.001). A significant difference was also noted in the relapse rate of SE within 24 h (6.7%, 2/30 vs. 31.3%, 5/16) [Chi-square 4.888, OR 0.157,95% CI 0.026–0.934; p = 0.040]; however, the relapse rates of NCSE within 24 h were not statistically significant (p > 0.05), i.e. 20.0% (6/30) vs. 31.3% (5/16) for the phenobarbital and valproate groups (Chi-square 0.726, OR 0.550, 95% CI 0.138–2.197; p = 0.477) (Fig. 1).
Comparison of the effects of valproate and phenobarbital. Seizure was controlled in 81.1 and 44.4% of patients in the phenobarbital and valproate groups, respectively (p < 0.05), and relapse of SE within 24 h occurred in 6.7 and 31.3% of patients in the phenobarbital and valproate groups, respectively (p < 0.05). Relapse of NCSE within 24 h did not reach statistical significance (20.0 vs. 31.3%). SE status epilepticus, NCSE nonconvulsive status epilepticus
More severe adverse events were seen in the phenobarbital group (13.5 vs. 0%; p = 0.04), in which six patients had transient depressed respiration and two (5.4%) needed ventilation; five patients developed hypotension and two (5.4%) required vasopressor support. Moreover, two patients developed gastric motility insufficiency, two showed a transient transaminase increase, and one developed bone marrow suppression. After phenobarbital withdrawal, the patients returned to normal levels within 1 month. In contrast, in the valproate group, no patients showed hypotension or hypoventilation, and six showed transient hyperammonemia without hepatic injury or hyperammonemia encephalopathy. Hyperammonemia disappeared after 1–3 days’ administration of l-carnitine. Four patients showed a transient transaminase increase, which returned to normal levels after administration of glucuronolactone for 1 month (Fig. 2).
Comparison of the side effects of valproate and phenobarbital treatments. In the phenobarbital group, two patients (5.4%) had severe hypoventilation, two (5.4%) had severe hypotension, and one (2.7%) had bone marrow suppression. The total severe adverse event rate was 13.5%. Additionally, two patients developed gastric motility insufficiency and two patients showed a transient transaminase increase. No patients receiving valproate had severe adverse events; however, in the valproate group, six patients showed transient hyperammonemia and four showed a transient transaminase increase
The mean blood–drug level of phenobarbital and valproate 6–8 h after the end of the loading dose was 37.43 μg/ml (range 28.94–63.25) and 80.62 μg/ml (range 48.19–115.0), respectively. Twenty-three patients (14 in the phenobarbital group and 9 in the valproate group) with a past history of epilepsy had comedication (such as carbapenem, phenobarbital and valproate), which may influence the blood–drug level of phenobarbital or valproate.
The phenobarbital group showed better outcomes at discharge and at 3 months than the valproate group, but these differences did not reach significance. The mortality (phenobarbital vs. valproate) rates were 8.1% (3/37) vs. 16.6% (6/36) at discharge, and 16.2% (6/37) vs. 30.5% (11/36) at 3 months. Trends for the risk of developing post-SE symptomatic epilepsy were 26.3% (5/19) and 42.8% (6/14) for the phenobarbital and valproate groups, respectively.
4 Discussion
In this trial, phenobarbital was successful in 81.1% of cases, and at nearly twice the rate of the valproate group (44.4%). In former studies, the termination rate with phenobarbital was seen to reach a high level, which can be equal to lorazepam and levetiracetam [13, 14, 18–22]. Thus, for our method, we chose a low intravenous rate (50 mg/min), which did not decrease the termination rate of phenobarbital.
The mechanisms of phenobarbital-induced termination of SE may be related to the following factors. Phenobarbital could activate γ-aminobutyric acid (GABA) receptors and could thus increase the opening frequency of chloride channels. In general, benzodiazepines are thought to increase the open time of chloride channels. Additionally, phenobarbital could increase the open times of chloride channels by directly acting on them. Moreover, phenobarbital could decrease the release of glutamic acid [23–27]. Moreover, valproate mainly acts on ion channels and GABA receptors [26, 27].
In our study, six patients had transient hypopnea and only two needed ventilation; five patients developed hypotension and two required vasopressor support in the phenobarbital group. Of these, only two patients were under 60 years of age, while the remaining patients were older than 60 years of age. Side effects were less severe with valproate, and no patients in that group developed hypopnea or hypotension. These low rates of hypoventilation and hypotension were the same as in previous studies [10–12], and these results indicate that intravenous valproate is a safe method for older patients.
Our results showed lower rates of severe hypotension and hypoventilation with phenobarbital than in previous studies [13, 14]. The low incidence of severely depressed respiration and hypotension may be related to the dose and intravenous rate of phenobarbital used in our study. The mechanisms of respiratory and circulatory depression caused by intravenous phenobarbital may be due to its action on the respiratory and circulatory centers. High doses and/or fast intravenous rates could result in higher blood–drug levels sooner, resulting in depressed respiratory and circulatory centers. Shaner et al. [14] prospectively compared the efficacy of phenobarbital with phenytoin and diazepam; phenobarbital was administered at a dose of 100 mg/min until 10 mg/kg had been reached. Two of the 18 patients (11%) receiving phenobarbital had hypotension, and one (5.5%) had arrhythmia. Treiman et al. [13] increased the loading dose (15 mg/kg) to 100 mg/min, and the rates of hypotension and hypoventilation increased. The rate of hypotension was 34% (31/91), while the rate of respiration depression was 13% (12/91). A study of phenobarbital in the pediatric population chose a lower rate (<60–100 mg/min) and a higher loading dose (20 mg). The rate of hypoventilation was 3% (1/30). Moreover, no patients had hypotension due to intravenous phenobarbital [11]. Considering these former studies, we used intravenous phenobarbital at a loading dose of 20 mg/kg, with a rate of 50 mg/min. Our high termination rate may be ascribed to the loading dose (20 mg/kg). Only two patients had severe hypoventilation or hypotension, respectively, which may due to the lower bolus rate. Meanwhile, we paid close attention to the vital signs when administering intravenous phenobarbital. Once the patient began to show hypopnea or hypotension, we stopped or stepped-down phenobarbital for the time being. Mild hypoventilation and hypotension could be rectified through this method, and severe hypoventilation and hypotension could be cured by ventilation and vasopressor support.
Our results indicate that phenobarbital might improve the rates of successful SE treatment. The neurological outcomes of the phenobarbital group were better than those of the valproate group, although these differences did not reach significance. In a previous study, a good treatment protocol was confirmed to be associated with better seizure control and even shorter intensive care unit (ICU) stay and hospital length of stay [28]. Moreover, Scholtes et al. [29] found the mortality rate may be as low as 8% in patients receiving adequate therapy, and as high as 45% in those receiving insufficient therapy. Therefore, it is essential to terminate SE in the early minutes to reduce irreversible cerebral and systemic injury.
In addition, in developing countries, where many newer AEDs are not yet approved, expenditure on AEDs is a potentially limiting factor that could limit the use of some of the newer AEDs available. Thus, its relatively low expense is another advantage of phenobarbital, in addition to its high termination rate and low relapse rate. If the administered drug was not effective and/or a severe adverse event was reported, patients would require admission to an ICU. Patients in the phenobarbital group had a lower relapse rate of SE than in the valproate group, which could further decrease the expense.
The limitations of this study are as follows. We did not investigate whether a short-term and high-dose phenobarbital regimen could lead to cognitive dysfunction. Additionally, these results cannot be taken as strong evidence for best practices for the treatment of GCSE in adults because the patients were from a single center and the sample size was relatively small. The difference in mean age (37.14 vs. 45.26 years) may result from the relatively small sample size, while, in the phenobarbital group, lower age may be one factor that explains the better outcome in this group.
5 Conclusions
We report a modified method of intravenous phenobarbital (which is more effective than intravenous valproate for Chinese adult patients with GCSE) for initial drug treatment of GCSE. The occurrence of serious respiratory depression and hypotension caused by phenobarbital was reduced by decreasing the intravenous infusion rate; however, even at a lower infusion rate than typically used in other institutions, intravenous phenobarbital resulted in more serious adverse events than intravenous valproate. The better outcomes in the phenobarbital group compared with the valproate group suggest that phenobarbital should be considered for the early successful treatment of GCSE. Further studies are warranted to confirm our results.
References
Coeytaux A, Jallon P, Galobardes B, et al. Incidence of status epilepticus in French-speaking Switzerland: (EPISTAR). Neurology. 2000;55:693–7.
Knake S, Rosenow F, Vescovi M, et al. Incidence of status epilepticus in adults in Germany: a prospective, population-based study. Epilepsia. 2001;42:714–8.
Hirsch LJ. Intramuscular versus intravenous benzodiazepines for prehospital treatment of status epilepticus. N Engl J Med. 2012;366:659–60.
Logroscino G, Hesdorffer DC, Cascino G, et al. Time trends in incidence, mortality, and case-fatality after first episode of status epilepticus. Epilepsia. 2001;42:1031–5.
Wu YW, Shek DW, Garcia PA, et al. Incidence and mortality of generalized convulsive status epilepticus in California. Neurology. 2002;58:1070–6.
Li JM, Chen L, Zhou B, et al. Convulsive status epilepticus in adults and adolescents of southwest China: mortality, etiology, and predictors of death. Epilepsy Behav. 2009;14:146–9.
Cranford RE, Leppik IE, Patrick B, et al. Intravenous phenytoin in acute treatment of seizures. Neurology. 1979;29:474–9.
Gilad R, Izkovitz N, Dabby R, et al. Treatment of status epilepticus and acute repetitive seizures with i.v. valproic acid vs. phenytoin. Acta Neurol Scand. 2008;118:296–300.
Mehta V, Singhi P, Singhi S. Intravenous sodium valproate versus diazepam infusion for the control of refractory status epilepticus in children: a randomized controlled trial. J Child Neurol. 2007;22:1191–7.
Agarwal P, Kumar N, Chandra R, et al. Randomized study of intravenous valproate and phenytoin in status epilepticus. Seizure. 2007;16:527–32.
Malamiri RA, Ghaempanah M, Khosroshahi N, et al. Efficacy and safety of intravenous sodium valproate versus phenobarbital in controlling convulsive status epilepticus and acute prolonged convulsive seizures in children: a randomised trial. Eur J Paediatr Neurol. 2012;16:536–41.
Chen WB, Gao R, Su YY, et al. Valproate versus diazepam for generalized convulsive status epilepticus: a pilot study. Eur J Neurol. 2011;18:1391–6.
Treiman DM, Meyers PD, Walton NY, et al. A comparison of four treatments for generalized convulsive status epilepticus. Veterans Affairs Status Epilepticus Cooperative Study Group. N Engl J Med. 1998;339:792–8.
Shaner DM, McCurdy SA, Herring MO, et al. Treatment of status epilepticus: a prospective comparison of diazepam and phenytoin versus phenobarbital and optional phenytoin. Neurology. 1988;38:202–7.
Trinka E. What is the relative value of the standard anticonvulsants: phenytoin and fosphenytoin, phenobarbital, valproate, and levetiracetam? Epilepsia. 2009;50:40–3.
Brophy GM, Bell R, Claassen J, et al. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care. 2012;17:3–23.
Holtkamp M, Othman J, Buchheim K, et al. Predictors and prognosis of refractory status epilepticus treated in a neurological intensive care unit. J Neurol Neurosurg Psychiatry. 2005;76:534–9.
Misra UK, Kalita J, Maurya PK. Levetiracetam versus lorazepam in status epilepticus: a randomized, open labeled pilot study. J Neurol. 2012;259:645–8.
Silbergleit R, Lowenstein D, Durkalski V, et al. RAMPART (Rapid Anticonvulsant Medication Prior to Arrival Trial): a double-blind randomized clinical trial of the efficacy of intramuscular midazolam versus intravenous lorazepam in the prehospital treatment of status epilepticus by paramedics. Epilepsia. 2011;52:45–7.
Swisher CB, Doreswamy M, Gingrich KJ, et al. Phenytoin, levetiracetam, and pregabalin in the acute management of refractory status epilepticus in patients with brain tumors. Neurocrit Care. 2012;16:109–13.
Berning S, Boesebeck F, van Baalen A, et al. Intravenous levetiracetam as treatment for status epilepticus. J Neurol. 2009;256:1634–42.
Eue S, Grumbt M, Muller M, et al. Two years of experience in the treatment of status epilepticus with intravenous levetiracetam. Epilepsy Behav. 2009;15:467–9.
Loddenkemper T, Talos DM, Cleary RT, et al. Subunit composition of glutamate and gamma-aminobutyric acid receptors in status epilepticus. Epilepsy Res. 2014;108:605–15.
Raol YH, Zhang G, Budreck EC, et al. Long-term effects of diazepam and phenobarbital treatment during development on GABA receptors, transporters and glutamic acid decarboxylase. Neuroscience. 2005;132:399–407.
Skerritt JH, Johnston GA. Enhancement of GABA binding by benzodiazepines and related anxiolytics. Eur J Pharmacol. 1983;89:193–8.
Macdonald RL, Kelly KM. Antiepileptic drug mechanisms of action. Epilepsia. 1993;34:S1–8.
Anyanwu E, Harding GF. The involvement of taurine in the action mechanism of sodium valproate (VPA) in the treatment of epilepsy. Acta Physiol Pharmacol Ther Latinoam. 1993;43:20–7.
Aranda A, Foucart G, Ducasse JL, et al. Generalized convulsive status epilepticus management in adults: a cohort study with evaluation of professional practice. Epilepsia. 2010;51:2159–67.
Scholtes FB, Renier WO, Meinardi H. Generalized convulsive status epilepticus: causes, therapy, and outcome in 346 patients. Epilepsia. 1994;35:1104–12.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported by the National Key Department of Neurology funded by the Chinese Health and Family Planning Committee, and the National Key Department of Critical Care Medicine funded by the Chinese Health and Family Planning Committee.
Conflict of interest
Su Yingying, Liu Gang, TianFei, Ren Guoping, Jiang Mengdi, Brian Chun, Zhang Yunzhou, Zhang Yan, Ye Hong, GaoDaiquan, and Chen Weibi declare they have no conflicts of interest.
Ethical approval
This study was approved by the Ethics Committee of Xuanwu Hospital, Capital Medical University. Written informed consent was obtained from the legal representatives of the patients.
Rights and permissions
About this article
Cite this article
Su, Y., Liu, G., Tian, F. et al. Phenobarbital Versus Valproate for Generalized Convulsive Status Epilepticus in Adults: A Prospective Randomized Controlled Trial in China. CNS Drugs 30, 1201–1207 (2016). https://doi.org/10.1007/s40263-016-0388-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-016-0388-6