Abstract
Background and Objectives
Levomilnacipran is a serotonin and norepinephrine reuptake inhibitor with balanced potency for the reuptake inhibition of norepinephrine and serotonin, approved in the USA for the treatment of major depressive disorder (MDD) in adults. We conducted studies in healthy human subjects to investigate pharmacokinetic interactions when levomilnacipran extended-release (ER) is administered in combination with an inhibitor (ketoconazole), an inducer (carbamazepine), or a substrate (alprazolam) of cytochrome P450 (CYP) 3A4.
Methods
Randomised, open-label studies were conducted in healthy volunteers (n = 34 ketoconazole, n = 34 carbamazepine, n = 30 alprazolam) and pharmacokinetic parameters were determined when levomilnacipran was administered alone or together with the relevant study drug.
Results
Co-administration of ketoconazole with levomilnacipran ER increased levomilnacipran maximum concentration (C max) by 39 % [90 % confidence interval (CI) 31–47 %] and area under the concentration–time curve (AUC) by 57 % (90 % CI 47–67 %), whereas carbamazepine reduced the C max and AUC of levomilnacipran by 26 % (90 % CI 22–30 %) and 29 % (90 % CI 26–32 %), respectively. Levomilnacipran at steady state had no significant effect on the pharmacokinetics of a single 1 mg dose of alprazolam extended release (XR); neither did single-dose alprazolam XR affect the steady-state pharmacokinetics of levomilnacipran. No new safety concerns were noted in these studies.
Conclusions
Based on these results, the levomilnacipran ER dose should not exceed 80 mg once daily when used with ketoconazole, compared to 120 mg once daily in the absence of ketoconazole. No dose adjustment for levomilnacipran is suggested when levomilnacipran ER is co-administered with carbamazepine or other CYP3A4 inducers. Co-administration with levomilnacipran of drugs metabolised by CYP3A4, such as alprazolam, requires no dose adjustment due to pharmacokinetic considerations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Levomilnacipran exposure was increased by approximately 50 % when it was co-administered with ketoconazole, a strong CYP3A4 inhibitor; a maximum dose of 80 mg of levomilnacipran extended release (ER) is therefore recommended when the drug is used with ketoconazole or other strong CYP3A4 inhibitors, compared to 120 mg once daily in the absence of strong CYP3A4 inhibitors. |
The pharmacokinetics of levomilnacipran were not clinically meaningfully affected by co-administration with carbamazepine, an inducer of CYP3A4; thus, dose adjustments are not required. |
Maximal-dose levomilnacipran at steady state did not affect the pharmacokinetics of single-dose alprazolam extended release (XR), a substrate of CYP3A4; neither did single-dose alprazolam XR affect the steady-state pharmacokinetics of levomilnacipran ER. Thus, dose adjustment is generally not needed based on pharmacokinetic considerations for drugs metabolised by CYP3A4 enzymes when they are co-administered with levomilnacipran ER. |
1 Introduction
Levomilnacipran (1S, 2R-milnacipran; Fetzima®, Forest Laboratories, LLC, St Louis, MO, USA) is a potent and selective serotonin and norepinephrine reuptake inhibitor (SNRI) approved by the US Food and Drug Administration (FDA) for the treatment of major depressive disorder (MDD) in adults. Levomilnacipran has balanced potency for inhibiting the norepinephrine transporter and the serotonin transporter. Conversely, the SNRIs duloxetine and venlafaxine have greater potency for serotonin reuptake inhibition than norepinephrine reuptake inhibition [1, 2]. An extended-release (ER) formulation was developed to facilitate once-daily dosing.
The efficacy and safety of levomilnacipran ER in the treatment of MDD have been evaluated in a large phase II study [3] and four phase III studies [4–7]. Four of these studies showed a statistically significant improvement for levomilnacipran ER on the Montgomery–Åsberg Depression Rating Scale total score compared with placebo [3–6]. A 48-week, open-label, follow-up study [8] examined the longer-term safety and tolerability of levomilnacipran in patients who had completed one of three earlier trials [4, 6, 7]. The results supported the safety and tolerability profile observed during the earlier studies. Post hoc pooled analyses of the five studies indicated that levomilnacipran ER was effective across a wide range of patients with MDD [9] and that functional impairment was significantly improved compared with placebo, regardless of the baseline level of functional impairment [10].
Pharmacokinetic studies of the ER formulation showed that levomilnacipran has a median time to reach maximum drug plasma concentration (t max) of 6–8 h and an apparent terminal elimination half-life (t ½) of 12 h [11, 12]. The pharmacokinetics of levomilnacipran are dose proportional following a single dose of 25–120 mg and multiple doses of 25–300 mg/day. Food does not have a significant effect on the bioavailability of levomilnacipran ER capsules [12].
Levomilnacipran is eliminated primarily by renal excretion; about 58 % of an orally administered dose is excreted unchanged in the urine. The remainder is eliminated by multiple metabolic pathways including glucuronidation, desethylation and p-hydroxylation. Desethylation to form N-desethyl levomilnacipran (also called F17400) is a major metabolic pathway accounting for approximately 18 % of total clearance; none of the other metabolic pathways contributes more than 5 % of total clearance in humans. In vitro studies have shown that, while multiple cytochrome P450 (CYP) enzymes are capable of catalysing this desethylation, CYP3A4 is the primary catalyst [13]. Therefore, there is the potential that levomilnacipran pharmacokinetics may be influenced by CYP3A4 modulators. None of the identified metabolites are pharmacologically active [11].
In vitro studies using validated methods showed that levomilnacipran did not induce CYP 1A2, 2C9, 2C19 or 3A4/5 when tested using freshly isolated human hepatocytes [14]. Nor did it directly inhibit CYP1A2, 2A6, 2C8, 2C9, 2C19, 2D6 or 2E1 in a pooled human liver microsomal system; only CYP3A4/5 was inhibited, with a half-maximal inhibitory concentration (IC50) of >30 µM [15]. As this is about 21-fold higher than the steady-state maximum plasma concentration of 1.4 µM achieved with 120 mg/day [11], the highest recommended therapeutic dose, the potential for levomilnacipran to inhibit CYP3A4/5 is low. Similarly, N-desethyl levomilnacipran did not directly inhibit CYP1A2, 2B6, 2C8, 2C9, 2C19, 2D6 or 3A4/5 at clinically relevant concentrations [16]. No time-dependent or metabolism-dependent inhibition was observed for levomilnacipran or the metabolite at concentrations exceeding those that are clinically relevant. In addition, based on in vitro evaluations, drug transporters of P-glycoprotein—BCRP, OATP1B1, OATP1B3, OAT1, OAT3 or OCT2—have no significant interaction with levomilnacipran at therapeutically relevant concentrations [11]. Thus, the in vitro studies suggested that there is low potential for levomilnacipran to inhibit the metabolism of substrates of CYP3A4.
In order to further evaluate the in vitro findings, three in vivo pharmacokinetic studies were conducted in healthy human subjects to investigate pharmacokinetic interactions when levomilnacipran ER is administered in combination with an inhibitor (ketoconazole), an inducer (carbamazepine) or a substrate (alprazolam) of CYP3A4.
2 Methods
2.1 Study Designs
All three studies were designed in accordance with the FDA guidelines for drug-interaction studies [17]. No concomitant medications were permitted during the studies. Since food has no significant effect on the pharmacokinetics of levomilnacipran, study drugs were administered with a meal to potentially improve tolerability. As food affects the bioavailability of alprazolam, subjects were required to take the drug alone or co-administered with levomilnacipran under fasted conditions. In all three studies, blood samples were collected at appropriate predefined intervals for analysis of the relevant drug concentrations.
2.1.1 Study 1 (Levomilnacipran ER Plus Ketoconazole)
This was a single-centre, randomised, open-label, two-period crossover study of the effects of steady-state ketoconazole on the pharmacokinetics of a single dose of levomilnacipran ER in healthy subjects. Subjects were randomised to one of two treatments (levomilnacipran alone or combined levomilnacipran and ketoconazole) in two sequences as described in Online Resource 1.
2.1.2 Study 2 (Levomilnacipran ER Plus Carbamazepine Extended Release [XR])
This was a single-centre, open-label, fixed-sequence, multiple-dose, four-period study in which subjects received Treatments A (levomilnacipran alone); B (carbamazepine alone); C (combined levomilnacipran and carbamazepine); and D (carbamazepine down-taper) in a fixed order with a washout period between Treatments A and B (Online Resource 2).
2.1.3 Study 3 (Levomilnacipran ER Plus Single-Dose Alprazolam Extended Release [XR])
This was single-centre, randomised, open-label, 2 × 2 crossover study to assess the effect of levomilnacipran ER at steady state on the pharmacokinetics of alprazolam in healthy subjects. Participants were randomised to one of two treatments (alprazolam alone or combined alprazolam and levomilnacipran) in two sequences as described in Online Resource 3.
2.2 Inclusion and exclusion criteria
The studies were conducted in healthy, non-smoking adults aged 18–45 years with a body mass index (BMI) of between 18 and 30 kg/m2, and resting pulse rate of 50–100 beats per minute (bpm). Female participants were required to have a negative pregnancy test at screening and on Day −1, and agreed to use a non-hormonal double-barrier method of contraception during the study period.
Exclusion criteria for all three studies included: known hypersensitivity to study treatments, selective serotonin reuptake inhibitors (SSRIs) or other noradrenergic drugs; clinically significant electrocardiogram (ECG) or laboratory abnormalities; history of alcohol or substance abuse within the past 5 years; positive test for cocaine, methadone, barbiturates, amphetamines, benzodiazepines, alcohol, cannabinoids, opiates, phencyclidine or cotinine; consumption of caffeine or grapefruit-containing products within 48 h or alcohol consumption 72 h before Day 1; concomitant medications (within 14 days) or hormonal drugs (within 30 days) before study; pregnancy or breastfeeding; suicide risk or history of narrow-angle glaucoma. Study 2 had an additional exclusion criterion of Asian ancestry or allele positive for HLA-B* 1502.
Subjects underwent physical examination and clinical laboratory testing prior to receiving study drug(s). All participants provided informed consent at screening. Study protocols were approved and studies overseen by the designated independent Institutional Review Board: Independent Investigational Review Board, Plantation, Florida, USA (Studies 1 and 3) and the PRACS Institute Ltd Institutional Review Board (Study 2). The studies were conducted in compliance with the principles of good clinical practice.
2.3 Bioanalytical Methods
Blood sampling was performed as shown in the Electronic Supplementary Material (Online Resources 1, 2 and 3). Validated liquid chromatography–tandem mass spectrometry (LC-MS/MS) methods were used to measure plasma concentrations of drugs and their metabolites (see Online Resource 4).
2.4 Pharmacokinetic Analyses
Pharmacokinetic parameters were derived from plasma concentrations by non-compartmental analysis using WinNonlin® (Pharsight, Cary, NC) version 5.2.1 (Study 1) or version 6.1 (Studies 2 and 3).
In Study 1 (levomilnacipran and ketoconazole), the pharmacokinetic population comprised all subjects who had evaluable pharmacokinetic parameters in both treatment periods. For levomilnacipran, the following were determined: area under the plasma concentration versus time curve (AUC) from time zero to time t (AUC0–t) and from time zero to infinity (AUC0–∞) (using the linear trapezoidal rule), maximum concentration (C max), t max, t ½, apparent total clearance of drug from plasma after oral administration (CL/F) and apparent volume of distribution at steady state (V SS/F). For N-desethyl levomilnacipran, C max, t max, AUC0–t, AUC0–∞ and t ½ were determined. Log-transformed values for the C max and AUC of levomilnacipran and N-desethyl levomilnacipran for levomilnacipran administered with ketoconazole or alone were compared by means of an analysis-of-variance (ANOVA) model using SAS version 9.1.3 under the UNIX operating system. A general linear model was fitted with sequence, subject within sequence, treatment and period as factors.
In Study 2 (levomilnacipran and carbamazepine XR), the pharmacokinetic population comprised all subjects who had evaluable pharmacokinetic parameters for both treatments in each comparison. The following pharmacokinetic parameters were assessed for levomilnacipran, N-desethyl levomilnacipran, carbamazepine and carbamazepine-10,11-epoxide: AUC during the dosing interval, τ, at steady state (AUC0–τ,SS), C max at steady state (C max,SS), t max at steady state (t max,SS), average plasma drug concentration at steady state (C av,SS), and minimum plasma drug concentrations at steady state (C min,SS). The t ½ of levomilnacipran and N-desethyl levomilnacipran were also determined. Log-transformed values for C max,SS and AUC0–τ,SS of levomilnacipran, N-desethyl levomilnacipran, carbamazepine and carbamazepine-10,11-epoxide for drug in combination or alone were compared by means of ANOVA models using SAS version 9.2 under the Windows operating system. General linear models were fitted with treatment and subject as factors.
In Study 3 (levomilnacipran and alprazolam), the pharmacokinetic population was defined as all subjects who completed the study and had evaluable pharmacokinetic parameters. For levomilnacipran, AUC0–τ, C max,SS, C av,SS, C min,SS and t max,SS, and for alprazolam, C max, AUC0–t, AUC0–∞ (using the linear trapezoidal rule), t max, t ½, CL/F and V z/F (apparent volume of distribution during terminal phase after non-intravenous administration) were determined. The pharmacokinetic parameters C max and AUC (after single or multiple dose, as applicable) were compared between treatments (drug in combination vs. drug alone) using ANOVA. A general linear model with sequence, subject within sequence, treatment and period as factors was fitted to log-transformed values of C max and AUC.
For all three studies, two-sided 90 % confidence intervals (CIs) were constructed for the ratio of least squares (LS) geometric means of C max and the relevant AUC parameters for the relevant drugs administered in combination versus drug alone. The 90 % CI for the LS geometric means ratios of C max and AUC parameters needed to be within 80–125 % in order to conclude that each drug had no effect on the pharmacokinetic parameters of the other drug [18]. T max for the relevant drug alone or in combination with the other was compared using the Wilcoxon signed-rank test.
2.5 Safety
Safety was assessed by means of adverse event (AE) monitoring, clinical laboratory evaluations, vital sign assessments, ECGs, physical examinations and Columbia–Suicide Severity Rating Scale (C-SSRS) results. An AE was “any unfavorable and unintended sign (including an abnormal laboratory finding, for example), symptom, or disease temporally associated with the use of a medicinal product, whether or not considered related to the medicinal product” [19]. AEs were recorded as they were reported spontaneously by the subjects, and subjects were asked about their well-being each time vital signs were taken. AEs were classified as mild, moderate or severe by investigators, based on the following definitions: a mild AE was an annoyance to the subject but did not further hinder baseline functioning; a moderate AE caused the subject some discomfort or interference with normal activities but was not hazardous to health; a severe AE caused the subject to experience severe discomfort or severely limited or prevented normal activities and represented a definite hazard to health.
Participants who took one or more doses of any of the study drugs were included in the safety population. Any AE occurring subsequent to the first dose of study drug was counted as a treatment-emergent AE (TEAE). Incidence tables were compiled for AEs; for other safety parameters, descriptive statistics were calculated.
3 Results
3.1 Study 1 (Levomilnacipran ER and Ketoconazole)
3.1.1 Pharmacokinetics
Thirty-four healthy subjects were enrolled and all completed Study 1. Mean age ± standard deviation (SD) was 38.2 ± 5.9 years; mean BMI 26.1 ± 2.3 kg/m2; 17 participants (50 %) were female; 88.2 % were white and 11.8 % black.
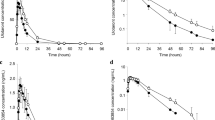
Administration of levomilnacipran ER with ketoconazole resulted in a 57 % increase in both AUC0–t and AUC0–∞ and a 39 % increase in C max of levomilnacipran compared with administration of levomilnacipran ER alone (all statistically significant as indicated by the 90 % CIs for the geometric LS means ratios) (Fig. 1; Table 1). Median t max was delayed for 2 h (p < 0.0001), and clearance reduced from 22 to 14 L/h. T½ was similar for the two treatment arms (Table 1).
Plasma concentrations of a levomilnacipran and b N-desethyl-levomilnacipran versus time following a single-dose administration of 80 mg levomilnacipran ER alone (Treatment A) and in combination with 400 mg ketoconazole at steady state (Treatment B). Pharmacokinetic analysis population (N = 33). Values shown are mean ± standard deviation. ER extended release
For N-desethyl levomilnacipran, AUC0–t and AUC0–∞ were also elevated by approximately 22 and 20 % respectively, following co-administration with steady-state ketoconazole. C max was reduced by 14 % (statistically significant). Median t max was 12 h for both treatments; however, the range of t max was wider, and the mean t max was longer (17.46 vs. 10.94 h), with co-administration (p < 0.0001). Mean t ½ was similar for both treatment arms (Table 1).
3.1.2 Safety Analyses
More TEAEs were reported with co-administration than with levomilnacipran ER alone. The most frequently reported TEAE was headache, reported by 10 subjects with co-administration and none with levomilnacipran ER alone (Table 2). No serious AEs (SAEs) were reported; all TEAEs were considered by the investigator to be mild in intensity.
A small mean increase in creatinine was observed in participants in Sequence I (12.48 μmol/L), which was larger than in Sequence II (1.56 μmol/L). Pulse rate increased by mean (±SD) 9.4 (±10.3) bpm in the safety population, with changes similar between treatments. No other clinically meaningful findings regarding vital signs or ECG parameters were observed; no suicidal ideation or behaviour was reported.
3.2 Study 2 (Levomilnacipran ER Plus Carbamazepine XR)
3.2.1 Pharmacokinetics
Thirty-four healthy subjects were enrolled; eight discontinued prematurely (four due to TEAEs, three due to protocol violations, one withdrew consent). Mean age ± SD was 26.3 ± 6.6 years; mean BMI was 25.1 ± 2.7 kg/m2; 11 participants (32.2 %) were female; 79.4 % were white and 20.6 % black.
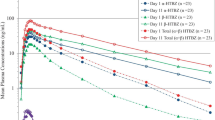
Administration of levomilnacipran ER with carbamazepine XR resulted in a 29 and 26 % decrease in levomilnacipran AUC0–τ and C max,SS, respectively, compared with levomilnacipran ER alone (statistically significant) (Fig. 2; Table 3). The AUC0–τ and C max,SS for N-desethyl levomilnacipran were elevated by 70 and 73 %, respectively, for combined treatment compared with levomilnacipran ER alone (statistically significant) (Table 3).
Plasma concentrations of a levomilnacipran and b N-desethyl levomilnacipran at steady state (levomilnacipran ER 120 mg OD) versus time in the absence and presence of 200 mg BID carbamazepine XR. Pharmacokinetic analysis population (N = 27). Values shown are mean ± standard deviation. BID twice daily, ER extended release, OD once daily, XR extended release
Carbamazepine AUC0–τ and C max,SS were decreased by 2 and 4 %, respectively, when carbamazepine XR and levomilnacipran ER were co-administered (not statistically significant) (Fig. 3; Table 4). AUC0–τ and C max,SS of carbamazepine-10,11-epoxide were increased by 42 and 36 %, respectively (statistically significant).
Plasma concentrations of a carbamazepine and b carbamazepine-10,11-epoxide at steady state (carbamazepine XR 200 mg BID) in the absence and presence of levomilnacipran at steady state (levomilnacipran ER 120 mg OD). Pharmacokinetic analysis population (N = 27). Values shown are mean ± standard deviation. BID twice daily, ER extended release, OD once daily, XR extended release
3.2.2 Safety Analyses
The number of subjects experiencing TEAEs was similar between treatment periods, although there were more TEAEs in the combined treatment period (Treatment C) than levomilnacipran (Treatment A) or carbamazepine treatment (Treatment B) alone (Table 5). All TEAEs were mild or moderate in intensity.
One subject in each treatment group discontinued due to AEs (four in total). This included one 39-year-old male who experienced an SAE [atrial fibrillation (AF)] on Day 11, considered moderate in intensity and related to levomilnacipran administration. The subject recovered from the AF with rapid ventricular response and aberrancy the next day, after withdrawal from the study. Other withdrawals were due to rash (two subjects) and urinary tract obstruction (one subject).
One subject experienced a decrease in weight ≥7 %; no other clinically significant changes in vital signs, clinical laboratory or ECG parameters were observed. No suicidal ideation or behaviour was reported. The combined administration was generally well tolerated, although with a higher frequency of TEAEs than with either drug alone.
3.3 Study 3 (Levomilnacipran ER Plus Single-Dose Alprazolam XR)
3.3.1 Pharmacokinetics
Thirty subjects were enrolled and all completed the study. Mean age ± SD was 36.5 ± 7.4 years; mean BMI ± SD was 26.21 ± 3.01 kg/m2; 12 participants (40 %) were female; 93.3 % were white and 6.7 % black.
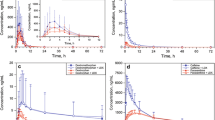
Combined administration did not markedly alter the AUC and C max of alprazolam (Fig. 4; Table 6). Median t max for alprazolam was similar when administered alone or with levomilnacipran (9 vs. 8 h; p = 0.3756).
Plasma concentrations of alprazolam after administration of single-dose alprazolam XR (1 mg) in the absence and presence of levomilnacipran at steady state (levomilnacipran ER 120 mg OD). Pharmacokinetic analysis population (N = 30). Values shown are mean ± standard deviation. ER extended release, OD once daily, XR extended release
Levomilnacipran AUC0–τ, C max,SS and C min,SS were not meaningfully affected by co-administration with single-dose alprazolam (Fig. 5; Table 7). Median t max,SS for levomilnacipran was similar (5 h) in the absence or presence of single-dose alprazolam, but in some subjects individual t max,SS was delayed in the presence of alprazolam (p = 0.0055) (Table 7).
3.3.2 Safety Analyses
There were no premature discontinuations, deaths or SAEs. No suicidal ideation or behaviour was reported. TEAEs reported in two or more patients during the trial are shown in Table 8. The most common TEAE in both treatment groups was somnolence, a known side-effect of alprazolam [20].
Treatment-emergent AEs were reported more frequently with combined administration than with alprazolam XR alone. However, Treatment A was only 1 day in duration while Treatment B was 14 days in duration. All AEs were considered mild, except for one incidence of moderate urinary retention in the combined group.
There were no clinically significant changes in clinical laboratory results, vital signs or ECG parameters except for mean ventricular heart rate, which increased by (mean ± SD) 18.9 ± 10.0 bpm from screening to end of study. Systolic and diastolic blood pressure increased by 3.4 ± 10.4 and 1.0 ± 7.6 mm Hg, respectively. Only two subjects had potentially clinically significant changes in vital signs at any point during the study. One had a high pulse rate of 122 bpm 6 h after dosing with levomilnacipran alone, but 92 bpm (close to predose value) 11 h after dosing. A second subject had a low pulse of 48 bpm at 4 h after dosing with single-dose alprazolam alone, but 64 bpm upon repeat.
4 Discussion
The studies reported here investigated the effects of a known strong CYP3A4 inhibitor (ketoconazole) and a strong CYP3A4 inducer (carbamazepine) on levomilnacipran pharmacokinetics because earlier in vitro results had shown that CYP3A4 is the predominant CYP isozyme involved in the metabolism of levomilnacipran (Forest Laboratories, Data on file, Xenotech Study no XT104114), and therefore the one most susceptible to drug-drug interactions. Additionally, the effect of levomilnacipran on the pharmacokinetics of alprazolam, a CYP3A4 substrate, in healthy adults was investigated. Alprazolam was chosen as the CYP3A4 substrate because it is likely to be co-prescribed with levomilnacipran ER in patients with psychiatric disorders.
Ketoconazole co-administered with levomilnacipran ER in healthy adults had a statistically significant impact on the pharmacokinetics of levomilnacipran, increasing the AUC0–t and AUC0–∞ of levomilnacipran by 57 %, and those of N-desethyl levomilnacipran by about 20 %. C max of levomilnacipran and N-desethyl levomilnacipran increased by 39 and 14 %, respectively, when co-administered with ketoconazole.
N-desethylation, mediated mainly by CYP3A4, contributes to about 18 % of the total clearance of levomilnacipran. The increase in AUC of levomilnacipran resulting from co-administration with ketoconazole is therefore slightly greater than expected if it were assumed that CYP3A4 is solely responsible for the conversion of levomilnacipran to N-desethyl levomilnacipran and that this pathway was completely blocked. Also, the AUC of N-desethyl levomilnacipran was increased by co-administration with ketoconazole, rather than decreased as would be expected, suggesting that besides the inhibition of the CYP3A4 metabolic pathway, other mechanisms may also be involved in this interaction. For example, the delayed levomilnacipran t max in the presence of ketoconazole suggests that ketoconazole may affect absorption of levomilnacipran. Ketoconazole has been reported to affect transporters [21, 22] and renal function [23]; thus, alterations of these functions by ketoconazole may also affect the disposition of both levomilnacipran and N-desethyl levomilnacipran in the body because renal excretion is the main elimination pathway for both levomilnacipran and the metabolite [11]. Furthermore, as indicated by in vitro CYP phenotyping results [13], CYP3A4 is likely not the sole enzyme involved in the formation of N-desethyl levomilnacipran, and ketoconazole may have additional, unquantified effects on these alternate enzymes. In a study in hepatically impaired subjects, the increase in levomilnacipran AUC in the severely impaired participants relative to healthy control subjects was only approximately 30 %, consistently indicating that hepatic metabolism plays a minor role in levomilnacipran elimination [12].
Overall, concomitant administration of levomilnacipran ER with ketoconazole was well tolerated and there were no clinically meaningful effects of co-administration on safety parameters. The increased number of headaches reported with co-administration was likely due to an increase of levomilnacipran exposure to levels that would be expected with a single-dose administration of a 120 mg dose. In clinical practice, levomilnacipran doses of 120 mg are administered following up-titration with a starting dose of 20 mg; thus, patients would not be exposed to high-plasma levomilnacipran exposures without prior administration of lower doses.
Based on these results (57 % increase in levomilnacipran AUC), and considering the overall safety profile of levomilnacipran ER and available capsule strengths (20, 40, 80, and 120 mg), it is recommended that the dose of levomilnacipran ER should not exceed 80 mg once daily when used with strong CYP3A4 inhibitors such as ketoconazole [11].
Carbamazepine also appeared to have a statistically significant effect on the metabolism of levomilnacipran via CYP3A4. C max,SS and AUC0-τ for levomilnacipran were lower by 26 and 29 %, respectively, and C max,SS and AUC0-τ for N-desethyl levomilnacipran were higher by around 70 % under co-administration, compared with levomilnacipran ER alone. The decreases in levomilnacipran plasma exposure are not considered clinically meaningful, as levomilnacipran has demonstrated efficacy and safety over a wide dose range of 40–120 mg/day [4], and dosing increases are based on individual efficacy and tolerability.
The plasma exposure of carbamazepine was unchanged when administered with levomilnacipran ER. However, AUC0–τ and C max,SS of carbamazepine-10,11-epoxide were increased by 36 and 42 %, respectively. These increases are unlikely to result from any interaction with levomilnacipran, which has been shown in in vitro studies to not inhibit CYP3A4 at clinically relevant levels reported above. It is possible that steady state might not have been reached for carbamazepine 10,11-epoxide, given that the carbamazepine-mediated induction half-life for the formation of the metabolite may be up to 1180 h [24]. Concomitant administration of levomilnacipran ER with carbamazepine was well tolerated and there were no clinically meaningful effects of co-administration on safety parameters.
Consistent with the lack of pharmacokinetic effect of levomilnacipran on carbamazepine, the pharmacokinetics of alprazolam, a CYP3A4 substrate, were not altered following multiple-dose administration of levomilnacipran at the highest recommended therapeutic dose of 120 mg/day. These in vivo observations are in agreement with the in vitro findings that levomilnacipran is a poor inhibitor of CYP3A4 as well as other CYP enzymes evaluated and does not induce CYP3A4 [15, 16]. Therefore, it can also be expected that levomilnacipran is unlikely to interfere with drugs metabolised by other CYP enzymes. Concomitant alprazolam plus levomilnacipran demonstrated no additional safety and tolerability issues compared with each of the drugs administered separately.
The safety profile was generally consistent with what would be expected based on the mechanisms of action (reuptake inhibition of serotonin and norepinephrine). There was one SAE of atrial fibrillation; however, this was not reported as an AE in any of the clinical trials [3–7].
5 Conclusions
Co-administration of levomilnacipran with ketoconazole, a strong CYP3A4 inhibitor, increased levomilnacipran exposure by up to 57 %, with the possible involvement of multiple mechanisms; it is conservatively recommended that the dose of levomilnacipran ER should not exceed 80 mg once daily when used with ketoconazole or other strong CYP3A4 inhibitors (maximum recommended levomilnacipran ER dose is 120 mg once daily).
Co-administration of levomilnacipran with carbamazepine, an inducer of CYP3A4, did not cause clinically meaningful changes in the pharmacokinetics of levomilnacipran.
Based on the results of these drug–drug interaction studies, modulators of other CYP isozymes are not expected to affect the pharmacokinetics of levomilnacipran to a clinically significant degree, because in vitro studies have shown that biotransformation of levomilnacipran via N-desethylation is facilitated primarily by CYP3A4.
Furthermore, as in vitro studies demonstrated only a minor inhibition of CYP3A4 and lack of inhibition of other major CYP enzymes at levels of levomilnacipran much higher than therapeutic concentrations, the lack of meaningful pharmacokinetic changes in alprazolam pharmacokinetics when co-administered with levomilnacipran suggests that no dose adjustment for pharmacokinetic reasons would generally be recommended for drugs metabolised by CYP enzymes when they are co-administered with levomilnacipran ER.
References
Auclair AL, Martel JC, Assié MB, et al. Levomilnacipran (F2695), a norepinephrine-preferring SNRI: profile in vitro and in models of depression and anxiety. Neuropharmacology. 2013;70:338–47.
Deecher DC, Beyer CE, Johnston G, et al. Desvenlafaxine succinate: a new serotonin and norepinephrine reuptake inhibitor. J Pharmacol Exp Ther. 2006;318:657–65.
Montgomery SA, Mansuy L, Ruth A, et al. Efficacy and safety of levomilnacipran sustained release in moderate to severe major depressive disorder: a randomized, double-blind, placebo-controlled, proof-of-concept study. J Clin Psychiatry. 2013;74:363–9.
Asnis GM, Bose A, Gommoll CP, et al. Efficacy and safety of levomilnacipran sustained release 40 mg, 80 mg, or 120 mg in major depressive disorder: a phase 3, randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2013;74:242–8.
Bakish D, Bose A, Gommoll C, et al. Levomilnacipran ER 40 mg and 80 mg in patients with major depressive disorder: a phase III, randomized, double-blind, fixed-dose, placebo-controlled study. J Psychiatry Neurosci. 2014;39:40–9.
Sambunaris A, Bose A, Gommoll CP, et al. A phase III double-blind, placebo-controlled, flexible-dose study of levomilnacipran ER extended release in patients with major depressive disorder. J Clin Psychopharmacol. 2014;34:47–56.
Gommoll C, Greenberg W, Chen C. A randomized, double-blind, placebo-controlled study of flexible doses of levomilnacipran ER (40–120 mg/day) in patients with major depressive disorder. J Drug Assess. 2014;3:10–9.
Mago R, Forero G, Greenberg WM, et al. Safety and tolerability of levomilnacipran ER in major depressive disorder: results from an open-label, 48-week extension study. Clin Drug Invest. 2013;33:761–71.
Montgomery SA, Gommoll CP, Chen C, et al. Efficacy of levomilnacipran extended-release in major depressive disorder: pooled analysis of 5 double-blind, placebo-controlled trials. CNS Spectr. 2014;5:1–9.
Sambunaris A, Gommoll C, Chen C, et al. Efficacy of levomilnacipran extended-release in improving functional impairment associated with major depressive disorder: pooled analyses of five double-blind, placebo-controlled trials. Int Clin Psychopharmacol. 2014;29:197–205.
Forest Pharmaceuticals Inc. Fetzima® (levomilnacipran) extended-release capsules: U.S. Prescribing Information. Forest Pharmaceuticals, Inc.: St. Louis; 2013.
Chen L, Boinpally R, Greenberg WM, et al. Effect of hepatic impairment on the pharmacokinetics of levomilnacipran following a single oral dose of a levomilnacipran extended-release capsule in human participants. Clin Drug Invest. 2014;34:351–9.
Forest Laboratories. Data on file. In vitro cytochrome P450 reaction phenotyping of F2695 in human liver microsomes. Xenotech Study Number: XT104114. 2011.
Forest Laboratories. Data on file. Evaluation of human drug-metabolizing enzyme induction properties of F2695: in vitro experiments. Pierre Fabre Médicament Study no CEPC 05-0173. 2006.
Forest Laboratories. Data on file. Evaluation of human cytochrome P450 inhibitory properties of F2695: in vitro experiments. Pierre Fabre Médicament Study no CEPC 05-0174. 2006.
Forest Laboratories. Data on file. In vitro evaluation of F17400 as an inhibitor of cytochrome P450 (CYP) enzymes in human liver microsomes. XenoTech Study Number: XT105102. 2012.
US Food and Drug Administration. Guidance for Industry: In-Vivo Drug Metabolism/Drug Interaction Studies—Study Design, Data Analysis, and Recommendations for Dosing and Labeling. 1999 Nov. http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM072119.pdf. Accessed Mar 2010. Guidelines in use at time of study; guidelines subsequently amended: see Guidance for Industry: Drug Interaction Studies—Study Design, Data Analysis, Implications for Dosing, and Labeling Recommendations, February 2012. Available from: http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM292362.pdf. Accessed October 2013.
US Food and Drug Administration. Guidance for Industry, Drug Interaction Studies—Study Design, Data Analysis, and Implications for Dosing and Labeling. September, 2006. http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM072119.pdf. No longer available online. Guidelines in use at time of study; guidelines subsequently amended: see Guidance for Industry: Drug Interaction Studies—Study Design, Data Analysis, Implications for Dosing, and Labeling Recommendations, February 2012. Available from: http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM292362.pdf. Accessed Dec 2013.
International Conference on Harmonisation—Efficacy (E2A), March 1995. Available from: http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM073087.pdf. Accessed July 2015.
Pfizer, Inc. Xanax® XR CIV (alprazolam) extended-release tablets: U.S. Prescribing Information. Pfizer: USA: 2013.
Kim RB, Leake B, Cvetkovic M, et al. Modulation by drugs of human hepatic sodium-dependent bile acid transporter (sodium taurocholate cotransporting polypeptide) activity. J Pharmacol Exp Ther. 1999;291:1204–9.
Wang EJ, Lew K, Casciano CN, et al. Interaction of common azole antifungals with P-glycoprotein. Antimicrob Agents Chemother. 2002;46:160–5.
Fernandez PC, Wallace DW, Ryan K, et al. Effects of oral ketoconazole on renal function in healthy volunteers. Clin Pharmacol Ther. 2005;77:P81.
Magnusson MO, Dahl ML, Cederberg J, et al. Pharmacodynamics of carbamazepine-mediated induction of CYP3A4, CYP1A2, and Pgp as assessed by probe substrates midazolam, caffeine, and digoxin. Clin Pharmacol Ther. 2008;84:52–62.
Acknowledgments
We thank Hao Chen (Forest Research Institute, Inc., NY) and Valerie Brunner (Pierre Fabre Médicament, Toulouse, France) for their work on the in vitro studies that preceded this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
These studies were supported by funding from Forest Research Institute, Inc., an affiliate of Actavis, Inc. (New York, NY), and Pierre Fabre Médicament, Boulogne, France. Both companies were involved in the study design, collection (via contracted clinical investigator sites), analysis and interpretation of data, and the decision to present these results.
Writing assistance, editorial, and logistical support for this manuscript was provided by Grace Townshend and Daria Renshaw of Watermeadow Medical, UK, and funded by Forest Research Institute, Inc.
Conflicts of interest
LC, RB and AP are all employees of Forest Research Institute, Inc., an affiliate of Actavis, Inc.
LC, RB and AP hold stock/stock options in Actavis, Inc.
WMG, NG, JW and PG were employees of Forest Research Institute, Inc., at the time of these studies. WMG held stock/stock options in Forest Research Institute, Inc. while an employee, but no longer holds them.
Ethical approval
All procedures in the three studies were in accordance with the 1964 Helsinki Declaration (and its amendments), and the Ethical Committee or institutional review board that approved the study.
Informed consent
Written informed consent was obtained from all subjects.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chen, L., Boinpally, R., Gad, N. et al. Evaluation of Cytochrome P450 (CYP) 3A4-Based Interactions of Levomilnacipran with Ketoconazole, Carbamazepine or Alprazolam in Healthy Subjects. Clin Drug Investig 35, 601–612 (2015). https://doi.org/10.1007/s40261-015-0318-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-015-0318-2