Abstract
Research and drug developments fostered under orphan drug product development programs have greatly assisted the introduction of efficient and safe enzyme-based therapies for a range of rare disorders. The introduction and regulatory approval of 20 different recombinant enzymes has enabled, often for the first time, effective enzyme-replacement therapy for some lysosomal storage disorders, including Gaucher (imiglucerase, taliglucerase, and velaglucerase), Fabry (agalsidase alfa and beta), and Pompe (alglucosidase alfa) diseases and mucopolysaccharidoses I (laronidase), II (idursulfase), IVA (elosulfase), and VI (galsulfase). Approved recombinant enzymes are also now used as therapy for myocardial infarction (alteplase, reteplase, and tenecteplase), cystic fibrosis (dornase alfa), chronic gout (pegloticase), tumor lysis syndrome (rasburicase), leukemia (l -asparaginase), some collagen-based disorders such as Dupuytren’s contracture (collagenase), severe combined immunodeficiency disease (pegademase bovine), detoxification of methotrexate (glucarpidase), and vitreomacular adhesion (ocriplasmin). The development of these efficacious and safe enzyme-based therapies has occurred hand in hand with some remarkable advances in the preparation of the often specifically designed recombinant enzymes; the manufacturing expertise necessary for commercial production; our understanding of underlying mechanisms operative in the different diseases; and the mechanisms of action of the relevant recombinant enzymes. Together with information on these mechanisms, safety findings recorded so far on the various adverse events and problems of immunogenicity of the recombinant enzymes used for therapy are presented.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Regulatory approval of nine recombinant enzymes has enabled effective enzyme-replacement therapy for a number of rare lysosomal storage diseases involving enzyme deficiency, in particular, α-glucosidase in the glycogen storage disorder Pompe disease; α-d -galactosidase A and β-glucocerebrosidase for the lipid storage disorders Fabry disease and Gaucher disease, respectively; and α-l -iduronidase, iduronate-2-sulfatase, N-acetylgalactosamine-6-sulfatase, and N-acetylgalactosamine-4-sulfatase for mucopolysaccharidoses types I, II, IVA, and VI, respectively, where, in each case, accumulated, and ultimately toxic, substrates include dermatin, heparan, and keratan sulfates. |
Of the remaining approved enzyme preparations, three are tissue plasminogen activators, alteplase, reteplase, and tenecteplase, administered for acute myocardial infarction, while the other eight cover a range of disorders: cystic fibrosis (dornase alfa), chronic gout (pegloticase), tumor lysis syndrome (rasburicase), leukemia (l -asparaginase), some collagen-based disorders such as Dupuytren’s contracture (collagenase), severe combined immunodeficiency disease (pegademase bovine), detoxification of methotrexate (glucarpidase), and vitreomacular adhesion (ocriplasmin). |
Adverse events range from boxed warnings for severe allergic reactions, including anaphylaxis, to rare effects on the heart, lungs, liver, blood, and skin as well as a variety of mild to moderate commonly seen responses such as gastrointestinal symptoms, headache, and mild cutaneous reactions, but side effects are generally not serious. |
1 Introduction
A large number and variety of enzyme defects have been identified in humans, many leading to diseases produced by enzyme deficiency or altered amounts of metabolites. One may think that the existing knowledge of enzymology, together with implication of an enzyme-based defect, would lead to rapid progress in the development of successful targeted therapies for some of the diseases. However, much progress in our understanding of cell and molecular biology was needed before significant advances leading to registered efficacious pharmaceuticals could occur. The so-called storage diseases provided both the best early examples of a clear association between enzyme deficiency and disease as well as candidates for a successful therapeutic approach to treatment. For treatment to be successful, a number of requirements were seen to be essential. First, it was clear that not all storage diseases were suitable targets for therapy [1]. Some diseases produce irreversible damage, for example, ganglioside GM2 storage diseases Tay–Sachs disease and Sandhoff’s disease, where central nervous system (CNS) damage that occurs early in life is untreatable. Other factors that need to be considered include the likelihood of producing sufficient specific enzyme; its stability; the possibility of delivering the enzyme to the cell target where it needs to act; the enzyme’s likely antigenicity and the consequent antibody response in treated patients; and the frequency of the disease—a rare disease with only a few patients might not justify research and development efforts and costs, even under an orphan drug development program [1, 2].
2 Toward Successful Enzyme-Replacement Therapy (ERT): Gaucher Disease
Early evidence obtained from experiments using cultured skin fibroblasts from patients with a mucopolysaccharide storage disease or mucopolysaccharidosis (MPS), together with cells of a different genotype, indicated that post-translational modification of lysosomal enzymes could correct previously defective glycosaminoglycan catabolism [3]. Subsequent investigations showed that the corrective modification resulted from the recognition by complementary receptors of d -mannose-6-phosphate on the modified lysosomal enzymes [2, 4–9]. During the same period as these studies, lysosomal enzymes injected into rats were shown to avoid rapid clearance and to be specifically taken up by liver reticuloendothelial cells via recognition of mannose residues [10–12]. Importantly, the complementary mannose receptors were demonstrated on the surface of macrophages, and their recognition spectrum was shown to extend beyond this sugar to N-acetyl-d -glucosamine and l -fucose [13, 14]. Once bound to the receptors, enzyme is rapidly internalized and transported to the lysosomes. The discoveries of specific recognition of phosphorylated mannose residues, mannose receptor-mediated uptake of lysosomal enzymes, and the presence of these receptors on macrophages demonstrated that a lysosomal enzyme needs to be specifically recognized by its target cells. These insights led on to the first successful enzyme-replacement therapy (ERT) for type I Gaucher disease [15], which occurs with a frequency of 1 in 75,000 births worldwide, making it the most prevalent of the sphingolipid storage disorders [16]. Gaucher disease is the result of an inborn error of metabolism due to a deficiency of the lysosomal acid β-glucosidase glycoprotein, β-glucocerebrosidase (glucosylcerimidase; β-glucosyl-N-acylsphingosine glucohydrolase), which cleaves β-d -glucosylceramide (glucocerebroside) into glucose and ceramide. The enzyme’s substrate is a widely distributed cell membrane component and, in the absence of β-glucocerebrosidase, glucocerebroside and other glycolipids accumulate by as much as 20- to 100-fold in the lysosomes of cells, particularly macrophages and other cells of the reticuloendothelial system [15]. With this background, glucocerebrosidase prepared from human placenta and marketed as Ceredase® was used to reverse the clinical manifestations of type I Gaucher disease [17, 18] by targeting the patients’ macrophages after sequential deglycosylation to expose mannose residues [19]. Imiglucerase, a recombinant, deglycosylated glucocerebrosidase prepared in Chinese hamster ovary (CHO) cells by DNA technology, was soon introduced. Because it proved at least as clinically effective as Ceredase® and could provide a pathogen-free preparation in almost unlimited amounts, it (as Cerezyme®) soon replaced its predecessor.
3 Approved Enzymes as Replacement Therapy for Lysosomal Storage Diseases
In an effort to encourage the development of products for the diagnosis and treatment of rare or so-called orphan diseases, countries, beginning with the USA, have introduced legislation to provide incentives for developers and manufacturers who would otherwise have been unable to cover the costs involved in bringing a drug to a very small market [20]. For example, the US FDA Office of Orphan Products Development (OOPD) provides incentives in cases involving fewer than 200,000 people in the USA where, since 1983, more than 400 drugs and biologic products for rare diseases have been brought to market under the Orphan Drug Designation programs. This compares with a total of ten products developed in the previous decade [21]. The recombinant enzyme biologics covered in this review are regulated and approved by the FDA Center for Drug Evaluation and Research (CDER) [22] rather than the Center for Biologics Evaluation and Research, which retains regulatory responsibility for bacterial and human cellular products, gene therapy products, vaccines, allergenic extracts, antitoxins, antivenoms, blood, blood components, and plasma-derived products. With the emphasis here being on the recombinant proteins involved in ERT for lysosomal storage diseases as well as other approved orphan drug recombinant enzymes for treatment of rare diseases, the well-known and long-used enzymes hyaluronidase and streptokinase have not been included, nor have the serine protease and transglutaminase coagulation factors involved in the coagulation pathways, since the sheer volume, complexity, and specialization of the mechanisms and disease states associated with the science and therapy of clotting and hemostasis requires the space for a review of its own. Likewise, although pancrelipase (Creon®) is indicated for the treatment of pancreatic insufficiency due to cystic fibrosis and chronic pancreatitis, the relatively poorly defined nature of this extract of porcine pancreas glands containing multiple enzymes, including lipases, proteases, and amylases, does not fit with the highly purified, mainly recombinant enzyme preparations toward which this review is directed.
Utilizing the scientific insights summarized above and the still-expanding manufacturing expertise in biologics, orphan drug research and development programs have made remarkable progress in introducing efficacious and safe enzyme-based therapies for a range of rare disorders. Central amongst these disorders, and as a direct result of the knowledge and experience gained in the development of ERT for Gaucher disease, are successful ERTs for a small but growing number of other lysosomal storage diseases. A list of these diseases, together with the responsible deficient enzymes, and the accumulating products that cause the signs and symptoms of the diseases currently being treated with approved recombinant enzyme preparations are set out in Table 1. Depending on the particular MPS, the accumulated products produce clinical manifestations such as short stature, coarse features, motor dysfunction, cardiomyopathy, ocular abnormalities, skeletal dysplasia, hepatosplenomegaly, and mental retardation. Approved ERTs are now administered for a second lipid storage disorder, Fabry disease, for the glycogen storage disorder, Pompe disease, and for types I, II, IVA, and VI MPS. In addition to the individual deficient enzymes and resultant accumulated products (Table 1), the specificities, properties, and mechanisms of action of the nine approved recombinant enzymes currently used as ERT for lysosomal storage diseases (alglucosidase alfa, agalsidase beta, imiglucerase, taliglucerase alfa, velaglucerase alfa, laronidase, idursulfase, elosulfase alfa, and galsulfase) are set out in Table 2. Three of these recombinant enzymes, the human β-glucocerebrosidases imiglucerase [23, 24], taliglucerase alfa [25–27], and velaglucerase alfa [28–30] (Table 2), are each approved for treatment of Gaucher disease, but one of these, taliglucerase alfa, differs from the others in two significant ways. Taliglucerase alfa, produced in carrot root cells [31], is the first recombinant enzyme used for therapy that has been derived from a plant cell expression system. Taliglucerase alfa also shows differences in its glycosylation, a result of its core α(1-2)-d -xylose and α(1-3)-l -fucose, which is unique to plant-derived proteins [32].
Fabry disease is a second lipid storage disorder (sphingolipidosis), but in this case caused by a deficiency of an α-d-galactosidase, which results in a build-up of globotriaosylceramide, more commonly known as Gb3 or ceramide trihexoside. Gb3 accumulates in capillary endothelia, affecting in particular the kidneys, heart, eyes, brain, nervous tissue, and skin [33]. Progress in determining the efficacy of ERT for Fabry disease was greatly aided by ensuring an ongoing supply of recombinant human enzyme prepared in CHO cells [34] and development of a mouse model [35, 36]. Both agalsidase alfa (Replagal®) and agalsidase beta (Fabrazyme®) (Table 2) have received regulatory approval for the treatment of Fabry disease [37, 38], although the two preparations appear to be functionally indistinguishable [39–41].
A deficiency of lysosomal acid α-glucosidase in Pompe disease leads to an accumulation of glycogen, which causes myopathy throughout the body but especially in skeletal muscles, heart, liver, and the nervous system [42]. In the early ERT studies, recombinant human α-glucosidase, or alglucosidase alfa, was produced in large scale in CHO cells and in milk of transgenic rabbits [43, 44]. Both enzyme preparations reduced lysosomal glycogen storage in animals and had a prominent effect on cardiac hypertrophy, cardiac function, and survival in human infants [42, 45]. Alglucosidase alfa currently approved by both the FDA and the European Medicines Agency (EMA) is produced by CHO cells (Table 2).
MPS types I, II, IVA, and VI are due to deficiencies of α-l -iduronidase, iduronate-2-sulfatase, N-acetylgalactosamine-6-sulfatase, and N-acetylgalactosamine-4-sulfatase, respectively. Each produce accumulations of glycosaminoglycans, in particular dermatan sulfate, heparan sulfate and chondroitin sulfate. Laronidase, a recombinant human α-l -iduronidase enzyme secreted by overexpressing CHO cells and modified to contain complex oligosaccharides [46, 47] is used in ERT for MPS I (also called Hurler syndrome) and clinically milder variants (Tables 1, 2) [48]. Idursulfase, a recombinant form of iduronate-2-sulfatase (Tables 1, 2), has been approved by both the FDA and the EMA as a safe and effective treatment for MPS II or Hunter syndrome. However, in common with each of the enzymes used for ERT in lysosomal storage diseases and which are too large to cross the blood–brain barrier, idursulfase is probably not an effective treatment for the CNS manifestations of the disease [49]. The enzyme removes the sulfate group from the 2-position of dermatan and heparan sulfates [50] and while the complementary DNA (cDNA) sequence predicts a 550 amino acids precursor, the mature protein is secreted as a 525 amino acid protein after cleavage of the 25 amino acid signal sequence; the following eight amino acids are also removed from the proprotein [51]. Elosulfase alfa, a CHO cell-derived recombinant form of N-acetylgalactosamine-6-sulfatase [52] (Tables 1, 2), was granted marketing approval by the FDA and the EMA in 2014 [53, 54] for the treatment of patients with MPS IVA, also known as Morquio A syndrome, an autosomal recessive disorder caused by a deficiency of the enzyme [55]. In 2005, galsulfase, a recombinant form of N-acetylgalactosamine-4-sulfatase (Tables 1, 2), was approved by the FDA for the treatment of patients with MPS VI (Maroteaux–Lamy syndrome), an autosomal recessive disease due to deficiency of N-acetylgalactosamine-4-sulfatase [56–58]. Although ERT with galsulfase has been relatively successful in treating some aspects of MPS VI disease, such as growth, puberty, and pulmonary function, it has been disappointing in alleviating joint, ophthalmic, and CNS symptoms. Starting treatment at an earlier age may be beneficial for growth, and some aspects of the syndrome may be modified by longer periods of treatment [58].
4 Other Enzymes Approved for Therapy
Of the remaining enzymes in the current CDER Therapeutic Biologic Products list, three are tissue plasminogen activators (tPA) while the other eight cover a range of diseases, including cancers, immunodeficiency, heart disorders, cystic fibrosis, macular adhesion, and disorders involving collagen.
4.1 Tissue Plasminogen Activators
Natural human tPA is a serine protease synthesized by endothelial cells. It is a single polypeptide chain of 527 amino acids, MW ~70 kDa, but in the presence of plasmin it is cleaved into two chains linked by one interchain disulfide bond [59–61]. For the correct folding of tPA, correct pairing of the 17 disulfide bonds in the molecule is required. tPA is made up of five structural domains: a looped ‘finger’ domain near the N-terminal, a growth factor domain, the kringle 1 and kringle 2 domains and, next to the latter, the serine protease domain. The finger and kringle 2 domains bind fibrin clots while the protease domain with its catalytic site at the C-terminus catalyzes the conversion of plasminogen to plasmin [59–61]. Since tPA does not cause side effects such as systemic hemorrhaging and depletion of fibrinogen, investigations were undertaken to provide a suitable high yielding, reliable source of the protein. This led to transfection of CHO cells with the tPA gene, extraction of the recombinant product from the culture medium [62] and attempts to produce the protein from Escherichia coli [63, 64]. Currently approved tPAs are alteplase, reteplase, and tenecteplase (Table 2). Whereas alteplase is glycosylated and has 527 amino acids, the so-called third-generation recombinant tPAs reteplase and tenecteplase are variants of tPA engineered for a longer half-life and resistance to inhibition [65]. Deletion mutant reteplase is not glycosylated and has only 355 amino acids due to deletion of three of the tPA domains, kringle 1, finger, and epidermal growth factor domains. The kringle 2 and protease domains are retained [66], representing amino acids 1–3 and 176–527. The aim in developing reteplase was to produce a faster thrombolytic agent and one with a longer effective half-life without increasing the risk of thrombosis. Tenecteplase is the most fibrin-specific of the tPAs. The 527 amino acid recombinant protein has modifications at three sites, positions 103, 117, and 296–9 (Table 2) that result in an increase in half-life, resistance to plasminogen activator inhibitor (PAI)-1 and thrombolytic potency against platelet-rich thrombi [67]. Like natural human tPA, the recombinant forms bind fibrin in clots via the fibronectin finger (except reteplase) and kringle 2 domains before protease domain-mediated cleavage of a plasminogen Arg-Val bond to form plasmin which, in turn, exerts a thrombolytic action by degrading fibrin.
4.2 Asparaginase
Specific for the non-essential amino acid l -asparagine, the amidohydrolase l-asparaginase is prepared from E. coli and Dickeya dadantii, formerly named Erwinia chrysanthemi. Three asparaginase preparations are currently approved, one each from E. coli and D. dadantii and a pegylated preparation, pegaspargase, from E. coli (Table 2). A recombinant E. coli form has been developed and is being tested [68]. Depletion of the supply of asparagine leads to cell cycle arrest in the G1 phase, inhibition of protein synthesis and apoptosis of lymphocytic leukemia cells. Use of the enzyme in acute lymphocytic leukemia (ALL) is based on the fact that susceptible leukemia cells cannot synthesize asparagine due to lack of the enzyme asparagine synthase and depend on an endogenous source of the amino acid for survival [69, 70]. Pegaspargase is a monomethoxypolyethylene glycol succinimidyl conjugate of E. coli l -asparaginase. It shows increased half-life and decreased immunogenicity and appears to be associated with improved outcomes when administered for ALL [71].
4.3 Collagenase
Collagenases are proteinases that hydrolyze collagen and it is this property that has seen the enzyme from Clostridium histolyticum become the first approved non-surgical treatment for Dupuytren’s contracture [72, 73] (Table 2). Injection of collagenase into a Dupuytren’s cord, which is mainly interstitial collagen, results in enzymatic cleavage and disruption of the cord. Collagenase as Xiaflex® [72] and Xiapex® [73] is a mixture of class I (AUX-I) and class II (AUX-II) C. histolyticum collagenases in a required ratio. Each class hydrolyses collagen at different sites but they act in a complementary manner to degrade the protein. Class I collagenases (α, β, γ, and η), products of the colG gene, hydrolyze collagen near the amino and carboxy termini, generating large proteolytic fragments. Class II collagenases (δ, ε, and ζ), products of the colH gene, cleave interior sites of the molecule, generating smaller fragments [74]. Together, this different, but complementary, substrate specificity leads to effective degradation of the entire collagen molecule [75]. All seven collagenases, α, β, γ, δ, ε, ζ, and η, are zinc proteinases functionally related to matrix metalloproteinases (MMPs) which, among other activities, degrade the extracellular matrix. Although it has been suggested that the sequence homology shared between AUX-I, AUX-II, and human MMPs indicates potential immunological cross-reactivity between the proteins, with resultant antibody-induced inhibition of MMPs, studies so far show no evidence of any clinical adverse events associated with MMP inhibition in patients treated with collagenase [76].
4.4 Dornase Alfa
Dornase alfa is a 260 amino acid recombinant human deoxyribonuclease I (rhDNase I) identical in composition to the natural enzyme (Table 2). Viscous extracellular DNA, released mainly by disintegrating neutrophils during infection, accumulates in sputum of patients with cystic fibrosis, contributing to reduced pulmonary function and frequent pulmonary infection [77]. Mucus containing significant amounts of extracellular DNA from degenerating leukocytes is also a problem in bronchiectasis patients [78], patients with respiratory syncytial virus bronchiolitis [79], and in non-cystic fibrosis pediatric patients with atelectasis [80]. Dornase alfa (Table 2) converts extracellular DNA to 5′-phosphonucleotide end products, reducing both sputum viscosity in the airways and adhesiveness of lung secretions without affecting intracellular DNA and has proven to be an effective treatment in cystic fibrosis [81–83] and the other conditions mentioned.
4.5 Glucarpidase
Glucarpidase (Table 2), a recombinant pseudomonas carboxypeptidase G2 produced in E. coli, is used clinically to hydrolyze methotrexate and other antifolates [84]. Methotrexate, administered for various cancers, is eliminated in the urine, so patients with renal impairment given the drug may experience high plasma concentrations. Glucarpidase is indicated in such patients, ensuring that methotrexate is eliminated enzymatically, mainly by hepatic mechanisms, and not by the kidneys. Toxic blood levels of the drug can be rapidly decreased by intravenous administration of glucarpidase [85]. Leucovorin, a reduced folate and potential substrate for glucarpidase, should not be given with the enzyme that degrades it. In addition, the drug competes with methotrexate for the enzyme [86].
4.6 Ocriplasmin
The use of plasmin to degrade fibrin polymers has been a priority in human therapy for more than 60 years. In the recombinant protein age, it was found that intracellular plasminogen activators made the production of plasminogen, the precursor of plasmin, difficult. This led to the production of short forms of plasmin that retained fibrinolytic activity. Ocriplasmin (also known as des-kringle 1–5 plasmin or microplasmin) (Table 2), a proteolytic enzyme and truncated form of human plasmin produced in a yeast Pichia pastoris expression system [87], lacks all five kringle domains and is composed of 249 amino acids in the form of two polypeptide chains linked by two disulfide bonds joining residues 6 and 124 and 16 and 24. Four intrachain disulfide bonds stabilize the larger polypeptide chain of 230 amino acids [88]. Ocriplasmin has activity against the clinically relevant plasmin receptors fibronectin and laminin, components of the vitreoretinal interface [89]. Vitreomacular adhesion may lead to traction and macular holes, but clinical trials have shown that intravitreal injection of ocriplasmin can induce separation of the vitreous and macular surfaces, thereby resolving vitreomacular traction and closing macular holes [89–91].
4.7 Pegademase Bovine
Pegademase [92, 93], the first enzyme approved by the FDA as an orphan drug, is adenosine deaminase of bovine intestine origin [94] extensively pegylated (Table 2) to increase the half-life. Pegademase, used as therapy for severe combined immunodeficiency disease (SCID), also provided the first successful enzyme treatment for an inherited disease. SCID is a primary (i.e., inherited) immune deficiency caused by several different genetic mutations affecting the immune system, with at least 12 genes implicated [95]. The disease is referred to as ‘combined’ because both cell-mediated (T lymphocytes) and humoral (B lymphocytes) immunity are affected [96, 97]. The most common genetic defect in SCID is an X-linked mutation or the so-called gamma chain defect leading to decreased amounts of immunoglobulin G. This form represents about 50 % of cases, while defects involving the gene for adenosine deaminase account for ~15 %. A deficiency of adenosine deaminase leads to the accumulation of adenosine, 2′-deoxyadenosine, and their metabolites, which are toxic to lymphocytes. A deficiency of T lymphocytes, particularly functional helper T cells and B lymphocytes, results in a markedly decreased production of antibodies and impairment of both arms of the adaptive immune response [95–97]. Therapy with pegademase bovine has been shown to diminish the frequency of opportunistic infections and relieve symptoms of diarrhea, failure to thrive, and dermatitis. Note also that treatment with the enzyme does not preclude a subsequent bone marrow transplant from a human leukocyte antigen (HLA)-identical donor.
4.8 Pegloticase
Rasburicase (see Sect. 4.9), developed for treating tumor lysis syndrome (TLS) in pediatric cancer patients, was also found to lower serum urate levels in patients with gout, but the use of rasburicase for this purpose was found to be limited by its immunogenicity and relatively short half-life. Pegloticase (Table 2) was developed to overcome this [98]. Pegylated to reduce its potential for immunogenicity and to increase its circulatory half-life, pegloticase, a recombinant porcine/baboon variant uricase (urate oxidase) produced in E. coli, is used for therapy of gout previously refractory to conventional therapy with uricostatic (e.g., allopurinol) and uricosuric drugs (e.g., probenecid, colchicine, sulfinpyrazone). Nine of the 30 lysines of this tetrameric peptide are pegylated, giving a final MW of 545 kDa [99, 100]. The enzyme urate oxidase, which is absent in humans, catalyzes the oxidation of uric acid to 5-hydroxyisourate and hydrogen peroxide. The former compound is unstable and breaks down to racemic allantoin, which is much more soluble than uric acid and is readily excreted. Pegloticase has been evaluated for efficacy in at least eight clinical studies [98, 101].
4.9 Rasburicase
Rasburicase (Table 2), a recombinant Aspergillus flavus-derived urate oxidase expressed in Saccharomyces cerevisiae, is almost identical to the natural Aspergillus enzyme, differing only by having a higher specific activity and by a modified reactive cysteine [102]. Rasburicase has proved effective in managing TLS [103–105], which usually occurs 48–72 h after initiation of cancer therapy when large numbers of tumor cells undergo apoptosis in a short time, releasing their intracellular contents into the circulation. This causes an ionic imbalance involving hyperkalemia and hyperphosphatemia, secondary hypercalcemia and hyperuricemia, and possibly acute kidney injury and death [106, 107]. In pediatric patients with acute leukemia and lymphoma, rasburicase has proved to be the treatment of choice and superior to allopurinol, but results with adults have been less clear. However, in a study of the efficacy of the preparation for the prevention and treatment of hyperuricemia during induction of chemotherapy for aggressive non-Hodgkin lymphoma in adults, results showed the enzyme to be a highly effective, fast-acting, and reliable therapy [108].
5 Safety of Approved Enzymes
Two general points need emphasis in relation to the safety of enzymes administered as ERTs. Since the enzyme preparations are, in the main, similar to the enzymes produced naturally in humans, adverse events, especially severe ones, are generally not expected. They do occur, of course, but the symptom range is often relatively small and reactions tend to be mild. However, note that since enzymes are proteins, there is always the potential for immediate allergic reactions, including anaphylaxis, and boxed warnings mentioning anaphylaxis have been issued for six of the enzymes listed in Table 2. Second, many of the enzymes have been developed and administered under orphan drug programs and have therefore been given to relatively small numbers of patients, meaning that collected safety data constitute a much smaller body of results than is usually the case with new approved medical agents.
5.1 Adverse Events Caused by Enzymes Used as Therapy for Lysosomal Storage Diseases
5.1.1 Agalsidase Beta for Fabry Disease
An infusion reaction, occurring in ~10–14 % of patients, is the most common adverse event seen during administration of agalsidase for Fabry disease. Reactions, usually mild with no sign of respiratory symptoms, urticaria, or changes in vital signs, occur with a higher frequency (~18 %) in children. Symptoms tend to be easily controllable with antihistamines and corticosteroids. The overall general absence of severe adverse events is reflected in each of the reported adverse event categories (Table 2). For example, cardiac disorders, when they occur, are commonly tachycardia and/or palpitations, and gastrointestinal reactions tend to be nausea, vomiting, and diarrhea [38, 39, 109–113].
5.1.2 Alglucosidase Alfa for Pompe Disease
Now more than a decade old, the Genzyme Corporation MA, USA-sponsored Pompe Registry, the world’s largest repository of worldwide data on Pompe disease, was set up to further understand the natural history and clinical symptomatology of, and treatment outcomes for, the disorder. Valuable information recorded and disseminated includes age at symptom onset, diagnostic methods, mutations, symptoms, and clinical manifestations of infantile-onset versus adult-onset disease.
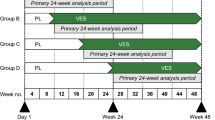
The two registered commercial preparations of alglucosidase alfa (Table 2), Lumizyme® and Myozyme®, are seen by the FDA as being biologically different preparations due to a different manufacturing process. Lumizyme® is approved by the FDA for ERT for late-onset, i.e., non-infantile, Pompe disease without evidence of cardiac hypertrophy in patients more than 8 years old; Myozyme® is approved for ERT for infantile-onset Pompe disease. Despite the apparent enzyme identity of the two preparations, the listed adverse reactions of each show some significant differences. Whereas both carry warnings for severe allergic reactions, including life-threatening anaphylaxis and cardiorespiratory failure, Lumizyme® is responsible for a wide range of reactions, including pyrexia flushing, hyperhidrosis, headache, hypertension, dizziness, rash, and urticaria, while for Myozyme®, infusion reactions, infections such as pneumonia and respiratory syncytial virus, respiratory distress/failure, and gastrointestinal problems predominate [114–116]. This difference is probably related as much to the age of patients and the administered dose of enzyme as to the alleged ‘biological difference’ between the preparations, with Lumizyme® given to older patients with late-onset disease and Myozyme® used to treat infants. In a randomized study of alglucosidase alfa for late-onset Pompe disease in 60 patients, most enzyme-induced adverse events were not serious except for three cases of anaphylaxis, two with respiratory and cutaneous reactions, and the third with severe tongue swelling. Serum immunoglobulin E (IgE) antibodies to alglucosidase alfa were detected in two of the patients [117]. Myozyme® treatment of 18 patients with infantile-onset Pompe disease caused mild to moderate infusion reactions in 11 within 2 h of the infusion. The most common adverse manifestations, urticaria, fever, and decreased oxygen saturation, occurred in the patients given 40 mg/kg [118].
5.1.3 Recombinant Enzymes Used to Treat Gaucher Disease: Imiglucerase, Taliglucerase Alfa, and Velaglucerase Alfa
Imiglucerase, taliglucerase alfa, and velaglucerase alfa, each administered for long-term ERT for Gaucher disease, show a similar spectrum of adverse events, with immediate type I hypersensitivity reactions being the most prominent (Table 2) [24, 119]. As with all orphan drugs, limited safety information was available at the time of marketing authorization. A long-term international post-marketing safety surveillance of imiglucerase carried out on more than 4,500 patients treated with the drug over an 8-year period (1997–2004) found that the most common and consistently reported adverse events could be classified into three categories: general disorders and administration site reactions (i.e., pyrexia, chills, chest discomfort); skin and subcutaneous tissue disorders (pruritus, rash, urticaria); respiratory, thoracic, and mediastinal disorders (dyspnea, cough, throat irritation). Adverse events related to imiglucerase were most frequently associated with infusion of enzyme. They occurred with a low incidence, generally <1 %, and were predominantly self-limiting. Post-marketing analysis of adverse events in children (aged 2–12 years) given imiglucerase identified dyspnea, fever, nausea, flushing, vomiting, and coughing as the most common events. The most common events for adolescents and adults were headache, pruritus, and rash [120]. The effect on safety of the frequency of administration of imiglucerase was assessed in a comparison of intravenous infusions given to adults once every 4 or every 2 weeks with the same total monthly dose. The frequency of adverse events, (which were generally mild) was comparable between the treatment groups [121].
A summary of the adverse events following taliglucerase alfa, including a warning for anaphylaxis, allergy, and infusion reactions, recorded by the FDA [25, 122] is shown in Table 2. In a phase III multinational double-blind, 9-month, 20-infusion clinical trial, taliglucerase alfa-related adverse events were mild/moderate and transient. No serious drug-related events occurred, although two patients (6 %) developed hypersensitivity reactions [26]. A total of 20 adverse events related to taliglucerase alfa treatment were reported in eight patients with Gaucher disease studied for bone marrow responses; one experienced a hypersensitivity reaction during infusion, one had infusion-related dizziness, chills, and nausea, and one developed a fixed drug reaction [123]. Some clinicians believe that taliglucerase alfa seems to have the poorest safety profile of the three recombinant enzymes used to treat Gaucher disease, and while usage may reflect this (Sect. 6), there is currently an absence of figures to decide the question.
As with imiglucerase and taliglucerase alfa used for ERT, velaglucerase alfa is generally well tolerated, with drug-induced adverse events usually mild to moderate [28, 124]. The list of adverse events (Table 2) for velaglucerase alfa is similar to those seen with the other two β-glucocerebrosidases although there are reports of severe prolonged activated partial thromboplastin time and allergic dermatitis occurring with velaglucerase alfa [30]. The safety of the enzyme was assessed in 12 patients with type I Gaucher disease in a 9-month phase I/II and extension study. Adverse events with an incidence of >10 % were infusion reactions, dizziness, headache, nausea, back pain, bone pain, and pyrexia. No serious events related to therapy were reported. Events with an incidence of >10 % and related to treatment during the extension study were tremor, epistaxis, abdominal pain, pain in extremity, and fatigue [125]. Results from an FDA-approved Early Access Program using pre-licensed velaglucerase alfa revealed no enzyme-related serious adverse events and no withdrawals. One patient out of the 71 treated who had previously had an allergic reaction to taliglucerase, experienced an allergic reaction during the first infusion of velaglucerase, and a second switch-over patient had a fixed drug reaction at the first infusion [126].
5.1.4 Laronidase for MPS I
Results of trials designed to examine the efficacy and safety of laronidase (α-l -iduronidase) in the treatment of MPS I showed that the enzyme is generally well tolerated with few events being treatment related and few, if any, serious adverse reactions [127]. Apart from an FDA boxed warning issued for the potential of anaphylaxis and in common with other enzymes used in ERT, the list of side effects is not extensive and lacks serious events (Table 2) [128]. In a long-term trial, laronidase infusions provoked mostly mild and easily managed reactions in 53 % of 40 patients. One patient experienced an anaphylactic reaction but, in the main, reactions markedly diminished after 6 months [129].
5.2 Idursulfase for MPS II
A phase II/III idursulfase ERT study of 32 Hunter syndrome patients (aged 5–31) showed that the enzyme was well tolerated over the 1-year treatment period. Again, the most common adverse events were infusion-based reactions. The incidence of these reactions reached a maximum between weeks 4 and 12 and declined thereafter. Adverse events occurring with at least a 9 % greater frequency than in the placebo-treated group were headache, nasopharyngitis, abdominal pain, arthralgia, pruritus, pruritic rash, swelling at the infusion site, urticaria, dyspepsia, anxiety, and chest wall pain [130]. A follow-up long-term, open-label extension study showed that 50 of the 94 patients (53 %) experienced at least one infusion-related reaction, with headache, urticaria, and pyrexia the most common symptoms [131]. In a Japanese idursulfase ERT study of ten adult patients with MPS II, five of ten patients experienced drug-related infusion reactions occurring within 24 h of the infusion. Skin reactions, namely urticaria and erythema, resulted in patients who showed the highest incidence. Two patients experienced serious reactions, one involving flushing, diffuse urticaria, and numbness of the tongue after commencement of the fifth infusion [132]. A study designed to evaluate the occurrence of infusion-related reactions in patients with MPS II receiving idursulfase reported 65 reactions in 33 patients (31.7 %) in the first year of ERT, with almost all of the initial reactions occurring within the first 3 months. Most reactions were mild to moderate and could be managed by slowing the rate of infusion or by giving antihistamines or antipyretics [133]. Idursulfase is yet another enzyme used for ERT that carries an FDA black box warning of the risk of anaphylaxis after/during infusion of the drug [134]. A list of the adverse events to idursulfase assembled by the FDA is shown in Table 2.
5.2.1 Elosulfase Alfa for MPS IVA
Collected results from six different clinical trials involving 235 patients reveal that ~19 % of patients infused with elosulfase alfa experience a hypersensitivity reaction, with 8 % classified as anaphylactic. This finding is reflected in an FDA box warning (Table 2). Enzyme efficacy did not appear to be impaired in the hypersensitive patients [135]. Safety data collected in a phase III controlled study of ERT with elosulfase alfa for MSP IVA (176 patients aged ≥5 years) showed that 22.4 % of patients had an adverse reaction leading to an extended interruption or discontinuation of infusions [136]. A full list of adverse events (mostly mild such as nausea, vomiting, chills, headache, and abdominal pain) to the enzyme when used as ERT is set out in an EMA assessment report [54] and the FDA full prescribing information [137].
5.2.2 Galsulfase for MPS VI
Galsulfase is generally considered to be a relatively safe drug when used for ERT [57], with infusion-related reactions being the most commonly occurring, and predominate, adverse event. This is not unusual with the enzymic preparations used for ERT or, in fact, for intravenously administered protein therapeutics in general. Other reported adverse events following galsulfase include headache, pyrexia, limb, chest and ear pain, visual abnormalities, anxiety, dyspepsia, upper respiratory infection,s and cough [138, 139] (Table 2). In their extended examination of galsulfase therapy for MPS VI in phase I, II, III, and long-term follow-up studies, Harmatz and colleagues [140–143] observed an incidence of infusion reactions of 20–75 %. Serious drug-related adverse events were uncommon, with a total of only 1.8 % of patients experiencing such reactions in the published studies; three of the more serious were asthma, apnea, and urticaria. An assessment of the efficacy and safety of galsulfase for MPS VI in 34 children aged <5 years [144] showed no serious infusion-related reactions, although eight children (24 %) experienced some treatment-related adverse events. Infusions were continued in each case with the aid of slower infusion rates and antipyretics if needed. Skin rash and edema occurred in one patient who had been receiving ERT for 2 years, and single episodes of tachycardia, skin rash, nausea, elevated blood pressure, and pyrexia were recorded.
Slower infusion rates and pretreatment with antihistamines, steroids, and/or antipyretics have often been used in attempts to manage infusion reactions during ERT. For example, in one report of the successful management of a reaction in a young patient that precluded further therapy, a significant reduction in the rate of infusion was slowly reversed over a period of months while, at the same time, steroid premedication was introduced. The patient ultimately tolerated infusions, with no adverse effects [145].
There has been a report of a single case of thrombocytopenia after the third ERT infusion of galsulfase. A decrease in dose of the enzyme, followed by a subsequent return to the normal dose led to a reversal of the condition. The authors speculated that antibodies to galsulfase may have been the cause [146]. With ocular pathology such as corneal clouding, ocular hypertension, and optic nerve swelling (papilledema) common in MPS VI patients, the report of reversed papilledema and improved visual acuity in an 11-year-old MPS VI patient receiving galsulfase is both curious and encouraging [147].
5.3 Adverse Events Caused by Other Enzymes Used for Enzyme Replacement Therapy
5.3.1 Tissue Plasminogen Activators
The most frequently seen and potentially serious adverse event associated with thrombolytic agents is bleeding [148, 149], especially at intracranial, gastrointestinal, retroperitoneal, and pericardial sites. In an international randomized trial (GUSTO) conducted in 1,081 hospitals in 15 countries and involving 41,021 patients with evolving myocardial infarction, tPA was compared with streptokinase and heparin (subcutaneous and intravenous). Mortality rates in the four treatment groups were 7.2 % for subcutaneous streptokinase and heparin; 7.5 % for intravenous streptokinase and heparin; 6.3 % for tPA and intravenous heparin; and 7 % for the combination of both thrombolytics with intravenous heparin. These figures reveal a 14 % reduction (95 % confidence interval 5.9–21.3) in mortality compared with tPA. Corresponding rates for hemorrhagic stroke were 0.49, 0.54, 0.72, and 0.94 %, respectively, a significantly higher incidence for tPA (p = 0.03). For death and disabling stroke combined, the incidence was lower in the tPA group (6.9 %) than in the streptokinase groups (7.8 %; p = 0.006) [150]. Combined results from trials conducted in the late 1980s showed an incidence of stroke of 1.2 % for patients receiving alteplase and 0.9 % for patients receiving placebo [151–154]. Intracerebral hemorrhage is a severe adverse event for tPA therapy for acute myocardial infarction, but for alteplase, the frequency of intracerebral hemorrhage combined with cerebral infarction and subdural hematoma is comparable to incidences of adverse events seen with other thrombolytic agents in myocardial infarction [155]. Use of alteplase to salvage dysfunctional central venous access devices due to thrombosis was undertaken to analyze the efficacy and safety of the drug after administration of up to 2 mg, which was instilled into the lumen of the central venous catheter and allowed to remain for up to 2 h. If the device was still occluded, the procedure was repeated. A total of 1,064 patients with dysfunctional catheters were treated. Serious adverse events occurring within 30 days of treatment were gastrointestinal bleeding (0.3 %), thrombosis (0.3 %), and sepsis (0.4 %). No cases of intracranial hemorrhage or embolic events were seen [156]. Intrapleural installation has also produced adverse reactions to alteplase. For example, in one study where the enzyme was used in the management of complicated pleural effusion or empyema, chest pain and bleeding at the chest tube site were seen in 6 and 2 %, respectively of 120 patients [157]. At least 41 cases of orolingual angioedema after alteplase administration have been recorded. Although rare, the condition, characterized by swelling of the upper lip and tongue, develops within minutes of injection, causing airway obstruction and breathing problems. These characteristics of the reaction show a clear resemblance to a type I immediate hypersensitivity anaphylactic-like response mediated by IgE antibodies [158]. A number of studies have reported that the development of orolingual angioedema is associated with the use of angiotensin-converting enzyme (ACE) inhibitors (see, for example, Hill et al. [159]). Sepsis, venous thrombosis, and allergic reactions are other well-known adverse events resulting from alteplase therapy [160, 161].
As with other thrombolytics, bleeding is the most common adverse event seen with reteplase and tenecteplase (Table 2). There appears to be no significant difference in the risk of hemorrhage and stroke between reteplase and alteplase, and the risk of stroke (1.2 % for reteplase in 3,288 patients) is similar to that for other thrombolytic agents [162, 163]. The incidence of intracranial hemorrhage for reteplase is ~0.8 %; this increases with age and elevated blood pressure. Any bleeding, regardless of severity, is said to occur with an incidence of ~20 %. In a comparison of thrombolysis achieved with reteplase and alteplase in patients with acute myocardial infarction, there was no significant difference in bleedings requiring a transfusion or in the incidence of hemorrhagic stroke [164]. Chest pain is a common side effect of reteplase, occurring in more than 10 % of patients. Cardiac events such as arrhythmias, circulatory collapse, and another heart attack are seen in 1–10 %, and heart or heart valve damage, blood clot in the lungs, and hypersensitivity occur in 0.1–1 % of treated patients. To evaluate the safety of tenecteplase, 3,235 patients with acute myocardial infarction were given the enzyme as a single bolus (30–50 mg). Total stroke rate at 30 days was 1.5 %, and intracranial hemorrhage occurred in 25 patients (0.77 %). Death, death or nonfatal stroke, or severe bleeding occurred in 6.4, 7.4, and 2.8 % of patients, respectively [165]. A comparison of single-bolus tenecteplase with front-loaded alteplase in acute myocardial infarction revealed an almost identical 30-day mortality rate (6.18 % tenecteplase vs. 6.15 % alteplase), similar rates of intracranial hemorrhage (0.93 vs. 0.94 %), and a similar rate of death or non-fatal stroke at 30 days, but there were fewer non-cerebral bleeding complications and less need for blood transfusions with tenecteplase [166]. The similarity in side effects between alteplase, reteplase, and tenecteplase extends to the possibility of allergic reactions including anaphylaxis; the incidence of such reactions to tenecteplase is <1 %. Other recorded adverse events to tenecteplase include nausea, vomiting, fever, hypotension, and a range of cardiac abnormalities. Expanded lists of side effects for the three tPAs are set out in the regulatory literature [160, 161, 167–169].
5.3.2 l-Asparaginase
Allergic reactions (including anaphylaxis), pancreatitis, hyperglycemia, hepatotoxicity, and abnormal liver function, posterior reversible encephalopathy syndrome (PRES), CNS dysfunction, and thrombosis are listed as the most serious adverse events amongst multiple toxic effects induced by l -asparaginase therapy [170] (Table 2). More than 30 years ago, l -asparaginase-induced coagulopathy involving intracranial hemorrhage with thrombosis of the extremities, immune hemolytic anemia, and abnormal collagen-stimulated platelet aggregation was described and discussed [171]. This profound effect on the coagulation and fibrinolytic systems appears to be the result of drug-impaired synthesis of proteins, including fibrinogen, antithrombin III, protein C, and plasminogen [172]. The incidence of thrombotic complications is in the range of 3–7 %, usually occurring within days of l -asparaginase administration [173]. Hypersensitivity reactions to the enzyme, occasionally fatal, are well-known, especially in children, where allergic sensitivity can sometimes be avoided by switching from the E. coli to the Dickeya (Erwinia) enzyme. The impact of l -asparaginase-induced hypersensitivity on the duration of survival was assessed in adults with ALL. Leukemia-free survival did not correlate with the occurrence of hypersensitivity reactions and, in general, E. coli l -asparaginase was well tolerated. The authors concluded that the possibility of l -asparaginase becoming inactivated by an immune response becomes less important when secondary treatment with Dickeya enzyme is available [174]. A comparison of E. coli l -asparaginase (half-life 26 h) and polyethylene glycol (PEG)-conjugated enzyme (half-life 5.5 days) for treatment of children with ALL showed no correlation between l -asparaginase activity and serum levels. This trial, involving 118 children [175], ultimately led to FDA approval of pegaspargase for the first-line treatment of ALL. A recent successful pediatric treatment regimen of multiple doses of intravenous pegaspargase for adult leukemia patients showed hyperbilirubinemia and transaminitis as the most common grade 3/4 toxicities [176]. An interesting combination of two complications of l -asparaginase therapy was recently reported in a patient who developed transient diabetes mellitus with ketoacidosis and acute pancreatitis [177].
5.3.3 Collagenase
Many of the adverse events recorded for collagenase (Table 2) are associated with the use of the enzyme to treat Dupuytren’s contracture and Peyronie’s disease. Reactions occurring in ≥5 % of patients with Dupuytren’s contracture include peripheral edema, contusion, injection site reactions, pain in extremities, and pruritus. In Peyronie’s disease, the most frequently reported events are penile hematoma, swelling, pain, and ecchymoses; erectile dysfunctions; and genital pruritus [72, 73, 178–183].
5.3.4 Dornase Alfa
Treatment of 968 adult and child cystic fibrosis patients with aerosoled recombinant human DNase for 24 weeks proved to be well tolerated, with only voice alteration and laryngitis observed more often in the treatment group than in the placebo group. Even these reactions were mild and resolved within 21 days. No signs of anaphylaxis were seen [81]. Adverse events occurring in a 12-week trial of dornase alfa administered to patients with advanced cystic fibrosis predominately involved the respiratory system, but no overall difference between the test and placebo groups were seen. Cystic fibrosis-related adverse events such as chest pain, dyspnea, and hemoptysis occurred with similar frequency in both groups. No serious adverse events were recorded. Non-respiratory events that occurred more frequently (≥3 %) in the dornase alfa recipients included fever, rhinitis, pharyngitis, a decrease in forced vital capacity (FVC), voice alteration, and dyspepsia. Adverse events involving sputum changes (consistency, color, increase or decrease) and its mobilization (eg., inability to bring it up), and deaths during the treatment period, were similar in the treated and control groups [82]. A controlled trial of dornase alfa conducted before and after physiotherapy produced 34 adverse events in 26 of 52 cystic fibrosis patients. Upper respiratory tract infections caused by viruses and suppurative lung disease exacerbated by sputum pathogens accounted for the majority of the events [83]. Rash, urticaria, abdominal pain, nausea, vomiting, pyrexia, and headache have also been reported following dornase alfa therapy [184].
5.3.5 Glucarpidase
A number of studies show that glucarpidase is generally well tolerated, with no major adverse events requiring intervention. The most common adverse events reported from clinical trials and compassionate use experience are flushing, paresthesia, headache, shaking, hypotension, nausea and vomiting, tingling fingers, burning of face and extremities, and a feeling of warmth [185–189].
5.3.6 Ocriplasmin
Two double-blind, phase III clinical trials comparing a single intravitreal injection of ocriplasmin with placebo injection in patients with symptomatic vitreomacular adhesion found a similar incidence of ocular events in the two groups. Events associated with vitreous detachment, namely, vitreous floaters, photopsia, injection site pain, and conjunctival hemorrhage occurred in 68.4 % of eyes injected with the recombinant enzyme and in 53.5 % of placebo-injected eyes (p < 0.001). Vitreous floaters occurred in 16.8 % of the treated group and 7.5 % of the placebo group. There was no difference in the incidence of serious ocular events such as macular hole, retinal detachment, or visual acuity [89]. The most commonly reported adverse reactions (≥5 %) in patients treated with ocriplasmin listed by the FDA [190] are vitreous floaters, conjunctival hemorrhage, eye pain, photopsia, blurred vision, macular hole, reduced visual acuity, visual impairment, and retinal edema (Table 2). A recently published post-marketing safety survey of 2,465 retinal physicians in the USA that sought responses to questions on the frequency of use of ocriplasmin and incidences of ocular events received 270 responses concerning 1,056 eyes treated with the enzyme [191]. Reported incidences of adverse events were as follows: acute decline in visual acuity, 179 (17 %); development of submacular fluid or serous retinal detachment, 108 (10.2 %); dyschromatopsia, 96 (9.1 %); progression of vitreomacular traction to macular hole, 92 (8.7 %); development of retinal detachment, 28 (2.7 %); development of retinal tear, 21 (2 %); development of afferent pupillary defect, 19 (1.8 %); electroretinographic abnormalities, 6 (0.6 %); crystalline lens instability, 4 (0.4 %); and vasculitis, 3 (0.3 %). Interestingly, only 15.9 % of the physicians who observed an adverse event had reported the event to the FDA. There have been a few other important reports in the post-marketing period on side effects following intravitreal ocriplasmin, including vision loss that correlated with outer retinal disruption [192] and darkened vision even though there were improvements in vitreomacular adhesion and visual acuity [193]. A somewhat more disturbing case of acute pan-retinal structural and functional abnormalities involving visual acuity loss, pupillary abnormality, and visual field constriction after ocriplasmin suggested to the authors that the many adverse effects were due to the widespread occurrence of laminin in the eye and the consequent diffuse protease effect of ocriplasmin throughout the retina [194].
5.3.7 Pegademase Bovine
Because pegademase bovine is an orphan drug, the relatively small pool of patients and voluntary nature of reporting adverse events in the post-marketing period means that clinical experience with the enzyme is still less than what might be considered desirable (Table 2). Hypersensitivity reactions have so far not been reported and a fairly small range of adverse events, including injection site reactions, headache, and pain, were noted in early clinical trials [92, 93]. In the first months of a developing restoration of the immune response, a transient immune dysregulation may occur. This has seen the development of cases of thrombocytopenia and hemolytic anemia, sometimes associated with virus infections or sepsis [195, 196]. Transient thrombocytosis has also been reported [197]. The long-term effects of pegademase therapy are not yet known but it is already clear that, in some patients, full T-cell immune function is not achieved. Low T-cell numbers have led to cases of malignancy, likely reflecting reduced immune surveillance [198].
5.3.8 Pegloticase
The FDA has issued a black box warning for anaphylaxis and infusion reactions during and after administration of pegloticase, and has listed warnings and precautions for gout flares and the possibility of exacerbation of congestive heart failure [100]. Other adverse reactions listed by regulatory agencies are chest pain, contusion or ecchymosis, nausea, vomiting, nasopharyngitis, and constipation [99, 100] (Table 2). A recently published retrospective analysis of the FDA Adverse Event Reporting System database identified 118 cases of adverse events involving pegloticase in the USA; 14 were pegloticase-associated cardiovascular events; 35 were infusion reactions; 26 were related to gout; and 11 were cases of anaphylaxis induced by the enzyme. Cardiovascular events, infusion-related reactions, gout flares, and anaphylaxis were found to occur more frequently than statistically expected [199]. An evaluation of the long-term (up to 3 years) safety of pegloticase in the treatment of refractory chronic gout revealed that infusion reactions were the most frequent adverse event. Reactions were less often seen in patients receiving biweekly treatment and those who showed a sustained low urate response [200]. Note that pegloticase is contraindicated in patients with glucose-6-phosphate dehydrogenase deficiency (see following section).
5.3.9 Rasburicase
Anaphylaxis to rasburicase and hemolysis and methemoglobinemia are the subjects of an FDA black box warning for the enzyme [201]. The latter two events are relevant to patients with glucose-6-phosphate dehydrogenase deficiency whose erythrocytes are subject to the oxidative stress of hydrogen peroxide produced during the rasburicase-catalyzed conversion of uric acid to allantoin. Methemoglobinemia and/or hemolysis may result from the production of the peroxide. Consequently, rasburicase is contraindicated in patients with known glucose-6-phosphate dehydrogenase deficiency. There are now a number of reports of methemoglobinemia and/or hemolysis in adults and children in the literature, leading to a recommendation to screen patients thought to be at risk [202, 203]. Rasburicase degrades uric acid in blood and plasma at room temperature, causing interference with the measurement of uric acid. This has resulted in a fourth contribution to the FDA boxed warning for the enzyme, with the directive to immediately chill collected blood samples and perform the assay within 4 h of collection. In an assessment of the safety of rasburicase and a comparison with allopurinol in adults at risk of tumor lysis syndrome, adverse events, mainly allergic in nature, were more common in the rasburicase groups. Most reactions were grade 1 or 2; no anaphylaxis or grade 4 hypersensitivity were reported [204]. The most common adverse reactions (incidence ≥20 %) occurring in rasburicase-treated patients with hematologic malignancies are vomiting, nausea, pyrexia, peripheral edema, anxiety, headache, abdominal pain, constipation, and diarrhea (Table 2) [201].
5.4 Antibody Responses to Enzymes
In theory at least, there is always the possibility of an immune response to enzyme therapy, and this carries with it the potential to adversely affect both the efficacy and the safety and perhaps to also influence subsequent treatments. Immunologically based adverse events may manifest as anaphylaxis in the form of cardiovascular collapse, bronchospasm, angioedema, urticaria, and erythema; as an infusion reaction; cytokine-release syndrome; an autoimmune reaction; a cytotoxic type II and immune complex type III hypersensitivities; or as delayed cell-mediated type IV cutaneous hypersensitivities [205]. On the other hand, as often reported, the presence of antibodies to a particular protein may have no clinical consequences [206]. Recently, the FDA issued a draft guidance, Immunogenicity assessment for therapeutic protein products [207], an approach to evaluating and mitigating immune responses to a therapeutic proteins that might affect its therapeutic action. Attention is drawn to the fact that immunogenicity is influenced by both product-specific and patient-specific factors, conclusions borne out by experience obtained with ERT, especially for patients with lysosomal storage diseases. In 2003, Brooks et al. [208] drew attention to studies that collectively showed that antibody responses to enzymes used in ERT are variable. Percentages of patients with an antibody response to therapy for Gaucher disease, MPS I, MPS II, MPS VI, Fabry disease, and Pompe disease were 15, 91, 11, 100, 89, 55, and 66 %, respectively. Most of the antibodies were of the IgG and not the IgE class. It was further pointed out that the relationship of enzyme pharmacokinetics to antibody production was not clear and that, over the long-term, some patients develop immune tolerance with the adverse effects of antibodies becoming of less concern. The authors concluded that most patients with lysosomal storage diseases receiving ERT who mounted an immune response continued therapy, sometimes with premedication and/or a reduced infusion rate. The production of antibodies inhibiting the therapeutic effect appeared to be a rare occurrence, but it was suggested that the occasional high-titer, high-affinity antibodies might be important. Later, enzyme therapy with either agalsidase alfa or beta for Fabry disease revealed antibodies in males occurred more often to agalsidase beta [38] and that, unlike males, females did not develop detectable antibodies to the enzymes [209, 210]. In another (long-term) study, 40 % of adult females developed antibodies only to agalsidase beta [211]. Agalsidase antibodies that developed in male Fabry disease patients were found to frequently interfere with the urinary excretion of Gl3 (deacylated Gb3 or globotriaosylceramide) [210], a glycosphingolipid more elevated in plasma than Gb3 [212]. However, a retrospective analysis of data from 134 patients of the potential impact of IgG antibodies to agalsidase beta on the efficacy of ERT for Fabry disease failed to show a correlation between antibody titers to the enzyme and the onset of clinical events. In addition, no significant association was found between IgG titers and elevated levels of Gl3, but there was a suggestion that clearance of Gl3 may be impaired in patients with high antibody titers [213]. The questions of the presence of antibodies and the reduction of Gl3 in plasma and urine following infusion of agalsidase (alfa and beta), and resultant treatment outcomes, were further examined in a long-term study. Anti-agalsidase antibodies remained for up to 10 years of ERT, and their presence was associated with a subdued decrease in plasma Gl3 and a negative effect on urinary Gb3 reduction. The authors concluded that these results “may reflect worse treatment outcome” [214]. Women with Fabry disease proved more tolerant to agalsidase beta than males with the disease (58 vs. 11 %); most men developed antibodies to the enzyme (73 %), whereas most women did not (12 %). Men who developed anti-agalsidase antibodies appear to be more likely to experience infusion reactions (26 %) than women (11 %) and those who are seronegative [215].
Results from clinical trials on infantile-onset Pompe disease showed 34 of 38 (89 %) patients had IgG antibodies to alglucosidase alfa, and there were indications that those with high titers may experience reduced clinical efficacy. In late-onset disease, a high proportion of patients, if not all, developed antibodies and did so within the first 3 months. There appeared to be no associated inhibition of enzyme activity or adverse events [114, 115]. Approximately 15 % of patients with Gaucher disease developed IgG antibodies to imiglucerase in the first year of therapy, but antibodies rarely developed after 1 year of therapy. Almost one-half of the patients with antibodies to imiglucerase experienced symptoms of hypersensitivity [28]. In two studies, IgG antibodies were detected in 53 and 14 % of patients treated with taliglucerase alfa, but the relevance of these antibodies to the enzyme’s efficacy and to adverse events such as infusion reactions remains unclear [122]. Only about 4 % of patients receiving velaglucerase developed antibodies to the enzyme. These developed late in a 1-year trial, were of the IgG class, and were neutralizing in action [28]. Most patients with MPS I who received laronidase developed antibodies by week 12 (mean ~53 days). During weeks 1–12, plasma clearance of enzyme increased in proportion to antibody titer, but by week 26 clearance was back to week 1 levels in spite of sometimes elevated antibody titers [127, 128]. MPS II patients aged ≤7 years with gene deletion, rearrangement, or different mutations experienced a higher incidence of anti-idursulfase antibody formation than patients with missense mutations. One-half of patients aged ≥5 years given the enzyme developed anti-idursulfase antibodies, and the incidence of hypersensitivity reactions was higher in patients with the antibodies. Approximately 40 % of the antibody-positive patients had antibodies that neutralized enzyme activity or cell uptake of enzyme [134]. Trials have shown that, by week 4 of treatment of MPS IVA patients with elosulfase alfa, antibodies developed in all patients and antibody titers are maintained or increased thereafter during therapy. All patients had antibodies that inhibited binding of the enzyme to the mannose-6-phosphate receptor, but titers were not assessed, thus not allowing an examination of any association between neutralizing antibody and treatment [137]. Clinical studies showed that 98 % of MPS VI patients treated with galsulfase developed complementary antibodies within 4–8 weeks of treatment. Evaluation of sera for potential relationships of antibodies to clinical outcomes revealed no clear and consistent relationship between antibody titers on the one hand and neutralizing antibody, infusion reactions, IgE antibodies, and urinary glycosaminoglycan levels on the other [138, 139].
With regard to tissue plasminogen activators, no re-administration studies or any other studies for immunogenicity or tolerance have been undertaken with alteplase, reteplase, and tenecteplase. Three of 487 patients tested for anti-tenecteplase antibodies had a positive titer at 30 days [169].
Approximately one-quarter of patients treated with l -asparaginase from E. coli develop antibodies to the bacterial enzyme. The incidence of antibodies is higher after the second exposure, hypersensitivity reactions occur more often in patients with antibodies, and reactions may be associated with increased clearance of enzyme. Data are inadequate on neutralizing antibodies, but higher levels appear to correlate with decreased enzymatic activity [170]. In a study of children with ALL, high titers of antibody were associated with low E. coli l -asparaginase activity but not with pegasparaginase activity [175].
At 30 days after the commencement of administration of collagenase to patients with Dupuytren’s contracture, high incidences of an antibody response were seen to AUX-I (92 %) and AUX-II (86 %). High titers to both proteins were recorded after the fourth injection. Neutralizing antibodies to AUX-1 and AUX-2 were detected in 10 and 21 % of patients, respectively, but no correlations of antibody frequency, titers, or neutralizing capacity to clinical response or adverse events were seen [178].
Fewer than 5 % of patients treated with dornase alfa have developed complementary antibodies, no patients have developed IgE antibodies to the enzyme, and there have been no reports of serious allergic reactions to dornase alfa. Importantly, improvements in pulmonary function still occurred, even after the appearance of antibodies [184].
In clinical studies reported by the FDA, 16 of 96 patients (17 %) developed anti-glucarpidase antibodies following administration of the recombinant carboxypeptidase; 12 patients developed antibodies after a single injection, while the remaining four patients received two doses [188].
There appears to be no reports of hypersensitivity reactions to pegademase bovine injection, although antibodies are produced to the agent in some patients. Antibodies have been detected 3–8 months after the beginning of therapy, and a small percentage of the patients with antibodies display enhanced enzyme clearance [195]. After 5 months of therapy, one of 12 patients demonstrated enhanced clearance of plasma pegademase bovine that correlated with the appearance of antibody that reacted with the bovine enzyme and with adenosine deaminase. In what was essentially an attempt to induce tolerance, the patient was given an increased dose of enzyme intramuscularly twice a week instead of weekly. No adverse effects resulted, plasma levels of adenosine deaminase were restored, and the patient was returned to weekly doses after 4 weeks [92].
Anti-pegloticase antibodies were detected in a high proportion of patients (89 % [99]) and 92 % [100]) given the enzyme. High antibody titers were detected 3 weeks after the beginning of treatment, indicating the presence of IgM [99]. In some studies, high titer antibodies were associated with failure to maintain pegloticase-induced normal uric acid levels and showed some correlation with a higher incidence of infusion reactions [100]. In a study of the relationship between efficacy and antibody development in patients treated for chronic refractory gout, anti-pegloticase antibodies were determined and antibody titers were examined for possible relationships with serum pegloticase, uric acid concentrations, and risk of infusion reactions. Patients’ diminished responsiveness to pegloticase was found to be associated with high titers of antibody that increase clearance of the enzyme, with the consequent failure to decrease uric acid levels. Lack of response to the enzyme also saw an increased risk of infusion reactions [216].
Anti-rasburicase antibodies may develop and inhibit enzyme activity in patients given the drug. Of pediatric patients with a hematologic malignancy, 11 % developed antibodies in clinical trials within 1 month of first administration, while trials with adults with hematologic malignancies showed antibodies in 18 %, enzyme-neutralizing IgG antibodies in 8 %, and anti-rasburicase IgE antibodies in 6 % of patients from day 14 to 24 months following five daily doses of rasburicase [201]. However, in a phase III study comparing rasburicase with allopurinol in controlling plasma uric acid in pediatric patients with hematologic malignancies, the enzyme did not prove to be highly immunogenic. Overall, the incidence of anti-rasburicase antibodies was low, with only 2 % positive for enzyme-neutralizing antibodies and no patients positive for IgE antibodies to rasburicase [204].
Immunogenicity has not yet been evaluated for ocriplasmin.
Although it seems to be assumed that PEG is not immunogenic and non-antigenic, some pegylated agents elicit anti-PEG antibodies in animal studies, and anti-PEG may limit the therapeutic efficacy of pegasparaginase in ALL and of pegloticase in patients with gout. It has therefore been suggested that the immunogenicity and antigenicity of approved pegylated compounds be carefully examined in humans [217].
6 Living with Enzyme-Replacement Therapy
As can be readily imagined, living with ERT for a lysosomal storage disease and the medical interventions it necessitates, is a major part of patients’ and their families’ lives since ERT is time consuming, costly, disruptive due to required hospital visits, and distressing because of many associated uncertainties associated with the disorders. With these points in mind, a recent exploration of the experiences of young patients and their families in Australia examined the impact of receiving ERT for a lysosomal storage disorder on the health-related quality of life of patients with Pompe disease, Gaucher disease, or MPS types I or II. Findings highlighted the challenges and coping strategies of living with the disorders and the lifetime treatments required [218]. Communication with family members and professionals was deemed especially important, and interventions to deal with the disease were given high priority. On the positive side, some improvements in physical and psychosocial well-being were noted, and the importance of positive thinking and ways to manage uncertainty were described.
In a survey published in 2014 by the European Gaucher Alliance, an umbrella group established in 1994 to support patient organizations for the disease, valuable information was obtained in response to important questions such as numbers affected, specific treatments, availability of and access to treatments, support for patients, patient organizations, and funding sources [219]. Inequalities in access to treatment in different countries were revealed; for example, 6 % of patients in 20 countries were untreated because of a lack of funding and 3 of 27 countries relied entirely on humanitarian aid. Main concerns expressed were difficulties associated with access to treatment, reimbursement, specialist treatment centers, home infusions, and doctors with expertise in Gaucher disease. The survey revealed that funding was almost always limited to one or a very few sources, and two member organizations had no external funding source at all. Of great concern is the fact that awareness of and expertise in Gaucher disease within the medical community is low, sometimes resulting in long delays or gaps in receiving a correct diagnosis and appropriate medical treatment. Amongst rare diseases, Gaucher disease at least has the relative good fortune of having a number of fairly effective and specific non-neuronopathic treatments available. Imiglucerase is the most widely employed treatment, being used in 64 % of patients, followed by velaglucerase alfa (23 %) and taliglucerase alfa and miglustat (each 4 %). Of great concern for now and the future is the high cost of ERT for the lysosomal storage diseases. Current treatments for Gaucher disease for example, depending on the patient’s weight and dosage, is estimated to be US$200,000–380,000 or about €154,000–292,000 per patient per year [219]. Often with deteriorating economic conditions, it is hard to see how patients, and most countries, can afford such seemingly ever-increasing, and already high if not unaffordable, medical costs.
References
Beutler E. Enzyme replacement therapy. TIBS. 1981;6:95–6.
Neufeld EF. Enzyme replacement therapy—a brief history. In: Mehta A, Beck M, Sunder-Plassmann G, editors. Fabry disease: Perspectives from 5 years of FOS. Oxford: Oxford Pharmagenesis; 2006. Ch 10.
Frantanoni JC, Hall CW, Neufeld EF. The defect in Hurler’s and Hunter’s syndromes: faulty degradation of mucopolysaccharide. Proc Natl Acad Sci USA. 1968;60:699–706.
Hickman S, Neufeld EF. A hypothesis for I-cell disease: defective hydrolases that do not enterlysosomes. Biochem Biophys Res Commun. 1972;49:992–9.
Kaplan A, Achord DT, Sly WS. Phosphohexosyl components of a lysosomal enzyme are recognized by pinocytosis receptors on human fibroblasts. Proc Natl Acad Sci USA. 1977;74:2026–30.
Kaplan A, Fischer D, Achord DT, Sly WS. Phosphohexosyl recognition is a general characteristic of pinocytosis of lysosomal glycosidases by human fibroblasts. J Clin Invest. 1977;60:1088–93.
Ullrich K, Mersmann G, Weber E, et al. Evidence for lysosomal enzyme recognition by human fibroblasts via a phosphorylated carbohydrate moiety. Biochem J. 1978;170:643–50.
Hasilik A, Neufeld EF. Biosynthesis of lysosomal enzymes in fibroblasts. Phosphorylation of mannose residues. J Biol Chem. 1980;255:4946–50.
Varki A, Kornfeld S. Structural studies of phosphorylated high mannose-type oligosaccharides. J Biol Chem. 1980;255:10847–58.
Achord DT, Brot FE, Sly WS. Inhibition of the rat clearance system for agalacto-orosomucoid by yeast mannans and by mannose. Biochem Biophys Res Commun. 1977;77:409–15.
Achord DT, Brot FE, Bell CE, et al. Human β-glucuronidase: in vivo clearance and in vitro uptake by a glycoprotein recognition system on reticuloendothelial cells. Cell. 1978;15:269–78.
Schlesinger PH, Doebber TW, Mandell BF, et al. Plasma clearance of glycoproteins with terminal mannose and N-acetylglucosamine by liver non-parenchymal cells. Studies with β-glucuronidase, N-acetyl- β-d -glucosaminidase, ribonuclease B and agalacto-orosomucoid. Biochem J. 1978;176:103–9.
Stahl PD, Rodman JS, Miller MJ, et al. Evidence for receptor-mediated binding of glycoproteins, glycoconjugates, and lysosomal glycosidases by alveolar macrophages. Proc Natl Acad Sci USA. 1978;75:1399–403.
Pontow SE, Kery V, Stahl PD. Mannose receptor. Int Rev Cytol. 1992;137B:221–44.
Grabowski GA, Petsko GA, Kolodny EH. Gaucher disease. http://www.ommbid.com/OMMBID/the_online_metabolic_and_molecular_bases_of_inherited_disease/b/abstract/part16/ch146. Accessed 11 Sept 2014.
Meikle PJ, Hopwood JJ, Clague AE, et al. Prevalence of lysosomal storage disorders. JAMA. 1999;281:249–54.
Barton NW, Furbish FS, Murray GJ, et al. Therapeutic response to intravenous infusions of glucocerebrosidase in a patient with Gaucher disease. Proc Natl Acad Sci USA. 1990;87:1913–6.
Barton NW, Brady RO, Dambrosia JM, et al. Replacement therapy for inherited enzyme deficiency—macrophage-targeted glucocerebrosidase for Gaucher disease. N Engl J Med. 1991;324:1464–70.
Furbish FS, Steer CJ, Krett NL, et al. Uptake and distribution of placental glucocerebrosidase in rat hepatic cells and effects of sequential deglycosylation. Biochim Biophys Acta. 1981;673:425–34.
Shar RR. Regulatory framework for the treatment of orphan diseases. In: Mehta A, Beck M, Sunder-Plassmann G, editors. Fabry disease: Perspectives from 5 years of FOS. Oxford: Oxford Pharmagenesis; 2006. Ch 11.
FDA. For Industry. Developing products for rare diseases and conditions. http://www.fda.gov/forindustry/DevelopingProductsforrareDiseasesConditions/default.htm. Accessed 11 Sept 2014.
FDA. CDER Therapeutic Biologic Products. CDER billable biologic product list. http://www.fda.gov/drugs/developmentapprovalprocess/druginnovation/default.htm. Accessed 11 Sept 2014.
Deegan PB, Cox TM. Imiglucerase in the treatment of Gaucher disease: a history and perspective. Drug Des Devel Ther. 2012;6:81–106.
Cerezyme® (imiglucerase). http://www.cerezyme.com/~/media/CerezymeUS/Files/pdf/cerezyme_pi.pdf Accessed 11 Sept 2014.
Elelyso® (taliglucerase alfa). FDA clinical review. http://www.accessdata.fda.gov/drugsatfda_docs/nda/2012/022458Orig1s000MedR.pdf. Accessed 11 Sept 2014.
Zimran A, Brill-Almon E, Chertkoff R, et al. Pivotal trial with plant cell-expressed recombinant glucocerebrosidase, taliglucerase alfa, a novel enzyme replacement therapy for Gaucher disease. Blood. 2011;118:5767–73.
Hollak CEM. An evidence-based review of the potential benefits of taliglucerase alfa in the treatment of patients with Gaucher disease. Core Evid. 2012;7:15–20.
VPRIV® (velaglucerase alfa). FDA clinical review. http://www.accessdata.fda.gov/drugsatfda_docs/nda/2010/022575s000medr.pdf. Accessed 11 Sept 2014.
Aerts JMFG, Yasothan U, Kirkpatrick P. Velaglucerase alfa. Nat Rev Drug Discov. 2010;9:837–8.
Turkia HB, Gonzalez DE, Barton NW, et al. Velaglucerase alfa enzyme replacement therapy compared with imiglucerase in patients with Gaucher disease. Am J Hematol. 2013;88:179–84.
Shaaltiel Y, Bartfeld D, Hashmueli S, et al. Production of glucocerebrosidase with terminal mannose glycans for enzyme replacement therapy of Gaucher’s disease using a plant cell system. Plant Biotechnol J. 2007;5:579–90.
Brumshtein B, Salinas P, Peterson B, et al. Characterization of gene-activated human acid-beta-glucosidase: crystal structure, glycan composition, and internalization into macrophages. Glycobiology. 2010;20:24–32.
Mehta A, Beck M, Sunder-Plassmann G, editors. Fabry disease: perspectives from 5 years of FOS. Oxford: Oxford Pharmagenesis; 2006.
Ioannou YA, Bishop DF, Desnick RJ. Overexpression of human alpha-galactosidase A results in its intracellular aggregation, crystallization in lysosomes, and selective secretion. J Cell Biol. 1992;11:1137–50.
Ohshima T, Murray GJ, Swaim WD, et al. Alpha-galactosidase A deficient mice: a model of Fabry disease. Proc Natl Acad Sci USA. 1997;94:2540–4.
Ioannou YA, Zeidner KM, Gordon RE, et al. Fabry disease: preclinical studies demonstrate the effectiveness of alpha-galactosidase A replacement in enzyme-deficient mice. Am J Human Genet. 2001;68:14–25.
Replagal® (agalsidase alfa). EMA Scientific discussion. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Scientific_Discussion/human/000369/WC500053608.pdf. Accessed 11 Sept 2014.
Fabrazyme® (agalsidase beta) http://www.accessdata.fda.gov/drugsatfda_docs/label/2003/agalgen042403LB.pdf. Accessed 11 Sept 2014.
Lee K, Jin X, Zhang K, et al. A biochemical and pharmacological comparison of enzyme replacement therapies for the glycolipid storage disorder Fabry disease. Glycobiology. 2003;13:305–13.
Sakuraba H, Murata-Ohsawa M, Kawashima I, et al. Comparison of the effects of agalsidase alfa and agalsidase beta on cultured human Fabry fibroblasts and Fabry mice. J Hum Genet. 2006;51:180–8.
Vedder AC, Linthorst GE, Houge G, et al. Treatment of Fabry disease: outcome of a comparative trial with agalsidase alfa or beta at a dose of 0.2 mg/kg. PLoS One. 2007;2(7):e598.
van der Ploeg AT, Reuser AJJ. Lysosomal storage disease 2. Pompe’s disease. Lancet. 2008;372:1342–63.
Van Hove JL, Yang HW, Wu JY, et al. High-level production of recombinant human lysosomal acid alpha-glucosidase in Chinese hamster ovary cells which targets to heart muscle and corrects glycogen accumulation in fibroblasts from patients with Pompe disease. Proc Natl Acad Sci USA. 1996;93:65–70.
Bijvoet AG, Kroos MA, Pieper FR, et al. Recombinant human acid alpha-glucosidase: high-level production in mouse milk, biochemical characteristics, correction of enzyme deficiency in GSDII KO mice. Hum Mol Genet. 1998;7:1815–24.
Kishnani PS, Corzo D, Nicolino M, et al. Recombinant human acid [alpha]-glucosidase: major clinical benefits in infantile-onset Pompe disease. Neurology. 2007;68:99–109.
Zhao K-W, Faull KF, Kakkis ED, et al. Carbohydrate structure of recombinant human α-l-iduronidase secreted by Chinese hamster ovary cells. J Biol Chem. 1997;272:22758–65.
Brooks DA, Fabrega S, Hein LK, et al. Glucosidase active site mutations in human α-l-iduronidase. Glycobiology. 2001;11:741–50.
Jameson E, Jones S, Wraith JE. Enzyme replacement therapy with laronidase (Aldurazyme) for treating mucopolysaccharidosis type I. Cochrane Database Syst Rev. 2013;9:CD009354. doi:10.1002/14651858.CD009354.pub2.
Burrow TA, Leslie ND. Review of the use of idursulfase in the treatment of mucopolysaccharidosis II. Biol Targets Ther. 2008;2:311–20.
Neufeld EF, Muenzer J. The mucopolysaccharidoses. In: Scriver CR, Beaudet AL, Sly WS, et al., editors. The metabolic and molecular basis of inherited disease. 8th ed. New York: McGraw-Hill; 2001. p. 3421–52.
Wilson PJ, Morris CP, Anson DS, et al. Hunter syndrome: isolation of an iduronidat-2-sulfatase cDNA clone and an analysis of patient DNA. Proc Natl Acad Sci USA. 1990;87:8531–5.
Tomatsu S, Montano AM, Gutierrez M, et al. Characterization and pharmacokinetic study of recombinant human N-acetylgalactosamine-6-sulfate sulfatase. Mol Genet Metab. 2007;91:69–78.
Vimizim® (elosulfase alfa). FDA: Highlights of prescribing information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2014/125460s000lbl.pdf. Accessed 12 Sept 2014.
EMA: Assessment report. Vimizim® (elosulfase alfa). http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Public_assessment_report/human/002779/WC500169242.pdf. Accessed 12 Sept 2014.
Tomatsu S, Montano AM, Oikawa H, et al. Mucopolysaccharidosis type IVA (Morquio disease): clinical review and current treatment. Curr Pharm Biotechnol. 2011;12:931–45.
Hopwood JJ, Bate G, Kirkpatrick P. Galsulfase. Nat Rev Drug Discov. 2006;5:101–2.
Valayannopoulos V, Nicely H, Harmatz P, et al. Mucopolysaccharidosis VI. Orphanet J Rare Dis. 2010;5:5. doi:10.1186/1750-1172-5-5.
Lourenҫo CM, Giugliani R. Evaluation of galsulfase for the treatment of mucopolysaccharidosis VI (Maroteaux–Lamy syndrome). Expert Opin Orphan Drugs. 2014;2:407–17.
Pennica D, Holmes WE, Kohr WJ, et al. Cloning and expression of human tissue-type plasminogen activator cDNA in E. coli. Nature. 1983;301:214–21.
Ny T, Elgh F, Lund B. The structure of the human tissue-type plasminogen activator gene: correlation of intron and exon structures to function and structural domains. Proc Natl Acad Sci USA. 1984;81:5355–9.
Collen D, Lijnen HR. The tissue-type plasminogen activator story. Arterioscler Throm Vasc Biol. 2009;29:1151–5.
Cartwright T. Production of t-PA from animal cell culture. In: Spier RE, Griffiths JB, editors. Animan cell biotechnology, vol. 5. London: Academic Press; 1992. p. 217–45.
Sarmientos P, Duchesne M, Denéfle P, et al. Synthesis and purification of active human tissue plasminogen activator from Escherichia coli. Nat Biotechnol. 1989;7:495–501.
Datar RV, Cartwright T, Rosen C-G. Process economics of animal cell and bacteria fermentations: a case study analysis of tissue plasminogen activator. Biotechnology. 1993;11:349–57.
Longstaff C, Williams S, Thelwell C. Fibrin binding and the regulation of plasminogen activators during thrombolytic therapy. Cardiovasc Hematol Agents Med Chem. 2008;6:212–23.
Manosroi J, Tayapiwatana C, Gotz F, et al. Secretion of active recombinant human tissue plasminogen activator derivatives in Escherichia coli. Appl Environ Microbiol. 2001;67:2657–64.
Melandri G, Vagnarelli F, Calabrese D, et al. Review of tenecteplase (TNKase) in the treatment of acute myocardial infarction. Vasc Health Risk Manag. 2009;5:249–56.
Pieters R, Appel I, Kuehnel HJ, et al. Pharmacokinetics, pharmacodynamics, efficacy, and safety of a new recombinant asparaginase preparation in children with previously untreated acute lymphoblastic leukemia: a randomized phase 2 clinical trial. Blood. 2008;112:4832–8.
Broome JD. Evidence that the l-asparaginase of guinea pig serum is responsible for its antilymphoma effects. Nature. 1961;191:1114–5.
Rytting ME. Role of l-asparaginase in acute lymphoblastic leukemia: focus on adult patients. Blood Lymphat Cancer Targets Ther. 2012;2:117–24.
Wetzler M, Sanford BL, Kurtzberg J, et al. Effective asparagine depletion with pegylated asparaginase results in improved outcomes in adult acute lymphoblastic leukemia: Cancer and Leukemia Group B Study 9511. Blood. 2007;109:4164–7.
Xiaflex® (collagenase clostridium histolyticum). FDA: Highlights of prescribing information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2010/125338lbl.pdf. Accessed 12 Sept 2014.
Xiapex®. EMA: Summary of product characteristics. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002048/WC500103373.pdf. Accessed 12 Sept 2014.
Matsushita O, Okabe A. Clostridial hydrolytic enzymes degrading extracellular components. Toxicon. 2001;39:1769–80.
Mookhtiar KA, Van Wart HE. Clostridium histolyticum collagenases: a new look at some old enzymes. Matrix Suppl. 1992;1:116–26.
Edkins TJ, Koller-Eichhorn R, Alhadeff JA, et al. Assessment of potential cross-reactivity of human endogenous matrix metalloproteinases with collagenase Clostridium histolyticum antibodies in human serum obtained from patients with Dupuytren’s contracture. Clin Vaccine Immunol. 2012;19:562–9.
Shak S, Capon DJ, Hellmiss R, et al. Recombinant human Dnase I reduces the viscosity of cystic fibosis sputum. Proc Natl Acad Sci USA. 1990;87:9188–92.
Picot R, Das I, Reid L. Pus, deoxyribonucleic acid and sputum viscosity. Thorax. 1978;33:235–42.
Nasr SZ, Strouse PJ, Soskolne E, et al. Efficacy of recombinant human deoxyribonuclease I in the hospital management of respiratory syncytial virus bronchiolitis. Chest. 2001;120:203–8.
Hendriks T, de Hoog M, Lequin MH, et al. Dnase and atelectasis in non-cystic fibrosis pediatric patients. Crit Care. 2005;9:R351–6.
Fuchs HJ, Borowitz DS, Christiansen DH, et al. Effect of aerosolized recombinant human DNase on exacerbations of respiratory symptoms and on pulmonary function in patients with cystic fibrosis. N Engl J Med. 1994;331:637–42.
McCoy K, Hamilton S, Johnson C, The Pulmozyme Study Group. Effects of 12-week administration of dornase alfa in patients with advanced cystic fibrosis lung disease. Chest. 1996;110:889–95.
Fitzgerald DA, Hilton J, Jepson B, et al. A crossover, randomized, controlled trial of dornase alfa before versus after physiotherapy in cystic fibrosis. Pediatrics. 2005;116:e549–54.
Sherwood RF, Melton RG, Alwan SM, et al. Purification and properties of carboxypeptidase G2 from Pseudomonas sp. strain RS-16. Use of a novel triazine dye affinity method. Eur J Biochem. 1985;148:447–53.
Green JM. Glucarpidase to combat toxic levels of methotrexate in patients. Ther Clin Risk Manag. 2012;8:403–13.
Hempel G, Lingg R, Boos J. Interactions of carboxypeptidase G(2) with 6S-leucovorin and 6R-leucovorin in vitro: implications for the application in case of methotrexate intoxications. Cancer Chemother Pharmacol. 2005;55:347–53.
Nagai N, Demarsin E, Van Hoef B, et al. Recombinant human microplasmin: production and potential therapeutic properties. J Thromb Haemost. 2003;1:307–13.
Aerts F, Noppen B, Fonteyn L, et al. Mechanism of inactivation of ocriplasmin in porcine vitreous. Biophys Chem. 2012;165–166:30–8.
Stalmans P, Benz MS, Gandorfer A, et al. Enzymatic vitreolysis with ocriplasmin for vitreomacular traction with macular holes. N Engl J Med. 2012;367:606–15.
Mitchell MD, Miller DM. Looking at ocriplasmin as a new option in eye disease. Drugs Today. 2012;48:519–24.
Syed YY, Dhillon S. Ocriplasmin: a review of its use in patients with symptomatic vitreomacular adhesion. Drugs. 2013;73:1617–25.
Adagen® (pegademase bovine). http://www.accessdata.fda.gov/drugsatfda_docs/label/2008/019818s042lbl.pdf. Accessed 13 Sept 2014.
Adagen® (pegademase bovine). Product monograph. Sigma-Tau Pharmaceuticals Inc. http://www.adagen.com/pdf/Adagen_Monograph_Final.pdf. Accessed 13 Sept 2014.
Skonezny P. Process for preparing dideoxyinosine using adenosine deaminase enzyme. US Patent US20040175804, issued September 9, 2004.
Hershfield MS, Mitchell BS. Immunodeficiency diseases caused by adenosine deaminase deficiency and purine nucleoside phosphorylase deficiency. In: Scriver CR, Beaudet AL, Sly WS, et al., editors. The metabolic and molecular basis of inherited disease. 7th ed. New York: McGraw-Hill; 1995. p. 1725–68.
Wong HK. Severe combined immunodeficiency. http://www.emedicine.com/derm/TOPIC879.HTM. Accessed 13 Sept 2014.
Puck JM. Neonatal screening for severe combined immunodeficiency. Curr Opin Allergy Clin Immunol. 2007;7:522–7.
Ea H-K, Richette P. Critical appraisal of the role of pegloticase in the management of gout. Open Access Rheumatol Res Rev. 2012;4:63–70.
Krystexxa® (pegloticase). EMA: CHMP assessment report. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Public_assessment_report/human/002208/WC500138365.pdf. Accessed 13 Sept 2014.
Krystexxa® (pegloticase). FDA: Highlights of prescribing information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2012/125293s034lbl.pdf. Accessed 13 Sept 2014.
Sundy JS, Baraf HSB, Yood RA, et al. Efficacy and tolerability of pegloticase for the treatment of chronic gout in patients refractory to conventional treatment. Two randomized controlled trials. JAMA. 2011;306:711–20.
Bayol A, Capdevielle J, Malazzi P, et al. Modification of a reactive cysteine explains differences between rasburicase and Uricozyme, a natural Aspergillus flavus uricase. Biotechnol Appl Biochem. 2002;36:21–31.
Ho VQ, Wetzstein GA, Patterson SG, et al. Abbreviated rasburicase dosing for the prevention and treatment of hyperuricemia in adults at risk for tumor lysis syndrome. Support Cancer Ther. 2006;3:178–82.
Campara M, Shord SS, Haaf CM. Single-dose rasburicase for tumor lysis syndrome in adults: weight-based appreoach. J Clin Pharm Ther. 2009;34:207–13.
Kennedy LD, Ajiboye VO. Rasburicase for the prevention and treatment of hyperuricemia in tumor lysis syndrome. J Oncol Pharm Pract. 2010;16:205–13.
Howard SC, Jones DP, Pui C-H. The tumor lysis syndrome. N Engl J Med. 2011;364:1844–54.
Perry Wilson F, Berns JS. Onco-nephrology: tumor lysis syndrome. Clin J Am Soc Nephrol. 2012;7:1730–9.
Coiffier B, Mounier N, Bologna S, et al. Efficacy and safety of rasburicase (recombinant urate oxidase) for the prevention and treatment of hyperuricemia during induction chemotherapy of aggressive non-Hodgkin’s lymphoma: results of the GRAAL1 (Groupe d’Etude des Lymphomes de l’Adulte Trial on Rasburicase Activity in Adult Lymphoma) Study. J Clin Oncol. 2003;21:4402–6.
Schiffmann R, Kopp JB, Austim HA, et al. Enzyme replacement therapy in Fabry disease. A randomized controlled trial. JAMA. 2001;285:2743–9.
Australian public assessment report for agalsidase alfa ghu. https://www.tga.gov.au/pdf/auspar/auspar-replagal.pdf. Accessed 13 Sept 2014.
Banikazemi M, Bultas J, Waldek S, et al. Agalsidase-beta therapy for advanced Fabry disease. A randomized trial. Ann Intern Med. 2007;146:77–86.
Germain DP, Waldek S, Banikazemi M, et al. Sustained, long-term renal stabilization after 54 months of agalsidase β therapy in patients with Fabty disease. J Am Soc Nephrol. 2007;18:1547–57.
Schiffmann R, Ries M, Timmons M, et al. Long-term therapy with agalsidase alfa for Fabry disease: safety and effects on renal function in a home infusion setting. Nephrol Dial Transplant. 2006;21:345–54.
Lumizyme® (alglucosidase alfa). FDA: Highlights of prescribing information. http://www.lumizyme.com/~/media/LumizymeUS/Files/lumizyme_prescribing_information.pdf. Accessed 13 Sept 2014.
Myozyme® (alglucosidase alfa). FDA: highlights of prescribing information. http://www.myozyme.com/~/media/MyozymeUS/Files/Documents/mz_pi.pdf. Accessed 13 Sept 2014.
Myozyme® (alglucosidase alfa). EMA: summary of product characteristics. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000636/WC500032125.pdf. Accessed 13 Sept 2014.
van der Ploeg AT, Clemens PR, Corzo D, et al. A randomized study of alglucosidase alfa in late-onset Pompe’s disease. N Engl J Med. 2010;362:1396–406.
Kishnani PS, Corzo D, Leslie ND, et al. Early treatment with alglucosidase alfa prolongs long-term survival of infants eith Pompe disease. Pediatr Res. 2009;66:329–35.
Cerezyme® (imiglucerase). http://www.cerezyme.com/~/media/CerezymeUS/Files/pdf/cerezyme_pi.pdf. Accessed 13 Sept 2014.
Starzyk K, Richards S, Yee J, et al. The long-term international safety experience of imiglucerase therapy for Gaucher disease. Mol Genet Metab. 2007;90:157–63.
Kishnani PS, DiRocco M, Kaplan P, et al. A randomized trial comparing the efficacy and safety of imiglucerase (Cerezyme) infusions every 4 weeks versus every 2 weeks in the maintenance therapy of adult patients with Gaucher disease type 1. Mol Genet Metab. 2009;96:164–70.
Elelyso® (taliglucerase). FDA: highlights of prescribing information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2012/022458lbl.pdf. Accessed 13 Sept 2014.
van Dussen L, Zimran A, Akkerman EM, et al. Taliglucerase alfa leads to favorable bone marrow responses in patients with type I Gaucher disease. Blood Cells Mol Dis. 2013;50:206–11.
Morris JL. Velaglucerase alfa for the management of type 1 Guacher disease. Clin Ther. 2012;34:259–71.
Zimran A, Altarescu G, Philips M, et al. Phase 1/2 and extension study of velaglucerase alfa replacement therapy in adults with type 1 Guacher disease: 48-month experience. Blood. 2010;115:4651–6.
Elstein D, Altarescu G, Maayan H, et al. Booster-effect with velaglucerase alfa in patients with Gaucher disease switched from long-term imiglucerase therapy: early access program results from Jerusalem. Blood Cells Mol Dis. 2012;48:45–50.
Wraith JE, Clarke LA, Beck M, et al. Enzyme replacement therapy for mucopolysaccharidosis I: a randomized, double-blinded, placebo-controlled, multinational study of recombinant human α-l -iduronidase (laronidase). J Pediatr. 2004;144:581–8.
Aldurazyme® (laronidase). FDA: highlights of prescribing information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2010/125058s0186lbl.pdf. Accessed 15 Sept 2014.
Clarke LA, Wraith JE, Beck M, et al. Long-term efficacy and safety of laronidase in the treatment of mucopolysaccharidosis I. Pediatr. 2009;123:229–40.
Muenzer J, Wraith JE, Beck M, et al. A phase II/III clinical study of enzyme replacement therapy with idursulfase in mucopolysaccharidosis II (Hunter syndrome). Genet Med. 2006;8:465–73.
Muenzer J, Beck M, Eng CM, et al. Long-term, open-label extension study of idursulfase in the treatment of Hunter syndrome. Genet Med. 2011;13:95–101.
Okuyama T, Tanaka A, Suzuki Y, et al. Japan Elaprase Treatment (JET) study: Idursulfase enzyme replacement therapy in adult patients with attenuated Hunter syndrome (mucopolysaccharidosis II, MPS II). Mol Genet Metab. 2010;99:18–25.
Burton BK, Whiteman DAH. On behalf of the HOS investigators. Incidence and timing of infusion reactions in patients with mucopolysaccharidosis type II (Hunter syndrome) on idursulfase therapy in the real-world setting: a perspective from the Hunter Outcome Survey (HOS). Mol Genet Metab. 2011;103:113–20.
Eleprase® (idursulfase). FDA: Highlights of prescribing information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/125151s0152lbl.pdf. Accessed 15 Sept 2014.
Elosulfase alfa. Canadian expert opinion. Recommendations for the use of elosulfase alfa in the management of MorquioA Syndrome (MPS IVA). June 16, 2014. http://www.garrod.ca/wp-content/uploads/Elosulfase-Canadian-Expert-Opinion.pdf. Accessed 15 Sept 2014.
Hendriksz CJ, Burton B, Fleming TR, et al. Efficacy and safety of enzyme replacement therapy with BMN 110 (elosulfase alfa) for Morquio A syndrome (mucopolysaccharidosis IVA): a phase 3 randomised placebo-controlled study. J Inherit Metab Dis. 2014. doi:10.1007/s10545-014-9715-6.
Vimizim® (elosulfase alfa). FDA: Highlights of prescribing information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2014/125460s000lbl.pdf. Accessed 15 Sept 2014.
Naglazyme® (galsulfase). FDA: Highlights of prescribing information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/125117s111lbl.pdf. Accessed 15 Sept 2014.
Galsulfase EMA. Scientific discussion. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Scientific_Discussion/human/000640/WC500024285.pdf. Accessed 15 Sept 2014.
Harmatz P, Kramer WG, Hopwood JJ, et al. Pharmacokinetic profile of recombinant human N-acetylgalactosamine 4-sulphatase enzymereplacement therapy in patients with mucopolysaccharidosis VI (Maroteaux–Lamy syndrome): a phase I/II study. Acta Paediatr Suppl. 2005;94:61–8.
Harmatz P, Ketteridge D, Giugliani R, et al. Direct comparison of measures of endurance, mobility, and joint function during enzyme-replacement therapy of mucopolysaccharidosis VI (Maroteaux–Lamy syndrome): results after 48 weeks in a phase 2 open-label clinical study of recombinant human N-acetylgalactosamine 4-sulfatase. Pediatrics. 2005;115:e681–9.
Harmatz P, Giugliani R, Schwartz I, et al. Enzyme replacement therapy for mucopolysaccharid- osis VI: a phase 3, randomized, double-blind, placebo-controlled, multinational study of recombinant human N-acetylgalactosamine 4-sulfatase (recombinant human arylsulfatase B or rhASB) and follow-on, open-label extension study. J Pediatr. 2006;148:533–9.
Harmatz P, Giugliani R, Schwartz IV, et al. Long-term follow-up of endurance and safety outcomes during enzyme replacement therapy for mucopolysaccharidosis VI: final results of three clinical studies of recombinant human N-acetylgalactosamine 4-sulfatase. Mol Genet Metab. 2008;94:469–75.
Horovitz DDG, Magalhães TSPC, Acosta A, et al. Enzyme replacement therapy with galsulfase in 34 children younger than five years of age with MPS VI. Mol Genet Metab. 2013;109:62–9.
Kim KH, Decker C, Burton BK. Successful management of difficult infusion-associated reactions in a young patient with mucopolysaccharidosis type VI receiving recombinant human arylsulfatase B (galsulfase [Naglazyme]). Pediatr. 2008;121:e714–7.
Doğan M, Cesur Y, Peker E, et al. Thrombocytopenia associated with galsulfase treatment. Hum Exp Toxicil. 2011;30:768–71.
Koseoglu ST, Harmatz P, Turbeville S, et al. Reversed papilledema in an MPS VI patient with galsulfase (Naglazyme) therapy. Int Ophthalmol. 2009;29:267–9.
Califf RM, Topol EJ, George BS, et al. Hemorrhagic complications associated with the use of intravenous tissue plasminogen activator in treatment of acute myocardial infarction. Am J Med. 1988;85:353–9.
Bovill EG, Terrin ML, Stump DC, et al. Hemorrhagic events during therapy with recombinant tissue-type plasminogen activator, heparin, and aspirin for acute myocardial infarction. Results of the Thrombolysis in Myocardial Infarction (TIMI), phase II trial. Ann Intern Med. 1991;115:256–65.
The GUSTO investigators. An international randomized trial comparing four thrombolytic strategies for acute myocardial infarction. N Engl J Med. 1993;329:673–82.
Topol EJ, Morris DC, Smalling RW, et al. A multicenter, randomized, placebo-controlled trial of a new form of intravenous recombinant tissue-type plasminogen activator (Activase) in acute myocardial infarction. J Am Coll Cardiol. 1987;9:1205–13.
Guerci AD, Gerstenblith G, Brinker JA, et al. A randomized trial of intravenous tissue plasminogen activator for acute myocardial infarction with subsequent randomization to elective coronary angioplasty. N Engl J Med. 1987;317:1613–8.
O’Rourke M, Baron D, Keogh A, et al. Limitation of myocardial infarction by early infusion of recombinant tissue-type plasminogen activator. Circulation. 1988;77:1311–5.
Van de Werf F, Arnold AER, The European Cooperative Study Group for recombinant tissue type plasminogen activator. Intravenous tissue plasminogen activator and size of infarct, left ventricular function, and survival in acute myocardial infarction. Brit Med J. 1988;297:1374–9.
Gore JM, Sloan M, Price TR, et al. Intracerebral hemorrhage, cerebral infarction, and subdural hematoma after acute myocardial infarction and thrombolytic therapy in the Thrombolysis in Myocardial Infarction Study. Thrombolysis in myocardial infarction, phase II, pilot and clinical trial. Circulation. 1991;83:448–59.
Semba CP, Deitcher SR, Li X, The COOL Investigators, et al. Treatment of occluded central venous catheters with alteplase: results in 1064 patients. J Vasc Interv Radiol. 2002;2002(13):1199–205.
Thommi G, Nair CK, Aronow WS, et al. Efficacy and safety of intrapleural installation of alteplase in the management of complicated pleural effusion or empyema. Am J Ther. 2007;14:341–5.
Yayan J. Onset of orolingual angioedema after treatment of acute brain ischemia with alteplase depends on the site of brain ischemia: a meta-analysis. N Amer J Med Sci. 2013;5:589–93.
Hill MD, Lye T, Moss H, et al. Hemi-orolingual angioedema and ACE inhibition after alteplase treatment of stroke. Neurology. 2003;60:1525–7.
CathfloTM Activase® [Alteplase]. http://www.accessdata.fda.gov/drugsatfda_docs/label/2001/altegen090401lb.pdf. Accessed 11 Oct 2014.
Activase® (Alteplase, recombinant; recombinant tissue plasminogen activator, rt-PA) Cathflo® Activase® (Alteplase). Investigator brochure. Summary of changes September 19, 2013. http://braininjuryoutcomes.com/mistie-documents/finish/67/386. Accessed 11 Oct 2014.
Noble S, McTavish D. Reteplase. A review of its pharmacological properties and clinical efficacy in the management of acute myocardial infarction. Drugs. 1996;52:589–605.
Simpson D, Siddiqui MA, Scott LJ, et al. Spotlight on reteplase in thrombotic occlusive disorders. BioDrugs. 2007;21:65–8.
Bode C, Smalling RW, Berg G, et al. Randomized comparison of coronary thrombolysis achieved with double-bolus reteplase (recombinant plasminogen activator) and front-loaded, accelerated alteplase (recombinant tissue plasminogen activator) in patients with acute myocardial infarction. The RAPID II Investigators. Circulation. 1996;94:891–8.
Van de Werf F, Cannon CP, Luyten A, et al. Safety assessment of a single-bolus administration of TNK tissue-plasminogen activator in acute myocardial infarction: the ASSENT-1 trial. The ASSENT-1 Investigators. Am Heart J. 1999;137:786–91.
Van de Werf F, Adgey J, Ardissino D, et al. Single-bolus tenecteplase compared with front-loaded alteplase in acute myocardial infarction: the ASSENT-2 double-blind randomized trial. Lancet. 1999;354:716–22.
Clinical review of reteplase. http://www.fda.gov/downloads/Drugs/DevelopmentApprovalProcess/HowDrugsareDevelopedandApproved/ApprovalApplications/TherapeuticBiologicApplications/ucm107736.pdf. Accessed 11 Oct 2014.
Rapilysin. Summary of product characteristics. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000105/WC500046734.pdf. Accessed 11 Oct 2014.
TNKaseTM Tenecteplase recombinant. http://www.fda.gov/downloads/drugs/developmentapprovalprocess/howdrugsaredevelopedandapproved/approvalapplications/therapeuticbiologicapplications/ucm200875.pdf. Accessed 11 Oct 2014.
Elspar® (asparaginase). FDA: Highlights of prescribing information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/101063s5169lbl.pdf. Accessed 11 Oct 2014.
Cairo MS. Adverse reactions to l -asparaginase. Am J Pediatr Hematol Oncol. 1982;4:335–9.
Zakarija A, Kwaan HC. Adverse effects on hemostatic function of drugs used in hematologic malignancies. Semin Thromb Hemost. 2007;33:355–64.
Beinart G, Damon L. Thrombosis associated with l -asparaginase therapy and low fibrinogen levels in adult acute lymphoblastic leukemia. Am J Hematol. 2004;77:331–5.
Larson RA, Fretzin MH, Dodge RK, et al. Hypersensitivity reactions to l -asparaginase do not impact on the remission duration of adults with acute lymphoblastic leukemia. Leukemia. 1998;12:660–5.
Avramis VI, Sencer S, Periciou AP, et al. A randomized comparison of native Escherichia coli asparaginase and polyethylene glycol conjugated asparaginase for treatment of children with newly diagnosed standard-risk acute lymphoblastic leukemia: a Children’s Cancer Group study. Blood. 2002;99:1986–94.
Douer D, Aldoss I, Lunning MA, et al. Pharmacokinetics-based integration of multiple doses of intravenous pegasparaginase in a pediatric regimen for adults with newly diagnosed acute lymphoblastic leukemia. J Clin Oncol. 2014;32:905–11.
Quintanilla-Flores DL, Flores-Caballero MA, Rodriguez-Gutierrez R, et al. Acute pancreatitis and diabetic ketoacidosis following l -asparaginase/prednisone therapy in acute lymphoblastic leukemia. Case Reports in Oncological Medicine 2014; article ID 139169, pp 3. doi:10.1155/2014/139169.
XiaflexTM (collagenase clostridium histolyticum). FDA: Highlights of prescribing information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2010/125338lbl.pdf. Accessed 13 Oct 2014.
Hurst LC, Badalamente MA, Hentz VR, et al. Injectable collagenase clostridium histolyticum for Dupuytren’s contracture. N Engl J Med. 2009;361:968–79.
Gilpin D, Coleman S, Hall S, et al. Injectable collagenase clostridium histolyticum: a new surgical treatment for Dupuytren’s disease. J Hand Surg Am. 2010;35:2027–38.
Coleman S, Gilpin D, Kaplan FT, et al. Efficacy and safety of concurrent collagenase clostridium histolyticum injections for multiple Dupuytren’s contractures. J Hand Surg. 2014;39:57–64.
Gelbard M, Lipshultz LI, Tursi J, et al. Phase 2b study of the clinical efficacy and safety of collagenase clostridium histolyticum in patients with Peyronie disease. J Urol. 2012;187:2268–74.
Gelbard M, Goldstein I, Hellstrom WJG, et al. Clinical efficacy, safety and tolerability of collagenase clostridium histolyticum for the treatment of Peyronie disease in 2 large double-blind, randomized, placebo-controlled phase 3 studies. J Urol. 2013;190:199–207.
Product monograph. PrPulmozyme® (dornase alfa) recombinant. http://www.rochecanada.com/fmfiles/re7234008/Research/ClinicalTrialsForms/Products/ConsumerInformation/MonographsandPublicAdvisories/Pulmozyme/Pulmozyme_PM_E.pdf. Accessed 13 Oct 2014.
Widemann BC, Balis FM, Murphy RF, et al. Carboxypeptidase-G2, thymidine, and leukovorin rescue in cancer patients with methotrexate-induced renal dysfunction. J Clin Oncol. 1997;15:2125–34.
Buchen S, Ngampolo D, Melton RG, et al. Carboxypeptidase G2 rescue in cancer patients with methotrexate intoxication and renal failure. Br J Cancer. 2005;92:480–7.
Widemann BC, Jayaprakash N, Howard SC, et al. Clinical trial and compassionate use experience with glucarpidase for methotrexate toxicity. J Clin Oncol. 2012;30(Suppl):6530.
Voraxaze® (glucarpidase). FDA: Highlights of prescribing information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2012/125327lbl.pdf. Accessed 13 Oct 2014.
Rattu MA, Shah N, Lee JM, et al. Glucarpidase (voraxaze), a carboxypeptidase enzyme for methotrexate toxicity. P T. 2013;38:732–44.
Jetrea® (ocriplasmin). FDA: Highlights of prescribing information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2012/125422s000lbl.pdf. Accessed 13 Oct 2014.
Shah SP, Jeng K, Fine HF, et al. Postmarketing surveillance survey of adverse events of ocriplasmin (Jetrea®). Invest Ophthalmol Vis Sci. 2014;55:E-Abstr 2208.
Freund KB, Shah SA, Shah VP. Correlation of transient vision loss with outer retinal disruption following intravitreal ocriplasmin. Eye (Lond). 2013;27:773–4.
Tibbetts MD, Reichel E, Witkin AJ. Vision loss after intravitreal ocriplasmin: correlation of spectral-domain optical coherence tomography and electroretinography. JAMA Ophthalmol. 2014;132:487–90. doi:10.1001/jamaophthalmol.2013.8258.
Fahim AT, Khan NW, Johnson MW. Acute panretinal structural and functional abnormalities after intravitreous ocriplasmin injection. JAMA Ophthalmol. 2014;132:484–6. doi:10.1001/jamaophthalmol.2013.8142.
Hershfield M, Mitchell BS. Immunodeficiency diseases caused by adenosiune deaminase deficiency and purine nucleoside phosphorylase deficiency. In: Scriver CR, Beaudet AL, Sly WS, Valle D, editors. The metabolic and molecular basis of inherited disease. New York: McGraw-Hill; 2001. p. 2585–625.
Hershfield MS. Combined immunodeficiencies due to purine enzyme defects. In: Steim ER, Ochs HD, Winkelstein JA, editors. Immunologic disorders in infants and children. Philadelphia: WB Saunders; 2004. p. 480–504.
Marwaha VR, Italia DH, Esper H, et al. Extreme thrombocytosis in response to PEG-ADA: early therapeutic and risk indicators. Clin Pediatr (Phila). 2000;39:183–6.
Booth C, Gaspar HB. Pegademase bovine (PEG-ADA) for the treatment of infants and children with severe combined immunodeficiency (SCID). Biol Targets Ther. 2009;3:349–58.
Gentry WM, Dotson MP, Williams BS, et al. Investigation of pegloticase-associated adverse events from a nationwide reporting system database. Am J Health Syst Pharm. 2014;71:722–7.
Becker MA, Baraf HSB, Yood RA, et al. Long-term safety of pegloticase in chronic gout refractory to conventional treatment. Ann Rheum Dis. 2013;72:1469–74.
Elitek (rasburicase). FDA: Highlights of prescribing information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/103946s5083lbl.pdf. Accessed 14 Oct 2014.
Browning LA, Kruse JA. Hemolysis and methemoglobinemia secondary to rasburicase administration. Ann Pharmacother. 2005;39:1932–5.
Ng JS, Edwards EM, Egelund TA. Methemoglobinemia induced by rasburicase in a pediatric patient: a case report and literature review. J Oncol Pharm Pract. 2012;18:425–31.
Cortes J, Moore JO, Maziarz RT, et al. Control of plasma uric acid in adults at risk for tumor lysis syndrome: efficacy and safety of rasburicase alone and rasburicase followed by allopurinol compared with allopurinol alone—results of a multicenter phase III study. J Clin Oncol. 2010;28:4207–13.
Baldo BA, Pham NH. Drug allergy: clinical aspects, diagnosis, mechanisms, structure–activity relationships. New York: Springer; 2013.
Deegan PB. Fabry disease, enzyme replacement therapy and the significance of antibody responses. J Inherit Metab Dis. 2012;35:227–43.
FDA. Immunogenicity assessment for therapeutic protein products, 2013. Available at http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM338856.pdf. Accessed 14 Sept 2014.
Brooks DA, Kakavanos R, Hopwood JJ. Significance of immune response to enzyme-replacement therapy for patients with a lysosomal storage disorder. Trends Mol Med. 2003;9:450–3.
Linthorst GE, Hollak CE, Donker-Koopman WE, et al. Enzyme therapy for Fabry disease: neutralizing antibodies toward agalsidase alpha and beta. Kidney Int. 2004;66:1589–95.
Vedder AC, Breunig F, Donker-Koopman WE, et al. Treatment of Fabry disease with different dosing regimens of agalsidase: effects on antibody formation and GL-3. Mol Genet Metab. 2008;94:319–25.
Whybra C, Miebach E, Mengel E, et al. A 4-year study of the efficacy and tolerability of enzyme replacement therapy with agalsidase alfa in 36 women with Fabry disease. Genet Med. 2009;11:441–9.
Aerts JM, Groener JE, Kuiper S, et al. Elevated globotriaosylsphingosine is a hallmark of Fabry disease. Proc Natl Acad Sci. 2008;105:2812–7.
Bénichou B, Goyal S, Sung C, et al. A retrospective analysis of the potential impact of IgG antibodies to agalsidase β on efficacy during enzyme replacement therapy for Fabry disease. Mol Genet Metab. 2009;96:4–12.
Rombach SM, Aerts JMFG, Poorthuis BJHM, et al. Long-term effect of antibodies against infused alpha-galactosidase A in Fabry disease on plasma and urinary (lyso)Gb3 reduction and treatment outcome. PLoS One. 2012;7:e47805.
Wilcox WR, Linthorst GE, Germain DP, et al. Anti-α-galactosidase A antibody response to agalsidase beta treatment: data from the Fabry Registry. Mol Genet Metab. 2012;105:443–9.
Lipsky PE, Calabrese LH, Kavanaugh A, et al. Pegloticase immunogenicity: the relationship between efficacy and antibody development in patients treated for refractory chronic gout. Arthritis Res Ther. 2014;16:R60. doi:10.1186/ar4497.
Garay RP, El-Gewely R, Armstrong JK, et al. Antibodies against polethylene glycol in healthy subjects and in patients treated with PEG-conjugated agents. Expert Opin Drug Deliv. 2012;9:1319–23.
Freedman R, Sahhar M, Curnow L, et al. Receiving enzyme replacement therapy for a lysosomal storage disorder: a preliminary exploration of the experiences of young patients and their families. J Genet Couns. 2013;22:517–32.
Znidar I, Collins-Histed T, Niemeyer P, et al. The European Gaucher Alliance: a survey of member patient organisations’ activities. Healthcare environments and concerns. Orphanet J Rare Dis. 2014;9:134. http://www.ojrd.com/content/9/1/134.
Conflict of interest
No financial contribution or any other assistance was received by the author in relation to the preparation and presentation of this work. No potential conflict of interest is, or has been, involved.
Author information
Authors and Affiliations
Corresponding author
Additional information
B. A. Baldo (retired) was formerly with Molecular Immunology Unit, Royal North Shore Hospital of Sydney, Kolling Institute of Medical Research and Department of Medicine, University of Sydney, Sydney, Australia.
Rights and permissions
About this article
Cite this article
Baldo, B.A. Enzymes Approved for Human Therapy: Indications, Mechanisms and Adverse Effects. BioDrugs 29, 31–55 (2015). https://doi.org/10.1007/s40259-015-0116-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40259-015-0116-7