Abstract
Etravirine is a second-generation non-nucleoside reverse transcriptase inhibitor (NNRTI) for the treatment of human immunodeficiency virus type 1 infection. It is a potent inhibitor of HIV reverse transcriptase and retains activity against wild-type and most NNRTI-resistant HIV. The pharmacokinetic profile of etravirine and clinical data support twice-daily dosing, although once-daily dosing has been investigated in treatment-naïve and treatment-experienced persons. Despite similar pharmacokinetic and pharmacodynamic results compared with twice-daily dosing, larger studies are needed to fully support once-daily etravirine dosing in treatment-naïve individuals. Etravirine is reserved for use in third- or fourth-line antiretroviral treatment regimens, as recommended, for example, in treatment guidelines by the US Department of Health and Human Services—Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents Living with HIV. Etravirine exhibits the potential for bi-directional drug–drug interactions with other antiretrovirals and concomitant medications through its interactions with cytochrome P450 (CYP) isozymes: CYP3A4, CYP2C9, and CYP2C19. This review summarizes the pharmacokinetic and pharmacodynamic parameters of etravirine, with particular attention to information on drug–drug interactions and use in special patient populations, including children/adolescents, women, persons with organ dysfunction, and during pregnancy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Etravirine is active against wild-type and non-nucleoside reverse transcriptase inhibitor (NNRTI)-resistant HIV virus, and is indicated for use in third- or fourth-line antiretroviral treatment regimens in children, adolescents, and adults. |
Etravirine demonstrates bi-directional drug–drug interaction potential through its interaction as a cytochrome P450 isozyme substrate, inhibitor, and inducer. |
Insufficient data are available to support inclusion in treatment guidelines for the use of etravirine in treatment-naïve persons or administered as once-daily dosing. |
1 Introduction
Etravirine is a second-generation non-nucleoside reverse transcriptase inhibitor (NNRTI) developed for use in the setting of NNRTI-resistant human immunodeficiency virus type 1 (HIV-1) infection due to its activity against NNRTI-resistant HIV strains and a higher genetic barrier to the development of resistance [1]. Etravirine is indicated for use in treatment-experienced persons aged 2 years and older with HIV-1, and retains activity against HIV virus containing NNRTI resistance mutations, including K103N and G190S/A. However, single resistance mutations at L100I, K101E/H/P, and Y181C/I/V impact etravirine response [1,2,3]. Development of drug resistance to etravirine often occurs after emergence of multiple NNRTI mutations [4,5,6]. Thus, etravirine demonstrates a higher genetic barrier to development of drug resistance compared with first-generation NNRTI’s. Phase III clinical trials demonstrated the effectiveness of etravirine compared with placebo when used in combination with an optimized antiretroviral (ARV) background regimen in treatment-experienced children, adolescents, and adults. Therefore, etravirine is commonly reserved for use within third-line antiretroviral therapy (ART) regimens [7,8,9].
Etravirine was approved for use by the US FDA in 2008 and is available in 25, 100, and 200 mg tablets that can be swallowed whole or dispersed in liquid. It is administered as 200 mg twice daily for adults, and with weight-based dosing, not to exceed the adult dose, for children and adolescents aged 2–18 years [10, 11]. Etravirine is metabolized extensively through various cytochrome P450 (CYP) enzymes exhibiting inhibitory (CYP2C19, CYP2C19) and inductive (CYP3A4) properties, posing various considerations for drug–drug interactions (DDIs), as discussed in Sect. 3 [12].
The pharmacokinetic (PK) and pharmacodynamic (PD) characteristics of etravirine were described in Clinical Pharmacokinetics in 2009 [11]. This review summarizes and discusses the clinical PK and PD of etravirine from 2009 to the present in healthy subjects and children, adolescents, and adult persons with HIV, with special regard to dosing frequency, comorbidities, and special populations. DDIs with other ARTs and concomitant medications are also summarized. A review of publications for inclusion in this review was made through a PubMed search using the terms ‘etravirine’ or ‘TMC125’ in combination with ‘pharmacokinetics’, ‘pharmacodynamics’, ‘pharmacogenomics’, ‘pharmacology’, ‘drug transporter’, or ‘drug interactions’.
2 Biopharmaceutics and Pharmacokinetics
2.1 Pharmacokinetics
Etravirine PK have been described in healthy volunteers and individuals with HIV. A significant change in tablet formulation was made during phase II and III studies that significantly improved oral bioavailability and led to the present commercially marketed formulation for which the PK are described herein [13]. Dose and formulation selection have been previously extensively reviewed by Scholler-Gyure et al. [11].
2.2 Absorption
After an oral dose of etravirine, maximum plasma concentrations (Cmax) are reached within 2.5–5 h [14, 15]. The proximal small intestine is likely the primary site of etravirine absorption via passive diffusion [16]. A significant food effect has been shown in fasted and fed studies of healthy volunteers. In the fasted state, daily exposures [area under the concentration–time curve (AUC)] of etravirine were approximately 50% lower than with a meal. Meals consisting of 345–1160 kcal and 17–70 g of dietary fat did not demonstrate significant differences in etravirine bioavailability. A high fiber breakfast (685 kcal, 3 g fat) increased AUC by 25%, while a light breakfast (345 kcal, 17 g fat) increased exposures by 20% [17]. Current etravirine labeling recommends administration following a meal, although the specific meal type is not defined and differences in PK by meal types are likely not clinically relevant [17, 18]. Drug interactions with agents that lower gastric pH, such as ranitidine and omeprazole, did not show a clinically significant effect on absorption [18, 19]. Similarly, PK studies investigating the effect of crushing etravirine tablets have found no clinically significant effect on absorption [20, 21].
2.3 Distribution
Etravirine is extensively (99.9%) bound to plasma proteins. In vitro experiments show 99.6% is bound to albumin (HSA), while 97.7% is bound to α-1-glycoprotein (AAG) [18]. The blood-to-plasma ratio for etravirine is 0.7 [22]. The median protein binding adjusted half maximal effective concentration (EC50) for MT4 cells infected with HIV-1/IIIB in vitro is approximately 4 ng/mL [18]. Antiviral activity of etravirine is covered further in Sect. 4.1. Studies investigating the effect of changes in plasma proteins on antiviral activity of etravirine have shown minimal effect. In the presence of 1 mg/mL AAG or 45 mg/mL HAS (both physiologically excess), EC50 fold changes of 1 and 3 were found [2]. It is worth noting that for highly protein bound drugs, their propensity to displace other highly protein bound drugs may lead to a clinical effect on the displaced drug. In a study of warfarin and etravirine coadministration in rats, clearance of S-warfarin increased approximately threefold in the presence of etravirine. A significant decrease in the amount of warfarin bound to albumin in the presence of etravirine (99.34% vs. 92.38%) was also observed. The changes in unbound concentrations of warfarin were the likely mechanism of increased warfarin clearance [23].
The reported apparent volume of distribution (Vd) of etravirine in the central compartment is 422 L [24]. As etravirine is largely protein bound in circulation, a limited amount of drug passes into the cerebrospinal fluid (CSF). Studies of CSF penetration of etravirine indicate the drug is similarly highly protein bound in the CNS (98.4%). Overall, etravirine CSF concentrations constitute approximately 4.3% of total plasma etravirine, and no correlation between CSF or plasma albumin concentrations and CSF concentrations of etravirine were found [25]. While total CSF concentrations of etravirine in adults with HIV have been shown to be above the in vitro concentration required to inhibit viral replication by 50% (IC50) [26], the unbound fraction of drug in the CSF did not reach the IC50 of etravirine in similar studies of individuals with HIV [25].
Two studies in HIV-infected women receiving etravirine 200 mg twice daily, found cervicovaginal fluid exposures were greater than blood plasma exposures, one reporting a ratio of 1.2 [27, 28]. Seminal and rectal tissue concentrations of etravirine were evaluated in 12 HIV-negative men over 8 days of etravirine 200 mg twice daily. Seminal plasma concentrations of etravirine were approximately 85% lower than those in blood plasma, while protein binding in seminal plasma was less than that of blood plasma, at around 97%. Conversely, exposures of etravirine in rectal tissue were higher than exposures in blood plasma by 20- to 40-fold [29].
2.4 Metabolism and Elimination
Etravirine is primarily metabolized by the CYP3A4, CYP2C9, and CYP2C19 isoenzymes of the CYP family. Oxidation of the parent compound to (mono- and di-)methylhydroxylated metabolites appears to be the major route of metabolism (Fig. 1), with subsequent glucuronidation of these hydroxyl metabolites [30, 31]. The major metabolites of etravirine are > 90% less active against reverse transcriptase than the parent [32]. In mass balance studies, 94.9% of an oral dose was collected by 168 h postdose, and 93.7% of the dose was recovered in feces and 1.2% was recovered in urine. Of the dose captured in the feces, unchanged drug accounted for 81–86% of the administered dose [31]. The terminal elimination half-life of etravirine derived from mass balance studies was 41 h [18, 31]. Etravirine has minimal renal elimination [31], and no studies have been conducted to investigate use in patients with renal impairment.
Metabolism of etravirine (from Scholler-Gyure et al. [11])
2.5 Pharmacokinetics in Healthy Subjects
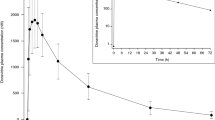
The PK of the etravirine commercial formulation were evaluated in two phase I clinical trials [14]. Daily doses of 200–400 mg were investigated in once- and twice-daily dosing schedules. Overall, equal daily doses resulted in similar exposures, and the exposures were dose proportional across the doses studied [14]. Minimum plasma concentrations (Cmin) were 25–26% lower, while Cmax concentrations were 42–44% higher, with daily dosing compared with twice-daily dosing [14]. Steady state exposures of etravirine after 7 days of dosing demonstrated accumulation ratios of 2.5- to 4-fold for AUC and Cmax [14]. Steady state PK parameters of etravirine in HIV-negative, healthy volunteers are shown in Table 1; representative concentration versus time profiles are shown in Fig. 2.
Pharmacokinetic profile of etravirine administered as 400 mg od [n =37] and 200 mg bid [n =39] of the commercial formulation for 8 days in healthy subjects. Data are expressed as mean (standard deviation) [from Scholler-Gyure et al. [11]. od once daily, bid twice daily
2.6 Pharmacokinetics in HIV-Positive Individuals
Etravirine PK in individuals with HIV were largely derived from the phase III DUET-1 and DUET-2 trials. A general trend for lower concentrations in HIV-infected persons has been observed [14]. Mean (standard deviation [SD]) etravirine AUC from 0 to 12 h (AUC12) and Cmin were 5506 (4710) ng h/mL and 393 (391) ng/mL, respectively, in 575 participants from these two studies. Inter- and intrasubject variability (coefficient of variation) of apparent oral clearance (CL/F) were 60% and 40%, respectively. Etravirine PK were not significantly influenced by sex, age, race, or treatment duration [24]. Hepatitis co-infection was associated with a 1.35-fold increase in AUC12 (p =0.0028) [33]. Subjects with hepatitis B virus co-infection had an 8.3% increase in etravirine CL/F, whereas those with hepatitis C virus co-infection had a 24% decrease in CL/F [24, 33]. Etravirine PK exhibits relatively low interpatient variability (approximately 50% for CL/F); recent studies found approximately 13% and 5% of the interpatient variability in CL/F arises from concomitant ARVs and pharmacogenomics, respectively [34,35,36]. Steady-state PK parameters of etravirine in HIV-positive individuals are shown in Table 1.
2.7 Pharmacokinetics in Special Populations
2.7.1 Hepatic Insufficiency
Phase I mass balance studies of etravirine indicate the primary elimination pathway is via hepatobiliary metabolism (> 93%), whereas renal elimination plays only a minor role (approximately 1.2%) [31]. Studies in HIV-negative volunteers with mild (Child–Pugh A) or moderate (Child–Pugh B) hepatic impairment have shown comparable etravirine exposures (AUC12) to healthy individuals matched for age, sex, race, and body mass index [37]. After 8 days of twice-daily 200 mg dosing, AUC12 was 13% and 18% lower in participants with mild and moderate hepatic impairment, respectively, while Cmax was 13% and 2% lower in the mild and moderate groups, respectively, compared with healthy volunteers. No dose adjustment of etravirine is needed in individuals with mild to moderate hepatic impairment [37]. Etravirine PK have not been evaluated in individuals with severe hepatic impairment.
2.7.2 Pregnancy
Etravirine exposures (AUC12) were 34% higher and CL/F was 52% lower in the third trimester, compared with postpartum, in 15 pregnant women receiving etravirine (200 mg twice daily) containing ART. Median (range) C12 was higher in the third trimester compared with postpartum [0.48 (0.08–1.94) vs. 0.38 (0.07–1.14) μg/mL]. The likely explanation is a pregnancy-induced decrease in CYP2C19 expression [38]. Median cord blood-to-maternal plasma ratios at delivery were 0.52 (range 0.19–4.25). No dose adjustment of etravirine is recommended in pregnant women [38].
2.7.3 Pediatrics
A phase I/II study investigated etravirine PK in 21 treatment-experienced pediatric patients split into two cohorts (Cohort 1: age 2 to < 6 years; Cohort 2: age 1 to < 2 years). Participants received weight-band dosing: 75 mg twice daily (8 to < 10 kg); 100 mg twice daily (10 to < 20 kg); or 125 mg twice daily (20 to < 25 kg) [39, 40]. Etravirine was used in combination with two other ARVs, including a ritonavir-boosted protease inhibitor (PI). The geometric means (CV%) of time to reach Cmax (Tmax), Cmax, and AUC12 for Cohorts 1 and 2 were 4.5 h (42%) versus 2 h (75%), 466 ng/mL (84%) versus 390 ng/mL (89%), and 3823 ng h/mL (95%) versus 3328 ng h/mL (94%), respectively [40].
A Phase I study of 21 patients (> 6–18 years of age) included two stages of etravirine dosing: 4 mg/kg twice daily and 5.2 mg/kg twice daily. Mean (SD) Cmax and AUC12 were 495 (453) versus 757 (680) ng/mL and 4050 (3602) versus 6141 (5586) ng h/mL for the 4 mg/kg and 5.2 mg/kg doses [10]. The 5.2 mg/kg dose showed comparable exposures to adults receiving 200 mg twice daily and was selected for further pediatric development. Table 1 summarizes the etravirine PK parameters in pediatric and adolescent populations [12, 34].
3 Drug–Drug Interactions
Absorption-related DDIs have not been observed with changing gastric pH (ranitidine). An increase in etravirine exposure was observed with omeprazole (Table 2); however, the mechanism is inhibition of etravirine metabolism via CYP2C19 rather than increasing gastric pH [11, 41]. Scholler-Gyure et al. summarized the in vitro and in vivo modified Cooperstown 5 + 1 cocktail results [11], showing etravirine is an inducer of CYP3A and an inhibitor of CYP2C9 and CYP2C19 [41]. Given these characteristics, DDIs between etravirine and coadministered medications are expected. The effect of etravirine on drug transporters in one in vitro study found etravirine did not inhibit p-glycoprotein, was not a substrate for the ABC transporters, and was both an inducer and inhibitor of BCRP/ABCG2 [42]. In vivo data suggest that etravirine is a weak p-glycoprotein inhibitor, as demonstrated by a 19% increase in Cmax of single-dose digoxin (Table 3) [11, 43]. Because etravirine is most commonly used as part of a third-line ART regimen, it is typically combined with multiple classes of ARVs, which may be perpetrators of DDIs. Available DDI data with non-ARV concomitant drugs that result in a change in etravirine PK are summarized in Table 2; changes in the coadministered drug PK and clinical recommendations based on bidirectional effects of the combination are provided in Table 3. A comprehensive reference for DDIs may be found in the Department of Health and Human Services (DHHS) Adult and Adolescent HIV Treatment Guidelines (https://aidsinfo.nih.gov/guidelines/html/1/adult-and-adolescent-treatment-guidelines/0) or the Liverpool drug interactions website (hiv-druginteractions.org).
This review focuses on DDIs when combining etravirine with concomitant ARVs to construct a fully suppressive ART regimen. Table 4 describes the results of PK studies to assess the bidirectional influence of etravirine and individual ARVs. Most studies were conducted in healthy volunteers, with a crossover study design, unless noted otherwise. Data with older ARVs can be found in a prior review by Scholler-Gyure et al. [11]. Some DDI studies discussed in this review were conducted with the initial, lower bioavailability formulation; however, the product labeling applies the findings from these DDI studies to the current commercial product based on similar findings from studies repeated with the commercial product [18, 41, 44].
3.1 Combining Etravirine with Other Antiretrovirals
3.1.1 Entry Inhibitors
The AUC of maraviroc 300 mg twice daily was decreased 53% in combination with etravirine (Table 4), resulting in the recommendation to increase maraviroc to 600 mg twice daily when coadministered [45]. When etravirine and maraviroc (150 mg twice daily) were coadministered with darunavir/ritonavir, the maraviroc AUC was 3.1-fold higher than 150 mg twice daily without a ritonavir-boosted PI (geometric means ratio [GMR] 3.1, 90% confidence interval [CI] 2.57–3.74) [45]. Therefore, when maraviroc and etravirine are coadministered with a ritonavir-boosted PI, the PI dosing recommendations should be followed as CYP3A inhibition by the ritonavir-boosted PI is expected to overcome the CYP3A induction by etravirine [11, 44]. A population PK analysis of the DUET trials found no interaction between etravirine and enfuvirtide [24], and none is expected between etravirine and ibalizumab.
Fostemsavir, a prodrug of temsavir, is an investigational attachment inhibitor metabolized by esterase-mediated hydrolysis, CYP oxidation, and glucuronidation [46]. If approved, fostemsavir may be a useful agent to combine with etravirine, given expected use for highly treatment-experienced patients. When fostemsavir 600 mg twice daily was combined with etravirine 200 mg twice daily, the AUC of temsavir was decreased 50% (Table 4). However, when fostemsavir and etravirine were combined with darunavir/ritonavir 600/100 mg twice daily, the temsavir AUC increased 34% (GMR 1.34, 90% CI 1.17–1.53). The authors concluded the interactions were not clinically meaningful in either scenario, based on safety and efficacy from an ongoing phase IIb study [47].
3.1.2 Integrase Strand Transfer Inhibitors
The various metabolic pathways of integrase strand transfer inhibitors (INSTIs) influence the effect of etravirine coadministration [7]. Raltegravir and cabotegravir are both primarily metabolized by UGT1A1, while bictegravir and dolutegravir are metabolized by CYP3A4 and UGT1A1. Raltegravir, bictegravir, and dolutegravir do not induce or inhibit enzymes involved in etravirine metabolism. Elvitegravir is metabolized by CYP3A4 and is only available as a combined tablet with cobicistat, a CYP3A inhibitor, resulting in the potential for this combination to influence etravirine exposure. Bictegravir has not been evaluated with etravirine, but etravirine is expected to significantly decrease bictegravir exposure and coadministration is not recommended [7]. Data with other INSTIs and etravirine are summarized below.
No significant change in the raltegravir AUC or etravirine PK were found in a healthy volunteer study (Table 4) [48]. Based on these data, twice-daily raltegravir may be coadministered with etravirine with no dose adjustment. However, raltegravir 1200 mg once daily should be avoided in combination with etravirine because of the 34% decrease in raltegravir Cmin [7].
Dolutegravir (50 mg daily) combined with etravirine (200 mg twice daily) resulted in a 71% and 88% decrease in dolutegravir AUC and C24, respectively (Table 4) [49]. Dolutegravir (50 mg daily) was also evaluated with etravirine (200 mg twice daily) plus lopinavir/ritonavir 400/100 mg twice daily or darunavir/ritonavir 600/100 mg twice daily to assess the three-way interaction [49]. With lopinavir/ritonavir and etravirine, the dolutegravir AUC and C24 were 11% and 28% higher, respectively, compared with dolutegravir alone (geometric least square means [GLSM] ratio AUC: 1.11, 90% CI 1.02–1.20; C24: 1.28 (90% CI 1.13–1.45)]. With darunavir/ritonavir and etravirine, the dolutegravir AUC and C24 were 25% and 37% lower, respectively [GLSM ratio AUC: 0.75, 90% CI 0.69–0.81; C24: 0.63, 90% CI 0.52–0.76]. Based on these results, if dolutegravir is combined with etravirine, a ritonavir-boosted PI, either atazanavir, lopinavir, or darunavir, each boosted with ritonavir, must also be given. In this combination, dolutegravir 50 mg once daily may be used in patients without INSTI resistance; however, due to the potential for lower dolutegravir exposure, twice-daily dolutegravir may be considered by some providers for persons with INSTI resistance [7]. The investigational (as of this writing) INSTI cabotegravir (30 mg orally daily), was evaluated in combination with etravirine (200 mg twice daily), with no change observed in cabotegravir PK parameters (Table 4). Therefore, it is expected that no dose adjustment is necessary.
Etravirine is not recommended with elvitegravir/cobicistat, based on the interaction with darunavir/cobicistat described in Sect. 3.1.5 [7]. Elvitegravir/ritonavir was studied in combination with etravirine in healthy volunteers and resulted in no change in either elvitegravir or etravirine PK (Table 4) [44]. Because elvitegravir-only tablets were discontinued by the manufacturer, this combination is no longer available.
3.1.3 Nucleoside/Nucleotide Reverse Transcriptase Inhibitors
A crossover study of etravirine with tenofovir disoproxil fumarate in healthy volunteers found a 15% increase in tenofovir exposure (Table 4) [50]. The increase in tenofovir is hypothesized to be related to p-glycoprotein inhibition by etravirine [50]. A similar effect may be observed with tenofovir alafenamide, also due to p-glycoprotein inhibition, but this has not yet been studied. In the same study, a 19% decrease in etravirine exposure was observed (Table 4) [50], and a population PK model from the DUET trial found that tenofovir disoproxil fumarate was also associated with 26% lower etravirine AUC12 (p =0.0005) [24]. The product labeling reflects current opinion that these changes are not clinically significant. No significant DDIs are expected with other nucleoside/nucleotide reverse transcriptase inhibitors (NRTIs) [11, 44].
3.1.4 Non-Nucleoside Reverse Transcriptase Inhibitors
Due to the shared mechanism of action and prior data finding that dual-NNRTI-based regimens were not effective [7], etravirine is not recommended in combination with other NNRTIs. Both efavirenz and nevirapine significantly decrease the AUC of etravirine by 41–55% (Table 4) due to the induction of etravirine metabolism via CYP3A4, CYP2C9, and CYP2C19 [11, 44].
3.1.5 Protease Inhibitors
PIs are substrates for, and inducers or inhibitors of, multiple CYP enzymes [7]; thus, there are significant DDIs when combining etravirine with PIs. Etravirine exposure decreased (AUC 33–35%; Cmin 45–49%) when combined with darunavir/ritonavir or lopinavir/ritonavir, with no change in darunavir exposure and modestly lower lopinavir AUC (13%) and Cmin (20%) [Table 4]. Despite this, no dose adjustment is recommended with these PIs as the reduction in etravirine exposure was observed during the phase III clinical trials, which leads to the licensure of etravirine, at the standard dose, in combination with boosted PIs.
One study evaluated etravirine in combination with cobicistat-boosted PIs [51]. Comparisons were conducted in two cohorts: (1) patients receiving ART with darunavir/cobicistat (800/150 mg once daily) added etravirine 400 mg once daily to their background regimen for 14 days; or (2) patients receiving ART with etravirine (400 mg once daily) added darunavir/cobicistat 800/150 mg once daily to their background regimen for 7 days. No change in etravirine Cmax, Cmin, or AUC before and after the addition of darunavir/cobicistat was observed (Table 4). In contrast, the cobicistat AUC and C24 were 30% and 64% lower, respectively (least square means [LSM] ratio AUC: 0.70, 90% CI 0.56–0.87; Cmin: 0.34, 95% CI 0.23–0.50). This reduction in cobicistat exposure contributed to a 56% lower darunavir C24, but no change in the darunavir Cmax or AUC (Table 4). Therefore, when combining etravirine with darunavir, it is recommended to use ritonavir as the PK booster. Based on these data, etravirine is also not recommended in combination with cobicistat-boosted atazanavir.
No dose adjustment is recommended, but caution is advised, when etravirine is combined with fosamprenavir/ritonavir due to a 69% higher amprenavir AUC observed in patients adding etravirine to a fosamprenavir/ritonavir-containing ART, and atazanavir/ritonavir due to a lower atazanavir exposure (AUC 14%, Cmin 38%) and 30% higher etravirine AUC (Table 4) [11, 44]. Dose escalation of atazanavir/ritonavir to 400/100 mg once daily was compared with 300/100 mg once daily plus etravirine 200 mg twice daily. Atazanavir/ritonavir 400/100 mg resulted in atazanavir exposure similar to 300/100 mg in the absence of etravirine, and etravirine exposure was only modestly lower (16%) than historic data. Because no significant difference was observed in virologic outcomes or safety parameters between the two atazanavir/ritonavir doses, the authors concluded a dose increase of atazanavir/ritonavir to 400/100 mg was not necessary in combination with etravirine [52]. Etravirine should not be combined with PIs administered without a PK enhancer due to lower PI exposure [11, 44].
4 Pharmacogenomics
A two-step pharmacogenetics-based population PK study among HIV-1-infected patients was used to evaluate both genetic and non-genetic factors associated with etravirine metabolism. Etravirine mean CL/F, Vd, and mean duration of absorption time (D1) were determined using 289 etravirine plasma samples from 144 patients: CL/F 41 L/h (CV 51.1%); Vd 1325 L; D1 1.2 h. Coadministration of darunavir/ritonavir and tenofovir disoproxil fumarate were identified as non-genetic factors associated with an increase in etravirine CL/F, 40% (95% CI 13–69%) and 42% (95% CI 17–68%), respectively. Only one genetic factor, the single nucleotide polymorphism (SNP) rs4244285 (CYP2C19*2), was associated with a change in etravirine CL/F, resulting in a 23% (95% CI 8–38%) reduction in CL/F [35]. The effect of CYP3A5*3 polymorphism expression on darunavir plasma concentrations was evaluated with and without etravirine. Darunavir concentrations, in the presence of concomitant etravirine (and ritonavir) were significantly lower in two subgroups of patients expressing the CYP3A5*3 SNP (n =13) compared with patients without the SNP (n =16): darunavir/ritonavir 800/100 mg daily, 1385 ng/ml (95% CI 886–2165) versus 3141 ng/ml (95% CI 2042–4831); darunavir/ritonavir 600/100 mg twice daily, 1486 ng/ml (95% CI 725–3044) versus 3141 ng/ml (95% CI 2042–4831) [53]. A population PK modeling study using 4728 plasma etravirine concentration samples from 817 adult patients from four clinical trials found higher etravirine concentrations among CYP2C9 and CYP2C19 slow metabolizers [54].
5 Pharmacodynamics
5.1 Antiviral Activity
In vitro etravirine antiviral activity was observed against all HIV-1 group M viruses (EC50 < 5 nM; fold change in EC50 values [FC] < 4). Reduced antiviral activity of etravirine was observed in HIV-1 group O (EC50 = 13 nM; FC = 9.9) and HIV-2 viruses (EC50 = 3.5 µM). Etravirine exhibited activity against 97% of NNRTI-resistant strains (EC50 < 100 nM). EC50 values > 10 nM with FC > 10 were observed for etravirine among three HIV-1 viruses harboring resistance (L100I + K103 N, Y181I, F227C) [2].
5.2 Resistance
Unlike first-generation NNRTIs (efavirenz, nevirapine), the single mutation K103 N has no effect on etravirine antiviral activity. The development of etravirine resistance requires selection for multiple HIV drug resistance mutations likely secondary to its adaptability through molecular structural flexibility [2, 55]. In vitro drug resistance selection studies have identified that L100I, K101P, V179I/F, Y181C, G190E, M230L, and Y318F may affect etravirine activity [55, 56]; yet, the presence of single mutations at L100I, K101P, and Y181C have clinically reduced the susceptibility and efficacy of etravirine [18, 55, 56].
5.3 Children/Adolescents
Etravirine has been evaluated in children (1 to < 12 years of age) and adolescents (≥ 12 to < 18 years of age). A phase I/II study of etravirine in combination with an optimized background regimen that included a ritonavir-boosted PI was conducted in children split into two age-based cohorts (cohort 1: 2 to < 6 years of age; cohort 2: 1 to < 2 years of age). Twenty-five participants received weight-band etravirine dosing: 75 mg twice daily (8 to < 10 kg); 100 mg twice daily (10 to < 20 kg); and 125 mg twice daily (20 to < 25 kg) [39, 40]. Of those completing 24 weeks, virologic suppression (intent to treat [ITT]; HIV RNA < 400 copies/mL) was 94% (15/16) and 25% (1/4) in cohorts 1 and 2, respectively. One participant in cohort 1 and three in cohort 2 experienced virologic failure; the authors stated the majority of resistance mutations observed were similar to those in adults. Two participants in cohort 2 had AUC12 below the 10th percentile, potentially explaining the lower rate of virologic suppression in that cohort. Rash was the most common adverse event occurring in 17 participants (cohort 1, n =13; cohort 2, n =4) [39]. Overall, the safety of etravirine in this pediatric population was consistent with its use in adults [39, 57]. The poorer virologic response in children 1 to < 2 years of age (cohort 2) forms the basis for approval in children 2 years of age and older.
A phase I study among virologically suppressed (HIV RNA < 50 copies/mL) children and adolescents (6–17 years of age) on a lopinavir/ritonavir-based ART regimen evaluated etravirine PK and dosing, using dosing of 4 mg/kg twice daily or 5.2 mg/kg twice daily. All patients remained virologically suppressed (< 50 copies/mL) independent of etravirine dosing treatment arm [10]. The PIANO (Paediatric study of Intelence As an NNRTI Option) study, was a single-arm, open-label, phase II evaluation of etravirine added to failing background regimens in treatment-experienced children and adolescents. With the addition to etravirine, 57 of 101 (56%) participants achieved virologic suppression (HIV RNA < 50 copies/mL, ITT) at week 48 [6]. Newly emergent NNRTI resistance was detected in 18 of 30 (60%) participants who were not virologically suppressed, of which Y181C was the most commonly detected (n =8). Other emergent resistance mutations observed were V90I, L100I, and E138A, in three participants each [5, 6]. Lower weight, Asian race, and adolescence were identified as negative predictors of etravirine exposure. An exposure–response relationship was observed, with fewer participants achieving virologic suppression in the lower AUC12 quartile (lowest AUC12 quartile: ≤ 2704 ng·h/mL; virologic suppression: 41% vs. 67–76%) [34].
Etravirine is indicated for use in third-line therapy in treatment-experienced children (2–12 years of age) and adolescents (13 to < 18 years of age) weighing at least 10 kg. Dose recommendations are 100 mg twice daily (10 to < 20 kg), 125 mg twice daily (20 to < 25 kg), 150 mg twice daily (25 to < 30 kg), and 200 mg twice daily (≥ 30 kg) [18, 39, 58].
5.4 Adults
5.4.1 Antiretroviral Therapy (ART) Treatment-Experienced Persons
In the etravirine DUET-1 and DUET-2 trials, ART-experienced adults with documented virologic failure, PI resistance (three or more drug resistance mutations) and NNRTI resistance (one or more drug resistance mutation) were randomized 1:1 to receive either etravirine 200 mg twice daily or placebo in addition to their current ARV regimens consisting of ritonavir-boosted darunavir with or without enfuvirtide [59,60,61]. The proportion of participants maintaining virologic suppression (HIV RNA < 50 copies/mL) was significantly higher in the etravirine arm compared with placebo (time to loss of virologic response (TLOVR): 57% vs. 36%; p <0.0001) in the 96-week pooled analyses [62]. In subgroup analyses, the etravirine arm demonstrated an improved virologic response compared with placebo regardless of baseline characteristics [63]. Higher background regimen activity (two or more active agents) resulted in better virologic response [64]. No associations were found between etravirine PK and virologic response or safety [12].
The Monetra study evaluated once-daily etravirine in virologically suppressed, NNRTI-experienced patients receiving etravirine 200 mg twice daily. After switching to etravirine 400 mg once daily, 23 of 24 (95%; 95% CI 78.4–99.7) patients at week 24 and 19 of 24 (85%; 95% CI 65.6–95.8) patients at week 48 maintained virologic suppression [65]. In the Etraswitch study, virologically suppressed, treatment-experienced patients received boosted PI-based regimens were randomized to switch from the boosted PI to etravirine 400 mg once daily or remain on the same regimen. Virologic suppression between treatment arms was similar: 20 of 22 (90.9%) in the etravirine arm and 20 of 21 (95.2%) in the control arm (ITT analysis, p =0.58). No protocol-defined virologic failures occurred [66]. On not responding to ART, treatment-experienced patients with multidrug resistance (three or more PI mutations, three or more NRTI mutations, three or fewer darunavir-associated resistance mutations, and three or fewer NNRTI mutations) were switched to etravirine 200 mg twice daily in combination with raltegravir 400 mg twice daily and darunavir/ritonavir 600/100 mg twice daily as a salvage regimen (n =100). The combination demonstrated high rates of virologic suppression at 24 weeks (90%; 95% CI 85–96%) and 48 weeks (86%; 95% CI 80–93%) [67].
An NRTI-sparing regimen of darunavir/ritonavir plus once-daily etravirine was studied in 54 patients in INROADS, a single-arm study of ART-naïve and -experienced patients. Naïve patients had at least one transmitted resistance mutation to either efavirenz or nevirapine, and no resistance to either darunavir or etravirine. Treatment experienced patients did not have resistance to either darunavir or etravirine and had not experienced more than two virologic failures while taking a PI-based regimen. Virologic suppression at week 48 was achieved in 40 of 45 (89%; 95% CI 79.7–98.1) subjects in the ITT, non-virologic failure censored population, and in 37 of 54 (69%; 95% CI 56.1–80.9) subjects by FDA snapshot analysis in the ITT population. Seven patients (13%) experienced virologic failure, three non-responders and four rebounders. Two who did not respond to treatment developed emergent etravirine resistance-associated mutations, including L100I, E138G (in both patients), Y181C, and M230L [68]. The recent single-arm ETRAL study evaluated etravirine (200 mg twice daily) plus raltegravir (400 mg twice daily) among 165 participants virally suppressed on a boosted PI regimen and naïve to INSTIs or etravirine, and demonstrated 98.7% virologic suppression (ITT, 95% CI 95.0–99.7) at 96 weeks [69].
5.4.2 ART-Naïve Patients
In a single-arm study of ART-naïve participants (n =79), etravirine was administered as 400 mg once daily, with a NRTI backbone of tenofovir disoproxil fumarate/emtricitabine. At week 48, 61 of 79 participants (77%; 95% CI 66–86%) achieved virologic suppression. Eleven participants (14%) experienced virologic failure; genotype testing in three of five patients with HIV RNA > 500 copies/mL revealed all three developed emergent drug resistance. Two patients had single mutations; one with E138 K and one with Y181C. The remaining patient had numerous mutations, including V75I, E138 K, Y181C, M184I, K219E, and M230L. Adverse events (higher than grade 2) occurred in 18 patients (22.8%), with rash being the most common in five patients (6.3%) [70].
The Study of Etravirine Neuropsychiatric Symptoms versus Efavirenz (SENSE) trial compared once-daily etravirine (n =79) with efavirenz (n =78), both in combination with two NRTIs, among treatment-naïve participants. Etravirine demonstrated non-inferiority to efavirenz at week 48 in both the ITT and per-protocol analyses (76% vs. 74% and 92% vs. 89%, respectively; p <0.05). Eleven patients (etravirine arm, four; efavirenz arm, seven) experienced virologic failure by the TLOVR algorithm. No NNRTI- or NNRTI-emergent drug resistance was observed in the four patients (5.1%) with virologic failure in the etravirine arm. Three of seven patients in the efavirenz arm developed emergent drug resistance—one with V106I and M184I, one with K103 N, and one patient with K103 N, P225H, and M184 V [71].
In these two small studies investigating etravirine use in treatment-naïve patients, etravirine was efficacious, but not to the same degree as currently recommended first-line therapies [72,73,74,75,76]. The development of etravirine-specific drug resistance mutations was observed in a small number of participants; the safety profile was acceptable, with few neuropsychiatric adverse events. Due to the small populations in these studies, more data are needed to support etravirine use as first-line therapy in treatment-naïve patients.
5.4.3 Special Populations
In phase IV studies, etravirine (200 mg twice daily) was investigated among HIV-infected pregnant women in the second or third trimester. Lower etravirine CL/F (52% reduction) and higher Cmax and C12 (39 and 36% increases, respectively) were observed but were considered not significant. Ten of 13 (77%) and 9/12 (75%) participants had HIV RNA < 50 copies/mL in the third trimester and at delivery, respectively. Data for 13 study infants available showed all were HIV negative. However, three infants (23.1%) were born with congenital abnormalities [38]. Etravirine 200 mg twice daily administered with an optimized background regimen was evaluated in 15 women in the second trimester of pregnancy. Except for one participant, all women had HIV RNA < 400 copies/mL throughout the study period. Of the participants receiving continued treatment throughout the study, 12/13 (92.3%) and 10/11 (90.9%) had HIV RNA < 50 copies/mL in the second and third trimesters, respectively. The authors concluded etravirine demonstrated acceptable safety [77]. Etravirine penetrates well into breast milk, with higher concentrations observed in breast milk than in plasma.
5.5 Safety
Etravirine has been associated with minimal adverse events and demonstrated a favorable safety profile throughout the clinical trials. Rash was most common compared with placebo (20.5% vs. 11.8%; p < 0.0001) in the pooled 96-week analysis of DUET-1 and DUET-2. Rash development was mild to moderate in nature and resolved within 1–2 weeks with continued treatment. Discontinuation due to rash was low in both the etravirine (2.2%) and placebo (0%) arms. Women were more likely than men to develop a rash in the etravirine arm (31.7% vs. 19.3%; p =0.029) but not in the placebo arm (11.6% vs. 11.8%). The overall incidence of hepatic adverse events was similar between treatment arms (etravirine 8.7% vs. placebo 7.1%; difference 1.6%; 95% CI − 1.5 to 4.6%). There was a trend for higher rates of grade 3 or 4 elevated triglycerides (TG) and total cholesterol (TC) but not low-density lipoprotein (LDL) with etravirine versus placebo (TG: 11.3% vs. 7.0%, p = 0.0117; TC: 9.2% vs. 6.0%, p = 0.0379; LDL: 9.4% vs. 8.1%, p = 0.4704) [57]. Changes in lipids were less commonly observed in etravirine-treated persons compared with efavirenz in the SENSE trial in a univariate analysis of change in lipid markers from baseline to week 48 (TC: efavirenz 4.2–5.2 mmol/L vs. etravirine 4.3–4.7 mmol/L, p < 0.001; LDL: efavirenz 2.4–3.0 mmol/L vs. etravirine 2.6–2.8 mmol/L, p =0.001; high-density lipoprotein: efavirenz 1.0–1.3 mmol/L vs. etravirine 1.1–1.2 mmol/L, p = 0.028) [78].
The presence of neuropsychiatric adverse events was thoroughly evaluated in the DUET trials and between etravirine and efavirenz. No significant difference was observed in the frequency of neuropsychiatric adverse events between etravirine and placebo (difference −2.2%; 95% CI − 7.6 to 3.2%). However, a previous history of psychiatric disorders was associated with the incidence of neuropsychiatric adverse events (etravirine: p < 0.0001; placebo: p = 0.0728). In further analyses of neuropsychiatric adverse events, the frequency per 100 patient-years was lower in the etravirine arm compared with placebo (12.6 vs. 16.8; relative risk 0.75; 95% CI 0.54–0.96) [57]. Patients treated with etravirine experienced lower rates of neuropsychiatric adverse events in the SENSE trial compared with efavirenz. The incidence of grades 1–4 neuropsychiatric adverse events in both treatment arms was highest at week 2 (efavirenz 39.7% vs. etravirine 13.9%; p < 0.001) and remained higher in the efavirenz arm at week 48 (21.5% vs. 6.3%; p = 0.011) [71].
6 Interpretations and Conclusions
Etravirine is a second-generation NNRTI, active against wild-type and NNRTI-resistant HIV, offering an alternative ARV for HIV-infected individuals with first-generation NNRTI resistance. The DHHS HIV treatment guidelines recommend etravirine only as twice-daily therapy, administered in combination with other ARVs in treatment-experienced children, adolescents, and adult persons. The clinical use of etravirine is limited by its poor palatability and twice-daily dosing. Once-daily etravirine for treatment-experienced patients is considered by some providers, given similar PK exposure and effectiveness (see Sect. 5.4.2) [65, 66], to reduce pill burden. This may be particularly useful in settings where therapeutic drug monitoring (TDM) is feasible, and appropriate exposure can be documented. Calcagno et al. described a putative etravirine Cmin threshold of 300 ng/mL, as well as a weighted genotypic inhibitory quotient (276 ng/mL), which may provide useful guidance for clinicians with access to TDM and seeking to utilize once-daily dosing [79]. However, the benefits of once-daily dosing in this population should be fully considered and thought to outweigh the potential risks of virologic failure and further development of HIV drug resistance. Larger trials are needed to validate the use of once-daily dosing for treatment-naïve persons, considering the currently recommended first-line regimens have higher efficacy rates than the 74–77% found with once-daily etravirine among treatment-naïve patients [70,71,72,73,74,75,76].
Etravirine has demonstrated an acceptable safety profile. Etravirine use in pregnant women shows exposure is increased 1.2- to 1.6-fold in pregnant women; however, no dose adjustment during pregnancy is recommended. While etravirine was well tolerated during the studies in pregnant women, the data are not sufficient to establish safety in the mother and infant or to assess teratogenicity. No dosage adjustments are recommended for etravirine use in patients with renal impairment or mild to moderate hepatic impairment. Data for etravirine in severe hepatic impairment are lacking and its use is not recommended. Special attention should be given with regard to bi-directional DDIs when using etravirine, as etravirine may be both a victim and perpetrator of drug interactions because it is a substrate for CYP3A4, CYP2C9, and CYP2C19, an inducer of CYP3A, and an inhibitor of CYP2C9 and CYP2C19.
References
Vingerhoets J, Tambuyzer L, Azijn H, Hoogstoel A, Nijs S, Peeters M, et al. Resistance profile of etravirine: combined analysis of baseline genotypic and phenotypic data from the randomized, controlled Phase III clinical studies. AIDS. 2010;24(4):503–14.
Andries K, Azijn H, Thielemans T, Ludovici D, Kukla M, Heeres J, et al. TMC125, a novel next-generation nonnucleoside reverse transcriptase inhibitor active against nonnucleoside reverse transcriptase inhibitor-resistant human immunodeficiency virus type 1. Antimicrob Agents Chemother. 2004;48(12):4680–6.
Wensing AM, Calvez V, Gunthard HF, Johnson VA, Paredes R, Pillay D, et al. 2017 update of the drug resistance mutations in HIV-1. Top Antivir Med. 2017;24(4):132–3.
Scherrer AU, Hasse B, von Wyl V, Yerly S, Boni J, Burgisser P, et al. Prevalence of etravirine mutations and impact on response to treatment in routine clinical care: the Swiss HIV Cohort Study (SHCS). HIV Med. 2009;10(10):647–56.
Tambuyzer L, Thys K, Hoogstoel A, Nijs S, Tomaka F, Opsomer M, et al. Assessment of etravirine resistance in HIV-1-infected paediatric patients using population and deep sequencing: final results of the PIANO study. Antivir Ther. 2016;21(4):317–27.
Tudor-Williams G, Cahn P, Chokephaibulkit K, Fourie J, Karatzios C, Dincq S, et al. Etravirine in treatment-experienced, HIV-1-infected children and adolescents: 48-week safety, efficacy and resistance analysis of the phase II PIANO study. HIV Med. 2014;15(9):513–24.
Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents with HIV. Department of Health and Human Services. http://aidsinfo.nih.gov/contentfiles/lvguidelines/AdultandAdolescentGL.pdf. Accessed 6 Jun 2019.
European AIDS Clinical Society Guidelines version 9.1, October 2018.
Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. 2nd Edition. Geneva: World Health Organization. 2016. http://www.who.int/hiv/pub/guidelines/hiv-testing-services/en/. Accessed 14 Jun 2019.
Konigs C, Feiterna-Sperling C, Esposito S, Viscoli C, Rosso R, Kakuda TN, et al. Pharmacokinetics and short-term safety and tolerability of etravirine in treatment-experienced HIV-1-infected children and adolescents. AIDS. 2012;26(4):447–55.
Scholler-Gyure M, Kakuda TN, Raoof A, De Smedt G, Hoetelmans RM. Clinical pharmacokinetics and pharmacodynamics of etravirine. Clin Pharmacokinet. 2009;48(9):561–74.
Kakuda TN, Wade JR, Snoeck E, Vis P, Scholler-Gyure M, Peeters MP, et al. Pharmacokinetics and pharmacodynamics of the non-nucleoside reverse-transcriptase inhibitor etravirine in treatment-experienced HIV-1-infected patients. Clin Pharmacol Ther. 2010;88(5):695–703.
Scholler M, Hoetelmans R, Beets G, et al. Substantial improvement of oral bioavailability of TMC125 using new tablet formulations in healthy volunteers [abstract no. 82]. In: 6th International Workshop of Clinical Pharmacology of HIV Therapy; 28–30 Apr 2005; Quebec.
Scholler-Gyure M, Kakuda TN, De Smedt G, et al. Pharmacokinetics of TMC125 in once- and twice-daily regimens in HIV-1 negative volunteers [abstract no. A-1427]. In: 47th Interscience Conference Agents and Chemotherapy; 17–20 Sep 2007; Chicago.
Kakuda TN, Scholler-Gyure M, Workman C, Arasteh K, Pozniak AL, De Smedt G, et al. Single- and multiple-dose pharmacokinetics of etravirine administered as two different formulations in HIV-1-infected patients. Antivir Ther. 2008;13(5):655–61.
Annaert P. Determination of the in vitro transport characteristics of TMC125, evaluation of the possible role of p-glycoprotein in TMC125 transport and assessment of possible inhibition of p-glycoprotein activity by TMC125: a study in Caco-2 monolayers. Nonclinical pharmacokinetics report, study no. TMC125-NC183 (FK4784). Beerse: Johnson & Johnson Pharmaceutical Research & Development; 2004 (data on file).
Scholler-Gyure M, Boffito M, Pozniak AL, Leemans R, Kakuda TN, Woodfall B, et al. Effects of different meal compositions and fasted state on the oral bioavailability of etravirine. Pharmacotherapy. 2008;28(10):1215–22.
Etravirine [prescribing information]. Titusville. NJ: Janssen Therapeutics; 2013.
Scholler-Gyure M, Kakuda TN, De Smedt G, Vanaken H, Bouche MP, Peeters M, et al. A pharmacokinetic study of etravirine (TMC125) co-administered with ranitidine and omeprazole in HIV-negative volunteers. Br J Clin Pharmacol. 2008;66(4):508–16.
Kakuda TN, Berckmans C, De Smedt G, Leemans R, Leopold L, Peeters M, et al. Single-dose pharmacokinetics of pediatric and adult formulations of etravirine and swallowability of the 200-mg tablet: results from three Phase 1 studies. Int J Clin Pharmacol Ther. 2013;51(9):725–37.
Sandkovsky U, Swindells S, Moore R, Acosta EP, Fletcher CV. Acceptable plasma concentrations of raltegravir and etravirine when administered by gastrostomy tube in a patient with advanced multidrug-resistant human immunodeficiency virus infection. Pharmacotherapy. 2012;32(2):142–7.
Mamidi RNVS. The plasma protein binding and blood distribution of TMC125 in animals and man. Nonclinical pharmacokinetics report, study no. TMC125-NC143 (FK5135). Beerse: Johnson & Johnson Pharmaceutical Research & Development; 2004 (data on file).
John J, John M, Wu L, Hsiao C, Abobo CV, Liang D. Effects of etravirine on the pharmacokinetics and pharmacodynamics of warfarin in rats. Br J Pharmacol. 2013;168(8):1851–8.
Kakuda TN, Scholler-Gyure M, Peeters M, et al. Pharmacokinetics of etravirine are not affected by sex, age, race, use of enfuvirtide or treatment duration in HIV-1 infected patients [abstract no. P34]. In: 9th International Workshop of Clinical Pharmacology of HIV Therapy; 7–9 Apr 2008; New Orleans.
Nguyen A, Rossi S, Croteau D, Best BM, Clifford D, Collier AC, et al. Etravirine in CSF is highly protein bound. J Antimicrob Chemother. 2013;68(5):1161–8.
Tiraboschi JM, Niubo J, Vila A, Perez-Pujol S, Podzamczer D. Etravirine concentrations in CSF in HIV-infected patients. J Antimicrob Chemother. 2012;67(6):1446–8.
Patterson K, Jennings S, Falcon R, Mrus J, Kashuba A. Darunavir, ritonavir, and etravirine pharmacokinetics in the cervicovaginal fluid and blood plasma of HIV-infected women. Antimicrob Agents Chemother. 2011;55(3):1120–2.
Clavel C, Peytavin G, Tubiana R, Soulié C, Courbon E, Crenn-Hebert C, et al. Etravirine concentrations in the cervicovaginal compartment in HIV-1-infected women receiving etravirine-containing antiretroviral therapy: DIVA 02 study. Antimicrob Agents Chemother. 2012;56(7):4018–20.
Brown KC, Patterson KB, Jennings SH, Malone SA, Shaheen NJ, Asher Prince HM, et al. Single- and multiple-dose pharmacokinetics of darunavir plus ritonavir and etravirine in semen and rectal tissue of HIV-negative men. J Acquir Immune Defic Syndr. 2012;61(2):138–44.
Raoof A, Mannens G, Mamidi R, et al. In vivo metabolism and mass balance of the anti-HIV compound TMC125 in laboratory animals and healthy volunteers [abstract no. M1342]. In: American Association of Pharmaceutical Scientists Annual Meeting and Exposition; 28 Oct–2 Nov 2006; San Antonio.
Scholler-Gyure M, Raoof A, Mannens G, et al. Mass-balance of 14C-labelled TMC125 in healthy volunteers [abstract no. 78]. In: 8th International Workshop of Clinical Pharmacology of HIV Therapy; 16–18 Apr 2007; Budapest.
Smeulders L. Overview of the antiviral activities of TMC125 metabolites on a panel of NNRTI viruses. Tibotec research report no. CB-SR-2004-00052-AVE-NNRTI. Mechelen: Tibotec; Feb 2005 (data on file).
Scholler-Gyure M, Kakuda TN, De Smedt G, Woodfall B, Berckmans C, Peeters M, et al. Effects of hepatic impairment on the steady-state pharmacokinetics of etravirine 200 mg BID: an open-label, multiple-dose, controlled Phase I study in adults. Clin Ther. 2010;32(2):328–37.
Kakuda TN, Brochot A, Green B, Nijs S, Vis P, Opsomer M, et al. Pharmacokinetics and pharmacokinetic/pharmacodynamic relationships of etravirine in HIV-1-infected, treatment-experienced children and adolescents in PIANO. J Clin Pharmacol. 2016;56(11):1395–405.
Lubomirov R, Arab-Alameddine M, Rotger M, Fayet-Mello A, Martinez R, Guidi M, et al. Pharmacogenetics-based population pharmacokinetic analysis of etravirine in HIV-1 infected individuals. Pharmacogenet Genomics. 2013;23(1):9–18.
Ter Heine R, Mulder JW, van Gorp EC, Wagenaar JF, Beijnen JH, Huitema AD. Intracellular and plasma steady-state pharmacokinetics of raltegravir, darunavir, etravirine and ritonavir in heavily pre-treated HIV-infected patients. Br J Clin Pharmacol. 2010;69(5):475–83.
Scholler-Gyure M, Kakuda TN, De Smedt G, et al. Pharmacokinetics of TMC125 in HIV-negative volunteers with mild or moderate hepatic impairment [abstract no. A-1428]. In: 47th Interscience Conferrence on Antimicrobial Agents and Chemotherapy; 17–20 Sep 2007; Chicago.
Mulligan N, Schalkwijk S, Best BM, Colbers A, Wang J, Capparelli EV, et al. Etravirine pharmacokinetics in HIV-infected pregnant women. Front Pharmacol. 2016;7:239.
US FDA. Clinical and cross-discipline team leader review/addendum. NDA#22187/Supplement 024. 2018. https://www.fda.gov/media/115201/download. Accessed 27 Jun 2019.
MacBrayne CE, Rutstein R, Yogev R, et al. Etravirine pharmacokinetics in treatment-experienced children ages 1–< 6 years [abstract no. 465]. In: The Conference on Retroviruses and Opportunistic Infections; 4–7 Mar 2018; Boston.
Kakuda TN, Scholler-Gyure M, Hoetelmans RM. Pharmacokinetic interactions between etravirine and non-antiretroviral drugs. Clin Pharmacokinet. 2011;50(1):25–39.
Zembruski NC, Haefeli WE, Weiss J. Interaction potential of etravirine with drug transporters assessed in vitro. Antimicrob Agents Chemother. 2011;55(3):1282–4.
Kakuda TN, Van Solingen-Ristea RM, Onkelinx J, Stevens T, Aharchi F, De Smedt G, et al. The effect of single- and multiple-dose etravirine on a drug cocktail of representative cytochrome P450 probes and digoxin in healthy subjects. J Clin Pharmacol. 2014;54(4):422–31.
Kakuda TN, Scholler-Gyure M, Hoetelmans RM. Clinical perspective on antiretroviral drug-drug interactions with the non-nucleoside reverse transcriptase inhibitor etravirine. Antivir Ther. 2010;15(6):817–29.
Kakuda TN, Abel S, Davis J, Hamlin J, Scholler-Gyure M, Mack R, et al. Pharmacokinetic interactions of maraviroc with darunavir-ritonavir, etravirine, and etravirine-darunavir-ritonavir in healthy volunteers: results of two drug interaction trials. Antimicrob Agents Chemother. 2011;55(5):2290–6.
Fostemsavir Drug Information. AIDSinfo Health Professional. https://aidsinfo.nih.gov/drugs/508/fostemsavir/0/professional. Accessed 3 Sep 2019.
Savant Landry I, Tao X, Anderson J, Hesney M, Stonier M, Lubin S, Wang J, Hanna GJ, Boulton DW. HIV-1 Attachment Inhibitor Prodrug BMS-663068: Interactions with DRV/r and/or ETR [abstract no. 523]. In: The Conference on Retroviruses and Opportunistic Infections; 23–26 Feb 2015; Seattle.
Anderson MS, Kakuda TN, Hanley W, Miller J, Kost JT, Stoltz R, et al. Minimal pharmacokinetic interaction between the human immunodeficiency virus nonnucleoside reverse transcriptase inhibitor etravirine and the integrase inhibitor raltegravir in healthy subjects. Antimicrob Agents Chemother. 2008;52(12):4228–32.
Song I, Borland J, Min S, Lou Y, Chen S, Patel P, et al. Effects of etravirine alone and with ritonavir-boosted protease inhibitors on the pharmacokinetics of dolutegravir. Antimicrob Agents Chemother. 2011;55(7):3517–21.
Kakuda TN, Scholler-Gyure M, De Smedt G, Beets G, Aharchi F, Peeters MP, et al. Assessment of the steady-state pharmacokinetic interaction between etravirine administered as two different formulations and tenofovir disoproxil fumarate in healthy volunteers. HIV Med. 2009;10(3):173–81.
Molto J, Curran A, Miranda C, Challenger E, Santos JR, Ribera E, et al. Pharmacokinetics of darunavir/cobicistat and etravirine alone and co-administered in HIV-infected patients. J Antimicrob Chemother. 2018;73(3):732–7.
Orrell C, Felizarta F, Nell A, Kakuda TN, Lavreys L, Nijs S, et al. Pharmacokinetics of etravirine combined with atazanavir/ritonavir and a nucleoside reverse transcriptase inhibitor in antiretroviral treatment-experienced, HIV-1-infected patients. AIDS Res Treat. 2015;2015:938628.
Belkhir L, Elens L, Zech F, Panin N, Vincent A, Yombi JC, et al. Interaction between darunavir and etravirine is partly mediated by CYP3A5 polymorphism. PLoS One. 2016;11(10):e0165631.
Green B, Crauwels H, Kakuda TN, Vanveggel S, Brochot A. Evaluation of concomitant antiretrovirals and CYP2C9/CYP2C19 polymorphisms on the pharmacokinetics of etravirine. Clin Pharmacokinet. 2017;56(5):525–36.
Vingerhoets J, Azijn H, Fransen E, De Baere I, Smeulders L, Jochmans D, et al. TMC125 displays a high genetic barrier to the development of resistance: evidence from in vitro selection experiments. J Virol. 2005;79(20):12773–82.
Haddad M, Stawiski E, Benhamida J, Coakley E. Improved genotypic algorithm for predicting etravirine susceptibility: comprehensive list of mutations identified through correlation with matched phenotype. In: Poster presented at: 17th Conference on Retroviruses and Opportunistic Infections (CROI); 16–19 Feb 2010; San Francisco.
Girard PM, Campbell TB, Grinsztejn B, Hartikainen J, Rachline A, Nijs S, et al. Pooled week 96 results of the phase III DUET-1 and DUET-2 trials of etravirine: further analysis of adverse events and laboratory abnormalities of special interest. HIV Med. 2012;13(7):427–35.
Panel on Antiretroviral Guidelines for Pediatrics. Guidelines for the Use of Antiretroviral Agents in Pediatric HIV Infection. Department of Health and Human Services. https://aidsinfo.nih.gov/guidelines/html/2/pediatric-arv/0. Accessed 6 Jun 2019.
Katlama C, Haubrich R, Lalezari J, Lazzarin A, Madruga JV, Molina JM, et al. Efficacy and safety of etravirine in treatment-experienced, HIV-1 patients: pooled 48 week analysis of two randomized, controlled trials. AIDS. 2009;23(17):2289–300.
Lazzarin A, Campbell T, Clotet B, Johnson M, Katlama C, Moll A, et al. Efficacy and safety of TMC125 (etravirine) in treatment-experienced HIV-1-infected patients in DUET-2: 24-week results from a randomised, double-blind, placebo-controlled trial. Lancet. 2007;370(9581):39–48.
Madruga JV, Cahn P, Grinsztejn B, Haubrich R, Lalezari J, Mills A, et al. Efficacy and safety of TMC125 (etravirine) in treatment-experienced HIV-1-infected patients in DUET-1: 24-week results from a randomised, double-blind, placebo-controlled trial. Lancet. 2007;370(9581):29–38.
Katlama C, Clotet B, Mills A, Trottier B, Molina JM, Grinsztejn B, et al. Efficacy and safety of etravirine at week 96 in treatment-experienced HIV type-1-infected patients in the DUET-1 and DUET-2 trials. Antivir Ther. 2010;15(7):1045–52.
Clumeck N, Cahn P, Molina JM, Mills A, Nijs S, Vingerhoets J, et al. Virological response with fully active etravirine: pooled results from the DUET-1 and DUET-2 trials. Int J STD AIDS. 2010;21(11):738–40.
Trottier B, Di Perri G, Madruga JV, Peeters M, Vingerhoets J, Picchio G, et al. Impact of the background regimen on virologic response to etravirine: pooled 48-week analysis of DUET-1 and -2. HIV Clin Trials. 2010;11(4):175–85.
Schneider L, Ktorza N, Fourati S, Assoumou L, Courbon E, Caby F, et al. Switch from etravirine twice daily to once daily in non-nucleoside reverse transcriptase inhibitor (NNRTI)-resistant HIV-infected patients with suppressed viremia: the Monetra study. HIV Clin Trials. 2012;13(5):284–8.
Echeverria P, Bonjoch A, Puig J, Molto J, Paredes R, Sirera G, et al. Randomised study to assess the efficacy and safety of once-daily etravirine-based regimen as a switching strategy in HIV-infected patients receiving a protease inhibitor-containing regimen. Etraswitch study. PLoS One. 2014;9(2):e84676.
Yazdanpanah Y, Fagard C, Descamps D, Taburet AM, Colin C, Roquebert B, et al. High rate of virologic suppression with raltegravir plus etravirine and darunavir/ritonavir among treatment-experienced patients infected with multidrug-resistant HIV: results of the ANRS 139 TRIO trial. Clin Infect Dis. 2009;49(9):1441–9.
Ruane PJ, Brinson C, Ramgopal M, Ryan R, Coate B, Cho M, et al. The Intelence aNd pRezista Once A Day Study (INROADS): a multicentre, single-arm, open-label study of etravirine and darunavir/ritonavir as dual therapy in HIV-1-infected early treatment-experienced subjects. HIV Med. 2015;16(5):288–96.
Katlama C, Assoumou L, Valantin MA, Soulie C, Martinez E, Beniguel L, et al. Dual therapy combining raltegravir with etravirine maintains a high level of viral suppression over 96 weeks in long-term experienced HIV-infected individuals over 45 years on a PI-based regimen: results from the phase II ANRS 163 ETRAL study. J Antimicrob Chemother. 2019;74(9):2742–51.
Floris-Moore MA, Mollan K, Wilkin AM, Johnson MA, Kashuba AD, Wohl DA, et al. Antiretroviral activity and safety of once-daily etravirine in treatment-naive HIV-infected adults: 48-week results. Antivir Ther. 2016;21(1):55–64.
Gazzard B, Duvivier C, Zagler C, Castagna A, Hill A, van Delft Y, et al. Phase 2 double-blind, randomized trial of etravirine versus efavirenz in treatment-naive patients: 48-week results. AIDS. 2011;25(18):2249–58.
Clotet B, Feinberg J, van Lunzen J, Khuong-Josses MA, Antinori A, Dumitru I, et al. Once-daily dolutegravir versus darunavir plus ritonavir in antiretroviral-naive adults with HIV-1 infection (FLAMINGO): 48 week results from the randomised open-label phase 3b study. Lancet. 2014;383(9936):2222–31.
Gallant J, Lazzarin A, Mills A, Orkin C, Podzamczer D, Tebas P, et al. Bictegravir, emtricitabine, and tenofovir alafenamide versus dolutegravir, abacavir, and lamivudine for initial treatment of HIV-1 infection (GS-US-380-1489): a double-blind, multicentre, phase 3, randomised controlled non-inferiority trial. Lancet. 2017;390(10107):2063–72.
Lennox JL, DeJesus E, Lazzarin A, Pollard RB, Madruga JV, Berger DS, et al. Safety and efficacy of raltegravir-based versus efavirenz-based combination therapy in treatment-naive patients with HIV-1 infection: a multicentre, double-blind randomised controlled trial. Lancet. 2009;374(9692):796–806.
Orrell C, Hagins DP, Belonosova E, Porteiro N, Walmsley S, Falco V, et al. Fixed-dose combination dolutegravir, abacavir, and lamivudine versus ritonavir-boosted atazanavir plus tenofovir disoproxil fumarate and emtricitabine in previously untreated women with HIV-1 infection (ARIA): week 48 results from a randomised, open-label, non-inferiority, phase 3b study. Lancet HIV. 2017;4(12):e536–46.
Walmsley SL, Antela A, Clumeck N, Duiculescu D, Eberhard A, Gutierrez F, et al. Dolutegravir plus abacavir-lamivudine for the treatment of HIV-1 infection. N Engl J Med. 2013;369(19):1807–18.
Ramgopal M, Osiyemi O, Zorrilla C, Crauwels HM, Ryan R, Brown K, et al. Pharmacokinetics of total and unbound etravirine in HIV-1-infected pregnant women. J Acquir Immune Defic Syndr. 2016;73(3):268–74.
Fatkenheuer G, Duvivier C, Rieger A, Durant J, Rey D, Schmidt W, et al. Lipid profiles for etravirine versus efavirenz in treatment-naive patients in the randomized, double-blind SENSE trial. J Antimicrob Chemother. 2012;67(3):685–90.
Calcagno A, Marinaro L, Nozza S, Aldieri C, Carbone A, Ghisetti V, et al. Etravirine plasma exposure is associated with virological efficacy in treatment-experienced HIV-positive patients. Antiviral Res. 2014;108:44–7.
Kakuda TN, DeMasi R, van Delft Y, Mohammed P. Pharmacokinetic interaction between etravirine or darunavir/ritonavir and artemether/lumefantrine in healthy volunteers: a two-panel, two-way, two-period, randomized trial. HIV Med. 2013;14(7):421–9.
Ford SL, Gould E, Chen S, Lou Y, Dumont E, Spreen W, et al. Effects of etravirine on the pharmacokinetics of the integrase inhibitor S/GSK1265744. Antimicrob Agents Chemother. 2013;57(1):277–80.
Gutierrez-Valencia A, Martin-Pena R, Torres-Cornejo A, Ruiz-Valderas R, Castillo-Ferrando JR, Lopez-Cortes LF. Intracellular and plasma pharmacokinetics of 400 mg of etravirine once daily versus 200 mg of etravirine twice daily in HIV-infected patients. J Antimicrob Chemother. 2012;67(3):681–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The authors acknowledge support from the following grants from the National Institutes of Health: 1K23AI134307 (to Anthony T. Podany), 1R01HD085887-01A1 (to Kimberly K. Scarsi), and RO1 AI124965-04 and UM1AI06701 (to Courtney V. Fletcher).
Conflict of interest
Joshua P. Havens reports receiving grants from Gilead Sciences that are paid directly to the University of Nebraska Medical Center. Anthony T. Podany, Kimberly K. Scarsi and Courtney V. Fletcher report no conflicts of interest that are directly relevant to the content of this review.
Rights and permissions
About this article
Cite this article
Havens, J.P., Podany, A.T., Scarsi, K.K. et al. Clinical Pharmacokinetics and Pharmacodynamics of Etravirine: An Updated Review. Clin Pharmacokinet 59, 137–154 (2020). https://doi.org/10.1007/s40262-019-00830-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-019-00830-9