Abstract
Insufficient outcomes amongst adults with major depressive disorder (MDD) provide the impetus to identify and refine therapeutic targets that are most critical to outcome from patient, provider, and societal perspectives. Towards this aim, a pivotal shift towards the transnosological domain, cognition, is occurring in the study of MDD and other brain disorders. This paper aims to provide a framework for conceptualizing and prioritizing cognitive function amongst adults with MDD with a particular view to provide a conceptual framework for research and clinical priorities. We also summarize extant data pertaining to psychotropic effects, notably antidepressants, on the cognitive dimension/domain. This narrative review was based on articles identified through a PubMed/MEDLINE search of all English-language articles published between January 1966 and October 2014. The search words were major depressive disorder, depression, unipolar depression, cognition, cognitive dysfunction, cognitive deficit, and cognitive function. The search was supplemented with a manual review of relevant references. The selection of articles for inclusion in this review was based on overall methodological quality as well as on their pertinence to informing the framework described herein. Cognitive dysfunction in MDD is a discrete domain subserved by discrete yet overlapping substrates. There is a need to provide a glossary of terms commonly employed in the cognition literature for consensus as to the appropriate screening, measurement, and monitoring tools. The guiding principle of measurement-based care should include systematic assessment and measurement of cognition in subpopulations with MDD, as a tactic to improve outcome. Relatively few treatment strategies have demonstrated efficacy specifically for the cognitive domain in MDD. The antidepressant vortioxetine has replicated evidence of specific pro-cognitive effects in adults with MDD across multiple subdomains of cognitive function. Vortioxetine is a novel antidepressant that is hypothesized to act through a combination of direct effects on receptor activity and serotonin receptor inhibition, as well as other systems. Pro-cognitive effects for other US FDA-approved agents are suggested, but pseudospecificity has not been excluded as a possible explanation of their beneficial effects on cognitive function. A disparate assortment of other agents are currently under investigation for possible benefit in mitigating cognitive deficits and improving cognitive performance (e.g., intranasal insulin, erythropoietin, anti-inflammatory agents). Non-pharmacological approaches including, but not limited to, cognitive remediation (CR), aerobic exercise, and neuromodulation are promising.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Cognitive dysfunction is a core domain disturbance in adults with major depressive disorder (MDD) that is correlated with, yet independent of, mood domain symptoms. |
Disparate antidepressant modalities (e.g. pharmacotherapy, neuromodulation) would be expected to improve measures of cognitive function; notwithstanding, pseudospecificity can only be ruled out if studies employ methods to adjust for the contribution of mood symptoms (e.g. path analysis, subgroup analysis). |
Vortioxetine is the only approved/proven treatment for MDD with replicated evidence demonstrating direct and independent effects on cognitive function in adults with MDD across multiple subdomains of cognitive function. |
1 Introduction
Major depressive disorder (MDD) is a common, often severe disorder associated with high rates of non-recovery, recurrence, and comorbidity [1–3]. Convergent evidence indicates that MDD is the leading cause of disability amongst patients in both developed and emerging economies [4]. The principal source of cost and illness-associated morbidity is due to a significant decrease in role-function amongst affected individuals [5, 6]. Notwithstanding the widespread and increasing use of antidepressants within the general population, outcomes amongst individuals with MDD remain disappointing [7]. In the clinical ecosystem, adults with MDD receiving guideline-informed, measurement-based, integrated care exhibit significant rates of non-remission and functional impairment [8]. The foregoing portrait of MDD invites the need to identify and refine the dimensions/domains that are most critical to illness outcome from patient, provider, and societal perspectives [9].
MDD, like all mental disorders, is a phenotype comprising disturbances across discrete and finite psychopathological domains [10]. Cognitive dysfunction is identified as a transnosological domain critical to outcomes across disparate mental disorders including, but not limited to, schizophrenia, bipolar disorder, and autism [11]. Hitherto, disturbances in cognitive function have received less attention in MDD relative to other psychiatric populations [12]. Available data in MDD indicate that disturbance in cognitive function is a principal determinant of health outcomes in subsets of patients [12]. This paper is not intended to be a comprehensive and systematic review of cognitive dysfunction in MDD, as this has been reviewed by our group previously [12]. Instead, the primary aim herein is to provide a narrative review of literature pertaining to the domain of cognitive function in MDD.
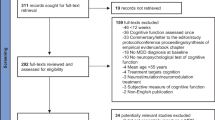
This narrative review was based on articles identified through a PubMed/MEDLINE search of all English-language articles published between January 1966 and October 2014. The search words were MDD, depression, unipolar depression, cognition, cognitive dysfunction, cognitive deficit, and cognitive function. The search was augmented with a manual review of the reference lists of included articles. The articles selected and included for review were based on overall methodological quality as well as on their pertinence to informing the framework described herein.
2 Cognitive Function Defined
A consensually agreed upon vocabulary for cognitive function does not exist. Descriptions of cognitive domains and subdomains have varied and have often employed an interchangeable language. A proposed taxonomy of hot and cold cognition has clinical resonance as well as heuristic value [13]. Hot cognition is defined as cognitive functions that are emotionally valenced. Examples of hot cognition would include, but are not limited to, catastrophic reactions to real and/or perceived slights, anhedonia, negativistic rumination, negative recall bias, and disproportionate attention to negative stimuli. Examples of cold cognition would include, executive function, information processing speed, learning and memory, as well as attention/concentration (Table 1). Neurobiologically, a discrete separation from hot and cold cognition does not exist.
Social cognition involves aspects of theory of mind, metacognition and mentalization [14]; social cognition interdigitates some aspects of both hot and cold cognition. Deficits in social cognition are particularly pronounced in individuals with pervasive developmental and psychotic disorders and are also identified in individuals with mood disorders [15, 16]. A robust body of literature has documented a negative cognitive emotional bias amongst adults with MDD towards negatively valenced facial pictures, providing an example of how hot cognitive dysfunction and social cognitive deficits may interact [17, 18].
2.1 Domains of Cognitive Function Affected in Major Depressive Disorder (MDD)
Disturbances in cognition (i.e., diminished ability to think, concentrate, or make decisions) as well as psychomotor slowing are criterion items for a major depressive episode (MDE) according to the Diagnostic and Statistical Manual of Mental Disorders fifth edition (DSM-5) [19]. All principal domains of cognitive function are adversely affected in adults with MDD (see Table 2). The majority of individuals actively symptomatic during a MDE exhibit or complain of cognitive dysfunction [12]. This empirically supported observation is non-surprising in light of the listing of cognitive dysfunction as a criterion item. It has also been reported that a substantial percentage of individuals exhibit measurable cognitive dysfunction despite being in ‘remission’ [20, 21]. Upon resolution of an MDE, measures of information processing speed as well as learning and memory may significantly improve but continue to exhibit abnormalities [22, 23].
The extent to which cognitive dysfunction, as part of a MDE, is clinically relevant has been instantiated by several lines of research. Qualitative research indicates that patient-reported measures of quality of life (e.g. vitality, vigor, and positive mental health), phenomenon that are not synonymous with, but are related to, cognition, are prioritized as treatment objectives by patients over total symptomatic remission [24, 25]. MDD does not decrease overall measures of intelligence, but does decrease cognitive performance across discrete measures, with effect sizes ranging from 0.2 to 0.8 [26]. The clinical relevance of the deficit in cognitive function is underscored by reports that approximately 25–50 % of patients with MDD exhibit a deficit in one or more cognitive faculties of one standard deviation or more below normative values [27]. The foregoing deficit is thought to be clinically relevant and seems to be in the same order of magnitude of deficits observed in other well-known disorders with cognitive dysfunction (e.g., mild cognitive impairment, attention-deficit hyperactivity disorder) [11].
2.2 Measuring Cognitive Function
For a comprehensive review of cognitive measures, see McIntyre et al. [12]. It is empirically established that measurement of depressive symptoms as part of chronic disease management improves outcome in MDD [8]. It is not known whether the screening, measurement, and systematic evaluation of cognitive function improves outcome in MDD. Well-known screening tools for dementing disorders [e.g., Mini-Mental Status Exam (MMSE), Montreal Cognitive Assessment (MoCA)], are not sufficiently sensitive to detect cognitive dysfunction amongst younger populations with MDD [12]. A comprehensive neurocognitive battery in patients with MDD is not suitable for the busy clinical ecosystem. Moreover, subjective baseline measures of cognitive dysfunction in MDD do not correlate with objective measures of cognitive function [12]. Notwithstanding the lack of baseline correlation, results in multiple sclerosis populations indicate that changes in objective cognitive measures highly correlate with changes in subjective measures of cognitive function [28, 29]. This latter observation suggests that subjective and objective measures may be evaluating overlapping yet discrete phenomena. Active depressive symptoms appear to be more likely to affect subjective when compared to objective measures [28]. A brief cognitive measure suitable for patients with MDD with broad conceptual coverage, sensitivity to change, appropriateness as a repeated measure, and immunity from practice effects and cultural influences does not currently exist. Several academic, professional, and independent proprietary organizations are developing such tools with an aim for widespread adoption in clinical practice, analogous to brief depression measures [e.g., Patient Health Questionnaire 9 (PHQ-9)].
2.3 Cognitive Dysfunction in MDD: A Discrete Domain or Epiphenomenon?
The probability of identifying objective and/or subjective disturbances in discrete domains of cognitive function is more likely to occur in symptomatically depressed adults with MDD [12, 26]. This foregoing highly replicated observation suggests that cognitive dysfunction may, in many cases, be an epiphenomenon in MDD and not a discrete psychopathological domain. Moreover, individuals with greater depression severity (e.g., with psychotic features) are more likely to exhibit disturbances in cognitive function than individuals with milder severity of illness [12]. However, even amongst ‘remitted’ individuals, adults with MDD continue to exhibit cognitive impairment at an effect size that is considered significant, i.e. 0.4–0.6. For individuals with highly severe/psychotic depression, the effect size estimate of cognitive dysfunction may be greater. The observation that cognitive deficits may also be seen in individuals who have fully ‘remitted’ indicates that cognitive dysfunction in depression is correlated with, but is dissociable from, mood items.
Several studies have indicated that hot and cold cognitive dysfunction may predate incident depression in select individuals [30]. Moreover, it has been observed that cognitive dysfunction not only persists despite amelioration of depressive symptoms but also may progress in subsets of individuals with MDD [12]. Family studies also indicate that amongst twins discordant for MDD, a greater likelihood of observing cognitive/information processing deficits in the unaffected individual is expected [31–33].
2.4 Relationship Between Cognitive Dysfunction and Health Outcomes in MDD
In contradistinction to research in schizophrenia, bipolar disorder, autism, and other lifelong disorders, the association between cognitive dysfunction in MDD and psychosocial outcomes has not been as extensively studied [34, 35]. Moreover, available studies have significant methodological limitations. Notwithstanding, consistent with other mental disorders, a preliminary conclusion would be that cognitive dysfunction is a principal determinant of psychosocial outcome in MDD. For example, it has been shown that baseline measures of cognitive function amongst inpatients with MDD predict functional outcomes 6 months post discharge [20, 36]. Moreover, amongst individuals with the greatest psychosocial outcome after an index major depressive episode, cognitive measures improve most. Conversely, individuals with minimal cognitive improvement have the lowest probability of psychosocial readjustment [20].
The global shift in economy towards a ‘human-capital’ economy reflects the polarization of the global workforce away from manual and simple skillsets towards the cognitive and complex. Advances in information and communication technology are paradoxically decreasing the likelihood of employment opportunity for many, with the exception of those with highly skilled cognitive abilities (i.e., association between technology, productivity and employment is referred to as the ‘Solow-Swan’ effect) [37]. These realities of the workplace underscore the importance of optimal cognitive function for workplace integration amongst individuals with MDD.
Surveys conducted amongst working populations indicate that disturbances in measures of cognition are often observed amongst working individuals with MDD. Moreover, patients with MDD who are unemployed are more likely to exhibit decreases in cognitive performance [37]. McIntyre et al. [12] reported that, amongst patients (i.e., aged 18–65 years) experiencing MDE as part of a DSM-IV-defined MDD, disturbances in measures of cognition accounted for a greater degree of variability in workplace performance than did total depression symptom severity [12] (see Fig. 1). The foregoing study is reported in greater detail later on in this article.
Cognitive measures account for more variability in workplace functioning than total depression severity [12]. HAM-D17 Hamilton Depression Rating Scale 17-Item
2.5 Neurobiological Substrates Subserving Cognitive Function
Brain substrates subserving cognitive function have been reviewed elsewhere [11, 38]. Briefly, it is posited that molecular alterations and related changes in neuronal/glial morphometry and integrity result in disturbances within and between brain circuits relevant to discrete cognitive domains [39]. For example, alterations to the default mode network, cognitive control network, emotional network, and salience network have all been implicated as relevant to disturbances in cognition (both hot and cold) [40, 41]. The National Institute of Mental Health (NIMH) Research Domain Criteria (RDoC) broadly aims to better understand brain substrates subserving normal and abnormal human brain phenomenon. A major emphasis of the RDoC initiative is to characterize brain substrates subserving the disparate domains and subdomains of cognitive function (e.g., positive valence, negative valence, social cognition) [10]. The introduction of the RDoC criteria is critical insofar as the taxonomy introduced by the National Institutes of Health (NIH) instantiates cognitive disturbance as a paradigmatic abnormality that is transnosological in nature and a primary focus of current and future research.
3 Treating Cognitive Dysfunction
3.1 Pharmacotherapy
3.1.1 Antidepressants
In a small study evaluating the effects of escitalopram compared with duloxetine in adults with DSM-IV-defined MDD (i.e., escitalopram: n = 36; duloxetine: n = 37) over 24 weeks, the authors determined that both treatments improved working memory as well as attention and disparate measures of executive function [42]. All subjects were assessed with conventional depression measures as well as with tests from the Cambridge Neuropsychological Test Automated Battery (CANTAB). The specific cognitive measures were premorbid intellectual function [i.e., Memory: Wechsler Adult Intelligence Scale (WAIS) III vocabulary subtest, WAIS III Digit Span, Spatial Working Memory; Attention: Rapid Visual Information Processing, Match to Visual Search; Executive Function: Stroop Test, Intra-Extra-Dimensional Set Shift, Stockings of Cambridge] [43, 44]. The authors noted that the performance at endpoint was still inferior to control group. The absence of a placebo in this underpowered study, as well as the lack of demonstration of direct effects specified a priori, leaves the results of this paper as impetus for more rigorous and refined study, and disallows conclusions about the direct effects of selective serotonin reuptake inhibitors (SSRIs) or selective norepinephrine reuptake inhibitors (SNRIs) on cognitive function [43, 44]. Refer to Table 3 for a summary of the effects of various antidepressants and psychotropic agents on measures of cognition in adults with MDD.
The effect of open-label mirtazapine on cognitive function was evaluated in adults (n = 71) with DSM-IV-defined moderate-to-severe MDE across 6 months of therapy. Cognition was assessed with the Wisconsin Card Sorting Test (WCST), the n-back test, Trails Making Tests (TMT) (Parts A and B), and the Stroop Colour Word Interference Test. Subjects received mirtazapine 30–60 mg daily over a period of 6 months (mean 39.5 ± 1.0). Mirtazapine treatment improved measures of cognition in the patient group to the extent that it was comparable to rates described in a healthy control reference group (n = 30). A total of 83 % of subjects were within the normal range for TMT (Part B), and 75 % were in the normal range for WCST. Mirtazapine treatment also significantly improved depressive symptoms; however, the absence of placebo and/or an a priori subgroup analysis, as well as the absence of other method approaches to determine direct effect, disallows any firm conclusions about mirtazapine’s putative, direct, and beneficial effects [45]. Moreover, any assertions of mirtazapine’s beneficial effects on cognition would need to be considered in light of the replicated evidence of clinically significant rates of sedation, somnolence, and possible interference with psychomotor performance associated with this agent [46].
Reboxetine was compared with paroxetine on measures of cognitive function in adults aged 18–65 years with MDD over a period of 8 weeks (n = 74; reboxetine: n = 25, paroxetine: n = 23; and placebo: n = 26). This analysis represents results from two identical, multi-center trials wherein the primary aim was to evaluate depression outcomes in MDD. Cognition was assessed with the Cognitive Drug Research (CDR) computerized assessment system. The CDR comprises simple reaction time, digit vigilance task, choice reaction time, numeric working memory, word recognition, and the critical flicker fusion. No significant differences were observed at endpoint for reboxetine or paroxetine treatment on the combined speed factor. However, the interpretation of this paper was that a within-group difference was observed on continuity of attention and combined speed score for the reboxetine-treated arm. The authors attempted to address the issue of pseudo-specificity by determining that the benefits in cognition were not correlated with changes in overall depression symptom severity score, as measured by the Hamilton Depression Rating Scale 17-Item (HAM-D-17) [47].
As part of a randomized, double-blind, placebo-controlled study, the primary effects of duloxetine on measures of cognition were evaluated in non-demented adults fulfilling DSM-IV criteria for MDD receiving either duloxetine (60 mg/day; n = 207) or placebo (n = 104) for 8 weeks. This study specified a priori an analytical plan that sought to determine possible direct effects of duloxetine on measures of cognition as evidenced by path analysis. The primary efficacy outcome was a composite neurocognitive metric comprising verbal learning and recall, digit-symbol substitution test (DSST), two-digit cancellation test, and letter-number sequencing. Secondary efficacy measures were changed from baseline on the Geriatric Depression Scale, HAM-D-17, Visual Analogue Scale for Pain, and the Clinical Global Impression Severity Scale [48].
Duloxetine significantly improved cognitive performance when compared with placebo in all subjects. Individuals with more severe depression were observed to experience notable improvements with duloxetine over placebo. The improvement in the composite cognitive score noted with duloxetine was driven mainly by improvements in verbal learning and memory. Significant differences were not seen in the duloxetine-treated group relative to placebo with the DSST, two-digit cancellation, and letter-number sequencing. Significant improvements in general symptomatic and functional measures were observed among depressed subjects treated with duloxetine, relative to placebo. In the pre-specified path analysis, it was determined that improvements in cognition were associated with a 90.9 % direct effect and a 9.1 % indirect effect through improvement in the Geriatric Depression Scale total score; similarly, there was an 81.3 % direct effect and an 18.7 % indirect effect through improvement in the HAM-D-17 score.
Vortioxetine, a novel, multi-modal antidepressant that acts on receptor activity and serotonin receptor inhibition, was initially investigated for possible beneficial effects on measures of cognition post hoc in a study primarily designed to compare vortioxetine (5 mg) versus placebo on measures of depressive symptoms in non-demented elderly (aged over 65 years) with recurrent moderate-to-severe depression [i.e., Montgomery–Asberg Depression Rating Scale (MADRS) score of at least 26 at screening and baseline visits] [49]. Cognitive function was assessed with the DSST and the Ray Visual Learning Test (RAVLT). The study included duloxetine (60 mg) as an active reference arm. At the end of 8 weeks of treatment, both vortioxetine- and duloxetine-treated subjects exhibited significant improvement in depression symptom severity as assessed with the 24-item HAM-D scale. Moreover, on the DSST, vortioxetine, but not duloxetine, showed significant improvement compared with placebo on the number of correct symbols. On the RAVLT, both vortioxetine and duloxetine showed an improvement compared with placebo on acquisition and delayed recall measures.
The standardized effect sizes for vortioxetine treatment using the DSST was 0.25. The effect size estimate using the DSST as the dependent measure in the duloxetine-treated subjects was 0.07. The RAVLT has two components (i.e. acquisition and recall). The effect size estimate for the total RAVLT in the vortioxetine-treated group was 0.27. For acquisition and recall, as measured by the RAVLT subscales, the vortioxetine effect sizes were 0.27 and 0.24, respectively. The total effect size using the RAVLT in the duloxetine-treated group was 0.33. The acquisition and recall subcomponent effect sizes in the duloxetine-treated group were 0.33 and 0.32, respectively. The foregoing effect sizes demonstrate significant differences between vortioxetine-treated and duloxetine-treated subjects on the DSST, while a similar effect size was observed for both treatments using RAVLT. Path analysis indicated that vortioxetine had an 83 % direct effect on the DSST (duloxetine 26 %); on RAVLT acquisition, vortioxetine had a 71 % direct effect (duloxetine 65 %); on the RAVLT recall, vortioxetine had a 72 % direct effect (duloxetine 66 %). The results of this industry-sponsored trial (i.e., Lundbeck) replicated the results of the aforementioned duloxetine trial insofar as demonstrating benefit for duloxetine and its effect on RAVLT measures and its lack of benefit on DSST [48].
A recent study with vortioxetine was the first to evaluate the effects of an antidepressant on measures of cognitive function in patients (i.e., aged 18–65 years) with DSM-IV-defined MDD [50]. This double-blind, randomized, fixed-dose, placebo-controlled study compared vortioxetine at two fixed doses (10 and 20 mg) versus placebo on measures of cognition in patients with recurrent, moderate-to-severe MDE (i.e., MADRS scores ≥26 at screening and baseline). The primary cognition measure was a composite of the DSST and RAVLT, expressed as a z-score with equal weighting given to both tests. Secondary objective measures were TMT (Part A and B), Stroop Test (Congruent/Incongruent), Simple Reaction Time, Choice Reaction Time, and the Perceived Deficits Questionnaire (PDQ). Additional secondary measures were change at baseline on MADRS, Clinical Global Scale-Improvement/Severity (CGS-I/S).
On the pre-defined primary efficacy analysis, both doses of vortioxetine were significantly superior to placebo in mean change from baseline to week 8 in the composite z-score, with a mean treatment difference to placebo of 0.36 (vortioxetine 10 mg) and 0.33 (vortioxetine 20 mg). At week 8, separation from placebo was seen for all secondary objective cognitive measures at both doses (10 and 20 mg) with the exception of vortioxetine 20 mg/day on the choice recognition test. On the PDQ total score and subscale scores at week 8, patients in both vortioxetine doses separated from placebo. Both vortioxetine doses demonstrated significant difference relative to placebo on depressive symptoms and CGI variables. The direct effects on the primary endpoint (i.e., combination of DSST and RAVLT) was established with path analysis wherein it was determined that the majority of benefit obtained on the composite cognition measure was a direct effect (i.e., 64 and 48 % for vortioxetine 10 and 20 mg, respectively, for the composite z-score).
Several lines of evidence indicate that subjective measures of cognition at baseline minimally correlate with objective measures of cognition. Moreover, results from patient-reported outcomes research indicates that measures that include patient perspective of cognitive function are prioritized as critical therapeutic objectives towards recovery in MDD [25]. Subjectively experienced cognitive function, as measured by the PDQ, significantly improved in the vortioxetine treatment group on the total score as well as each of the subdomain scores (i.e., planning/organization, attention/concentration, prospective and retrospective memory). The latter results indicate that vortioxetine improves both objective and subjective measures of cognitive function independent of its effect on depressive symptom severity.
The results of the McIntyre et al. [50] study were replicated and extended in a similar trial that primarily evaluated the effect of vortioxetine on measures of cognition (i.e., DSST) in patients (i.e., n = 602, age 18–65 years) with recurrent, moderate-to-severe (i.e., MADRS score ≥26 at screening and baseline) [78]. In addition to meeting criteria for an MDE, eligible subjects also needed to report subjective cognitive function (slow thinking, difficulty focusing and learning or remembering new information). The primary efficacy measure was change from baseline on the total score of the DSST. Secondary measures were the Groton Maze Learning Task, One-Back Task, Stroop Test, TMT (Part A and B), Simple Reaction Time and Choice Reaction Time, PDQ and Cognitive and Physical Functioning Questionnaire (CPFQ). Along with measures of cognition, additional secondary measures were improvement in depression symptom severity as well as functional status, as measured by the University of California San Diego Performance-Based Skills Assessment (UPSA) and the Workplace Limitations Questionnaire (WLQ) [51].
Methodological approaches that aim to evaluate patient functional status are fivefold: (1) patient-reported; (2) clinician-reported; (3) informant-reported; (4) in vivo evaluation (i.e. directly in ecosystem of interest); and (5) performance-based skills assessment. The UPSA has been validated, shown to be sensitive to change, is available in more than 20 languages, requires approximately 30 min for completion, and is demonstrated to be an easy to administer repeat measure. The UPSA evaluates five domains: communication, finance, planning recreational activities, transportation, and household chores. The UPSA brief (UPSA-B) evaluates communication and finance only and has been shown to have a high level of correlation with UPSA (approximately 0.9) as well as with general cognitive measures (approximately 0.5) and negative symptoms (approximately 0.3) in adults with schizophrenia [52].
After 8 weeks of randomized, double-blind, placebo-controlled flexible-dose treatment with vortioxetine (10–20 mg), a significant change from baseline on the primary cognition measure (i.e., DSST) was observed in the vortioxetine-treated sample as compared with the placebo-treated group. The active reference arm, i.e. duloxetine-treated subjects, did not exhibit a significant change relative to placebo on the DSST. Path analysis indicated that 75.7 % of vortioxetine’s effect on DSST was a direct effect, while the direct effect for duloxetine on DSST was 48.7 %. Significant benefit was also seen for vortioxetine and duloxetine on the PDQ total score. The estimated direct effect of vortioxetine on PDQ was 43 % while for duloxetine it was 45 %.
At the end of 8 weeks of treatment, a significant benefit was seen in the vortioxetine-treated subjects on the UPSA composite total score versus placebo, but not in the duloxetine-treated subjects. It was determined that 97 % of the effect of vortioxetine on UPSA was a direct effect compared to 67 % for duloxetine. Moreover, it was determined that vortioxetine-treated subjects exhibited a significant improvement relative to the placebo group on the UPSA-B total score while the duloxetine-treated subjects exhibited a non-significant change from placebo.
A relatively small percentage of subjects completed the WLQ (34 %) as subjects must have been employed for 14 days before baseline. This observation of low instrument completion makes the results of this particular instrument (which were non-significant for both groups) non-interpretable.
The results of the two studies with vortioxetine wherein the primary outcome of interest was cognitive function provide replicated direct evidence of clinically significant effects on objective measures of cognitive function; an effect that is largely a direct effect and not attributable to depressive symptom improvement. The replication of studies indicates that along with an advantage for vortioxetine on measures of cognition, vortioxetine treatment was also associated with significant improvement in measures of function while duloxetine treatment was not. The results of the foregoing vortioxetine studies with duloxetine as a reference, along with results in the two foregoing geriatric studies, indicate that although vortioxetine and duloxetine have similar beneficial effects on depression symptom severity, there are significant differences between these two agents in their ability to improve measures of cognition. Namely, duloxetine is capable of improving measures of learning and memory while vortioxetine improves a broader range of measures (i.e., executive function, learning and memory, processing speed, attention and concentration). Moreover, vortioxetine exerts a beneficial effect on self-rated measures of cognition and measures of function [50].
The link between improved measures of cognitive function and overall function/recovery underscores the importance of improving cognitive function in adults with MDD. For example, it has been reported that in adults with MDD who failed to recover successfully 6 months post discharge from hospital, measures of cognition are inferior to those with MDD who fully recover [20]. Recent results from the International Mood Disorders Collaborative Project (IMDCP) representing collaboration between the Mood Disorders Psychopharmacology Unit (MDPU), University Health Network, Toronto, Ontario, Canada, and the Cleveland Clinic, Cleveland, Ohio, USA, provide further evidence of the link between cognitive dysfunction and workplace function [77]. The IMDCP analyzed results that included adults (n = 260; aged 18–87 years) with DSM-IV-TR-defined MDD who were utilizing tertiary outpatient/inpatient services for MDD. Cognition was evaluated with the 18-item Attention/Deficit Hyperactivity Disorder self-report scale (ASRS). The ASRS evaluates two domains: inattention and hyperactivity-impulsivity. The inattention subscale was used to evaluate subjective symptoms over the past 6 months. The ASRS includes measures of organization/planning, memory, attention, and information/processing speed. The primary question addressed is the extent to which the overall depression symptom severity (i.e. as measured by HAM-D-17) explains variance in workplace performance [as measured by the Endicott Work Productivity Scale (EWPS)].
The EWPS assesses the degree of difficulty in accomplishing work objectives as well as changes in behavior related to work productivity, including absenteeism and presenteeism. It was determined that total depression symptom severity accounted for a relatively low percentage of variance on the EWPS (approximately 18 %) while self-reported measures of cognition (i.e., ASRS) accounted for 58 % of the variance on the EWPS scale. Taken together, results indicate that measures of cognition disproportionally account for the variance on functional outcomes when compared with total depressive symptom severity.
3.1.2 Psychostimulants
A robust and replicated body of controlled scientific evidence reliably indicates that psychostimulants as a class are not broadly effective in mitigating depressive symptoms in adults with MDD [53, 54]. Notwithstanding, the pharmacodynamic profile of psychostimulants suggests that this class of agents would be predicted to be differentially effective in the cognitive domain in adults with MDD. In keeping with that view, a randomized, double-blind, placebo-controlled parallel multi-center study evaluated and compared the effect of lisdexamfetamine versus placebo in adults with full or partial remission of depressive symptoms in MDD. Executive function was evaluated with a self-rated scale, BRIEF-A, which is a psychometrically validated executive function assessment tool. This study enrolled 143 adults (aged 18–55 years) with mild depressive symptoms (i.e. MADRS score ≤18) [55].
The primary endpoint was change from baseline to week 9 in BRIEF-A self-report. The secondary assessment included the BRIEF-A informant report as well as depression outcomes measured with MADRS. At the end of the study, the lisdexamfetamine-treated subjects exhibited greater improvement compared with placebo as measured by the BRIEF-A self-report scale. In addition to improvements in cognitive function, significant improvements in depressive symptoms were also reported. These results, which await replication, provide an important strategic approach for future drug and treatment development (i.e., the domain-specific targeting of symptoms and dysfunction in MDD rather than the traditional ‘broad spectrum’ approach) [55].
Modafinil has psychostimulant-like properties and has been demonstrated, with in vitro and in vivo studies, to block the reuptake of dopamine. Trial evidence in MDD demonstrates that modafinil, like psychostimulants, is not broadly an ‘antidepressant’; notwithstanding, modafinil does exert a significant effect, relative to placebo, on measures of fatigue and psychomotor performance [56]. The beneficial effects of modafinil on cognitive function have been demonstrated in healthy controls [57, 58]. The effect of modafinil on measures of cognitive function in younger individuals with MDD has not been sufficiently studied.
A reasonable expectation of possible benefit from a psychostimulant would be expected in discrete domains of cognitive function (i.e. executive function) in individuals receiving antidepressant therapy who continue to evince cognitive dysfunction. A similar therapeutic expectation may be extrapolated to modafinil.
3.1.3 Other Agents
Erythropoietin (EPO) has neurotrophic actions and aids neurocognitive function. One exploratory study investigated whether recombinant human EPO improves mood and memory in treatment-resistant depression [59]. Treatment-resistant depressed unipolar patients (n = 40) with HAM-D-17 score ≥17 were randomized to eight weekly EPO (Eprex; 40,000 IU) or saline infusions in a double-blind, placebo-controlled, parallel-group design. Patients were assessed at baseline and at weeks 5, 9, and 14. Primary outcome was reduction in HAM-D-17 score. Secondary outcome was remission rate, and tertiary outcomes were changes in RAVLT. Exploratory outcomes were depression and cognition composite scores. HAM-D-17, Global Assessment of Functioning (GAF), and remission rates showed no effects of EPO over saline but EPO produced mood-independent enhancement of verbal learning and memory, which was maintained 6 weeks after treatment completion. These findings highlight EPO as an interesting compound for add-on treatment of cognitive impairment in patients with MDD.
In addition to EPO, other agents with possible beneficial effects for the cognitive dimension/domain in MDD would include but are not limited to intranasally delivered insulin, anti-inflammatory agents [e.g. non-steroidal anti-inflammatory drugs (NSAIDs), cytokine modulators], amino acid modulators (e.g. ketamine), mitochondrial modulators (e.g. N-acetylcysteine), as well as agents relevant to cofactor intermediate synthesis (e.g. l-methylfolate, S-adenosylmethionine) [12, 60, 61]. For each of these agents, convergent evidence indicates that the foregoing systems may be relevant to the pathogenesis and/or treatment of mood disorders. With the exception of intranasally delivered insulin, most of the foregoing agents have not been primarily studied targeting the dimension/domain of cognition. Available evidence strongly indicates that intranasally delivered insulin is specifically beneficial to this dimension/domain based on results in amnestic mild cognitive impairment, Alzheimer’s disease, and bipolar disorder [62, 63].
3.2 Non-Pharmacological Approaches
3.2.1 Neurostimulation
Electroconvulsive therapy (ECT) has well established adverse effects on autobiographical memory. Notwithstanding, the totality of evidence indicates that ECT exerts a beneficial effect on measures of cognitive performance in adults with MDD. For example, a systematic review and meta-analysis of 84 studies comprising 2981 patients included 24 cognitive variables analyzed. The inclusion criteria consisted of an age of ≥18 years, and studies that only utilized bitemporal, right unilateral d’Elia, or Lancaster electrode positions. Mean age and anesthesia used in the studies were not stated in the original article. It was concluded, somewhat surprisingly, that no standardized retrograde amnesia tests were identified. Significant decrease in cognitive performance was observed from 0–3 days following ECT treatment in 72 % of variables. Effect sizes ranged from −1.10 to −0.21 at 4–15 days post-ECT. No negative effect sizes were observed after 15 days, with 57 % of variables showing positive effects sizes, ranging from 0.35 to 0.75. The possible contribution of anesthetics was not explored as the subgroup data were limited [64]. Nevertheless, these results should be interpreted with caution, as the follow-up time did not exceed 15 days; thus, it should not be interpreted to mean that ECT is without cognitive disadvantages.
A compelling rationale exists for evaluating other neuromodulatory modalities with a specific emphasis on the beneficial effects on measures of cognitive function [e.g., Repetitive Transcranial Magnetic Stimulation (rTMS)]. Preliminary evidence also indicates that deep brain stimulation (DBS) may have beneficial effects on measures of cognition [65, 66].
3.2.2 Aerobic Exercise
The results from several original studies as well as systematic reviews and meta-analyses have documented the unequivocal effect of exercise in adults with MDD [67, 68]. The beneficial effects of aerobic exercise on cognitive measures in older adults with MDD are suggested by available literature [69, 70]. However, no studies are available that have primarily evaluated disparate modalities of exercise on measures of cognition in patients with MDD. Such a study would need to embrace many of the methodological principles enumerated in Table 1 [71–73].
3.2.3 Cognitive Remediation
Cognitive remediation (CR) uses behavioral strategies to exert a beneficial effect across a broad range of interpersonal/social skills. The beneficial effects of CR have been documented in schizophrenia, autism, traumatic brain injury, as well as other brain disorders [74, 75]. Results from a single-center study enrolling adults with MDD (n = 33) sought to determine whether CR would result in improvement in neurocognition and general functioning compared with a waitlist control group. Neurocognition was evaluated with the Symbol Coding Task, Continuous Performance Test, Controlled Oral Word Association Test, Animal Naming Tests, Hopkins Verbal Learning Test, Letter-Number Sequencing, TMT (Part B), and Stroop. Interpersonal function was assessed with the Social Skills Performance Assessment (SSPA), general functioning with the Longitudinal Interval Follow-Up Evaluation Range of Impaired Functioning Tool (LIFE-RIFT), and adaptive skills were evaluated with the Advanced Finances Test.
CR was conducted weekly for 90 min per session for 10 weeks. The sessions included three participants per group and consisted of three components: computer-based drill-based exercises, strategic self-monitoring, and ‘bridging’. In addition, the participants were given homework activities [76]. At endpoint, a significant time-by-group interaction was noted for attention and information processing speed as well as verbal learning and memory. Time-by-treatment effects were also significant for executive function. However, no significant time-by-treatment group interactions were observed on the SSPA or the Advanced Finances test. A significant limitation of CR at this point in MDD is whether CR is able to exhibit ‘near-transfer’, i.e., does it benefit domains of cognition as well as ‘far-transfer’, i.e. transfer to the everyday real-world environment. More specifically, evidence is lacking that ‘near-transfer’ occurs reliably across most cognitive domains, and evidence of ‘far-transfer’ has not been reproduced.
4 Conclusions
Several conclusions can be derived from extant literature. First, cognition is a discrete and critical dimension/domain influencing health outcomes in MDD. The foregoing health outcomes may be mediated directly by cognition and/or indirectly (e.g., pseudospecificity, decreased compliance with treatment). Moreover, cognitive dysfunction is critical to health-related quality of life and may be a determinant of non-adherence in some individuals with MDD.
Second, the cognitive domain is subserved by discrete yet overlapping brain networks. There is a need for a glossary and consensually agreed upon definition(s) of cognitive function as well as a standardized measurement approach that concords with busy office practice. The clinical ecosystem requires an appropriate tool to screen, measure, and determine the effect of intervention on the dimension/domain of cognitive function.
Third, the first step towards mitigating cognitive dysfunction in MDD is via prevention of multiple episode course, attention to psychiatric comorbidity (e.g., anxiety disorders, substance abuse disorders), and medical comorbidity (e.g., obesity, diabetes mellitus, thyroid dysfunction). It also would be pragmatic to avoid, where possible, concomitant medications that interfere with cognitive function (e.g., benzodiazepines) as well as vigilance for the possible impairing effects of some antidepressants (e.g. tricyclic antidepressants) on cognitive function.
Fourth, relatively few antidepressants have been specifically studied as to their specific benefit in target domains independent of other domains in MDD. Broad-spectrum independent beneficial effects on cognition have been demonstrated for vortioxetine; more narrow benefits (e.g., learning and memory) have been demonstrated with duloxetine. For other antidepressants, pseudospecificity cannot be excluded as a possible explanation of their beneficial effects on the cognitive domain.
Finally, the pertinence of cognitive dysfunction in MDD is underscored by replicated evidence indicating that MDD debases human capital and is a leading cause of disability in both developed and developing nations. The tremendous cost associated with depression is related largely to impairment in role function. It remains an open question as to whether treatments capable of mitigating cognitive deficits may also be able to improve overall health outcomes (e.g., workplace performance) and illness trajectory in MDD.
References
Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA. 2003;289(23):3095–105.
Vasiliadis HM, Lesage A, Adair C, Wang PS, Kessler RC. Do Canada and the United States differ in prevalence of depression and utilization of services? Psychiatr Serv. 2007;58(1):63–71.
Birnbaum HG, Kessler RC, Kelley D, Ben-Hamadi R, Joish VN, Greenberg PE. Employer burden of mild, moderate, and severe major depressive disorder: mental health services utilization and costs, and work performance. Depress Anxiety. 2010;27(1):78–89.
Collins PY, Insel TR, Chockalingam A, Daar A, Maddox YT. Grand challenges in global mental health: integration in research, policy, and practice. PLoS Med. 2013;10(4):e1001434.
Kessler RC, Barber C, Birnbaum HG, Frank RG, Greenberg PE, Rose RM, et al. Depression in the workplace: effects on short-term disability. Health Aff (Millwood). 1999;18(5):163–71.
Greenberg PE, Kessler RC, Birnbaum HG, Leong SA, Lowe SW, Berglund PA, et al. The economic burden of depression in the United States: how did it change between 1990 and 2000? J Clin Psychiatry. 2003;64(12):1465–75.
Pratt LA, Brody DJ, Gu Q. Antidepressant use in persons aged 12 and over: United States, 2005–2008. NCHS Data Brief. 2011;76:1–8.
Trivedi MH, Rush AJ, Wisniewski SR, Nierenberg AA, Warden D, Ritz L, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry. 2006;163(1):28–40.
McIntyre RS. A vision for drug discovery and development: novel targets and multilateral partnerships. Adv Ther. 2014;31:245–6.
Insel TR. The NIMH Research Domain Criteria (RDoC) Project: precision medicine for psychiatry. Am J Psychiatry. 2014;171(4):395–7.
Millan MJ, Agid Y, Brune M, Bullmore ET, Carter CS, Clayton NS, et al. Cognitive dysfunction in psychiatric disorders: characteristics, causes and the quest for improved therapy. Nat Rev Drug Discov. 2012;11(2):141–68.
McIntyre RS, Cha DS, Soczynska JK, Woldeyohannes HO, Gallaugher LA, Kudlow P, et al. Cognitive deficits and functional outcomes in major depressive disorder: determinants, substrates, and treatment interventions. Depress Anxiety. 2013;30:515–27.
Roiser JP, Sahakian BJ. Hot and cold cognition in depression. CNS Spectr. 2013;18(3):139–49.
Pulcu E, Thomas EJ, Trotter PD, McFarquhar M, Juhasz G, Sahakian BJ, et al. Social-economical decision making in current and remitted major depression. Psychol Med. 2014;10:1–13.
Amft M, Bzdok D, Laird AR, Fox PT, Schilbach L, Eickhoff SB. Definition and characterization of an extended social-affective default network. Brain Struct Funct. 2015;220:1031–49.
Ladegaard N, Larsen ER, Videbech P, Lysaker PH. Higher-order social cognition in first-episode major depression. Psychiatry Res. 2014;216(1):37–43.
Harmer CJ, O’Sullivan U, Favaron E, Massey-Chase R, Ayres R, Reinecke A, et al. Effect of acute antidepressant administration on negative affective bias in depressed patients. Am J Psychiatry. 2009;166(10):1178–84.
Haddad AD, Williams JM, McTavish SF, Harmer CJ. Low-dose tryptophan depletion in recovered depressed women induces impairments in autobiographical memory specificity. Psychopharmacology (Berl). 2009;207(3):499–508.
Freedman R, Lewis DA, Michels R, Pine DS, Schultz SK, Tamminga CA, et al. The initial field trials of DSM-5: new blooms and old thorns. Am J Psychiatry. 2013;170(1):1–5.
Jaeger J, Berns S, Uzelac S, Davis-Conway S. Neurocognitive deficits and disability in major depressive disorder. Psychiatry Res. 2006;145(1):39–48.
Conradi HJ, Ormel J, de Jonge P. Presence of individual (residual) symptoms during depressive episodes and periods of remission: a 3-year prospective study. Psychol Med. 2010;8:1–10.
Luo LL, Chen X, Chai Y, Li JH, Zhang M, Zhang JN. A distinct pattern of memory and attention deficiency in patients with depression. Chin Med J. 2013;126(6):1144–9.
Mandelli L, Serretti A, Colombo C, Florita M, Santoro A, Rossini D, et al. Improvement of cognitive functioning in mood disorder patients with depressive symptomatic recovery during treatment: an exploratory analysis. Psychiatry Clin Neurosci. 2006;60(5):598–604.
Zimmerman M, Posternak MA, Chelminski I. Using a self-report depression scale to identify remission in depressed outpatients. Am J Psychiatry. 2004;161(10):1911–3.
Zimmerman M, McGlinchey JB, Posternak MA, Friedman M, Attiullah N, Boerescu D. How should remission from depression be defined? The depressed patient’s perspective. Am J Psychiatry. 2006;163(1):148–50.
Papakostas GI. Cognitive symptoms in patients with major depressive disorder and their implications for clinical practice. J Clin Psychiatry. 2014;75(1):8–14.
Gualtieri CT, Morgan DW. The frequency of cognitive impairment in patients with anxiety, depression, and bipolar disorder: an unaccounted source of variance in clinical trials. J Clin Psychiatry. 2008;69(7):1122–30.
Samartzis L, Gavala E, Zoukos Y, Aspiotis A, Thomaides T. Perceived cognitive decline in multiple sclerosis impacts quality of life independently of depression. Rehabil Res Pract. 2014;2014:128751.
Thelen JM, Lynch SG, Bruce AS, Hancock LM, Bruce JM. Polypharmacy in multiple sclerosis: relationship with fatigue, perceived cognition, and objective cognitive performance. J Psychosom Res. 2014;76(5):400–4.
Airaksinen E, Wahlin A, Forsell Y, Larsson M. Low episodic memory performance as a premorbid marker of depression: evidence from a 3-year follow-up. Acta Psychiatr Scand. 2007;115(6):458–65.
Watters AJ, Gotlib IH, Harris AW, Boyce PM, Williams LM. Using multiple methods to characterize the phenotype of individuals with a family history of major depressive disorder. J Affect Disord. 2013;150(2):474–80.
van Oostrom I, Franke B, Arias VA, Rinck M, Tendolkar I, Verhagen M, et al. Never-depressed females with a family history of depression demonstrate affective bias. Psychiatry Res. 2013;205(1–2):54–8.
Christensen MV, Kyvik KO, Kessing LV. Cognitive function in unaffected twins discordant for affective disorder. Psychol Med. 2006;36(8):1119–29.
Martinez-Aran A, Vieta E, Colom F, Reinares M, Benabarre A, Gasto C, et al. Cognitive dysfunctions in bipolar disorder: evidence of neuropsychological disturbances. Psychother Psychosom. 2000;69(1):2–18.
Godard J, Baruch P, Grondin S, Lafleur MF. Psychosocial and neurocognitive functioning in unipolar and bipolar depression: a 12-month prospective study. Psychiatry Res. 2012;196(1):145–53.
Insel TR. Translating scientific opportunity into public health impact: a strategic plan for research on mental illness. Arch Gen Psychiatry. 2009;66(2):128–33.
Diamond PA. What stock market returns to expect for the future? Soc Secur Bull. 2000;2:38–52.
Baune BT, Miller R, McAfoose J, Johnson M, Quirk F, Mitchell D. The role of cognitive impairment in general functioning in major depression. Psychiatry Res. 2010;176(2–3):183–9.
Krishnan V, Nestler EJ. Linking molecules to mood: new insight into the biology of depression. Am J Psychiatry. 2010;167(11):1305–20.
Greicius MD, Krasnow B, Reiss AL, Menon V. Functional connectivity in the resting brain: a network analysis of the default mode hypothesis. Proc Natl Acad Sci USA. 2003;100(1):253–8.
Uddin LQ, Kelly AM, Biswal BB, Xavier CF, Milham MP. Functional connectivity of default mode network components: correlation, anticorrelation, and causality. Hum Brain Mapp. 2009;30(2):625–37.
Herrera-Guzman I, Gudayol-Ferre E, Herrera-Guzman D, Guardia-Olmos J, Hinojosa-Calvo E, Herrera-Abarca JE. Effects of selective serotonin reuptake and dual serotonergic-noradrenergic reuptake treatments on memory and mental processing speed in patients with major depressive disorder. J Psychiatr Res. 2009;43(9):855–63.
Herrera-Guzman I, Gudayol-Ferre E, Herrera-Abarca JE, Herrera-Guzman D, Montelongo-Pedraza P, Padros BF, et al. Major Depressive Disorder in recovery and neuropsychological functioning: effects of selective serotonin reuptake inhibitor and dual inhibitor depression treatments on residual cognitive deficits in patients with Major Depressive Disorder in recovery. J Affect Disord. 2010;123(1–3):341–50.
Lam R, Lonn S, Despiegel N. Escitalopram versus serotonin noradrenaline reuptake inhibitors as second step treatment for patients with major depressive disorder: a pooled analysis. Int Clin Psychopharmacol. 2010;25(4):199–203.
Borkowska A, Drozdz W, Ziolkowska-Kochan M, Rybakowski J. Enhancing effect of mirtazapine on cognitive functions associated with prefrontal cortex in patients with recurrent depression. Neuropsychopharmacol Hung. 2007;9(3):131–6.
Sasada K, Iwamoto K, Kawano N, Kohmura K, Yamamoto M, Aleksic B, et al. Effects of repeated dosing with mirtazapine, trazodone, or placebo on driving performance and cognitive function in healthy volunteers. Hum Psychopharmacol. 2013;28(3):281–6.
Ferguson JM, Wesnes KA, Schwartz GE. Reboxetine versus paroxetine versus placebo: effects on cognitive functioning in depressed patients. Int Clin Psychopharmacol. 2003;18(1):9–14.
Raskin J, Wiltse CG, Siegal A, Sheikh J, Xu J, Dinkel JJ, et al. Efficacy of duloxetine on cognition, depression, and pain in elderly patients with major depressive disorder: an 8-week, double-blind, placebo-controlled trial. Am J Psychiatry. 2007;164(6):900–9.
Katona C, Hansen T, Olsen CK. A randomized, double-blind, placebo-controlled, duloxetine-referenced, fixed-dose study comparing the efficacy and safety of Lu AA21004 in elderly patients with major depressive disorder. Int Clin Psychopharmacol. 2012;27(4):215–23.
McIntyre RS, Lophaven S, Olsen CK. A randomized, double-blind, placebo-controlled study of vortioxetine on cognitive function in depressed adults. Int J Neuropsychopharmacol. 2014;30:1–11.
Patterson TL, Goldman S, McKibbin CL, Hughs T, Jeste DV. UCSD Performance-Based Skills Assessment: development of a new measure of everyday functioning for severely mentally ill adults. Schizophr Bull. 2001;27(2):235–45.
Olsson AK, Helldin L, Hjarthag F, Norlander T. Psychometric properties of a performance-based measurement of functional capacity, the UCSD Performance-based Skills Assessment—brief version. Psychiatry Res. 2012;197(3):290–4.
Candy M, Jones L, Williams R, Tookman A, King M. Psychostimulants for depression. Cochrane Database Syst Rev. 2008;2:CD006722.
McIntyre RS, Filteau M-J, Martin L, Patry S, Carvalho A, Cha DS, et al. Treatment-resistant depression: definitions, review of the evidence, and algorithmic approach. J Affect Disord. 2014;156:1–7.
Madhoo M, Keefe RSE, Roth RM, Sambunaris A, Wu J, Trivedi MH, et al. Lisdexamfetamine dimesylate augmentation in adults with persistent executive dysfunction after partial or full remission of major depressive disorder. Neuropsychopharmacol Off Publ Am Coll Neuropsychopharmacol. 2014;39(6):1388–98.
Goss AJ, Kaser M, Costafreda SG, Sahakian BJ, Fu CHY. Modafinil augmentation therapy in unipolar and bipolar depression: a systematic review and meta-analysis of randomized controlled trials. J Clin Psychiatry. 2013;74(11):1101–7.
Minzenberg MJ, Carter CS. Modafinil: a review of neurochemical actions and effects on cognition. Neuropsychopharmacol Off Publ Am Coll Neuropsychopharmacol. 2008;33(7):1477–502.
Kelley AM, Webb CM, Athy JR, Ley S, Gaydos S. Cognition enhancement by modafinil: a meta-analysis. Aviat Space Environ Med. 2012;83(7):685–90.
Miskowiak KW, Vinberg M, Christensen EM, Bukh JD, Harmer CJ, Ehrenreich H, et al. Recombinant human erythropoietin for treating treatment-resistant depression: a double-blind, randomized, placebo-controlled phase 2 trial. Neuropsychopharmacol Off Publ Am Coll Neuropsychopharmacol. 2014;39(6):1399–408.
Solé B, Jiménez E, Martinez-Aran A, Vieta E. Cognition as a target in major depression: new developments. Eur Neuropsychopharmacol [Internet]; 2015. http://linkinghub.elsevier.com/retrieve/pii/S0924977X14003514. Cited 15 Feb 2015.
Liu CS, Carvalho AF, McIntyre RS. Towards a “metabolic” subtype of major depressive disorder: shared pathophysiological mechanisms may contribute to cognitive dysfunction. CNS Neurol Disord Drug Targets. 2014;13(10):1693–707.
Reger MA, Watson GS, Frey WH, Baker LD, Cholerton B, Keeling ML, et al. Effects of intranasal insulin on cognition in memory-impaired older adults: Modulation by APOE genotype. Neurobiol Aging. 2005;27(3):451–8.
McIntyre RS, Soczynska JK, Woldeyohannes HO, Miranda A, Vaccarino A, Macqueen G, et al. A randomized, double-blind, controlled trial evaluating the effect of intranasal insulin on neurocognitive function in euthymic patients with bipolar disorder. Bipolar Disord. 2012;14(7):697–706.
Semkovska M, McLoughlin DM. Objective cognitive performance associated with electroconvulsive therapy for depression: a systematic review and meta-analysis. Biol Psychiatry. 2010;68(6):568–77.
Bergfeld IO, Mantione M, Hoogendoorn ML, Denys D. Cognitive functioning in psychiatric disorders following deep brain stimulation. Brain Stimul. 2013;6(4):532–7.
Demirtas-Tatlidede A, Vahabzadeh-Hagh AM, Pascual-Leone A. Can noninvasive brain stimulation enhance cognition in neuropsychiatric disorders? Neuropharmacology. 2013;64:566–78.
Mammen G, Faulkner G. Physical activity and the prevention of depression: a systematic review of prospective studies. Am J Prev Med. 2013;45(5):649–57.
Cooney GM, Dwan K, Greig CA, Lawlor DA, Rimer J, Waugh FR, et al. Exercise for depression. Cochrane Database Syst Rev. 2013;9:CD004366.
Pei Z, Meng R, Zhuang Z, Zhao Y, Liu F, Zhu MZ, et al. Cardiac peroxisome proliferator-activated receptor-gamma expression is modulated by oxidative stress in acutely infrasound-exposed cardiomyocytes. Cardiovasc Toxicol. 2013;13(4):307–15.
Legrand FD. Effects of exercise on physical self-concept, global self-esteem, and depression in women of low socioeconomic status with elevated depressive symptoms. J Sport Exerc Psychol. 2014;36(4):357–65.
Rethorst CD, Sunderajan P, Greer TL, Grannemann BD, Nakonezny PA, Carmody TJ, et al. Does exercise improve self-reported sleep quality in non-remitted major depressive disorder? Psychol Med. 2013;43(4):699–709.
Rethorst CD, Toups MS, Greer TL, Nakonezny PA, Carmody TJ, Grannemann BD, et al. Pro-inflammatory cytokines as predictors of antidepressant effects of exercise in major depressive disorder. Mol Psychiatry. 2013;18(10):1119–24.
Trivedi MH, Greer TL, Church TS, Carmody TJ, Grannemann BD, Galper DI, et al. Exercise as an augmentation treatment for nonremitted major depressive disorder: a randomized, parallel dose comparison. J Clin Psychiatry. 2011;72(5):677–84.
Elgamal S, McKinnon MC, Ramakrishnan K, Joffe RT, Macqueen G. Successful computer-assisted cognitive remediation therapy in patients with unipolar depression: a proof of principle study. Psychol Med. 2007;37(9):1229–38.
Thorsen AL, Johansson K, Loberg EM. Neurobiology of cognitive remediation therapy for schizophrenia: a systematic review. Front Psychiatry. 2014;5:103.
Bowie CR, Gupta M, Holshausen K, Jokic R, Best M, Milev R. Cognitive remediation for treatment-resistant depression: effects on cognition and functioning and the role of online homework. J Nerv Ment Dis. 2013;201(8):680–5.
McIntyre RS, Soczynska JK, Woldeyohannes HO, Alsuwaidan MT, Cha DS, Carvalho AF, et al. The impact of cognitive impairment on perceived workforce performance: results from the International Mood Disorders Collaborative Project. Compr Psychiatry. 2015;56:279–82.
Mahableshwarkar AR, Zajecka J, Jacobson W, Chen Y, Keefe RS. A randomized, placebo-controlled, active-referenced, double-blind, flexible-dose study of the efficacy of vortioxetine on cognitive function in major depressive disorder. Neuropsychopharmacology. 2015;40:2025–37.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Roger S. McIntyre is a consultant/receives speaker fees and/or research funding from Eli Lilly, AstraZeneca, Bristol Myers Squibb, Forest, Sunovion, Takeda, Otsuka, Pfizer, Shire, Merck, Lundbeck, Janssen-Ortho, and GSK.
Dr. Andre F. Carvalho is supported by a research fellowship award from the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq; level II; Brazil).
Dr. Maj Vinberg has been a consultant for Eli Lilly, Lundbeck, Servier, and AstraZeneca. Dr. Maj Vinberg’s conflicts of interest had no role in the present manuscript.
Holly X. Xiao, Kahlood Syeda, Dr. Maj Vinberg, Dr. Rodrigo B. Mansur, Nadia Maruschak, and Danielle S. Cha declare no conflict of interests.
Funding
This work was not supported by external funding.
Rights and permissions
About this article
Cite this article
McIntyre, R.S., Xiao, H.X., Syeda, K. et al. The Prevalence, Measurement, and Treatment of the Cognitive Dimension/Domain in Major Depressive Disorder. CNS Drugs 29, 577–589 (2015). https://doi.org/10.1007/s40263-015-0263-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-015-0263-x