Abstract
Dasabuvir is a nonstructural (NS) 5B non-nucleoside inhibitor of the hepatitis C virus (HCV) used in combination with ombitasvir/paritaprevir/ritonavir for the treatment of chronic HCV infection. It is primarily metabolized by cytochrome P450 (CYP) 2C8, with a minor contribution from CYP3A. Biotransformation of dasabuvir forms the M1 metabolite, which retains antiviral activity. Dasabuvir exhibits linear pharmacokinetics with a terminal half-life of approximately 5–8 h, allowing for twice-daily dosing. The M1 metabolite of dasabuvir is the major metabolite in plasma and has a half-life similar to that of dasabuvir. Dasabuvir exposures in Asian subjects are comparable with Caucasian subjects. The pharmacokinetic characteristics of dasabuvir are similar between healthy subjects and HCV-infected patients, and are not appreciably altered by mild, moderate, or severe renal impairment or dialysis. Dasabuvir pharmacokinetic parameters were not significantly altered in subjects with mild or moderate hepatic impairment; however, exposures were significantly increased in subjects with severe hepatic impairment. Dasabuvir should be administered with food to maximize absorption. Coadministration of dasabuvir with a strong CYP2C8 inhibitor increased dasabuvir exposures by greater than tenfold, whereas coadministration with strong CYP3A inhibitors increased dasabuvir exposures by less than 50%. Furthermore, coadministration of dasabuvir with a CYP3A inducer decreased dasabuvir exposures by 55–70%. Coadministration of dasabuvir with strong CYP2C8 inhibitors or strong CYP3A/CYP2C8 inducers is contraindicated. Results from several drug interaction studies demonstrated that dasabuvir in combination with ombitasvir/paritaprevir/ritonavir can be coadministered with most comedications that are commonly prescribed in HCV-infected patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Dasabuvir is a nonstructural 5B non-nucleoside inhibitor primarily metabolized by cytochrome P450 (CYP) 2C8, with a minor contribution from CYP3A, and is a substrate of P-glycoprotein and breast cancer resistance protein (BCRP), as well as an inhibitor of BCRP and uridine diphosphate glucuronosyltransferase (UGT) 1A1. |
Dasabuvir pharmacokinetics are similar between healthy subjects and hepatitis C virus-infected patients. |
Dasabuvir pharmacokinetics are not appreciably altered by renal impairment or dialysis. |
Dasabuvir pharmacokinetics are minimally affected by mild or moderate hepatic impairment. Exposures were significantly increased in subjects with severe hepatic impairment. |
Except for strong CYP2C8 inhibitors or CYP3A/2C8 inducers, the metabolism of dasabuvir is not significantly compromised by concomitant medications. |
Coadministration with dasabuvir may increase plasma concentrations of drugs that are substrates of UGT1A1 and BCRP. |
1 Introduction
The direct-acting antiviral (DAA) dasabuvir (formerly ABT-333) is a non-nucleoside inhibitor of the hepatitis C virus (HCV) RNA-dependent RNA polymerase encoded by the nonstructural (NS) 5B gene (Fig. 1). NS5B plays a critical role in the HCV replication cycle through its ability to initiate RNA synthesis without using an RNA primer. Dasabuvir inhibits HCV genotype (GT) 1a and 1b replicons with 50% effective concentration values of 7.7 and 1.8 nM, respectively, with a 13-fold decrease in inhibitory activity in the presence of 40% human plasma [1].
The dasabuvir 250 mg tablet taken twice daily is approved in the US, the EU, and other regions in combination with ombitasvir/paritaprevir/ritonavir 25/150/100 once daily ± ribavirin (RBV) for the treatment of HCV GT1a and 1b with and without compensated cirrhosis [2, 3]. Ombitasvir is an NS5A inhibitor, while paritaprevir (identified by Enanta Pharmaceuticals and AbbVie Inc.) is an NS3/4A protease inhibitor, which is combined with ritonavir, a pharmacokinetic enhancer that is not active against HCV. The combination of dasabuvir with ombitasvir/paritaprevir/ritonavir is referred to as the 3-direct-acting antiviral (3D) regimen. The 3D regimen has demonstrated high sustained virologic responses (SVR) when administered to subjects infected with chronic HCV GT1 infection. After 12 weeks of therapy with the 3D regimen plus ribavirin, 96–97% of GT1a treatment-naïve and treatment-experienced patients achieved an SVR12 [4–6], whereas after 12 weeks of therapy with the 3D regimen without ribavirin, 100% of GT1b-infected subjects without cirrhosis achieved an SVR12 [7, 8]. Furthermore, the SVR rate for GT1a cirrhotic subjects receiving the 3D regimen plus ribavirin for 12 or 24 weeks was 89 and 95%, respectively, while the SVR rate for GT1b cirrhotic subjects receiving 3D without ribavirin for 12 weeks was 100% [9]. This review focuses on the clinical pharmacokinetics of the dasabuvir component of the 3D regimen; the clinical pharmacokinetics of ombitasvir and paritaprevir/ritonavir have been reviewed separately [10, 11]. Key pharmacokinetic studies are summarized in Table 1.
2 Pharmacokinetics of Dasabuvir When Administered Alone
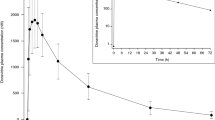
Following single-dose administration of dasabuvir capsules, maximum plasma concentrations (C max) were achieved within 3–4 h and the mean terminal phase elimination half-life ranged from 5 to 8 h (Study 1). Dasabuvir exhibited linear pharmacokinetics, with dose proportional increases in exposures (C max and area under the concentration–time curve [AUC]) over the range of 10–1200 mg. For the capsule formulation, increasing doses beyond 1200 mg did not increase dasabuvir exposures. Multiple dosing of dasabuvir capsules over a range of 200–1000 mg twice daily resulted in dose-proportional dasabuvir C max and AUC values, indicating linear pharmacokinetics (Study 3) (Table 2). The mean terminal half-life of dasabuvir was approximately 7 h. Little to no accumulation was seen at the lower doses, while at the highest dose of 1000 mg twice daily, a modest 65% accumulation was observed. Diurnal variation in dasabuvir pharmacokinetics was minimal.
The dasabuvir mean plasma concentration–time profiles after single and multiple doses are shown in Fig. 2.
3 Pharmacokinetics of Dasabuvir When Administered with Other Direct-Acting Antivirals
The pharmacokinetics of dasabuvir when administered with paritaprevir/ritonavir, with or without ombitasvir, was evaluated in a multiple-dose study (Study 5). Exposures of dasabuvir 400 mg twice daily decreased 50–60% in the presence of paritaprevir/ritonavir 200/100 mg {least squares mean ratio [90% confidence interval (CI)]: C max 0.41 [0.34–0.49]; AUC 0.50 [0.42–0.59]}. The effect of ombitasvir on dasabuvir exposures in the absence of paritaprevir/ritonavir was not evaluated. A cross-study comparison of dasabuvir exposures from the 3D regimen compared with a regimen without ombitasvir suggested that the addition of ombitasvir 25 mg to the combination of paritaprevir/ritonavir and dasabuvir increased dasabuvir exposures by approximately 30%. Thus, the addition of ombitasvir appears to counteract the decrease of dasabuvir exposures caused by paritaprevir/ritonavir.
The effect of dasabuvir on paritaprevir/ritonavir was also evaluated in Study 5. Coadministration of paritaprevir/ritonavir 200/100 mg with dasabuvir 400 mg led to an increase of approximately 50–65% in paritaprevir C max (least squares mean ratio [90% CI] 1.52 [1.02–2.26]) and AUC (1.66 [1.22–2.27]) values, respectively. Ritonavir C max and AUC values were minimally affected. Results of cross-study comparisons of the 3D versus 2D regimens indicated that dasabuvir had no effect on ombitasvir exposures.
4 Absorption, Distribution, Metabolism and Excretion
The absolute bioavailability of dasabuvir was determined for the 400 mg tablet (Study 6). The relative bioavailability of the dasabuvir 250 mg tablet (optimized tablet) in reference to the dasabuvir 400 mg tablet was also determined (Study 7). Taken together, the absolute bioavailability of dasabuvir from the 250 mg oral tablet was estimated to be approximately 71%.
Dasabuvir is >99.9% bound to human plasma proteins over a concentration range of 0.1–10 µM (0.05–5 µg/mL) [12]. At concentrations comparable to the C max with the 3D regimen, protein binding for dasabuvir did not show meaningful differences in subjects with different degrees of renal or hepatic impairment [13, 14]. The blood-to-plasma concentration ratio is approximately 0.7 in humans, indicating that dasabuvir is preferentially distributed into the plasma compartment of human whole blood [12].
Dasabuvir is predominantly metabolized by cytochrome P450 (CYP) 2C8 (60% in vitro) and, to a lesser extent, by CYP3A (30% in vitro), with minor contribution of other CYPs [15]. Following oral administration of a single dose of [14C]dasabuvir to humans, unchanged parent drug was the most abundant radioactive component in plasma (58% of total plasma radioactivity) [16]. Among seven metabolites identified in human plasma, M1 was characterized as a major metabolite (21% of total plasma radioactivity), while the other six were minor metabolites, each accounting for less than 10% of total radioactivity in plasma [16].
Exposure of the predominant M1 metabolite of dasabuvir has been characterized in phase I–III studies. When dasabuvir was administered alone in healthy subjects, the M1 metabolite to parent AUC ratio at steady state was 0.35. The ratio is higher when dasabuvir is administered as part of the 3D regimen, and was 0.58 at steady state in healthy subjects. The M1 metabolite is an active metabolite with similar antiviral activity compared with dasabuvir in vitro. The half-life of the M1 metabolite is similar to that of dasabuvir.
Following a single dose of 400 mg of 14C-dasabuvir, the total radiolabeled material was predominantly eliminated in the feces (94.4% of radioactive dose), with approximately 2% of the total radioactivity recovered in urine (Study 8) [16]. Unchanged dasabuvir in feces and urine accounted for 26 and 0.03%, respectively, of the total radioactivity recovered. Following a single dose of dasabuvir 400 mg, M1 was the most abundant metabolite in feces (31.5% of the total dose). Unchanged dasabuvir was the second major component of drug-related radioactivity in feces.
5 Dasabuvir Formulations and Food Effect
Three dasabuvir formulations, a 5 and 50 mg capsule, a 400 mg tablet, and a 250 mg tablet (optimized tablet), were evaluated in phase I relative bioavailability studies and phase Ib, II, and III studies. The 250 mg tablet is the available marketed formulation. The capsule formulation (8 × 50 mg) was bioequivalent to that of the 400 mg tablet formulation (least squares mean ratio [90% CI] of the 400 mg vs. 8 × 50 mg tablet 0.95 [0.81–1.11] for C max and 0.94 [0.82–1.07] for AUC). The 250 mg tablet formulation used in phase III studies also provides dasabuvir exposures that are comparable with those of the 400 mg tablet [used in phase II studies] (least squares mean ratio [90% CI] of the 250 mg vs. 400 mg tablet 0.90 [0.82–0.99] for C max and 0.96 [0.89–1.03] for AUC; results were not adjusted for dose) [Study 7].
Food had a moderate effect on the bioavailability of the 250 mg tablet (Study 9). Dasabuvir AUC and C max were 22–42% higher when the marketed 250 mg tablet was administered with a high-fat meal (consisting of 850 kcal with 59% of calories from fat) compared with fasting conditions (least squares mean ratio [90% CI]: C max 1.42 [1.10–1.82]; AUC 1.22 [1.01–1.46]). When administered with a moderate-fat meal (containing 612 kcal with 21% of calories from fat), dasabuvir AUC and C max increased approximately 30–53% relative to fasting conditions (C max 1.53 [1.19–1.96]; AUC 1.30 [1.08–1.55]. Because the fat content of a meal does not affect dasabuvir exposures, it is recommended dasabuvir be taken with food without regard to fat or calorie content [2, 3] because the other components of the 3D regimen have a larger food effect.
The dasabuvir tablet, along with coformulated ombitasvir/paritaprevir/ritonavir, is the first commercial product of the 3D regimen. Subsequently, a new formulation of the 3D regimen, referred to as the 3QD regimen, has been developed. This formulation included an extended-release layer of dasabuvir and immediate-release layer of ombitasvir/paritaprevir/ritonavir to allow for once-daily dosing. While paritaprevir C max was lower from this formulation and did not meet the bioequivalence criteria when compared with the 3D regimen, the AUC and C trough values that are more relevant for an antiviral product were comparable. This once-daily formulation was approved in the US based on bioavailability trials and exposure–response analyses to show comparability [17, 18].
6 Pharmacokinetics in Asian Subjects
The pharmacokinetics of dasabuvir was evaluated as a part of the 3D regimen in Han Chinese, Japanese and Caucasian subjects (Study 10). Following administration of the 3D combination (dasabuvir 400 mg twice daily + ombitasvir 25 mg once daily + paritaprevir/ritonavir 150/100 mg once daily) for 21 days, dasabuvir exposures in Chinese and Japanese subjects were comparable with Caucasian subjects (Table 3). The slightly higher exposures in Japanese subjects (40% higher C max and 29% higher AUC) is possibly due to cross-study comparison, the small number of subjects, or high intersubject variability. The difference is not considered to be clinically meaningful.
7 Pharmacokinetics in Hepatic and Renal Impairment
Dasabuvir pharmacokinetics when coadministered with ombitasvir plus paritaprevir/ritonavir have been evaluated in subjects with hepatic impairment (mild, Child–Pugh A; moderate, Child–Pugh B; and severe, Child–Pugh C; Study 11) or renal impairment (mild, creatinine clearance [CrCL] 60–89 mL/min; moderate, CrCL 30–59 mL/min; and severe, CrCL 15–29 mL/min; Study 12), including those on dialysis (Study 13) [13, 14]. The clinical pharmacokinetics of ombitasvir and paritaprevir/ritonavir have been reviewed separately [10, 11]. The results for dasabuvir and M1 are summarized in Table 4.
Dasabuvir pharmacokinetic parameters were not significantly altered in subjects with mild or moderate hepatic impairment, except for a decrease in C max in moderate impairment (Table 4). Severe hepatic impairment had little effect on dasabuvir C max but the AUC was increased. Dasabuvir M1 exposures were unaffected by mild hepatic impairment but were decreased by moderate hepatic impairment. Severe hepatic impairment had variable effects on dasabuvir M1 parameters as the C max decreased and the AUC increased [13].
Renal impairment had no clinically significant effect on dasabuvir exposures (Table 4). Although dasabuvir AUC increased by up to 21, 37, and 50% in subjects with mild, moderate, and severe renal impairment [14], these increases are not considered clinically meaningful to require dose adjustments [19]. Furthermore, CrCL was not a significant predictor of dasabuvir AUC in patients with chronic HCV infection and mild or moderate renal impairment [20]. In addition, the pharmacokinetics of dasabuvir were comparable between HCV-infected patients with stage 4 and 5 chronic kidney disease (including those on dialysis) and patients with normal renal function or mild renal impairment (Study 13) [21, 22].
8 Pharmacokinetics in Hepatitis C Virus Genotype 1-Infected Patients
Dasabuvir pharmacokinetics following dasabuvir monotherapy for 2–3 days were evaluated in HCV GT1-infected patients across dasabuvir doses of 100–1200 mg once daily and 100–800 mg twice daily in three clinical studies (Studies 1, 14, and 15). The dasabuvir half-life and AUC values in HCV-infected patients (Table 5) were similar to those observed in healthy subjects (Table 2).
Data from seven phase II/III studies in HCV GT1-infected patients were also analyzed using a population pharmacokinetic approach [23]. Dasabuvir pharmacokinetic parameters between HCV-infected patients and healthy subjects [12] are listed in Table 6. In this analysis, dasabuvir exposures in HCV-infected patients were slightly lower than, but generally comparable with, those observed in healthy subjects, likely due to sparse pharmacokinetic sampling in the phase II and III studies. Significant covariates for dasabuvir pharmacokinetics were cirrhosis, gender, CrCL and body weight on the apparent clearance, and age and body weight on apparent volumes. These covariates are expected to increase predicted drug exposures by less than 40%, which is not considered as clinically relevant as a change in exposure of 0.5–2.0-fold is not expected to alter the efficacy or safety of 3D therapy [23].
The 250 mg dose of dasabuvir (with exposures equivalent to the 400 mg dose used in monotherapy trials) was selected based on viral load decline in monotherapy trials, and efficacy, safety, and resistance data for dasabuvir in combination with other DAAs or pegylated interferon and ribavirin. The exposure-efficacy data from phase III trials also confirmed that the 250 mg dose of dasabuvir is the optimal dose [24].
9 Drug–Drug Interactions
Dasabuvir is primarily metabolized by CYP2C8, with a minor contribution from CYP3A. It has no inhibition or induction effects on CYP enzymes. In combination with ombitasvir and paritaprevir, dasabuvir inhibits uridine diphosphate glucuronosyltransferase (UGT) 1A1 isoenzymes. The clinical pharmacokinetics of ombitasvir and paritaprevir/ritonavir have been reviewed separately [10, 11]. Dasabuvir is also a substrate of the efflux transporters P-glycoprotein (P-gp) and breast cancer resistance protein (BCRP). It is an inhibitor of these same transporters; however, its net effect on transporter inhibition occurs when combined with paritaprevir and ritonavir, which are also P-gp and BCRP inhibitors.
A summary of the relevant mechanism-based drug–drug interactions for dasabuvir as a substrate or perpetrator is presented in Table 7. Most of these studies were conducted with dasabuvir as part of the 3D regimen that contains the potent CYP3A inhibitor ritonavir. Coadministration of dasabuvir with ketoconazole, a CYP3A and P-gp inhibitor, resulted in only a 41% increase in dasabuvir exposure and a less than 20% change in dasabuvir M1 exposure. The potent CYP2C8 inhibitor gemfibrozil increased dasabuvir C max to 2-fold and AUC to 11-fold compared with dasabuvir alone; dasabuvir M1 C max decreased by 20-fold and AUC decreased by 4-fold compared with dasabuvir alone. As a result, strong CYP2C8 inhibitors are contraindicated for coadministration with dasabuvir [25]. In contrast, the weak to moderate CYP2C8 inhibitor trimethoprim increased dasabuvir exposures by approximately 30% compared with dasabuvir alone. As a perpetrator, dasabuvir in combination with ombitasvir and paritaprevir inhibits UGT1A1 and BCRP, but not P-gp, as seen from the interactions with raltegravir, rosuvastatin, and digoxin, respectively.
Drug–drug interactions were also evaluated in several studies for antiretroviral drugs, immunosuppressants, and other commonly used medications [26–33]. Results from these studies suggest that drug–drug interactions between these agents and the 3D regimen are primarily mediated by other components of the regimens, besides dasabuvir, and are therefore not discussed in this review.
10 Conclusions
The clinical pharmacokinetics of dasabuvir alone were extensively evaluated when administered alone and as part of a combination with ombitasvir/paritaprevir/ritonavir. Dasabuvir demonstrated dose-proportional increases in exposure. The half-life of dasabuvir is approximately 5–8 h and therefore it is administered twice daily. Dasabuvir is minimally renally eliminated and its pharmacokinetics are not affected by renal impairment. The pharmacokinetics of dasabuvir are minimally affected by mild or moderate hepatic impairment; however, exposures are substantially elevated in subjects with severe hepatic impairment. Dasabuvir is metabolized predominantly by CYP2C8, with a minor contribution from CYP3A4, and is a substrate of P-gp and BCRP and an inhibitor of BCRP and UGT1A1. Except for strong CYP2C8 inhibitors or CYP3A/2C8 inducers, the metabolism of dasabuvir is not significantly compromised by concomitant medications.
References
Kati W, Koev G, Irvin M, Beyer J, Liu Y, Krishnan P, et al. In vitro activity and resistance profile of dasabuvir, a nonnucleoside hepatitis C virus polymerase inhibitor. Antimicrob Agents Chemother. 2015;59(3):1505–11.
Viekira Pak (ombitasvir, paritaprevir, and ritonavir tablets; dasabuvir tablets) [US package insert]. North Chicago: AbbVie Inc.; 2016.
Exviera (dasabuvir) [summary of product characteristics]. Maidenhead: AbbVie Ltd.; 2016.
Feld JJ, Kowdley KV, Coakley E, Sigal S, Nelson DR, Crawford D, et al. Treatment of HCV with ABT-450/r-ombitasvir and dasabuvir with ribavirin. N Engl J Med. 2014;370(17):1594–603.
Ferenci P, Bernstein D, Lalezari J, Cohen D, Luo Y, Cooper C, et al. ABT-450/r-ombitasvir and dasabuvir with or without ribavirin for HCV. N Engl J Med. 2014;370(21):1983–92.
Zeuzem S, Jacobson IM, Baykal T, Marinho RT, Poordad F, Bourliere M, et al. Retreatment of HCV with ABT-450/r-ombitasvir and dasabuvir with ribavirin. N Engl J Med. 2014;370(17):1604–14.
Hezode C, Asselah T, Reddy KR, Hassanein T, Berenguer M, Fleischer-Stepniewska K, et al. Ombitasvir plus paritaprevir plus ritonavir with or without ribavirin in treatment-naive and treatment-experienced patients with genotype 4 chronic hepatitis C virus infection (PEARL-I): a randomised, open-label trial. Lancet. 2015;385(9986):2502–9.
Andreone P, Colombo MG, Enejosa JV, Koksal I, Ferenci P, Maieron A, et al. ABT-450, ritonavir, ombitasvir, and dasabuvir achieves 97% and 100% sustained virologic response with or without ribavirin in treatment-experienced patients with HCV genotype 1b infection. Gastroenterology. 2014;147(2):359 e1–365 e1.
Feld JJ, Moreno C, Trinh R, Tam E, Bourgeois S, Horsmans Y, et al. Sustained virologic response of 100% in HCV genotype 1b patients with cirrhosis receiving ombitasvir/paritaprevir/r and dasabuvir for 12 weeks. J Hepatol. 2016;64(2):301–7.
Menon RM, Polepally AR, Khatri A, Awni WM, Dutta S. Clinical pharmacokinetics of paritaprevir. Clin Pharmacokinet. doi:10.1007/s40262-017-0520-x.
Badri PS, Shuster DL, Dutta S, Menon RM. Clinical pharmacokinetics of ombitasvir. Clin Pharmacokinet. doi:10.1007/s40262-017-0518-4.
Holkira Pak (ombitasvir/pritaprevir/ritonavir and dasabuvir) product monograph. St-Laurent: AbbVie Corp.; 2016.
Khatri A, Menon RM, Marbury TC, Lawitz EJ, Podsadecki TJ, Mullally VM, et al. Pharmacokinetics and safety of co-administered paritaprevir plus ritonavir, ombitasvir, and dasabuvir in hepatic impairment. J Hepatol. 2015;63(4):805–12.
Khatri A, Dutta S, Marbury T, Preston RA, Rodrigues L Jr, Wang H, et al. Pharmacokinetics and tolerability of anti-hepatitis C virus treatment with ombitasvir, paritaprevir, ritonavir, with or without dasabuvir, in subjects with renal impairment. Clin Pharmacokinet. 2017;56(2):153–63.
Bow DAJ, Liu J, Kavetskaia O, Menon R, de Morais SM, Nijsen M. A mechanistic non-clinical assessment of drug-drug interactions (metabolism and transporters) with the hepatitis C virus (HCV) regimen: ABT-450/r, ombitasvir and dasabuvir. AASLD/EASL Special Conference on Hepatitis C. New York, NY, 3–5 October 2014.
Shen J, Serby M, Reed A, Lee AJ, Menon R, Zhang X, et al. Metabolism and disposition of hepatitis C polymerase inhibitor dasabuvir in humans. Drug Metab Dispos. 2016;44(8):1139–47.
US FDA. FDA hepatitis update—approval of VIEKIRA XR extended release fixed dose combination tablets. https://content.govdelivery.com/accounts/USFDA/bulletins/158dd48. Accessed 16 Jan 2017.
Viekira XR (dasabuvir, ombitasvir, paritaprevir, and ritonavir extended release tablets) package insert. North Chicago: AbbVie Inc.; 2016.
US FDA, Center for Drug Evaluation and Research. Application number 206619Orig1s000. Summary review. http://www.accessdata.fda.gov/drugsatfda_docs/nda/2014/206619Orig1s000SumR.pdf. Accessed 16 Jan 2017.
Polepally AR, Badri PS, Eckert D, Mensing S, Menon RM. Effects of mild and moderate renal impairment on ombitasvir, paritaprevir, ritonavir, dasabuvir, and ribavirin pharmacokinetics in patients with chronic HCV infection. Eur J Drug Metab Pharmacokinet. doi:10.1007/s13318-016-0341-6.
Pockros PJ, Reddy KR, Mantry PS, Cohen E, Bennett M, Sulkowski MS, et al. Efficacy of direct-acting antiviral combination for patients with hepatitis C virus genotype 1 infection and severe renal impairment or end-stage renal disease. Gastroenterology. 2016;150(7):1590–8.
Shuster DL, Menon RM, Ding B, Li H, Cohen E, Cohen DE, et al. Ombitasvir, paritaprevir, ritonavir, dasabuvir and ribavirin pharmacokinetics in HCV-infected subjects with chronic kidney disease stage 4 (severe renal impairment) or stage 5 (end-stage renal disease). Hepatology. 2016;64(1 Suppl):975A.
Mensing S, Eckert D, Sharma S, Polepally AR, Khatri A, Podsadecki TJ, et al. Population pharmacokinetics of paritaprevir, ombitasvir, dasabuvir, ritonavir and ribavirin in hepatitis C virus genotype 1 infection: analysis of six phase III trials. Br J Clin Pharmacol. doi:10.1111/bcp.13138.
Khatri A, Mensing S, Podsadecki T, Awni W, Menon R, Dutta S. Exposure-efficacy analyses of ombitasvir, paritaprevir/ritonavir with dasabuvir ± ribavirin in HCV genotype 1-infected patients. Clin Drug Investig. 2016;36(8):625–35.
Menon RM, Badri PS, Wang T, Polepally AR, Zha J, Khatri A, et al. Drug–drug interaction profile of the all-oral anti-hepatitis C virus regimen of paritaprevir/ritonavir, ombitasvir, and dasabuvir. J Hepatol. 2015;63(1):20–9.
Badri PS, Dutta S, Wang H, Podsadecki TJ, Polepally AR, Khatri A, et al. Drug interactions with the direct-acting antiviral combination of ombitasvir and paritaprevir-ritonavir. Antimicrob Agents Chemother. 2015;60(1):105–14.
Polepally AR, King JR, Ding B, Shuster DL, Dumas EO, Khatri A, et al. Drug–drug interactions between the anti-hepatitis C virus 3D regimen of ombitasvir, paritaprevir/ritonavir, and dasabuvir and eight commonly used medications in healthy volunteers. Clin Pharmacokinet. 2016;55(8):1003–14.
Khatri A, Dutta S, Wang H, Podsadecki T, Trinh R, Awni W, et al. Evaluation of drug–drug interactions between hepatitis C antiviral agents ombitasvir, paritaprevir/ritonavir, and dasabuvir and HIV-1 protease inhibitors. Clin Infect Dis. 2016;62(8):972–9.
King JR, Dutta S, Cohen D, Podsadecki TJ, Ding B, Awni WM, et al. Drug–drug interactions between sofosbuvir and ombitasvir–paritaprevir–ritonavir with or without dasabuvir. Antimicrob Agents Chemother. 2015;60(2):855–61.
Zha J, Badri PS, Ding B, Uchiyama N, Alves K, Rodrigues-Jr L, et al. Drug interactions between hepatoprotective agents ursodeoxycholic acid or glycyrrhizin and ombitasvir/paritaprevir/ritonavir in healthy japanese subjects. Clin Ther. 2015;37(11):2560–71.
Badri P, Dutta S, Coakley E, Cohen D, Ding B, Podsadecki T, et al. Pharmacokinetics and dose recommendations for cyclosporine and tacrolimus when coadministered with ABT-450, ombitasvir, and dasabuvir. Am J Transplant. 2015;15(5):1313–22.
Badri PS, King JR, Polepally AR, McGovern BH, Dutta S, Menon RM. Dosing recommendations for concomitant medications during 3D anti-HCV therapy. Clin Pharmacokinet. 2016;55(3):275–95.
Khatri A, Trinh R, Zhao W, Podsadecki T, Menon R. Drug–drug interaction between the direct-acting antiviral regimen of ombitasvir/paritaprevir/ritonavir plus dasabuvir and the hiv antiretroviral agents dolutegravir or abacavir plus lamivudine. Antimicrob Agents Chemother. 2016;60(10):6244–51.
Acknowledgements
The authors thank AbbVie employee Amy K. Rohrlack for medical writing support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The studies summarized in this report were supported by AbbVie, who contributed to the study designs, research, and interpretation of data, and the writing, reviewing, and approving of the publication.
Conflicts of interest
Jennifer R. King, Jiuhong Zha, Amit Khatri, Sandeep Dutta, and Rajeev M. Menon are current or former AbbVie employees and may own AbbVie stock or stock options.
Rights and permissions
About this article
Cite this article
King, J.R., Zha, J., Khatri, A. et al. Clinical Pharmacokinetics of Dasabuvir. Clin Pharmacokinet 56, 1115–1124 (2017). https://doi.org/10.1007/s40262-017-0519-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-017-0519-3