Abstract
Background and Objectives
Dual antiplatelet therapy (DAPT) after percutaneous coronary intervention (PCI) reduces the incidence of thrombotic events but increases the risk of bleeding, which is associated with a substantial and durable risk of death and could offset the benefits of a reduction in thrombotic events. P2Y12 inhibitor monotherapy after short-term DAPT could be an option to reduce the risk of bleeding. We carried out a meta-analysis comparing P2Y12 inhibitor monotherapy after short-term DAPT with standard-term DAPT in patients undergoing PCI.
Methods
We searched the PubMed and EMBASE databases through 11 April 2020. Two authors independently reviewed and selected eligible trials. The DerSimonian–Laird method with the binary random-effects model was used to calculate the relative risk (RR) with 95% confidence interval (CI).
Results
Five trials involving 23,762 patients were included in the final analyses; four were open-label trials, while the TWILIGHT trial was double-blinded. Ticagrelor was used in three trials, and the other two trials included several P2Y12 inhibitors. P2Y12 inhibitor monotherapy after short-term DAPT significantly reduced the bleeding events, defined as Bleeding Academic Research Consortium (BARC) type 3 or 5 bleeding and Thrombolysis in Myocardial Infarction (TIMI) major or minor bleeding, by 39% (RR 0.61, 95% CI 0.38–0.99; p = 0.045) and 46% (RR 0.56, 95% CI 0.42–0.73; p < 0.001), respectively. A significant reduction in cardiovascular death was associated with P2Y12 inhibitor monotherapy after short-term DAPT (RR 0.75, 95% CI 0.58–0.98; p = 0.037; I2 = 0). No significant difference in all-cause mortality, myocardial infarction, stroke, or definite or probable stent thrombosis was observed.
Conclusions
This meta-analysis showed a significantly lowered risk of major bleeding and similar benefits of P2Y12 inhibitor monotherapy after short-term DAPT compared with standard-term DAPT in patients undergoing PCI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Compared with the standard-term dual antiplatelet therapy (DAPT), P2Y12 inhibitor monotherapy after short-term DAPT significantly reduced the bleeding events, defined as Bleeding Academic Research Consortium (BARC) type 3 or 5 bleeding and Thrombolysis in Myocardial Infarction (TIMI) major or minor bleeding, in patients undergoing PCI. |
P2Y12 inhibitor monotherapy after short-term DAPT also significantly reduced the incidence of cardiovascular death in patients undergoing PCI. |
Further large randomized trials are warranted to establish this novel approach. |
1 Introduction
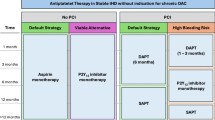
Dual antiplatelet therapy (DAPT) has been widely used in patients undergoing percutaneous coronary intervention (PCI) to prevent thrombotic events. Although the optimal duration of DAPT is still controversial, current guidelines recommend the use of DAPT for at least 6 months for patients with stable ischemic heart disease and 12 months for patients with acute coronary syndrome [1]; however, long-term use of DAPT may potentially increase the risk of bleeding. Severe bleeding has been reported in patients chronically taking DAPT and offset the ischemic benefits of DAPT [2, 3]. It is imperative to develop novel antiplatelet strategies that maintain efficacy for ischemic events while reducing the bleeding risk after PCI. Various approaches have been investigated in the past, and, among them, a short duration of DAPT followed by P2Y12 inhibitor monotherapy has recently been reported to maintain the same therapeutic effects but with less risk of bleeding. Several meta-analysis studies have been conducted on this topic but they have some limitations that will be discussed later. In this study, we conducted a contemporary meta-analysis to summarize the clinical findings from the trials comparing the use of short-term DAPT followed by P2Y12 inhibitor monotherapy versus standard-term DAPT.
2 Methods
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines for reporting the present meta-analysis. The PUBMED (1966–) and EMBASE (1980–) databases were searched through 11 April 2020 using web-based search engines for all clinical studies comparing P2Y12 inhibitor monotherapy after an abbreviated DAPT, with DAPT. The search was conducted using the following keywords: ‘P2Y12 inhibitor’, ‘ticagrelor’, ‘clopidogrel’, ‘prasugrel’, ‘percutaneous coronary intervention’, ‘stent’, ‘stenting’, ‘aspirin’, and ‘dual antiplatelet therapy’ (see electronic supplementary Table S1). Relevant studies were identified through a manual search of secondary sources, including references of initially identified articles, reviews, and commentaries. The references of any previous meta-analyses were reviewed for any articles not included in the main database search. The abstracts from major cardiovascular conferences were screened within the past year. Duplications were automatically removed using Endnote and Rayyan.
Two authors independently assessed the search results for eligibility, by title and/or abstract, using Rayyan. Differences were resolved through consensus between authors. Studies that met the following criteria were included in the meta-analysis: (1) compared standard-term DAPT with abbreviated DAPT followed by P2Y12 inhibitor monotherapy; (2) patients received PCI; and (3) reported the outcomes of interest, including bleeding and cardiovascular events. The included articles were restricted to the English language.
The primary endpoint was major bleeding events, while secondary outcomes included myocardial infarction (MI), stroke, cardiovascular death, all-cause death, and definite or probable stent thrombosis. Information regarding the study design, demographic characteristics, and various outcomes were extracted and assessed. The Cochrane Collaboration’s tool for assessing the risk of bias was used to evaluate the quality of the included trials.
The binary random-effects model with the DerSimonian–Laird method was adopted for the calculation of relative risk (RR) for each outcome of interest. The I2 statistic test was used for assessment of in-between study heterogeneity, with values < 25%, 25–50%, 50–75%, and > 75% corresponding to no, low, moderate, and high degrees of heterogeneity, respectively. We used a confidence interval (CI) of 95% and a p value < 0.05 as a reflection of statistically significant results in all our analyses. All analyses were conducted using OpenMeta[Analyst] software [4] and Review Manager 5.3.
3 Results
A total of 1074 records were identified from the PUBMED and EMBASE databases (see electronic supplementary Fig. S1) After removing duplicates, 932 records were screened by authors based on titles and abstracts. Full texts of seven articles were examined, with two additional articles identified through relevant articles (GLASSY and TICO) [5, 6]. Ultimately, a total of five studies including 23,762 patients were included in this meta-analysis (GLASSY, TWILIGHT, STOPDAPT-2, SMARTCHOICE, and TICO) [5, 7,8,9,10]. The results of the TICO trial were recently presented at the American College of Cardiology’s 69th Annual Scientific Session and Expo/World Heart Federation's World Congress of Cardiology; full-text had not been published at the time of writing. The GLASSY trial, a prespecified ancillary study of the GLOBAL LEADERS trial [11], examined centrally adjudicated outcomes rather than investigator-reported events, which may be associated with the detection bias. Unlike other included trials, the follow-up period of the GLOBAL LEADERS trial was 24 months instead of 12 months. To reduce the heterogeneity between studies and the potential detection bias, our meta-analysis only included the data collected from the GLASSY trial at the end of 12 months. Details of the baseline characteristics and clinical presentations are shown in Tables 1 and 2. The risk of bias of the included trials was generally low (see electronic supplementary Fig. S2); publication bias was not conducted due to the small number of trials included.
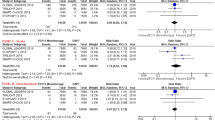
In the included trials, the bleeding outcomes were reported as BARC type 3 or 5 bleeding or TIMI major or minor bleeding. Compared with standard-term DAPT, short-term DAPT followed by P2Y12 inhibitor monotherapy significantly reduced the risk of BARC type 3 or 5 bleeding and TIMI major or minor bleeding by 39% (RR 0.61, 95% CI 0.38–0.99; p = 0.045) and 46% (RR 0.56, 95% CI 0.42–0.73; p < 0.001), respectively (Fig. 1). No significant difference was identified between the decline in BARC type 3 or 5 bleeding and TIMI major or minor bleeding (p = 0.68). A non-significant low heterogeneity (p = 0.189; I2 = 40%) was observed in the TIMI major or minor bleeding analysis, while a significant moderate heterogeneity (p = 0.016; I2 = 71%) was observed in the BARC 3 or 5 bleeding analysis. The sensitivity analysis found that the heterogeneity became statistically insignificant (p = 0.167) and I2 decreased to 44% when the GLASSY trial was removed. A subgroup analysis based on the P2Y12 inhibitors showed no significant difference in the BARC type 3 or 5 bleeding or TIMI major or minor bleeding between ticagrelor versus mixed P2Y12 inhibitors, with p-values of 0.63 and 0.10, respectively.
Among the secondary outcomes (Fig. 2), a significant reduction in cardiovascular death was associated with short DAPT followed by P2Y12 inhibitor monotherapy (RR 0.75, 95% CI 0.58–0.98; p = 0.037; I2 = 0). This significant reduction in cardiovascular death was not observed in the included individual trials. No other significant differences in all-cause mortality (RR 0.84, 95% CI 0.67–1.04; p = 0.109), MI (RR 0.94, 95% CI 0.78–1.13; p = 0.490), stroke (RR 0.96, 95% CI 0.56–1.64; p = 0.885), or definite or probable stent thrombosis (RR 0.99, 95% CI 0.68–1.43; p = 0.942) was identified. Overall, no significant heterogeneity was found in the analysis of the secondary outcomes.
4 Discussion
Our meta-analysis included five clinical trials with 23,762 patients and was the most comprehensive meta-analysis in this area at the time of writing. The results of our study favored short-term DAPT followed by P2Y12 inhibitor monotherapy versus standard-term DAPT for patients undergoing PCI. Furthermore, the major bleeding events analyzed in our meta-analysis included not only BARC type 3 or 5 bleeding but also TIMI major or minor bleeding. No significant differences in the major bleeding events were identified between P2Y12 inhibitors. There was no statistically significant difference in most secondary outcomes analyzed, including all-cause mortality, MI, stroke, and definite or probable stent thrombosis; however, a significant reduction in cardiovascular death, which has not been previously reported, was found in the patients receiving P2Y12 inhibitor monotherapy after short-term DAPT. Overall, the short-term DAPT followed by P2Y12 inhibitor monotherapy resulted in a lowered risk of bleeding while preserving ischemic benefits that were as good, if not better.
To the best of our knowledge, our meta-analysis was the first to report a significant decline in cardiovascular death in a cohort receiving P2Y12 inhibitor monotherapy after short-term DAPT compared with standard-term DAPT. Of note, the changes in cardiovascular death were not statistically significant among the included trials, perhaps due to insufficient power. The heterogeneity analysis showed a low risk of heterogeneity (p = 0.97; I2 = 0), indicating a consistent trend among all included trials. Cardiovascular death generally includes deaths that result from an acute MI, sudden cardiac death, heart failure, stroke, cardiovascular procedures, cardiovascular hemorrhage, and death due to other cardiovascular causes. Although it is difficult to differentiate the cause of the decline in cardiovascular death with limited information, we suspect that the decline in cardiovascular death may be driven by the reduction in the major bleeding events, in light of no significant changes in MI, stroke, or definite or probable stent thrombosis. Post-PCI bleeding was reported to be significantly associated with an increased mortality rate [12]. In our meta-analysis, major bleeding events were significantly reduced by the novel antiplatelet strategy; however, whether the reduction in the major bleeding events causes the decline in cardiovascular death needs further investigation.
The included trials shared a similar study design, although some slight differences existed in the duration of short-term DAPT, study populations, locations, DAPT regimens, follow-up terms, and the levels of blinding. Past medical history varied among the included trials, with the TWILIGHT trial having the most number of patients with previous MI and PCI, and the TICO trial having the least number of patients with previous MI and PCI. Most clinical presentations among participants in the included trials were comparable, including the percentage of second-generation drug-eluting stents, the location of lesions, radial artery access, and stent length per patient; however, indications for PCI were clinically different among trials. For example, the TWILIGHT trial excluded patients with ST-elevation myocardial infarction (STEMI); the TICO trial included 36% of patients with STEMI but excluded patients with stable coronary artery disease; and the STOPDAPT-2 trial included 62% of patients with stable coronary artery disease. Nevertheless, the primary and secondary clinical outcomes of these three trials showed similar trends in favoring the novel antiplatelet strategy; therefore, it is unclear how various clinical characteristics affected clinical outcomes.
A sensitivity analysis of the primary endpoint revealed that the heterogeneity in the meta-analysis of BARC 3 or 5 bleeding was majorly introduced by the GLASSY trial, in which the rate of BARC 3 or 5 bleeding in the intervention group was slightly higher than the control group at 30 days (37 vs. 24; RR 1.54, 95% CI 0.92–2.58; p = 0.095). Both groups received DAPT but with different regimens during the first 30 days after PCI. Specifically, patients in the intervention group received low-dose aspirin plus 90 mg ticagrelor twice daily, while, in the control group, patients with coronary artery disease received low-dose aspirin plus clopidogrel, and patients with acute coronary syndrome received low-dose aspirin plus 90 mg ticagrelor twice daily. It is unknown if the increased risk of BARC 3 or 5 bleeding was attributed to the different DAPT regimens, but ticagrelor was reported to be associated with a higher rate of major bleeding, including more instances of fatal intracranial bleeding compared with clopidogrel [13]. The elevated risk of intracranial bleeding associated with ticagrelor compared with clopidogrel may offset the benefits provided by the P2Y12 inhibitor monotherapy in reducing the bleeding events. Thus, the non-significance in BARC 3 or 5 bleeding could be explained by the different DAPT regimens carrying distinct bleeding risks.
Three meta-analysis studies have been conducted in this field, however they all have some limitations. The study by Wernly et al. was outdated, with only three trials included [14]; the study by Luo et al. did not include the TICO trial, and their meta-analysis of bleeding risk was conducted using mixed data from BARC type 3 or 5 bleeding and TIMI major or minor bleeding, raising some concerns about the validity of the statistical method [15]; and the study by Kumar et al. also did not include the TICO trial, and the study endpoints did not include the change of cardiovascular death, which was significant in our meta-analysis [16]. All three meta-analysis studies used data from the GLOBAL LEADERS trial, which had a considerably different trial design compared with other included trials. In light of these limitations, there is a need for a contemporary meta-analysis on this topic, performed with sound methodology and procedures. Meanwhile, a strength of our study was that we summarized baseline characteristics as well as clinical presentations for all included trials.
5 Limitations
There are several limitations to our study. First, there were some variations in the length of the initial DAPT therapy before the P2Y12 inhibitor monotherapy in the intervention group of these studies, and in the total length of the study. For TWILIGHT and SMART-CHOICE, the initial DAPT therapy was for 3 months, before switching to P2Y12 inhibitor monotherapy, whereas in STOPDAPT-2 and GLASSY, the initial DAPT therapy was for 1 month only. Although we only included the 12-month data from GLASSY instead of analyzing the full 24 months of data to give consistency in the time frame analyzed, the duration of TWILIGHT was 15 months as there was an initial 3-month period of DAPT treatment to ensure no major bleeding or ischemic events occurred before randomization into the 12-month treatment period. Second, as previously mentioned, variations exist in the selected P2Y12 inhibitors in the different studies,and even among the intervention and control groups of the studies. Third, the results of this study may not be generalizable to patients with complicated and high-risk PCI as only the TWILIGHT study included such a patient population, where there were lower major bleeding rates and no differences in death, MI, or stroke in the P2Y12 inhibitor monotherapy after 3 months of DAPT group. In contrast to TWILIGHT, Subhaharan et al. performed a systematic review and meta-analysis of patients with complex PCI and found that prolonged DAPT therapy (> 12 months) reduced cardiac mortality and major cardiovascular adverse events, with an increased major bleeding rate in comparison to a shorter duration of DAPT (3–12 months) [17]. Although this was a conflicting result, the authors’ definition of complex PCIs or high risk is not consistent and there is currently no guideline-directed definition of such groups of patients.
6 Conclusions
Our study showed that short-term DAPT followed by P2Y12 inhibitor monotherapy for 12 months was associated with a lower risk of major bleeding without sacrifice of ischemic benefits in patients undergoing PCI compared with standard-term DAPT. An additional benefit in reducing cardiovascular death was also observed for the first time. No difference in all-cause mortality, MI, stroke, and definite or probable stent thrombosis was identified in our meta-analysis, suggesting the preserved ischemic benefits of this novel antiplatelet strategy. The positive results of our meta-analysis add insight to the role of P2Y12 inhibitor monotherapy after short-term DAPT, although further large randomized trials are required to establish this novel approach. The ongoing STOPDAPT-2 ACS trial (NCT03462498) is designed to evaluate the efficacy and safety of reducing the duration of DAPT to 1 month after implantation of the everolimus-eluting cobalt-chromium stent in the setting of acute coronary syndrome [18]. The trial is estimated to be completed in March 2026 and the results will provide more evidence for the role of P2Y12 inhibitor monotherapy after short-term DAPT.
References
Levine GN, Bates ER, Bittl JA, Brindis RG, Fihn SD, Fleisher LA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. J Am Coll Cardiol. 2016;68(10):1082–115.
Mauri L, Kereiakes DJ, Yeh RW, Driscoll-Shempp P, Cutlip DE, Steg PG, et al. Twelve or 30 months of dual antiplatelet therapy after drug-eluting stents. N Engl J Med. 2014;371(23):2155–66.
Toyota T, Shiomi H, Morimoto T, Natsuaki M, Kimura T. Short versus prolonged dual antiplatelet therapy (DAPT) duration after coronary stent implantation: a comparison between the DAPT study and 9 other trials evaluating DAPT duration. PLoS ONE. 2017;12(9):e0174502.
Wallace BC, Dahabreh IJ, Trikalinos TA, Lau J, Trow P, Schmid CH. Closing the gap between methodologists and end-users: R as a computational back-end. J Stat Softw. 2012;49(5):1–15.
Franzone A, McFadden E, Leonardi S, Piccolo R, Vranckx P, Serruys PW, et al. Ticagrelor alone versus dual antiplatelet therapy from 1 month after drug-eluting coronary stenting. J Am Coll Cardiol. 2019;74(18):2223–34.
Kim C, Hong SJ, Shin DH, Kim BK, Ahn CM, Kim JS, et al. Randomized evaluation of ticagrelor monotherapy after 3-month dual-antiplatelet therapy in patients with acute coronary syndrome treated with new-generation sirolimus-eluting stents: TICO trial rationale and design. Am Heart J. 2019;212:45–52.
Mehran R, Baber U, Sharma SK, Cohen DJ, Angiolillo DJ, Briguori C, et al. Ticagrelor with or without aspirin in high-risk patients after PCI. N Engl J Med. 2019;381(21):2032–42.
Watanabe H, Domei T, Morimoto T, Natsuaki M, Shiomi H, Toyota T, et al. Effect of 1-month dual antiplatelet therapy followed by clopidogrel vs 12-month dual antiplatelet therapy on cardiovascular and bleeding events in patients receiving PCI: the STOPDAPT-2 randomized clinical trial. JAMA. 2019;321(24):2414–27.
Hahn J-Y, Song YB, Oh J-H, Chun WJ, Park YH, Jang WJ, et al. Effect of P2Y12 inhibitor monotherapy vs dual antiplatelet therapy on cardiovascular events in patients undergoing percutaneous coronary intervention: the SMART-CHOICE randomized clinical trial. JAMA. 2019;321(24):2428–37.
Jang Y. 410-08-ticagrelor with or without aspirin in acute coronary syndrome after percutaneous coronary intervention. In: ACC20/WCC scientific session. 2020.
Vranckx P, Valgimigli M, Jüni P, Hamm C, Steg PG, Heg D, et al. Ticagrelor plus aspirin for 1 month, followed by ticagrelor monotherapy for 23 months vs aspirin plus clopidogrel or ticagrelor for 12 months, followed by aspirin monotherapy for 12 months after implantation of a drug-eluting stent: a multicentre, open-label, randomised superiority trial. Lancet. 2018;392(10151):940–9.
Chhatriwalla AK, Amin AP, Kennedy KF, House JA, Cohen DJ, Rao SV, et al. Association between bleeding events and in-hospital mortality after percutaneous coronary intervention. JAMA. 2013;309(10):1022–9.
Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, Held C, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361(11):1045–57.
Wernly B, Rezar R, Gurbel P, Jung C. Short-term dual antiplatelet therapy (DAPT) followed by P2Y12 monotherapy versus traditional DAPT in patients undergoing percutaneous coronary intervention: meta-analysis and viewpoint. J Thromb Thrombolysis. 2020;49(1):173–6.
Luo L, Fu M, Li Y, Chen Z, Yu J, Luo J, et al. The efficacy and safety of P2Y12 inhibitor monotherapy in patients after percutaneous coronary intervention. Clin Cardiol. 2020;43(3):235–41.
Kumar A, Shariff M, Doshi R, Vaz IP. Abbreviated dual antiplatelet therapy followed by P2Y12 inhibitor monotherapy versus 12 months’ dual antiplatelet therapy post percutaneous coronary intervention: a systematic review and meta-analysis of randomized controlled trials. Am J Cardiovasc Drugs. 2019. https://doi.org/10.1007/s40256-019-00390-0(Epub 30 Nov 2019).
Subhaharan D, Mridha N, Singh K. Clinical benefits of prolonged dual antiplatelet therapy following complex percutaneous coronary intervention. Coron Artery Dis. 2020;31(3):273–8.
Kyoto University, Graduate School of Medicine. ShorT and OPtimal Duration of Dual AntiPlatelet Therapy-2 study for the patients with ACS. ClinicalTrials.gov. https://www.ClinicalTrials.gov/show/NCT03462498. Accessed 18 Apr 2020.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received to conduct this study.
Conflict of interest
Dr. Egolum serves on the speakers’ bureau for Pfizer. Ai-Chen Ho, Shanea Parker, Jordan Dimmel, Andrew Hawkins, and Hua Ling have no disclosures to declare.
Availability of Data and Material
Not applicable.
Code Availability
Not applicable.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ho, AC., Egolum, U., Parker, S. et al. P2Y12 Inhibitor Monotherapy After a Short Dual Antiplatelet Therapy Versus Standard-Term Dual Antiplatelet Therapy in Patients Undergoing Percutaneous Coronary Intervention: A Contemporary Meta-Analysis. Clin Drug Investig 40, 799–808 (2020). https://doi.org/10.1007/s40261-020-00947-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-020-00947-x