Abstract
Background and Objective
Tramadol hydrochloride is used worldwide as an analgesic drug with a unique dual function. The metabolic enzymes cytochrome P450 (CYP) 3A4, CYP2B6, and CYP2D6 and the various transporters [adenosine triphosphate-binding cassette B1/multidrug resistance 1/P-glycoprotein, organic cation transporter 1, serotonin transporter (SERT), norepinephrine transporter (NET)] and receptor genes (opioid receptor μ 1 gene) give possible genetic differences that might affect the pharmacokinetics and/or pharmacodynamics of tramadol. Therefore, the aim of this review is to present a systematic walkthrough of all possible genetic factors involved in the pharmacology of tramadol.
Method
A systematic literature search was conducted in PubMed and EMBASE involving all metabolic enzymes, drug transporters and receptors, as well as SERT and NET that are involved in the pharmacokinetics and pharmacodynamics of tramadol. An additional search on population pharmacokinetics with genetic factors as covariates was performed separately.
Results
A total of 56 studies (45 cohort and case-control studies, three case reports, six in vitro studies, and two animal studies) were included.
Conclusion
In this systematic review, the current knowledge on all possible genetic factors that might influence the metabolism or clinical efficacy of tramadol has been collected and summarized. Only the effect of CYP2D6 polymorphisms on the metabolism of tramadol and the consequent effect on pain relief has been thoroughly studied and sufficiently established as clinically relevant.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Cytochrome P450 (CYP) 2D6 polymorphism is the major genetic factor in the metabolism of tramadol. |
Other possible genetic factors besides CYP2D6 have been insufficiently researched to draw a proper conclusion. |
Hypothetically, the inter-individual variability of the bioavailability of tramadol within a CYP2D6 genotype group could be explained by the number of active multidrug resistance 1 alleles. |
Decreased activity of organic cation transporter might lead to increased O-desmethyltramadol plasma concentration. |
1 Background
Tramadol hydrochloride (tramadol) was synthesized in 1962 and marketed in 1977 in Germany by Grünenthal GmbH Stolberg. It became the leading analgesic drug in Germany [1, 2], and during the past 38 years it has been approved in over 100 countries, including the UK, USA, Republic of China and Canada [3].
Tramadol is a synthetic opioid with a unique dual analgesic effect by acting centrally through both the activation of the μ-opioid receptor and inhibiting norepinephrine (noradrenaline) and serotonin (5-hydroxytryptamine, 5-HT) reuptake [4]. Therefore, the indication of treatment ranges widely from moderate to moderately severe chronic pain [5] to chemotherapy-induced neuropathy [6]. The most common side effects are nausea, dizziness, drowsiness, sweating and dry mouth, while other well-established opioid-induced adverse events such as constipation and respiratory depression are uncommon [5].
The purpose of this systematic review is to provide an updated summary on the pharmacogenetics of tramadol. For introductory purposes, we briefly present an overview of the basics of clinical pharmacology of tramadol.
1.1 Clinical Pharmacology of Tramadol
Tramadol hydrochloride, (1RS,2RS)-2-[(dimethylamino)methyl]-1-(3-methoxyphenyl)-cyclohexanol hydrochloride, is structurally related to morphine and codeine. It has two chiral centres (Fig. 1) and is administered as a racemate of two enantiomers, (+)-tramadol and (−)-tramadol. The drug is available as drops, capsules and sustained-release formulations for oral use, suppositories for rectal use, and as a solution for intravenous, intramuscular and subcutaneous use [1].
The pharmacokinetics and pharmacodynamics of tramadol have previously been described in detail [1], and we present here a brief summary of the immediate-release formulation for an introductory general overview.
1.1.1 Pharmacokinetics
After a single oral dose of tramadol 100 mg, the bioavailability is 68 %, mostly owing to a first-pass metabolism of 20–30 %. The peak plasma concentration (C max) of about 300 µg/L is reached after 1.6 h [7]. The time to peak brain concentration is 10 min. After multiple doses (100 mg × 4) of tramadol, the bioavailability increases to 90–100 %, suggesting a saturation of the first-pass metabolism. C max increases linearly over the 50- to 400-mg dose range and reaches a steady-state peak of around 350 µg/L at maximum dosage. Additionally, C max increases 17 % after a high-fat meal compared with administration in the fasting state [1].
The plasma protein binding is 20 %, and tramadol is rapidly distributed in the body with a high tissue affinity reflected in a total distribution volume of 306 L. The initial distribution half-life is 6 min, but increases with time to 1.7 h [1]. The elimination is mainly through the liver but approximately 30 % of the parent drug is excreted unchanged via the kidneys together with the majority of the metabolites [7]. The biliary excretion of tramadol and its metabolites account for less than 1 %. The mean elimination half-life of tramadol is 5–6 h [1] and greatly dependent on the cytochrome P450 (CYP) 2D6 phenotype, and likely other genetic factors [8].
O-Desmethyltramadol (M1), the major active metabolite of tramadol, reaches C max 3 h after administration at 18–26 % of the C max value of tramadol. The mean elimination half-life is approximately 7 h [1].
1.1.2 Pharmacodynamics
Tramadol works through two distinctive mechanisms. As with other opioids, tramadol selectively activates the µ-opioid receptor mainly through the active metabolite (+)-M1 and to a lesser degree (−)-M1 and (±)-N,O-didesmethyl-tramadol (M5). Neither of the compounds has an affinity with the δ- and κ-opioid receptor. (+)-M1 has an affinity 700 times higher than its parent compound (±)-tramadol and 5.5 times less than morphine. (±)-M5 showed a 24 times higher affinity than (±)-tramadol [9]. Part of the opioid effect is miosis, which can be measured by pupillometry. Several studies have shown that the miotic effect of tramadol increases with the CYP2D6 enzymatic activity (poor metabolizer < intermediate metabolizer < extensive metabolizer) in correlation to the plasma concentration of M1 [10–12]. Naloxone only attenuates the analgesic effect of tramadol but abolishes its miotic effect, and this was the reason why an additional mechanism of action was suspected [13].
The parent compound is responsible for the inhibition of neuronal reuptake of norepinephrine and 5-HT. (+)-Tramadol is approximately fourfold more potent than (−)-tramadol in inhibiting serotonin reuptake [14], while (−)-tramadol is responsible for the inhibition of norepinephrine reuptake and induction of norepinephrine efflux [1]. The former effect is most likely owing to the inhibition of the serotonin transporter (SERT) [14], while the latter interferes with the norepinephrine transporter (NET) function [1]. Furthermore, (±)- and (+)-tramadol also increase serotonin efflux by an unknown mechanism [14].
Interestingly, the added analgesic value of each enantiomer of tramadol and M1 is lower than the actual effect of the drug, suggesting a synergistic behaviour of the racemate. In comparison, the severity of the adverse events of the racemic drug is less than the added value of each enantiomer by itself, suggesting in this case an antagonistic effect [1].
2 Methods
Following the PRISMA guidelines for systematic reviews [15], a research librarian and the first author conducted literature searches using the keywords: tramadol, pharmacogenomics, CYP2D6, UGT2B7, CYP3A4, SLC22A1, OCT1, OCT-1, ABCC2, ABCC-2, MDR-1, MDR1, SLC6A4, SERT, NET, OPRM-1 and OPRM1 for the pharmacogenetic search and the keywords: tramadol, drug interaction, drug interactions, interaction, interactions, human and humans for the drug interaction search. Strategies were based on identifying literature that holds information on the main topic tramadol combined with the appropriate keyword or keyword terms. Concepts were combined with Boolean operators (OR, AND) to ensure more than one concept was included in the result. A limit of “English language” was applied. The databases used included PubMed (Medline) and EMBASE (Exerpta Medica, Elsevier; Ovid). The databases were searched from inception until 15 December 2014.
The articles were independently screened by their titles and abstracts by the first author and two clinical pharmacologists. Case reports, case-control and cohort studies were eligible for inclusion if they reported original data on genetic variations of CYP2D6, CYP3A4, UGT2B7, OCT1, MDR1, SERT, NET and OPRM1 in relation to the pharmacokinetics and pharmacodynamics of tramadol as well as drug–drug interactions with tramadol. Abstracts and conference proceedings were excluded. Extracted articles were cross-referenced for additional original publications. If more than one study or updated data were available from the same cohort, the study or most recently updated data was chosen.
A separate PubMed search for population pharmacokinetic studies was performed (February 28th, 2015) using the search string “tramadol AND (pharmacokinetics OR pharmacokinetic study) AND (population OR pooled OR modelling)”. The limit of “English language” was applied.
3 Results
Figure 2 shows the process of study identification and selection for the first literature search, which identified 144 articles in PubMed and 298 articles in EMBASE. After removal of duplications (89 articles), articles were selected based on title and abstract by the first author. A total of 114 articles were critically viewed by the remaining two authors revealing 50 articles, which met the inclusion criteria. Further cross-reference searching revealed another four articles included in this review, resulting in a total of 54 eligible papers for review: 43 cohort and case-control studies, three case reports, six in vitro studies and two animal studies.
The second literature search identified 44 articles. By abstract screening only two of these were identified as population pharmacokinetic studies based on human data that included genotypes as covariates and were included in this review.
3.1 Overview of the Pharmacogenetics of Tramadol
The main metabolic pathways of tramadol consist of N- and O-demethylation (phase I reactions) and conjugation of O-demethylated metabolites (phase II reactions) (Fig. 1). Currently, 23 different metabolites (both active and inactive) of tramadol have been identified in humans [1].
The main enzymes in the phase I reactions are CYP2D6, CYP2B6 and CYP3A4. CYP2D6 is the main enzyme responsible for the O-desmethylation, and CYP2B6 and CYP3A4 are responsible for the N-demethylation. CYP2D6 transforms tramadol to O-desmethyltramadol (M1) separated into the respective enantiomers [7]. Studies have shown a higher affinity of (+)-tramadol to CYP2D6 than (−)-tramadol, and a smaller reduction in the biotransformation of (−)-tramadol to (−)-M1 in the case of a poor metabolizer, suggesting that a fourth CYP enzyme is involved in this process [16]. CYP2B6 and CYP3A4 are responsible for N-desmethylation of the enantiomers of tramadol with N-desmethyltramadol (M2) first in line. During phase I reactions, five different metabolites (M1–5) and their respective enantiomers are created. The remaining 23 metabolites of tramadol in humans are metabolized by phase II reaction and mainly derived from M1 and M5 conjugates via glucuronidation, sulphatation and hydroxylation. Known enzymes involved in this process are uridine 5′-diphospho (UDP)-glucuronosyltransferases (UGT)1A8 and UGT2B7 (Fig. 1) [7].
M1 is transported from the blood stream into the liver cell via the organic cation transporter (OCT)-1 (SLC22A1), and phase II metabolites are transported out of the liver cell by P-glycoprotein (P-gp) [adenosine triphosphate (ATP)-binding cassette (ABC)B1] efflux transporter encoded by the ABCB1 or multidrug resistance gene MDR-1 [7].
We present a systematic overview of genetic factors of the main metabolizing enzymes, transport proteins and receptors related to the pharmacokinetics and pharmacodynamics of tramadol. An overview of the results is presented in Table 1.
3.1.1 Drug-Metabolizing Enzymes
The cytochrome P450 (CYP) superfamily is the most important phase I drug-metabolizing enzyme, which oxidizes both endogenous substances and xenobiotics into more hydrophilic compounds. There are 57 functional CYP genes and 58 pseudogenes within 18 families in humans. CYP2D6 is one of the most investigated CYP, even though it only accounts for about 2–4 % of hepatic CYP enzymes. However, CYP2D6 catalyzes the metabolism of approximately 25 % of currently used drugs in the human liver [17].
There are two ways to determine a person’s specific CYP2D6 enzyme activity.
Genotyping is typically performed by polymerase chain reaction looking at the involved genes and possible variations. An assay was developed to determine possible poor metabolizers with the CYP2D6*3 and *4 alleles, the most common non-functional alleles in Caucasians, in just 60 min, making genotyping more accessible for future use [18].
Phenotyping is performed by oral ingestion of a probe drug followed by measurement of plasma or urine concentration of the parent compound and its metabolites. It is important that the enzyme responsible for producing the metabolites is known so that its activity can be measured. For CYP2D6, sparteine and debrisoquine were the golden probe drug standards used for a long time. Neither of these classical drugs have been marketed as a drug for a number of years, and other alternatives have been investigated. A study showed that tramadol can be used as a probe drug for CYP2D6 phenotyping with a sensitivity of 100 % and a specificity of 99.6 % [3].
3.1.1.1 CYP2D6
There are four different phenotypes that are generally used to describe the individual capability of CYP2D6 metabolism, though the clinical relevance of the intermediate metabolizer phenotype is somewhat controversial. The genotype-phenotype association has been subject to some controversy, and no true consensus exists as to the definition of which combination of genotype alleles constitutes the four phenotypes [19–21]. For the purpose of the review, the classification assigned by the Clinical Pharmacogenomics Implementation Consortium [22] was used. Poor metabolizers (PM) have two non-functional alleles; intermediate metabolizers (IM) have one reduced-function allele and a non-functional allele; extensive metabolizers (EM) have at least one fully functional allele or two reduced-function alleles. Ultra-rapid metabolizers (UM) have more than two functional alleles [19, 22]. Presently, at least 74 different human CYP2D6 variant alleles (*2 to *75) and a set of subvariants (e.g. CYP2D6*2A-M) has been identified, besides the wild-type allele *1, and designated by the Human Cytochrome P450 Allele Nomenclature Committee [23]. The frequency of the different genotypes varies among the ethnic groups. Thus, PMs have the lowest frequency in Asia (0–5 %), followed by Hispanics (2–7 %) and Caucasians (7–10 %). The frequency in Africans varies widely depending on which part of Africa they come from (0–19 %). The prevalence of UM is low among North Europeans (0.8–3.6 %), slightly higher in American Caucasians and Blacks (4.3 and 4.5 %, respectively) and significantly higher among Mediterranean Europeans (7–10 %). The highest frequency of UMs is among Black Ethiopians and Saudi Arabians (16 and 20 %, respectively) [17].
The PM phenotype is characterized by carrying 2 of the 22 existing null alleles (*3 to *8, *11 to *16, *18 to *21, *38, *40, *42, *44, *56 and *62), among which *3 (rs35742686), *4 (rs1065852, rs28371703, rs28371704, rs3892097), *5 (gene deletion), and *6 (rs5030655) account for approximately 97 % of all alleles causing the PM genotype in Caucasians. Null alleles encode no functional protein and there is no detectable enzyme activity [17].
The PM phenotype status can be achieved by carrying two null alleles or being subject to an effective drug–drug interaction. Thus, quinidine was a very potent inhibitor (inhibitor constant, ki equal to 15 nM) of the O-demethylation of tramadol in human liver microsomes, and this was the very first clear indication that this oxidation is catalyzed by CYP2D6 [24]. No similar study has been conducted in humans. In healthy volunteers, paroxetine reduced the production of M1, especially (+)-M1, significantly. The analgesic effect in all the experimental pain models (cold pressor test, electrical sural nerve stimulation and pressure pain tolerance threshold) was attenuated but not abolished [25]. The reduced μ-opioid receptor activation was measurable by pupillometry, showing reduced pupil constriction amplitude and increased pupil size [26]. A study of healthy subjects demonstrated that the weak CYP2D6 inhibitor escitalopram reduced the plasma concentration of (+)-M1 but not to a clinically relevant extent. Thus, the analgesic effect was unchanged but the miotic and sedative effects of tramadol were reduced [27]. A study conducted in drug abusers on maintenance methadone or buprenorphine therapy showed that concomitant intake of methadone significantly inhibited the formation of (±)-M1, resulting in insufficient pain management [28]. A possible interaction between tramadol and warfarin was examined, because there had been 17 reports in Sweden describing a possible interaction with increased international normalised ratio values. Ten out of 17 patients were genotyped for CYP2D6*3 and *4; CYP2C9*2 and *3; CYP2C19*2 variants. Eight out of the 10 genotyped had a defective CYP2D6 allele (PM or IM) and/or used a drug known to be a CYP2D6 inhibitor. These findings were not statistically significant, possibly owing to the small sample size [29].
The CYP2D6 PMs are also pharmacokinetically clearly different from the EMs. Thus, the areas under the plasma concentration-time curves (AUC) of (+)- and (−)-tramadol are increased, and the AUC of mainly (+)-M1 [30–34] and to a lesser degree (−)-M1, are decreased in PMs [16]. The half-life and time to peak plasma concentration of both enantiomers of tramadol and M1 were prolonged [31]. The tramadol/M1 ratio and the tramadol/M2 ratio correspond even post-mortem with the CYP2D6 genotype. Thus, the tramadol/M1 ratio is significantly higher in PMs than IMs, EMs or UMs, while the opposite is true in the case of the tramadol/M2 ratio [35].
The pharmacodynamic differences between PMs and EMs are illustrated by the need forhigher dosages of tramadol to achieve sufficient pain management and an increased need for rescue medication. In some PM patients, tramadol has no effect at all [18, 33, 36, 37]. In experimental pain studies, tramadol increased the pain pressure tolerance, nociceptive reflex threshold [30] and the pain tolerance threshold to single sural nerve stimulation significantly in PMs [32]. Pressure pain detection was only increased in EMs, and peak pain [30] and area under the pain curve in cold pressure tests was only reduced in EMs [30, 32]. In contrast, a study of cancer patients with oxaliplatin-induced polyneuropathy did not find a correlation between the reduction in pain, paraesthesia and dynamic allodynia and the (+)-M1 plasma concentration [6, 38].
Finally, the PM phenotype status influences the frequency and intensity of side effects. Several studies suggest that the frequency and intensity increases with a higher (+)-M1 concentration, thus PMs are mostly free of side effects while EMs usually have side effects of mild to moderate intensity, if any [18, 30]. UMs can experience life-threatening side effects (see later) [39, 40]. The onset of side effects in tramadol users was correlated with an increased plasma epinephrine concentration [16].
The IM phenotype is characterized by a combination of a null allele with a reduced-function allele (*10, *14, *17, *18, *36, *41, *47, *49, *50, *51, *54, *55 and *57). The reduced enzymatic activity may be the result of decreased protein stability, changes in substrate recognition and reduced affinity [17]. CYP2D6*10 (rs1065852, rs1135840, rs1058164) is the most extensively researched reduced-function allele because of a high occurrence rate in the Asian population of 51–70 % [41], while it only occurs at low frequencies (2–5 %) in Caucasians and African Americans [17]. An in vitro study showed that the tramadol clearance by CYP2D6*10 was reduced to 6.9 % of the clearance of the wild-type allele, while it was only reduced to 36 % in the CYP2D6*17 (rs28371706, rs16947, rs1135840, rs1058164) allele. Surprisingly, this reduction was not caused by reduced substrate-enzyme affinity as seen for other CYP2D6 substrates interacting with the *10 and *17 variants [42]. A study in Malaysian patients showed a correlation between the number of *10 alleles and an increase in the plasma concentration and half-life of tramadol [43]. These results were confirmed by two Chinese studies conducted in healthy subjects [44] and patients [45]. Additionally, these studies demonstrated that the clearance rate of tramadol and M1 was significantly decreased in heterozygous (*1/*10) carriers compared with *1/*1 controls [40]. Another study in Chinese patients showed a significantly higher intake of tramadol after surgery among patients homozygous for the *10 allele [41].
The EM phenotype is characterized by having at least one fully functional allele or two reduced-function alleles (e.g. *1/*17 x 2 or *41 x 2) [17, 46].
The UM phenotype is characterized by carrying a duplication or multi-duplication of functional and reduced-function alleles. The *53 (rs1135822, rs1135823, rs267608305) allele, which is found in a small percentage of South Asians, might cause ultra-rapid metabolism of tramadol even without duplication. The most common alleles involved in duplication are *1, *2, *4, *6, *10, *17, *29, *35, *43 and *45. The number of copies found can range from 0 to 13 causing a significant change in CYP2D6 activity when >2 [17]. The effect of double duplications of the alleles *1, *2 (rs16947, rs1135840), *35 (rs769258, rs16947, rs1135840, rs1080985, rs1058164) and *41 (rs16947, rs28371725, rs1135840, CYP2D6—1235A>G, rs28624811, rs28633410, rs1058164) on the pharmacokinetics and pharmacodynamics of tramadol was far smaller than expected, but still adverse effects were significantly more common in UMs [47]. There are several case reports on patients using tramadol who had serious adverse reactions not seen among PMs or EMs. A 66-year-old man receiving patient-controlled administration of tramadol was found unconscious and unresponsive with respiratory insufficiency 10 h after initiation of tramadol [39]. A 22-year-old female abuser of tramadol attempted suicide with an overdose of 4.5 g of tramadol. She had cardiac arrest, hypothermia, hypoglycaemia, lactic acidosis and renal failure [40]. In both cases, the patient was subsequently genotyped as an UM.
3.1.1.2 Children
Several studies on CYP2D6 maturation and genetic variation in (pre)term neonates and infants and the impact on tramadol metabolism have been performed. However, factors other than genetic variation have to be considered in children because the physiological composition (relative liver cell mass, body fat, size and weight) and maturation of hepatic and renal function in infants are substantially different than in adults [48].
In a whole series of trials aimed at investigating the disposition of tramadol related to CYP2D6 activity in neonates and infants [49–52], it was discovered that the clearance of tramadol was 23 % of the adult value at 25 weeks post-conception age (PCA), which slowly increased to 84 % by 44 weeks PCA. Hence, dose adjustment in preterm children is required [49]. Later, it was observed by collecting urine samples that 35 % of the tramadol dose was found in urine within the first 24 h in (pre)term neonates and infants. The parent compound contributed 79 %, M1 10 % and M2 only 3 % to overall urinary elimination. A significant correlation between the logarithmic ratio of urinary M/M1 and the child’s gestational age was found [50]. The inter-individual variations were not fully accounted for; thus, the importance of genetic polymorphisms in early age was studied subsequently. The interesting part is that the importance of CYP2D6 polymorphisms increases with age in relation to CYP2D6 maturation. In preterm neonates, genetic variation of the CYP2D6 gene has a smaller impact on the analgesic effect of tramadol, because the (±)-M1 formation clearance in general is very sparse at that age. However, with increasing age, the (±)-M1 formation clearance increases depending on existing CYP2D6 polymorphisms [51]. It was concluded that the metabolic clearance of tramadol is independent of the CYP2D6 genotype in preterm neonates, but from the age of 44 weeks, where maturation of CYP2D6 should be close to that of an adult, the metabolic clearance is dependent on both PCA and CYP2D6 polymorphisms [52].
3.1.1.3 CYP3A4, CYP3A5 and CYP2B6
CYP3A4 and CYP2B6 are the major enzymes involved in the formation of M2. CYP3A4 and CYP3A5 are distinct CYP enzymes of the 3A family with a substantial overlap of substrate specificity. Tramadol seems to be more specific for CYP2B6 than CYP3A4, but CYP3A4 is more abundant in the human liver with the concentration ranging from 44 to 250 pmol/mg of protein compared with CYP2B6 with a concentration ranging from 1 to 39 pmol/mg of protein [53]. CYP3A4 and CYP2B6 also catalyze the N-demethylation of M1 to M5 and M2 to M3 [7].
The most common polymorphisms of CYP3A4 are *1B (rs2740574), an adenine >guanine transition in the gene promoter region, *20 (rs67666821), a premature stop codon, and *22 (rs35599367), which also results in reduced CYP3A4 activity. The polymorphism CYP3A4*22 has a frequency of 8 % in Caucasians and 4 % in Asians and Africans. All other polymorphisms are even less common. A functional CYP3A5 enzyme is only expressed in 5–10 % of Caucasians, and this is because of a high frequency of the CYP3A5*3 (rs776746) splice mutation (A6986G transition in intron 3), while 60 % of Africans and African Americans have one. Thus, a non-functional CYP3A4 enzyme is much more likely to have an impact in the Caucasian population [54]. CYP2B6 has 53 allelic variants of which *5 (rs3211371) and *6 (rs3745274), a guanine >thymine transition in position 516, are the most prevalent variants. The frequency of the different polymorphisms of CYP2B6 vary widely among the different ethnicities [55].
A single interaction study between tramadol and itraconazole, a potent CYP3A4 inhibitor, was located. It did not show any alterations of the plasma concentration of tramadol or its metabolites [56]. We have not been able to identify studies on the effect on the plasma concentration of tramadol or its metabolites with the inhibition or induction of CYP3A5 or CYP2B6.
3.1.1.4 UGT2B7
UGT2B7, present in the liver and in the small intestine, is the major enzyme responsible for phase II reactions in the pathway of tramadol. In the liver, UGT2B7 has a threefold higher glucuronidation rate of (−)-M1 than (+)-M1, while such an effect is not apparent for intestinal UGT2B7 [57]. UGT2B7 is not very polymorphic, and to date there exist no variants that have been proven clinically relevant [58].
No studies have been found on the effect on the plasma concentration of tramadol or its metabolite M1 with the inhibition or induction of UGT2B7.
3.1.1.5 Clinical Significance of Genetic Variants in Drug-Metabolizing Enzymes
Currently, only the CYP2D6 phenotype is clinically relevant to treatment with tramadol, resulting in insufficient pain management in PMs or serious adverse effects in UMs. The available evidence does not allow for conclusions on the value of preemptive CYP2D6 genotyping and genotype classification in everyday clinical practice. In light of the frequency of UMs in different ethnicities, general genotyping in the North European population is unlikely to be of noteworthy clinical relevance. Among black Ethiopians and Saudi Arabians, where the frequency is between 16 and 20 %, genotyping might be hypothesized to reduce the frequency of serious adverse effects.
3.1.2 Transporter Proteins
3.1.2.1 OCT1
OCT1 or SLC22A1 is the most common organic cation transporter in the human liver. It plays an important role in transporting M1 from the blood stream into the liver cells for further metabolism [7]. There exist several well-known polymorphisms caused by amino acid substitution, Arg61Cys (rs12208357), Cys88Arg (rs55918055), Gly401Ser (rs34130495) and Gly465Arg (rs34059508), and deletion, Met420 (rs72552763). Approximately 10 % of the Caucasian population therefore has reduced or absent OCT1 activity [59].
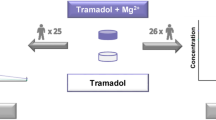
In a clinical study of healthy volunteers, categorized as IM, EM or UM of CYP2D6, the plasma concentration and AUC from 0 to 24 h (AUC0-24) of (+)-M1 increased, while the half-life of (+)-M1 shortened in correlation to the increasing number of inactive OCT1 alleles. This leads to prolonged miosis in volunteers carrying fewer active OCT1 alleles. However, when combining the polymorphisms of CYP2D6 (leading to an increase of the AUC of (+)-M1 for each active allele) and OCT1 (leading to a decrease of the AUC of (+)-M1 for each active allele), a statistically significant synergistic or antagonistic interaction was not found, suggesting OCT1 to be an independent and additive factor to the effects of CYP2D6 polymorphisms [59].
3.1.2.2 ABCB1/MDR1
The P-glycoprotein (P-gp) or ABCB1 or multidrug resistance 1 (MDR1) transporter belongs to the ATP-binding cassette (ABC) family, and it is primarily located in liver cells, renal tubules, enterocytes and in the endothelium of the blood–brain barrier. It serves as an efflux transporter and has broad substrate specificity, including many drugs. There are several known single nucleotide polymorphisms, C1236T (rs1128503), G2677T (rs2032582) and C3435T (rs1045642) that have been seen in association with increased and decreased expression of MDR1 [8]. The most researched single nucleotide polymorphism is C3435T. The genotype 3435TT leads to the lowest P-gp expression, thus causing increased drug accumulation in the cells and the brain. The frequency of the 3435TT genotype varies considerably among different ethnicities (Caucasians 24–28 %, Africans <7 % and south-west Asians 50 %) [60].
Tramadol has not been documented as a substrate for P-gp in an in vitro study [61]. A study with 21 healthy volunteers showed that the average C max and AUC0-24 values of (±)-tramadol, but not (±)-M1, increased with the increasing number of the 3435T alleles of MDR1 independently of the CYP2D6 status, but these findings were not statistically significant [62]. Hypothetically, the inter-individual variability of the bioavailability of tramadol within a CYP2D6 genotype group could be explained by this effect. In a later study, the analgesic effect in 156 patients undergoing knee arthroscopy was compared between the different MDR1 C3435T and CYP2D6 genotypes. The conclusion was that only the CYP2D6 genotype plays a role in the analgesic efficacy of tramadol [63]. In contrast, in a study of 250 Han Chinese, 2677T and 3435T alleles were more frequent among poor responders to tramadol. This finding appears counter-intuitive and there is no plausible biological mechanism to support such a finding [64]. However, the MDR1 3435T allele seems to have a protective association with alcohol dependency disorder [65]. The overall evidence does not support that tramadol is a substrate for P-pg to a clinically meaningful extent.
3.1.2.3 The Serotonin Transporter (SERT)
SERT belongs to the solute carrier (SLC) transporter family and is designated SLC6A4, and it is responsible for transporting serotonin back into the neuron. It is the binding site for some antidepressants (tricyclic antidepressants and selective serotonin reuptake inhibitors), resulting in an increased level of synaptic serotonin, thus raising the mood level. Tramadol is also known to inhibit serotonin reuptake by an unknown mechanism in humans. In a study with SERT knockout mice, the frequency of serotonin syndrome increased in heterozygous (+/−) and homozygous (−/−) knockout mice compared with wild-type (+/+) mice after administration of (±)-tramadol. The effect could be reduced in −/− mice by pre-treatment with a serotonin receptor (5-HT1A) antagonist, suggesting involvement of 5-HT1A in tramadol-induced serotonin syndrome. Additionally, it was found that the analgesic effect of tramadol was reduced by 58 % in −/− mice [66].
However, in humans, the serotonin transporter gene variant [5-HTTLPR (rs25531)] consists of a combination of long (l) (528 base pairs) and short (s) (484 base pairs) alleles in various combinations (l/l, l/s and s/s). Some studies have shown that patients diagnosed with depression and having the long allele in their genotype had a better response to selective serotonin reuptake inhibitor treatment than patients with the s/s genotype. The short variant of 5-HTTLPR has been associated with a 50 % reduction in serotonin uptake. There is a large variation in frequencies of the different 5-HTTLPR genotypes among different ethnicities as the s/s genotype frequency varies from 22–28 % in Caucasians to 56–60 % in Asians [67, 68]. We were unable to identify any studies on the analgesic effect of tramadol in relation to the different genotypes in humans.
Tramadol can cause nausea, which in some cases is treated with ondansetron, a 5-HT3 receptor antagonist. Part of the analgesic effect depends on increased serotonin levels and receptor activation, and consequently the hypothesis is that ondansetron would attenuate the analgesic effect. In a study including 179 abdominal surgery patients, there were no differences in the analgesic effect among the three groups (placebo, metoclopramide or ondansetron). Instead, it was concluded that ondansetron is very effective in treating tramadol-induced nausea and vomiting [69].
3.1.2.4 The Norepinephrine Transporter (NET)
NET belongs to the solute carrier transporter family, just like SERT, and is designated SLC6A2. It is responsible for transporting 90 % of released norepinephrine back into the presynaptic neurons for recycling. Several polymorphisms have been detected, while −182C>T (rs2242446), a point mutation located in the promoter region, and 1287G>A (rs5569), a silent mutation, are the most researched [70].
A study in bovine adrenal medullary cells showed that tramadol inhibits NET function at the same binding site as desipramine [71]. No studies have been located on possible polymorphisms to that binding site and possible effects on the plasma concentration of tramadol and M1.
3.1.2.5 Clinical Significance of Genetic Variants in Transporter Proteins
Currently, the existing evidence does not support a clinically important impact of genetic variants in transporter proteins. OCT1 might have a minor enhancing effect on the exposure of M1, but life-threatening side effects did not occur like in CYP2D6 UMs. SERT and NET polymorphisms might diminish the analgesic effect, but never completely remove it.
3.1.3 Opioid Receptor Genes
Downstream signaling from opioid receptor-ligand coupling is transmitted through G-proteins that inhibit the adenylate cyclase, activate inwardly rectifying K+ currents or inhibit voltage-dependent Ca2+ channels [9].
3.1.3.1 OPRM1
The opioid μ-receptor is coded by the OPRM1 gene and a well-known polymorphism substitute adenine with guanine in position 118 (A118G) (rs1799971). This leads to a possible altered function, causing a decreased efficacy of morphine and a significant increase in morphine and tramadol requirements in patients with at least one 118G allele [72]. Patients with an 118G allele in their genotype scored higher on the visual analog scale (VAS) for pain postoperatively than the patients homozygous for the wild-type 118A allele [73]. An association has been shown between the homozygous 118A genotype and increased frequency and severity of the adverse events of tramadol (nausea and vomiting) [74]. In a study of 250 Han Chinese subjects, among whom 150 were genotyped for A118G variants, no association between the different polymorphisms and the efficacy of tramadol was found [64].
3.1.3.2 Clinical Significance of Genetic Variants in the Opioid Receptor Gene
The available evidence does not suggest a clinically relevant impact of genetic variants in the OPRM1 gene.
3.1.4 Population Pharmacokinetics
Two population pharmacokinetic studies were identified that included genomic variants, discussed in this paper, as covariates. The first study reported data pooled from 298 humans. The data included concentrations of tramadol and M1, age, weight, sex, disease state and CYP2D6 genotype status as covariates. The standard non-linear mixed effect modelling suggested that the poor CYP2D6 metabolizing phenotype was associated with a 75 % reduction in the formation clearance of the M1 metabolite [75]. The second study developed a theoretical mathematical model for elimination of tramadol related to CYP2D6 genotype classification. The model’s prediction was compared with actual results from a small pharmacokinetic study of intravenous administration of tramadol in 16 healthy volunteers. The study only included data on dose, concentrations of tramadol and M1, and CYP2D6 genotype status. The model predicted approximately a twofold difference in elimination rate between poor and extensive metabolizers, which was in reasonable agreement with the observations from the clinical trial [76].
4 Conclusion
Several aspects of the pharmacogenomics of tramadol have been researched, but only the impact of CYP2D6 polymorphisms on the pharmacokinetics and pharmacodynamics of tramadol are well established. Depending on ethnicity of the patient, relevant genotyping may improve the outcome of tramadol treatment in pain management. Such a clinical approach awaits randomized controlled trials in relevant patient groups using a priori CYP2D6 phenotype classification as an intervention.
References
Grond S, Sablotzki A. Clinical pharmacology of tramadol. Clin Pharmacokinet. 2004;43:879–923.
Kizilbash A, Ngô-Minh CT. Review of extended-release formulations of tramadol for the management of chronic non-cancer pain: focus on marketed formulations. J Pain Res. 2014;7:149–61. doi:10.2147/JPR.S49502.
Pedersen RS, Damkier P, Brosen K. Tramadol as a new probe for cytochrome P450 2D6 phenotyping: a population study. Clin Pharmacol Ther. 2005;77:458–67. doi:10.1016/j.clpt.2005.01.014.
Cicero TJ, Adams EH, Geller A, et al. A postmarketing surveillance program to monitor Ultram (tramadol hydrochloride) abuse in the United States. Drug Alcohol Depend. 1999;57:7–22.
Danish Health and Medicines Authority. Summary of product characteristics: tramadol. Danish Health and Medicines Authority. 2015. http://www.produktresume.dk/docushare/dsweb/View/Collection-116.
Sindrup SH, Andersen G, Madsen C, et al. Tramadol relieves pain and allodynia in polyneuropathy: a randomised, double-blind, controlled trial. Pain. 1999;83:85–90.
Gong L, Stamer UM, Tzvetkov MV, et al. PharmGKB summary: tramadol pathway. Pharmacogenet Genomics 2014.
Bastami S, Haage P, Kronstrand R, et al. Pharmacogenetic aspects of tramadol pharmacokinetics and pharmacodynamics after a single oral dose. Forensic Sci Int. 2014;238:125–32. doi:10.1016/j.forsciint.2014.03.003.
Gillen C, Haurand M, Kobelt DJ, Wnendt S. Affinity, potency and efficacy of tramadol and its metabolites at the cloned human mu-opioid receptor. Naunyn Schmiedebergs Arch Pharmacol. 2000;362:116–21.
Fliegert F, Kurth B, Gohler K. The effects of tramadol on static and dynamic pupillometry in healthy subjects: the relationship between pharmacodynamics, pharmacokinetics and CYP2D6 metaboliser status. Eur J Clin Pharmacol. 2005;61:257–66. doi:10.1007/s00228-005-0920-y.
Slanar O, Nobilis M, Kvetina J, et al. Miotic action of tramadol is determined by CYP2D6 genotype. Physiol Res Acad Sci Bohemoslov. 2007;56:129–36.
Matouskova O, Slanar O, Chytil L, Perlik F. Pupillometry in healthy volunteers as a biomarker of tramadol efficacy. J Clin Pharm Ther. 2011;36:513–7. doi:10.1111/j.1365-2710.2010.01203.x.
Stoops WW, Lofwall MR, Nuzzo PA, et al. Pharmacodynamic profile of tramadol in humans: influence of naltrexone pretreatment. Psychopharmacology (Berl). 2012;223:427–38. doi:10.1007/s00213-012-2739-4.
Minami K, Uezono Y, Ueta Y. Pharmacological aspects of the effects of tramadol on G-protein coupled receptors. J Pharmacol Sci. 2007;103:253–60.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–9. doi:10.7326/0003-4819-151-4-200908180-00135.
Garcia-Quetglas E, Azanza JR, Sadaba B, et al. Pharmacokinetics of tramadol enantiomers and their respective phase I metabolites in relation to CYP2D6 phenotype. Pharmacol Res Off J Ital Pharmacol Soc. 2007;55:122–30. doi:10.1016/j.phrs.2006.11.003.
Zhou S-F. Polymorphism of human cytochrome P450 2D6 and its clinical significance: part I. Clin Pharmacokinet. 2009;48:689–723. doi:10.2165/11318030-000000000-00000.
Borlak J, Hermann R, Erb K, Thum T. A rapid and simple CYP2D6 genotyping assay: case study with the analgetic tramadol. Metabolism. 2003;52:1439–43.
Hicks JK, Swen JJ, Gaedigk A. Challenges in CYP2D6 phenotype assignment from genotype data: a critical assessment and call for standardization. Curr Drug Metab. 2014;15:218–32.
Gaedigk A, Simon SD, Pearce RE, et al. The CYP2D6 activity score: translating genotype information into a qualitative measure of phenotype. Clin Pharmacol Ther. 2008;83:234–42. doi:10.1038/sj.clpt.6100406.
Kirchheiner J. CYP2D6 phenotype prediction from genotype: which system is the best? Clin Pharmacol Ther. 2008;83:225–7. doi:10.1038/sj.clpt.6100455.
CYP2D6. In: PharmGKB. http://www.pharmgkb.org/gene/PA128. Accessed 17 Feb 2015.
Human cytochrome P450 (CYP) Allele Nomenclature Committee. http://www.cypalleles.ki.se/. Accessed 19 Jan 2015.
Paar WD, Frankus P, Dengler HJ. The metabolism of tramadol by human liver microsomes. Clin Investig. 1992;70:708–10.
Laugesen S, Enggaard TP, Pedersen RS, et al. Paroxetine, a cytochrome P450 2D6 inhibitor, diminishes the stereoselective O-demethylation and reduces the hypoalgesic effect of tramadol. Clin Pharmacol Ther. 2005;77:312–23.
Nielsen AG, Pedersen RS, Noehr-Jensen L, et al. Two separate dose-dependent effects of paroxetine: mydriasis and inhibition of tramadol’s O-demethylation via CYP2D6. Eur J Clin Pharmacol. 2010;66:655–60. doi:10.1007/s00228-010-0803-8.
Noehr-Jensen L, Zwisler ST, Larsen F, et al. Escitalopram is a weak inhibitor of the CYP2D6-catalyzed O-demethylation of (+)-tramadol but does not reduce the hypoalgesic effect in experimental pain. Clin Pharmacol Ther. 2009;86:626–33. doi:10.1038/clpt.2009.154.
Coller JK, Michalakas JR, James HM, et al. Inhibition of CYP2D6-mediated tramadol O-demethylation in methadone but not buprenorphine maintenance patients. Br J Clin Pharmacol. 2012;74:835–41. doi:10.1111/j.1365-2125.2012.04256.x.
Hedenmalm K, Lindh JD, Sawe J, Rane A. Increased liability of tramadol-warfarin interaction in individuals with mutations in the cytochrome P450 2D6 gene. Eur J Clin Pharmacol. 2004;60:369–72. doi:10.1007/s00228-004-0783-7.
Poulsen L, Arendt-Nielsen L, Brøsen K, Sindrup SH. The hypoalgesic effect of tramadol in relation to CYP2D6. Clin Pharmacol Ther. 1996;60:636–44. doi:10.1016/S0009-9236(96)90211-8.
Pedersen RS, Damkier P, Brøsen K. Enantioselective pharmacokinetics of tramadol in CYP2D6 extensive and poor metabolizers. Eur J Clin Pharmacol. 2006;62:513–21. doi:10.1007/s00228-006-0135-x.
Enggaard TP, Poulsen L, Arendt-Nielsen L, et al. The analgesic effect of tramadol after intravenous injection in healthy volunteers in relation to CYP2D6. Anesth Analg. 2006;102:146–50. doi:10.1213/01.ane.0000189613.61910.32.
Stamer UM, Musshoff F, Kobilay M, et al. Concentrations of tramadol and O-desmethyltramadol enantiomers in different CYP2D6 genotypes. Clin Pharmacol Ther. 2007;82:41–7. doi:10.1038/sj.clpt.6100152.
Halling J, Weihe P, Brosen K. CYP2D6 polymorphism in relation to tramadol metabolism: a study of faroese patients. Ther Drug Monit. 2008;30:271–5. doi:10.1097/FTD.0b013e3181666b2f.
Levo A, Koski A, Ojanpera I, et al. Post-mortem SNP analysis of CYP2D6 gene reveals correlation between genotype and opioid drug (tramadol) metabolite ratios in blood. Forensic Sci Int. 2003;135:9–15.
Paar WD, Poche S, Gerloff J, Dengler HJ. Polymorphic CYP2D6 mediates O-demethylation of the opioid analgesic tramadol. Eur J Clin Pharmacol. 1997;53:235–9.
Stamer UM, Lehnen K, Hothker F, et al. Impact of CYP2D6 genotype on postoperative tramadol analgesia. Pain. 2003;105:231–8.
Sindrup SH, Madsen C, Brøsen K, Jensen TS. The effect of tramadol in painful polyneuropathy in relation to serum drug and metabolite levels. Clin Pharmacol Ther. 1999;66:636–41. doi:10.1053/cp.1999.v66.103171001.
Stamer UM, Stuber F, Muders T, Musshoff F. Respiratory depression with tramadol in a patient with renal impairment and CYP2D6 gene duplication. Anesth Analg. 2008;107:926–9. doi:10.1213/ane.0b013e31817b796e.
Elkalioubie A, Allorge D, Robriquet L, et al. Near-fatal tramadol cardiotoxicity in a CYP2D6 ultrarapid metabolizer. Eur J Clin Pharmacol. 2011;67:855–8. doi:10.1007/s00228-011-1080-x.
Wang G, Zhang H, He F, Fang X. Effect of the CYP2D6*10 C188T polymorphism on postoperative tramadol analgesia in a Chinese population. Eur J Clin Pharmacol. 2006;62:927–31. doi:10.1007/s00228-006-0191-2.
Shen H, He MM, Liu H, et al. Comparative metabolic capabilities and inhibitory profiles of CYP2D6.1, CYP2D6.10, and CYP2D6.17. Drug Metab Dispos Biol Fate Chem. 2007;35:1292–300. doi:10.1124/dmd.107.015354.
Gan SH, Ismail R, Wan Adnan WA, Wan Z. Correlation of tramadol pharmacokinetics and CYP2D6*10 genotype in Malaysian subjects. J Pharm Biomed Anal. 2002;30:189–95.
Li Q, Wang R, Guo Y, et al. Relationship of CYP2D6 genetic polymorphisms and the pharmacokinetics of tramadol in Chinese volunteers. J Clin Pharm Ther. 2010;35:239–47. doi:10.1111/j.1365-2710.2009.01102.x.
Xu J, Zhang X-C, Lv X-Q, et al. Effect of the cytochrome P450 2D6*10 genotype on the pharmacokinetics of tramadol in post-operative patients. Pharm. 2014;69:138–41.
Nasare NV, Banerjee BD, Suryakantrao Deshmukh P, et al. CYP2D6*2 polymorphism as a predictor of failed outpatient tramadol therapy in postherpetic neuralgia patients. Am J Ther. 2013. doi:10.1097/MJT.0b013e31826fc491.
Kirchheiner J, Keulen J-THA, Bauer S, et al. Effects of the CYP2D6 gene duplication on the pharmacokinetics and pharmacodynamics of tramadol. J Clin Psychopharmacol. 2008. doi:10.1097/JCP.0b013e318160f827.
Allegaert K, Rochette A, Veyckemans F. Developmental pharmacology of tramadol during infancy: ontogeny, pharmacogenetics and elimination clearance. Paediatr Anaesth. 2011;21:266–73. doi:10.1111/j.1460-9592.2010.03389.x.
Allegaert K, Anderson BJ, Verbesselt R, et al. Tramadol disposition in the very young: an attempt to assess in vivo cytochrome. Br J Anaesth. 2005;95:231–9. doi:10.1093/bja/aei170.
Allegaert K, Van den Anker JN, Verbesselt R, et al. O-Demethylation of tramadol in the first months of life. Eur J Clin Pharmacol. 2005;61:837–42. doi:10.1007/s00228-005-0045-3.
Allegaert K, van den Anker JN, de Hoon JN, et al. Covariates of tramadol disposition in the first months of life. Br J Anaesth. 2008;100:525–32. doi:10.1093/bja/aen019.
Allegaert K, van Schaik RHN, Vermeersch S, et al. Postmenstrual age and CYP2D6 polymorphisms determine tramadol o-demethylation in critically ill neonates and infants. Pediatr Res. 2008;63:674–9. doi:10.1203/PDR.0b013e31816ff712.
Subrahmanyam V, Renwick AB, Walters DG, et al. Identification of cytochrome P-450 isoforms responsible for cis-tramadol metabolism in human liver microsomes. Drug Metab Dispos Biol Fate Chem. 2001;29:1146–55.
Werk AN, Cascorbi I. Functional gene variants of CYP3A4. Clin Pharmacol Ther. 2014;96:340–8. doi:10.1038/clpt.2014.129.
McGraw J, Waller D. Cytochrome P450 variations in different ethnic populations. Expert Opin Drug Metab Toxicol. 2012;8:371–82. doi:10.1517/17425255.2012.657626.
Hagelberg NM, Saarikoski T, Saari TI, et al. Ticlopidine inhibits both O-demethylation and renal clearance of tramadol, increasing the exposure to it, but itraconazole has no marked effect on the ticlopidine-tramadol interaction. Eur J Clin Pharmacol. 2013;69:867–75. doi:10.1007/s00228-012-1433-0.
Lehtonen P, Sten T, Aitio O, et al. Glucuronidation of racemic O-desmethyltramadol, the active metabolite of tramadol. Eur J Pharm Sci Off J Eur Fed Pharm Sci. 2010;41:523–30. doi:10.1016/j.ejps.2010.08.005.
Bhasker CR, McKinnon W, Stone A, et al. Genetic polymorphism of UDP-glucuronosyltransferase 2B7 (UGT2B7) at amino acid 268: ethnic diversity of alleles and potential clinical significance. Pharmacogenetics. 2000;10:679–85.
Tzvetkov MV, Saadatmand AR, Lötsch J, et al. Genetically polymorphic OCT1: another piece in the puzzle of the variable pharmacokinetics and pharmacodynamics of the opioidergic drug tramadol. Clin Pharmacol Ther. 2011;90:143–50. doi:10.1038/clpt.2011.56.
Ameyaw MM, Regateiro F, Li T, et al. MDR1 pharmacogenetics: frequency of the C3435T mutation in exon 26 is significantly influenced by ethnicity. Pharmacogenetics. 2001;11:217–21.
Kanaan M, Daali Y, Dayer P, Desmeules J. Uptake/efflux transport of tramadol enantiomers and O-desmethyl-tramadol: focus on P-glycoprotein. Basic Clin Pharmacol Toxicol. 2009;105:199–206. doi:10.1111/j.1742-7843.2009.00428.x.
Slanar O, Nobilis M, Kvetina J, et al. Pharmacokinetics of tramadol is affected by MDR1 polymorphism C3435T. Eur J Clin Pharmacol. 2007;63:419–21. doi:10.1007/s00228-006-0255-3.
Slanar O, Dupal P, Matouskova O, et al. Tramadol efficacy in patients with postoperative pain in relation to CYP2D6 and MDR1 polymorphisms. Bratisl Lekárske Listy. 2012;113:152–5.
Zhao Q, Sun J, Tao Y, et al. A logistic equation to determine the validity of tramadol from related gene polymorphisms and psychological factors. Pharmacogenomics. 2014;15:487–95. doi:10.2217/pgs.14.22.
Enabah D, El Baz H, Moselhy H. Higher frequency of C.3435 of the ABCB1 gene in patients with tramadol dependence disorder. Am J Drug Alcohol Abuse. 2014;40:317–20. doi:10.3109/00952990.2014.925468.
Fox MA, Jensen CL, Murphy DL. Tramadol and another atypical opioid meperidine have exaggerated serotonin syndrome behavioural effects, but decreased analgesic effects, in genetically deficient serotonin transporter (SERT) mice. Int J Neuropsychopharmacol Off Sci J Coll Int Neuropsychopharmacol CINP. 2009;12:1055–65. doi:10.1017/S146114570900011X.
Noskova T, Pivac N, Nedic G, et al. Ethnic differences in the serotonin transporter polymorphism (5-HTTLPR) in several European populations. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32:1735–9. doi:10.1016/j.pnpbp.2008.07.012.
Ng CH, Easteal S, Tan S, et al. Serotonin transporter polymorphisms and clinical response to sertraline across ethnicities. Prog Neuropsychopharmacol Biol Psychiatry. 2006;30:953–7. doi:10.1016/j.pnpbp.2006.02.015.
Rauers NI, Stuber F, Lee E-H, et al. Antagonistic effects of ondansetron and tramadol? A randomized placebo and active drug controlled study. J Pain Off J Am Pain Soc. 2010;11:1274–81. doi:10.1016/j.jpain.2010.03.003.
Zhao X, Huang Y, Ma H, et al. Association between major depressive disorder and the norepinephrine transporter polymorphisms T-182C and G1287A: a meta-analysis. J Affect Disord. 2013;150:23–8. doi:10.1016/j.jad.2013.03.016.
Sagata K, Minami K, Yanagihara N, et al. Tramadol inhibits norepinephrine transporter function at desipramine-binding sites in cultured bovine adrenal medullary cells. Anesth Analg. 2002;94:901–6 (table of contents).
Liu Y-C, Wang W-S. Human mu-opioid receptor gene A118G polymorphism predicts the efficacy of tramadol/acetaminophen combination tablets (ultracet) in oxaliplatin-induced painful neuropathy. Cancer. 2012;118:1718–25. doi:10.1002/cncr.26430.
De Capraris A, Cinnella G, Marolla A, et al. Micro opioid receptor A118G polymorphism and post-operative pain: opioids’ effects on heterozygous patients. Int J Immunopathol Pharmacol. 2011;24:993–1004.
Kim E, Choi C-B, Kang C, Bae S-C. Adverse events in analgesic treatment with tramadol associated with CYP2D6 extensive-metaboliser and OPRM1 high-expression variants. Ann Rheum Dis. 2010;69:1889–90. doi:10.1136/ard.2009.124347.
Allegaert K, Holford N, Anderson BJ, et al. Tramadol and O-desmethyl tramadol clearance maturation and disposition in humans: a pooled pharmacokinetic study. Clin Pharmacokinet. 2014. doi:10.1007/s40262-014-0191-9.
Di Patti F, Fanelli D, Pedersen RS, et al. Modelling the pharmacokinetics of tramadol: on the difference between CYP2D6 extensive and poor metabolizers. J Theor Biol. 2008;254:568–74. doi:10.1016/j.jtbi.2008.06.005.
Acknowledgments
We thank the research librarian Johan Wallin for his support and advice in the literature research.
Conflict of interest
DL, PD and KB report no conflict of interest. No sources of funding were used in the preparation of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lassen, D., Damkier, P. & Brøsen, K. The Pharmacogenetics of Tramadol. Clin Pharmacokinet 54, 825–836 (2015). https://doi.org/10.1007/s40262-015-0268-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-015-0268-0