Abstract
Background
Cancer is the third leading cause of mortality in the world, and cancer patients are more exposed to financial hardship than other diseases. This paper aimed to review studies of catastrophic healthcare expenditure (CHE) in cancer patients, measure their level of exposure to CHE, and identify factors associated with incidence of CHE.
Methods
This study is a systematic review and meta-analysis. Several databases were searched until February 2020, including MEDLINE, Web of Science, Scopus, ProQuest, ScienceDirect and EMBASE. The results of selected studies were extracted and analyzed using a random effects model. In addition, determinants of CHE were identified.
Results
Among the 19 studies included, an average of 43.3% (95% CI 36.7–50.1) of cancer patients incurred CHE. CHE varied substantially depending on the Human Development Index (HDI) of the country in which a study was conducted. In countries with the highest HDI, 23.4% of cancer patients incurred CHE compared with 67.9% in countries with the lowest HDI. Key factors associated with incidence of CHE at the household level included household income, gender of the household head, and at the patient level included the type of health insurance, education level of the patient, type of cancer and treatment, quality of life, age and sex.
Conclusion
The proportion of cancer patients that incur CHE is very high, especially in countries with lower HDI. The results from this review can help inform policy makers to develop fairer and more sustainable health financing mechanisms, addressing the factors associated with CHE in cancer patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Reviewed studies of health expenditures among cancer patients in different countries indicate substantial exposure of the patients and their households to CHE. |
The exposure of cancer patients to CHE is driven by the expensive care required, and demonstrates shortfalls in health financing mechanisms resulting in unfair contribution in the health system. |
Policy makers can plan a fairer financing system for cancer patients based on the key determinants identified in this review. |
1 Introduction
Health is a human right that is necessary in all the stages of life and must not be affected by wealth or income [1,2,3]. Presently, the rising costs of healthcare services and their impact on households and the economy have become major concerns for health policy makers [4,5,6,7]. Catastrophic health expenditure (CHE) is a measure of financial hardship experienced by households due to health expenditures. In other words, it refers to health expenditures exceeding a certain proportion of household income or expenditure and which are thus likely to displace other non-discretionary spending. The measurement of CHE therefore reflects a household’s ability to pay, and is not determined solely by health expenditure [8].
Cancer care affects the financial resources of all households, causing some to incur CHE—particularly those with household members at the end-of-life stage [9]. As the third leading cause of global mortality after cardiovascular diseases, cancer affects high-, low- and middle-income countries [10, 11]. By 2030, it is predicted that there will be 75 million cancer patients around the world [12].
Compared with other diseases, cancer treatment is very costly due to repeated hospitalization, numerous outpatient visits, laboratory services, advanced diagnostic tests, chemotherapy, rare and expensive medicines, surgery and radiotherapy among other necessary services [13]. Cancer can therefore impose a substantial economic burden and affect the daily activities of patients and their households, in addition to intangible costs such as pain and mental suffering, and wider impacts on health care systems and society [14].
Different measures of financial hardship exist that aim to capture the consequences of direct medical payments on individuals and their households [15,16,17]. Two indicators are commonly used, CHE and impoverishment. The former is intended to capture whether or not health expenditures will displace non-discretionary household spending, while measures of impoverishment indicate whether or not health expenditures push households into or deeper into poverty. Cancer treatment can endanger the finances of patients and their families given that it is usually aggressive and requires substantial resources, often leading to CHE [18].
The World Health Organization (WHO) considers fairness in health financing a key objective of national health systems and emphasizes the need to protect households against financial hardship, in other words, to provide financial risk protection [19]. The latter is a key dimension of Universal Health Coverage (UHC), which is a target of the third United Nations Sustainable Development Goal (SDG) on Health and Wellbeing. A system with fair financing is one in which households participate in financing health services expenditures based on their financial ability and do not experience financial hardship when doing so [20]. Different measures exist for evaluating the level of fairness in the financial participation of health services; CHE is a common indicator and is currently used to track progress toward UHC [21, 22], using thresholds of 10% and 25% of household income or expenditure for defining CHE. Another threshold used by the WHO states that households incur CHE when health payments exceed 40% of a household’s ability or capacity to pay, where ability to pay refers to non-food household expenditure [23, 24].
It is therefore important to investigate CHE in healthcare systems and to identify factors that put households at risk of incurring CHE. This can help health policy makers select preventive policies and corrective actions to reduce levels of CHE [25, 26]. Many studies in all income settings have analyzed the factors related to CHE [27, 28]. The results of one systematic review showed that a key reason for rising CHE rates is the financing mechanisms used in various health systems [29]. In many low- and middle-income countries, out-of-pocket payments (OOP) constitute a substantial proportion of national health spending and adequate prepayment mechanisms are often lacking. In addition, studies have reported that factors such as the household size, household income, receiving social support, having a member over 65 years and household head's employment status are associated with the incidence of CHE [28]. Among the social factors that affect levels of CHE at the population level, health insurance status and employment of the head of household are the most important in reducing levels of CHE. In contrast, having a member aged 60–65 years or older in the household is the most important factor that increases levels of CHE [15, 30,31,32,33,34]. Other evidence from India [35], Mexico [36], Turkey [37], Vietnam [38] and Burkina Faso [39] have also reported the economic status of households as a key factor influencing CHE level. In terms of health and healthcare, the frequency of using inpatient services, outpatient services, and dental care are the most important factors affecting levels of CHE [28]. This is in line with the findings from studies conducted in other settings indicating that the risk of incurring CHE increases with the frequency of using inpatient services [39,40,41].
Many studies have been conducted on CHE at a national or general population level, but fewer studies have considered CHE for specific diseases or groups of patients [28, 42]. To date, no review has been conducted of global evidence on financial hardship due to cancer. This was confirmed through searches in the following databases: JBI Database of Systematic Reviews and Implementation Reports, PubMed, ProQuest, Embase, Web of Science (via Clarivate), Campbell Collaboration, Cochrane Database of Systematic Reviews and PROSPERO. This study aims to address the gap in the literature with a systematic review and meta-analysis of evidence on patients’ exposure to CHE due to costs of cancer care, as well as factors affecting exposure to CHE. This study synthesizes results across populations and vulnerable groups to provide new insights into CHE due to cancer care and inform effective policies to redress this.
2 Methods
The review and the way it is reported is guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist [43].
2.1 Search Strategy
First, keywords were extracted from related studies, from which final search terms and their combinations were selected in collaboration with experts in health and economics, and librarians. The following platforms were searched for relevant studies: PubMed, Web of Science, Scopus, ProQuest, ScienceDirect and EMBASE, as well as Google Scholar. Search terms included ‘Catastrophe’ or ‘Catastrophic’ and ‘Cancer’ or ‘Neoplasm’ and ‘Expense*’ or ‘Financial or Cost*’ or ‘Expenditure*’ or ‘Payment*’ or ‘Spending’ (Appendix A, see electronic supplementary material [ESM]). Different combinations of the search terms were used to conduct a search of titles, abstracts, and the keywords of databases without applying any date restrictions until February 2020. All the review phases, including searching, screening, quality assessment, and data extraction were reviewed by two independent researchers (EH, LD). A third researcher’s (HHB) opinion was taken to address any discrepancies.
2.2 Inclusion Criteria
Studies that met the following criteria were included in the review:
-
Primary and secondary data analyses of CHE due to cancer.
-
Studies that investigated determinants of CHE among cancer patients.
-
Peer-reviewed publications.
-
Publications in English.
2.3 Exclusion Criteria
Methodological studies, studies that do not measure or report CHE, and studies that use approaches other than CHE to measure financial hardship were excluded.
2.4 Qualitative Evaluation of the Studies
First, the title and abstract of all identified studies were screened, from which a list of selected studies was prepared for full-text screening and quality assessment. The names of authors and journals were hidden and studies were provided to two members of the research team to consider the inclusion and exclusion criteria independently. Disagreements were resolved by a third reviewer. Following this, the quality of selected studies was evaluated using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) standard checklist [44]. This 22-part checklist qualitatively evaluates the different parts of an observation report. Checklist items are rated on a three-point scale (yes = 2, cannot tell = 1, and no = 0). The minimum and maximum potential scores using the checklist were 0 and 44. Studies evaluated for quality were divided into the following three groups: (a) low quality with score ≤ 15, (b) medium quality with score of 16–30, and (c) high quality with score ≥ 31 [45,46,47]. Only studies that acquired a score of 16 and above were selected for the meta-analysis.
2.5 Data Extraction
Data were extracted from the included studies using a data extraction table developed for the review (Table 1). The table included the name of the corresponding author, year of data collection, type of study, sample size, a quality assessment of included studies, estimated proportion of cancer patients that incurred CHE, and determinants of CHE.
2.6 Statistical Analysis
Study heterogeneity was investigated using Cochran’s Q and I2 index. An I2 >50% or a p value for the Q test < 0.10 indicates significant heterogeneity [17]. Since the results of Q test and I2 index indicated significant heterogeneity between the studies, a random effects model was used for meta-analysis and synthesized results were obtained from the Comprehensive Meta-Analysis (CMA) software, version 3. The possibility of publication bias was assessed using visual inspection of a funnel plot.
The combined effect of the studies based on the random effects model was obtained using CMA software, version 3. Some studies reported exposure to CHE using more than one method and threshold, in which case each method or threshold used was considered separately in the meta-analysis. In order to investigate determinants of CHE due to cancer, factors considered in included studies were collated and grouped into patient level and household level factors. Each determining factor is reported descriptively with the direction of the relationship (positive or negative), based on the number of times a given factor was considered in included studies.
3 Results
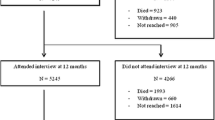
The search strategy captured 462 studies from the databases, and through a search of the reference list of studies included. Figure 1 charts the screening process of studies captured and reasons for exclusion at different stages. After the removal of duplicates and screening the titles and abstract, 33 articles met the inclusion criteria for full-text assessment. Following full-text screening, 19 studies were selected for the meta-analysis and key descriptive features of these are presented in Table 1. Additionally, determinants of CHE in included studies are shown in Table 2. The maximum rate of CHE due to cancer is estimated in the study by Tripathy et al. [48] in India with 74% of 1093 cancer patients incurring CHE, and the minimum rate of CHE was reported in the study by Choi et al. [49] in Korea with 6.2% of 3684 sampled households of cancer patients incurring CHE.
The analysis of publication bias using Egger's line regression test suggested the absence of statistically significant publication bias (p > 0.05). A visual inspection of the symmetry graphic in the funnel plot indicated no evidence of publication bias or small-study effects (Fig. 2). The p values for the Egger’s tests were 0.25 and 0.16, respectively, which suggests no bias in the results of included studies.
The Cochran Q test was statistically significant (p < 0.01), which indicates the presence of heterogeneity in the effect sizes of included studies, but the Q test is sensitive to an increase of effect size. The power of this test for investigating heterogeneity improves as the number of effect sizes increases. For this reason, I-square (I2) statistics, another commonly used index for heterogeneity, was employed. The index has values of 0–100, reporting heterogeneity as percentage values. A I2 value close to 100 indicates more heterogeneity in the effect sizes of studies considered [50]. In this case, I2 showed that 99.09% of the dispersion in levels of CHE reported in the studies analyzed is due to the moderator variables.
The results of the studies estimating the rate of CHE among households of cancer patients are reported in Fig. 3, including the rate estimated in each study, confidence intervals and combined results.
The overall rate of CHE among cancer patients, across studies, was estimated as 43.3% based on the random effects model (95% CI 36.7–50.1).
Given that different methods and thresholds were used to calculate the rate of CHE in the studies, a sub-group analysis was conducted based on the methods used to calculate CHE. The highest rate of CHE was found among the group of studies that used OOP > 10% of household income/expenditure (OOP ≥ 10% income) (Fig. 4). In this group, the rate of CHE incurred by households of cancer patients was calculated as 62.7%. The lowest rate of CHE was found among the group of studies that used OOP > 20% of household income/expenditure (OOP ≥ 20% income). In this group, the rate of CHE incurred by households of cancer patients was calculated as 16.7%.
The rate of CHE in households of cancer patients was grouped by countries based on the human development index (HDI), presented in Fig. 5. Countries were grouped into four HDI categories: (a) low HDI (0.350–0.554), (b) medium HDI (0.555–0.699), (c) high HDI (0.700–0.799), and (d) very high HDI (0.800–1.000). The average rate of CHE incurred by cancer patients was 23.4% in countries with very high HDI (South Korea, USA), 30.3% in countries with high HDI (Iran, China, Malaysia, Thailand), 52.1% in countries with medium HDI (Vietnam, Lao PDR, Indonesia, Philippines, India, Cambodia and Myanmar), and 67.9% in countries with low HDI (Haiti). The overall rate of CHE among cancer patients, across groups of countries based on the HDI, was estimated as 36.9% based on the random effects model with a 95% confidence interval of 31.2–43.1.
Meta regression was used to investigate the relationship between the rate of CHE incurred by cancer patients and HDI and a given study sample size. A statistically significant (p = 0.003) and negative relationship was found between the rate of CHE and study sample size. In other words, the rate of CHE decreases as the study sample size increases (Fig. 6). Results of the meta-regression also showed a statistically significant (p = 0.001) and negative relationship between HDI and the rate of CHE among cancer patients, where the latter decreases as HDI increases (Fig. 7).
3.1 Factors Affecting the Rate of Catastrophic Health Expenditure (CHE) Due to Cancer Care at the Patient Level
The type of health insurance and possession of supplemental insurance are key factors affecting the rate of CHE in cancer patients. Patients who have any type of insurance or prepayment mechanism that either covers extensive health services or has lower co-insurance or copayment rates are less exposed to CHE [51,52,53,54,55,56]. Gender, age and the education level of patients are some of the other factors affecting exposure to CHE. In general, females, the elderly and the less educated are more exposed to CHE [26, 53,54,55].
The type of treatment, location of the cancer in the body, stage of cancer and time period of cancer diagnosis are among the key clinical factors affecting the exposure of cancer patients to CHE [25, 26, 51, 52, 54, 55]. In the study conducted in Namazi hospital, Iran, patients receiving chemotherapy were exposed to a higher rate of CHE than patients receiving other medical treatments [51]. However, in a study conducted in the US by Davidoff et al. (2013), the patients treated by radiation and antineoplastics were more likely to incur CHE than other treatments [55]. The type and location of cancers resulting in the highest rates of CHE included liver cancer, gastrointestinal cancer, cancers related to the stomach, thoracic cancers, and respiratory cancers [26, 54].
In general, the rate of CHE increases with the progression of cancer from stages I to IV [54]. In addition, patients are most likely to incur CHE in the first year of disease diagnosis rather than following years [52]. In terms of the type of health service, the probability of incurring CHE increased as outpatient services and referrals to high-level hospitals increased [51, 53]. There is a relationship between the rate of CHE and the need for other family members to forego seeking care due to financial barriers, as well as the health-seeking behavior of patients at the time of disease [51, 55]. Given that the likelihood of patients and other household members to forego health services increases as household finances decrease, the probability of incurring CHE increases [51]. In addition, patients who seek health care with the minimum sense of malaise are more exposed to CHE [55].
The quality of life of patients is also one of the factors affecting exposure to CHE, which decreases as quality of life increases [26, 54]. In addition, Hierarchical Coexisting Conditions (HCCs) and functional status limitations of cancer patients have a direct relationship to exposure to CHE [55].
3.2 Factors Affecting the Rate of CHE Due to Cancer Care at the Household Level
Age, gender, the educational level of the head of household, number of household members, the marital status of the head of household, having health insurance, job status, disability in the household, the presence of elderly household members and self-rated health are among the factors affecting the rate of CHE among households of cancer patients (Table 3). In general, the older heads of households [52], female headed households [25, 52], less educated heads of households [52], the presence of a member above 65 years old in the household [56], married heads of households [52, 55], lack of health insurance [54], unemployment of headed households [54], the presence of a disable person in the household [56], presence of household members with chronic disease [56], bad self-rated health [52], small household size [52], and households living further away from medical centers [51] all increase the rate of CHE in households of cancer patients [25, 49, 52,53,54,55,56]. Household income [55], the percentage of costs incurred that are covered by health insurance [53] and not having paid work [54] are among the economic factors affecting the rate of CHE at the household level.
4 Discussion
This review identified various aspects of CHE management that can be tailored to achieve goals such as risk-sharing, cross-subsidization, financial protection of households and financial scheme viability. Firstly, it suggests that policy makers use prepaid and pooled mechanisms in the main public health insurance funds. This review suggests that community-based health insurance schemes can include poor people, including people and households below the poverty line [28, 57]. Factors that may facilitate inclusion of the poor include an affordable premium, external assistance and nesting the scheme within a larger organization that addresses other needs of the poor [27, 28, 35, 37, 46, 58]. Secondly, the financial risk borne by a scheme can be limited by placing a cap on the benefits provided. However, this also limits the extent of risk-pooling and cross-subsidization provided by the scheme. There will inevitably be cases where hospital expenditures far exceed this cap, with dire financial consequences for the insured [5, 8, 16, 26, 30, 33, 36, 57, 59]. Thirdly, in order to relieve the financial burden of expenditure on households, reimbursement under a scheme should be fast and easy. This needs administration of the scheme, particularly processing of claims, to happen as close to claimants as possible [19, 23, 36, 49, 52, 59,60,61].
Based on the review and meta-analysis results, the rate of CHE in households of cancer patients was estimated as 43.3% (CI 36.7–50.1). This is largely in line with the prevalence of perceived financial hardship in households of cancer patients, estimated to be between 14.8 and 78.8% during 2003–2013 in a systematic review by Azzani et al. [59].
A study by Xu et al. [30] that investigated health expenditure in 89 countries found that 150 million people incur CHE annually. In this study, there is a large difference in the rate of CHE between countries, with patients in low- or middle-income countries more exposed to CHE than in high-income countries [30]. Results from this study support the range of CHE across countries found by Xu et al. [30]. Cochran’s Q and I2 heterogeneous indicators showed that there is substantial heterogeneity between the rate of CHE in cancer studies depending on the country in which the study is based due to variations in economic, social, cultural and geographic aspects. In general, the rate of CHE among cancer patients had a negative and direct relationship with country HDI scores.
The presence and type of health insurance was one of the most important determinants of exposure to CHE across the studies. Patients with better insurance coverage (i.e., with better benefit packages or with low co-insurance rates) were less exposed to CHE. In a study conducted in Namazi hospital, Shiraz, cancer patients with Relief Committee insurance and armed forces insurance were less exposed to CHE than patients covered by other health insurance schemes [51]. Another study in Anhui, China, showed that patients with city employee medical insurance (CEMI) and city resident medical insurance (CRMI) were less exposed to CHE compared with patients covered by other health insurance schemes [53].
The age and gender of patients are two other factors determining the rate of CHE among cancer patients [26, 54]. Female patients were exposed to higher rates of CHE. This may be driven by the health-seeking behavior of female patients, who may seek care more often and thus incur more health expenditure than males [52]. Elderly patients were also more exposed to CHE in most studies. In general, elderly patients are less able to engage in economic activities and are more vulnerable to falling ill with cancer or other diseases. Health services and corresponding health expenditures are therefore usually higher for elderly patients than for younger patients [52, 53].
The possession of supplementary health insurance and higher levels of education were both factors that reduced the rate of CHE among cancer patients [53,54,55]. This may be driven by findings that a higher level of education can facilitate higher gains in health for a given level of health expenditure [62]. However, a study conducted by Panahi et al. [63] in the public hospitals of Tabriz, Iran, showed that higher levels of education increased the rate of CHE because higher levels of education increased awareness of available health services and healthcare. In other words, people with higher levels of education use more advanced/expensive health services and technologies compared with the less educated, thus increasing the likelihood of higher-educated people incurring CHE.
Using outpatient services, the health-seeking behavior of patients, and the need to forego health services due to financial barriers are also factors that affected the rate of CHE in cancer patients [51, 55]. Zhao et al. [53] showed that an additional chronic non-communicable disease was associated with an increase in the number of outpatient visits (incidence rate ratio 1·29, 95% CI 1·27–1·31), and the number of days spent in hospital as an inpatient (1·38, 95% CI 1·35–1·41) [64].
Household economic status is also a key factor determining CHE [65]. Azzani et al. [66] found that socioeconomic inequality plays an important role in the incidence of CHE across countries and that low-income households are at high risk of CHE and financial hardship from healthcare payments. Kavosi et al. [51] found that of patients who undergo chemotherapy, 74.1% faced CHE. Evidence showed that households located in the wealthier areas were at lower risk of CHE than poorer regions. Poorer households are more affected by CHE due to the long duration of cancer treatment and high costs of a cancer diagnosis and treatment [65]. A significant correlation has been reported between the type of treatment and incurring CHE.
The amount of time after cancer diagnosis as well as the stage of cancer were among the factors determining exposure to CHE in the studies [52, 54]. Based on the results from Choi et al. [52], households with cancer patients that are 1–2 years post-diagnosis were more likely to experience CHE compared with households of newly-diagnosed cancer patients (OR 1.78 and 1.36, respectively). Patients with stomach, ovarian, gastrointestinal, respiratory, and thoracic digestive cancers were exposed to the highest rates of CHE among the studies [53, 54].
The type of hospital and treatment received were also associated with CHE. Patients seeking care at higher level hospitals incurred higher expenditures than those at lower level hospitals. Patients seeking care at higher level hospitals had more serious conditions, and referrals to higher level hospitals therefore increase the probability of incurring CHE due to more expensive health services/procedures and severity of disease. A study conducted by Zhao et al. [53] in China showed that the exposure to CHE in cancer patients referring to prefecture and provincial hospitals was higher than in patients receiving care in other hospitals. Cancer patients require different treatments such chemotherapy, radiotherapy, hormone therapy, surgery, and medicine. Expenditures on these treatments vary across different countries. The expenditure on each treatment is affected by different country-level factors such as the advancement of medical sciences, technology, knowledge of medical equipment and drug production, as well as the economic and political conditions of countries for importing equipment and medicine. The study by Kavosi et al. [51] in Iran showed that patients who used chemotherapy were more likely to incur CHE than patients who used other treatments. However, another study conducted by Davidoff et al. [55] in the US found that patients who used radiation and antineoplastic drugs were more exposed to CHE.
At the household level, household income and the education level of the head of household are key factors that reduce the exposure of households of cancer patients to CHE [25, 26, 52,53,54,55,56]. Households with more educated heads of household are less exposed to CHE [52]. Based on the obtained results, higher economic status, income and wealth [52, 54, 55] reduce the probability of incurring CHE by improving the available finances for health in households. In the study by Zhao et al. [53], households where the head of household experienced a change in job status from employed to unemployed, and households where the head of household was unemployed with no change, were more likely to incur CHE compared with households who did not experience a change in employment status. Self-employment of household heads increases the rate of CHE because the self-employed have no fixed salary and their employment is not permanent, rather it is often periodic and seasonal [56].
The age and gender of the head of household are other factors affecting the probability of incurring CHE [25, 52]. The probability of developing health problems increases along with age. Older heads of households may therefore contribute less to household income but increase household health expenditures as they need more healthcare and thus increase the probability of incurring CHE [11, 52]. Accordingly, studies found that the presence of a household member over 65 years old with chronic diseases increased the rate of CHE [56]. With regards to gender, male heads of households have more job opportunities and can receive higher incomes than their female counterparts. Female heads therefore rely more on financial support from their children and retirement pensions of their husbands [52, 53]. For this reason, households with female heads experience higher rates of CHE [63].
Several other household-level factors influence exposure to CHE, namely the possession of health insurance, self-reported health status, distance from the nearest health facility, marital status and the household size. Possessing health insurance can improve household access to health services [54]. Furthermore, health insurance pre-payments reduce out-of-pocket payments for health services and therefore have the potential to lower the rate of CHE incurred by households [53]. While health insurance can be a protective factor against CHE, the extent to which health insurance schemes can protect against CHE needs to be considered, particularly for households living in rural areas [58]. According to the WHO, to reduce the risk of CHE, insurance schemes should be designed to include a mandatory benefits package—which is being done by a growing number of countries to progress toward universal coverage [67]. In addition, insurance coverage should be extended and cost- and risk-sharing arrangements need to be reformed [68].
With regards to health status, household heads with poorer health status are exposed more to CHE because poorer self-assessment indicates worse health conditions and health-seeking behaviors [52]. The rate of CHE increases as proximity to a health facility decreases due to increased expenditures incurred for travel, accommodation, and food [51]. In the study by Azzani et al. [59], household income, distance from a hospital, being a single parent and patients with impeded social, emotional and physical performance are the factors affecting perceived financial difficulty by patients and their households. However, results from included studies were mixed on the effect of the marital status of household heads on CHE, with some finding an increase in exposure to CHE [52, 55] and others a reduction [54]. In the study by Panahi et al. [63], the rate of CHE was found to be lower in hospitalized patients of households with single heads. Single heads of households have fewer individuals under their guardianship, and these households can therefore incur less health expenditures [63]. In the study by Choi et al. [60], households with two to four members had higher rates of CHE. However, in general, most studies found that the rate of CHE increases as the size of households increase because household expenditure increases while household income does not necessarily increase [61, 69]. Thus, the ability to pay often decreases among larger households and the probability of exposure to CHE increases.
4.1 Study Limitations
There are a few key limitations to this review that are important to consider. First, the review only considered articles published in English. A number of studies in other languages, have therefore likely been missed. Second, the review only included observational studies, and the relationship between determining factors in the households of cancer patients and other high-quality evidence (RCT, cohort, case–control) has been investigated. Therefore, the rate of CHE could not be clearly delineated. Third, insufficient information was available to calculate gender-based prevalence of CHE or risk factors that can have a significant impact on CHE. Fourth, although sub-group analyses were carried out by HDI, high heterogeneity existed among some other variables. Fifth, CHE is defined using different thresholds (ranging from 10 to 40%) in included studies. While sub-group analyses were conducted to estimate CHE incidence for each threshold, all of the different thresholds were included for the meta-regression and when identifying determinants of CHE because of insufficient data to consider each threshold in isolation. Sixth, no sensitivity analysis was performed on these data, because of high heterogeneity.
5 Conclusion
Reviewed studies of health expenditures among cancer patients in different countries indicate substantial exposure of these patients and their households to CHE. Nearly half of cancer patients are exposed to CHE, and this rate is especially high in countries with lower HDI scores. The exposure of cancer patients to CHE is driven by the expensive care required, and demonstrates shortfalls in health financing mechanisms resulting in unfair financial contribution in the health system. A number of factors at the patient and household affecting exposure of cancer patients to CHE were identified and synthesized. Incidence of CHE among patients with cancer do not automatically disappear with rising income. Health financing systems not only should allow patients with cancer to access health services when they need to, but also protect households from financial catastrophe by reducing OOPs.
Change history
07 October 2021
A Correction to this paper has been published: https://doi.org/10.1007/s40258-021-00686-w
References
Doshmangir L, Sajadi HS, Ghiasipour M, Aboutorabi A, Gordeev VS. Informal payments for inpatient health care in post-health transformation plan period: evidence from Iran. BMC public health. 2020;20(1):1–4.
Jakovljevic M, Timofeyev Y, Ekkert NV, Fedorova JV, Skvirskaya G, Bolevich S, et al. The impact of health expenditures on public health in BRICS nations. J Sport Health Sci. 2019;8(6):516.
Doshmangir L, Bazyar M, Rashidian A, Gordeev VS. Iran health insurance system in transition: equity concerns and steps to achieve universal health coverage. Int J Equity Health. 2021;20(1):1–14.
Moghadam MN, Banshi M, Javar MA, Amiresmaili M, Ganjavi S. Iranian household financial protection against catastrophic health care expenditures. Iran J Public Health. 2012;41(9):62.
Grima S, Spiteri JV, Jakovljevic M, Camilleri C. High out-of-pocket health spending in countries with a Mediterranean connection. Front Public Health. 2018;6:145.
Jakovljevic MB. BRIC’s growing share of global health spending and their diverging pathways. Front Public Health. 2015;3:135.
Jakovljevic M, Camilleri C, Rancic N, Grima S, Jurisevic M, Grech K, et al. Cold war legacy in public and private health spending in Europe. Front Public Health. 2018;6:215.
Rezaei S, Hajizadeh M, Ahmadi S, Sedghi S, Piroozi B, Mohamadi-Bolbanabad A, Homaie Rad E. Socioeconomic inequality in catastrophic healthcare expenditures in Western Iran: A decomposition analysis. International Journal of Social Economics. 2019;46(9):1049–60.
Moradi G, Safari H, Piroozi B, Qanbari L, Farshadi S, Qasri H, et al. Catastrophic health expenditure among households with members with special diseases: a case study in Kurdistan. Med J Islam Repub Iran. 2017;31:43.
Aghajani H, Etemad K, Goya MM, Ramezani R, Modirian M, Nadali F. Iranian Annual of National Cancer Registration Report. 2008-2009. 1st ed. Tehran: Tandis 2011:25–120
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7–30.
Barr RD, Feeny D, Furlong W. Economic evaluation of treatments for cancer in childhood. Eur J Cancer. 2004;40(9):1335–45.
Massa I, Balzi W, Altini M, Bertè R, Bosco M, Cassinelli D, Vignola V, Cavanna L, Foca F, Dall’Agata M, Nanni O. The challenge of sustainability in healthcare systems: frequency and cost of diagnostic procedures in end-of-life cancer patients. Supportive Care in Cancer. 2018;26(7):2201–2208.
Berki S. A look at catastrophic medical expenses and the poor. Health Aff. 1986;5(4):138–45.
Yabroff KR, Dowling EC, Guy GP Jr, Banegas MP, Davidoff A, Han X, et al. Financial hardship associated with cancer in the United States: findings from a population-based sample of adult cancer survivors. J Clin Oncol. 2016;34(3):259.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Longo CJ, Deber R, Fitch M, Williams AP, D’Souza D. An examination of cancer patients’ monthly “out-of-pocket” costs in Ontario, Canada. Eur J Cancer Care. 2007;16(6):500–7.
Asante A, Price J, Hayen A, Jan S, Wiseman V. Equity in health care financing in low-and middle-income countries: a systematic review of evidence from studies using benefit and financing incidence analyses. PLoS One. 2016;11(4):e0152866.
Wagstaff A. Measuring financial protection in health. Washington: World Bank Publications; 2008.
Abolhallaje M, Hasani S, Bastani P, Ramezanian M, Kazemian M. Determinants of catastrophic health expenditure in Iran. Iran J Public Health. 2013;42(Supple1):155.
Darvishi A, Amini-Rarani M, Mehrolhassani MH, Yazdi-Feyzabadi V. Fairness in household financial contribution to the Iran’s healthcare system from 2008 to 2018. BMC Research Notes. 2021;14(1):1–5.
Kutzin J. Health financing for universal coverage and health system performance: concepts and implications for policy. Bull World Health Organ. 2013;91(8):602–11.
Murray CJ, Xu K, Klavus J, Kawabata K, Hanvoravongchai P, Zeramdini R, et al. Assessing the distribution of household financial contributions to the health system: concepts and empirical application. Health systems performance assessment: debates, methods and empiricism, vol. 12. Geneva: World Health Organization; 2003.
Azzani M, Yahya A, Roslani AC, Su TT. Catastrophic health expenditure among colorectal cancer patients and families: a case of Malaysia. Asia Pac J Public Health. 2017;29(6):485–94.
The ACTION Study Group. Financial catastrophe, treatment discontinuation and death associated with surgically operable cancer in South-East Asia: Results from the ACTION Study. Surgery. 2015;157(6):971–82.
Aregbeshola BS, Khan SM. Determinants of catastrophic health expenditure in Nigeria. Eur J Health Econ. 2018;19(4):521–32.
Doshmangir L, Yousefi M, Hasanpoor E, Eshtiagh B, Haghparast-Bidgoli H. Determinants of catastrophic health expenditures in Iran: a systematic review and meta-analysis. Cost Eff Resour Alloc. 2020;18:1–21.
Rezaei S, Woldemichael A, Hajizadeh M, Kazemi Karyani A. Catastrophic healthcare expenditures among Iranian households: a systematic review and meta-analysis. International Journal of Human Rights in Healthcare. 2019;12(2):105–15.
Xu K, Evans DB, Carrin G, Aguilar-Rivera AM, Musgrove P, Evans T. Protecting households from catastrophic health spending. Health Aff. 2007;26(4):972–83.
Ghosh S. Catastrophic Payments and Impoverishment due to Out-of-Pocket Health Spending. Economic & Political Weekly. 2011;46(47):63.
Joglekar R. Can insurance reduce catastrophic out-of-pocket health expenditure? Indira Gandhi Institute of Development Research, Mumbai, 2012:112(1);2–29
Limwattananon S, Tangcharoensathien V, Prakongsai P. Equity in financing healthcare: impact of universal access to healthcare in Thailand. 2008;1(1577):1–36.
Somkotra T, Lagrada LP. Which households are at risk of catastrophic health spending: experience in Thailand after universal coverage: exploring the reasons why some households still incur high levels of spending—even under universal coverage—can help policymakers devise solutions. Health Aff. 2009;28(Suppl1):w467–78.
Mondal S, Lucas H, Peters D, Kanjilal B. Catastrophic out-of-pocket payment for healthcare and implications for household coping strategies: evidence from West Bengal, India. Economics Bulletin. 2014;34(2):1303–16.
Galárraga O, Sosa-Rubí SG, Salinas-Rodríguez A, Sesma-Vázquez S. Health insurance for the poor: impact on catastrophic and out-of-pocket health expenditures in Mexico. Eur J Health Econ. 2010;11(5):437–47.
Yardim MS, Cilingiroglu N, Yardim N. Catastrophic health expenditure and impoverishment in Turkey. Health Policy. 2010;94(1):26–33.
Van Minh H, Phuong NTK, Saksena P, James CD, Xu K. Financial burden of household out-of pocket health expenditure in Viet Nam: findings from the National Living Standard Survey 2002–2010. Soc Sci Med. 2013;96:258–63.
Su TT, Kouyaté B, Flessa S. Catastrophic household expenditure for health care in a low-income society: a study from Nouna District, Burkina Faso. Bull World Health Organ. 2006;84:21–7.
Adhikari SR, Maskay NM, Sharma BP. Paying for hospital-based care of Kala-azar in Nepal: assessing catastrophic, impoverishment and economic consequences. Health Policy Plan. 2009;24(2):129–39.
Wagstaff A, Doorslaer EV. Catastrophe and impoverishment in paying for health care: with applications to Vietnam 1993–1998. Health Econ. 2003;12(11):921–33.
Bazyar M, Pourreza A, Harirchi I, Akbari F, Mahmoudi M. Medical and non-medical direct costs of cancers in patients hospitalized in Imam Khomeini cancer institution-2010. Hospital. 2012;11(1):39–50.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9.
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Declaración de la Iniciativa STROBE (Strengthening the Reporting of Observational studies in Epidemiology): directrices para la comunicación de estudios observacionales. Gac Sanit. 2008;22(2):144–50.
Gheshlagh RG, Parizad N, Zahednezhad H, Sarokhani M, Sayehmiri K, Baghi V. Prevalence of restless leg syndrome in Iran: a systematic review and metanalysis. J Sleep Sci. 2016;1(3):131–8.
Ahmady S, Khajeali N, Sharifi F, Mirmoghtadaei ZS. Factors related to academic failure in preclinical medical education: a systematic review. J Adv Med Educ Prof. 2019;7(2):74.
Chen S-J, Shi L, Bao Y-P, Sun Y-K, Lin X, Que J-Y, et al. Prevalence of restless legs syndrome during pregnancy: a systematic review and meta-analysis. Sleep Med Rev. 2018;40:43–54.
Tripathy J, Prasad B, Shewade H, Kumar A, Zachariah R, Chadha S, et al. Cost of hospitalisation for non-communicable diseases in India: are we pro-poor? Trop Med Int Health. 2016;21(8):1019–28.
Choi J-W, Choi J-W, Kim J-H, Yoo K-B, Park E-C. Association between chronic disease and catastrophic health expenditure in Korea. BMC Health Serv Res. 2015;15(1):26.
Ghorbanizadeh V NT. Practical Guide meta-analysis software CMA2: Tehran: Jameshenasan; 2009;1:1–102
Kavosi Z, Delavari H, Keshtkaran A, Setoudehzadeh F. Catastrophic Health Expenditures and Coping Strategies in Households with Cancer Patients in Shiraz Namazi Hospital. Middle East Journal of Cancer. 2014;5(1):13–22.
Choi J-W, Cho K-H, Choi Y, Han K-T, Kwon J-A, Park E-C. Changes in economic status of households associated with catastrophic health expenditures for cancer in South Korea. Asian Pac J Cancer Prev APJCP. 2014;15(6):2713–7.
Zhao T, Cheng J, Chai J, Feng R, Liang H, Shen X, et al. Inpatient care burden due to cancers in Anhui, China: a cross-sectional household survey. BMC Public Health. 2016;16(1):308.
ACTION Study Group. Catastrophic health expenditure and 12-month mortality associated with cancer in Southeast Asia: results from a longitudinal study in eight countries. BMC Med. 2015;13(1):190.
Davidoff AJ, Erten M, Shaffer T, Shoemaker JS, Zuckerman IH, Pandya N, et al. Out of pocket health care expenditure burden for Medicare beneficiaries with cancer. Cancer. 2013;119(6):1257–65.
Kim JH, Kim SJ, Kwon SM. Effect of expanding benefit coverage for cancer patients on equity in health care utilization and catastrophic expenditure. Health Policy Manag. 2014;24(3):228–41.
Bazyar M, Rashidian A, Sakha MA, Mahdavi MRV, Doshmangir L. Combining health insurance funds in a fragmented context: what kind of challenges should be considered? BMC Health Serv Res. 2020;20(1):1–14.
Thu Thuong NT, Van Den Berg Y, Huy TQ, Tai DA, Anh BNH. Determinants of catastrophic health expenditure in Vietnam. Int J Health Plan Manag. 2020;36(2):316–33.
Azzani M, Roslani AC, Su TT. The perceived cancer-related financial hardship among patients and their families: a systematic review. Support Care Cancer. 2015;23(3):889–98.
Choi JW, Kim TH, Jang SI, Jang SY, Kim W-R, Park EC. Catastrophic health expenditure according to employment status in South Korea: a population-based panel study. BMJ Open. 2016;6(7):e011747.
Zheng A, Duan W, Zhang L, Bao X, Mao X, Luo Z, et al. How great is current curative expenditure and catastrophic health expenditure among patients with cancer in China? A research based on “System of Health Account 2011.” Cancer Med. 2018;7(8):4036–43.
Grossman, Michael, The Human Capital Model of the Demand for Health (April 1999). NBER Working Paper No. w7078, Available at SSRN: https://ssrn.com/abstract=206128
Panahi H, Janati A, Narimani M, Assadzadeh A, Mohammadzadeh P, Naderi A. Catastrophic expenditures for hospitalized patients in Tabriz, Iran. Payesh (Health Monitor). 2014;13(6):655–63.
Zhao Y, Atun R, Oldenburg B, McPake B, Tang S, Mercer SW, et al. Physical multimorbidity, health service use, and catastrophic health expenditure by socioeconomic groups in China: an analysis of population-based panel data. Lancet Glob Health. 2020;8(6):e840–9.
Li Y, Wu Q, Xu L, Legge D, Hao Y, Gao L, et al. Factors affecting catastrophic health expenditure and impoverishment from medical expenses in China: policy implications of universal health insurance. Bull World Health Organ. 2012;90:664–71.
Azzani M, Roslani AC, Su TT. Determinants of household catastrophic health expenditure: a systematic review. Malays J Med Sci MJMS. 2019;26(1):15.
Glassman A, Chalkidou K. Priority-setting in health: building institutions for smarter public spending. Washington, DC: Center for Global Development; 2012.
World Health Organization. Health financing strategy for the Asia Pacific Region (2010–2015): WHO Regional Office for South-East Asia. 2009;1–52.
Piroozi B, Zarei B, Ghaderi B, Safari H, Moradi G, Rezaei S, Ghaderi M, Amirhosseini S, Mohamadi-Bolbanabad A. Catastrophic health expenditure and its determinants in households with gastrointestinal cancer patients: evidence from new health system reform in Iran. International Journal of Human Rights in Healthcare. 2019;12(4):249–57.
Moghimi M, Imam-Zamiri R, Feizi AA, Rostamkhani MH, Ghormani R. The rule-of-law function of 11 – 520000 governments in supporting and reducing the Catastrophic health expenditure cancer patients in Zanjan province in 2008-2009. Health system. 2009:1(2);41–46.
Mahal A, Karan A, Engelgau M. The economic implications of non-communicable disease for India. The International Bank for Reconstruction and Development, NWWashington, DC 20433, 2010;1–142
O'Neill KM, Mandigo M, Pyda J, Nazaire Y, Greenberg SL, Gillies R, Damuse R. Out-of-pocket expenses incurred by patients obtaining free breast cancer care in Haiti: A pilot study. Surgery. 2015;158(3):747–55.
Leng A, Jing J, Nicholas S, Wang J. Catastrophic health expenditure of cancer patients at the end-of-life: a retrospective observational study in China. BMC palliative care. 2019;18(1):1–0.
Lee M, Yoon K. Catastrophic health expenditures and its inequality in households with cancer patients: a panel study. Processes. 2019;7(1):39.
Lee M, Yoon K, Choi M. Private health insurance and catastrophic health expenditures of households with cancer patients in South Korea. European journal of cancer care. 2018;27(5):e12867
Acknowledgements
The authors would like to thank the Research Center for Evidence-Based Health Management at Maragheh University of Medical Sciences for support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This article does not contain any studies with human participants or animals performed by any of the authors. Approval was not required for this study.
Consent for publication
Not required.
Availability of data and material
No additional data available.
Conflict of interest
All authors declare no competing interests.
Funding
Research support was provided by Tabriz Health Services Management Research Center at Tabriz University of Medical Sciences.
Authors' contributions
EH and LD did the literature review. EH and BE found the full text of some articles that were difficult to find. EH, LD and GJAJ designed the study. LD and HHB abstracted study information and additional data and assessed study quality. GJAJ, LD and HHB wrote the paper.
Informed consent
Not required.
Additional information
The original Online version of this article was revised : The co-author's affiliation has been incorrectly published.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Doshmangir, L., Hasanpoor, E., Abou Jaoude, G.J. et al. Incidence of Catastrophic Health Expenditure and Its Determinants in Cancer Patients: A Systematic Review and Meta-analysis. Appl Health Econ Health Policy 19, 839–855 (2021). https://doi.org/10.1007/s40258-021-00672-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-021-00672-2