Abstract
Background
In Australia, as in many other Western countries, patient surveys suggest the costs of medicines lead to deferring or avoiding filling of prescriptions. The Australian Pharmaceutical Benefits Scheme provides approved prescription medicines at subsidised prices with relatively low patient co-payments. The Pharmaceutical Benefits Scheme defines patient co-payment levels per script depending on whether patients are “concessional” (holding prescribed pension or other government concession cards) or “general”, and whether they have reached a safety net defined by total out-of-pocket costs for Pharmaceutical Benefits Scheme-approved medicines.
Objective
The purpose of this study was to explore the impact of costs on adherence to statins in this relatively low-cost environment.
Methods
Using data from a large-scale survey of older Australians in the state of New South Wales linked to administrative data from the national medical and pharmaceutical insurance schemes, we explore the relationships between adherence to medication regimes for statins and out-of-pocket costs of prescribed pharmaceuticals, income, other health costs, and a wide set of demographic and socio-economic control variables using both descriptive analysis and logistic regressions.
Results
Within the general non-safety net group, which has the highest co-payment, those with lowest income have the lowest adherence, suggesting that the general safety threshold may be set at a level that forms a major barrier to statin adherence. This is reinforced by over 75% of those who were not adherent before reaching the safety net threshold becoming adherent after reaching the safety net with its lower co-payments.
Conclusion
The main financial determinant of adherence is the concessional/general and safety net category of the patient, which means the main determinant is the level of co-payment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Adherence to statins by patients is associated with the size of the patient co-payment. |
The most affected group is the non-concessional patients with lower incomes, suggesting changed thresholds including the option of stepped thresholds may improve community health outcomes. |
Other factors impacting on adherence to statins including language spoken at home have direct policy implications. |
1 Background
In Australia, as in many other Western countries, patient surveys suggest the costs of medicines lead to deferring or avoiding filling of prescriptions [1, 2]. The Australian Pharmaceutical Benefits Scheme (PBS) provides approved prescription medicines with relatively low patient co-payments, leading to the question of why this is observed in Australia. This study explores the role of costs in adherence to statins.
Surveys report variable impacts of cost on medication adherence in Australia, with from 8% of all people to 23% of people who experience financial stress delaying or not using a prescribed medication owing to cost [1,2,3]. Increased patient costs were associated with lower medication adherence [4], and poorer health outcomes. Increases in prescription co-payments in 2005 were associated with reductions in prescriptions dispensed, with the largest reductions where there were over-the-counter alternatives, or where symptoms did not change with the medication [5]. In the UK [6], factors such as the severity of symptoms or the disease or whether patients found the medicine effective and necessary played a greater role than cost in decisions to fill prescriptions [6, 7]. An Australian discrete choice survey [8] found that perceived harms and benefits of medications were the most relevant factors in decisions about continuing medication.
Warren et al. [9] explored non-cost factors influencing adherence in the long-term use of statins in Australia and found older people were more adherent while those who speak a language other than English at home, those who smoke and those under psychological stress were less likely to adhere to prescribed statins. An extension of this study concluded that continuity of general practitioner (GP) care also influences adherence [10].
1.1 Australian Institutional Arrangements
The Australian healthcare system comprises public and private components including private health insurance. Programmes are managed at both national and state levels. The programmes relevant to this project are funded and managed by the national government, and comprise the PBS, and the Medicare Benefits Schedule (MBS), which supports the use of private medical services for private patients both out of hospital and in hospital, with a rebate fixed for each specific medical service. Both the MBS and PBS can involve patient co-payments.
The PBS funds approved prescribed pharmaceuticals, with patients required to make a fixed co-payment for each prescription and the PBS covering the remaining cost. Patients are classified as concessional or general with more than one in four Australians holding a concession card [11]. The PBS safety net operates on a family basis, with all members contributing towards meeting a spending threshold and all moving to lower co-payments once that threshold is reached. The co-payment for each PBS prescription depends on the patient category, labelled in this study as concessional non-safety net, concessional safety net (CSN), general non-safety net (GNSN) and general safety net (GSN). Table 1 shows the co-payments from January 2016.
Some prescriptions are priced below co-payment levels, for example most common antibiotics are priced below the general co-payment. Patients pay the full cost of these prescriptions with the PBS making no payment and these prescriptions are not recorded in the PBS system. While prices for the statins explored in this study are now below the general co-payment, this study relates to a period prior to the availability of most generic statin formulations on the PBS. As only 5.4% of statin purchases by concessional patients fell below the general co-payment level, reasonably complete information is available for all categories of patients.
This article, which expands previous analyses [9, 10], is part of a larger study addressing the role of costs in medication adherence through exploring the role of safety nets and other health costs potentially associated with adherence. We report here on the study of statins as they are an important life-saving class of medicines with effectiveness directly related to adherence, but because they treat asymptomatic disease are potentially sensitive to costs.
2 Methods and Data
2.1 Background to the Data Used
The principal data source is the Sax Institute’s 45 and Up Study [12], which is based on the population of the state of New South Wales, Australia. Prospective participants were randomly sampled from the enrolment base of Medicare Australia, which provides near-complete coverage of the population. People 80+ years of age and residents of rural and remote areas were oversampled. A total of 267,086 participants joined the study by completing a baseline questionnaire (between January 2006 and December 2009) and giving signed consent for follow-up and linkage of their information to routine health databases. About 18% of those invited participated and participants included about 11% of the New South Wales population aged 45 years and over. The representativeness of the survey has been documented [13]. However, even with this large sample, these response rates mean estimates of prevalence must be treated cautiously, while estimates of relationships can be treated with more confidence [14]. For the purposes of the present study, the linkage with PBS data for the period 2005–2011 permits patients to be tracked and their adherence to medications measured. Pharmaceutical Benefits Scheme data include numbers of scripts, costs of scripts, whether patients are general or concessional, and whether they have reached a safety net. Self-reported data from the survey provide broad information on the use of prescription and non-prescription medications over the period prior to the survey, together with relevant social and demographic information.
People may fail to purchase medications for a variety of reasons, including co-payments, lack of income and the impact of other health costs on available funds, and we first address the relationship between co-payments and statin adherence descriptively. Interpretation of the simple descriptive analysis is complex, in particular as factors that impact on adherence also impact on the likelihood of transition onto the safety nets. The purpose of this study is to identify the groups most likely to fail to adhere to their medications and to consider whether this is consistent with cost being a major factor, which requires the study of association rather than causality. The descriptive analysis and the modelling described explores this association. Approaches to improving adherence of this group require understanding of behaviour, and to explore the impact of price on adherence we track the adherence status of individuals who move onto the safety net.
To refine the initial analyses, we model annual adherence as a function of cost-related and social/demographic factors. As there are potentially many interactions between categories and other factors, modelling was undertaken separately for each patient category. Other health costs include MBS co-payments and the number of GP consultations, which both have highly skewed distributions that have been transformed to quintiles. Survey data are used to measure income and to identify whether survey respondents use complementary medicines or mainstream over-the-counter medications, and how many different prescribed medications they report using. These measures were drawn from the survey question “Have you taken any medications, vitamins or supplements for most of the last 4 weeks”. We classified medications listed in the survey as prescription only, complementary (vitamins, glucosamine) and over-the-counter mainstream medications (aspirin, paracetamol, pantoprazole and salbutamol).
Total PBS co-payments are in part determined by the quantum of statins, thus while these totals may impact on adherence, they have been excluded from the modelling to avoid issues of endogeneity. To address whether failing to purchase statins is related to costs of other prescription medications at a point of time, we use monthly data with descriptive analysis.
There is considerable evidence that patients on the safety nets are inclined to purchase more medications towards the end of the calendar year to save money in the early months of the following year (hoarding) [15]. However, hoarding would be compensated by “under-purchasing” at the start of the following year, meaning the impact on annual adherence would be small, and hoarding is not addressed in our analysis.
2.2 Annual Data
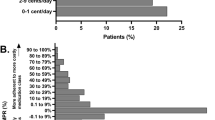
Statins are mostly sold in packs of 30 to be taken at one per day. The ratio of time expected to be covered by the quantity purchased to the number of days actually covered is referred to as a medication possession ratio (MPR). In the context of statins, the MPR is the quantity purchased divided by the number of days covered, assumed to be the time between purchases, with “adherence” defined by the commonly used threshold of an MPR greater than 80% [9].
Of the 267,068 people included in the 45 and Up Study, 106,808 claimed PBS benefits for statins. We removed observations that could not be analysed (e.g. all scripts on one day, values missing), and where adherence measures were not meaningful (e.g. fewer than 3 or more than 24 scripts in a year). Further, person-years were deleted if the average co-payment per individual pill was more than AUS$1.30 for general patients as the maximum co-payment was AUS$1.14 per pill in 2011, if the average quantity of pills purchased per day was more than three, or if there was a gap of 6 months or more between purchases in the year. The final sample was 442,344 person-years drawn from 94,114 individual respondents. Modelling is based on smaller samples, again as some independent variables have missing values. To minimise this problem we have used the “half scale rule” [16] to derive the Kessler mental health measure of psychological distress [17], and for categorical variables with large numbers of missing values we included a “missing” category.
We allocate person-years to the categories of concessional/general, depending on which forms the majority of total scripts in this person-year. We then define the person-year as “safety net” if more than 20% of scripts are under safety net arrangements, assuming 20% is large enough to impact on behaviour. Analyses using 10 and 30% differ in only minor ways from those in Tables 2, 3 and 4.
When tracking people from non-safety net to safety net status within each person-year, measurement of adherence is complicated by uncertainty regarding start and endpoints, which leads to some observations being deleted because of implausible MPR values. This, together with person-year classification of GSN and CSN categories including at least 20% of the year on the safety nets, led to somewhat different patterns to the main analysis and a total of 406,266 person-years in the transition analysis (Table 3).
2.3 Annual Analysis
The initial analysis examines annual adherence by category descriptively. This is done in two parts, first, by simple tabulation of average adherence rates by category for each person-year, and second, by following individual respondents’ transitions from non-safety to safety net status through a year to observe changes in adherence. The latter gives a more direct understanding of whether adherence follows price, but also shows the degree to which respondents who are adherent under the safety net were also adherent before reaching the safety net.
This is followed by logistic regression of adherence/non-adherence within each category using person-year units with a cluster adjustment for the multiple observations for individuals over years. The logistic regression was undertaken using demographic and health control variables comparable to previous studies [9]. Variables used to address cost included total MBS co-payments, number of GP visits, and numbers of different prescriptions, over-the-counter medications and “complementary” medications.
2.4 Monthly Data
One potential reason to not purchase statins could be if other medication costs were faced at the same time. Monthly data were used to explore whether purchases of other PBS medications in a month were related to purchases of statins. We report on all person-months for respondents who use statins, including months with and without statin use. From the 106,808 people included in the survey using statins, after removing those who had a gap in statin purchasing of 18 months or more, and those who purchased statins for 6 months or less, the final sample was 4,783,091 person-months of which 4,100,018 included statin use. For the person-months where there is a change of categories (mainly to safety net), the month is allocated to the category with the highest number of scripts.
2.5 Monthly Analysis
We examine prescription and co-payment patterns for statins and non-statins for each category. For the GNSN group, the majority of non-statin scripts are below the co-payment (around 63% of scripts in the concessional categories are priced below the GSN co-payment), thus this category is omitted.
The Sax Institute’s 45 and Up Study was approved by the University of New South Wales Human Research Ethics Committee. The project was approved by the New South Wales Population and Health Services Research Ethics Committee (Reference No.: 2013/11/487). Analysis was undertaken in Stata 12.1 (StataCorp LP, College Station, TX, USA).
3 Results
3.1 Annual Analysis
Table 2 shows the average rate of statin adherence for each category. The highest levels of adherence are in the CSN group, which has a zero co-payment for those purchases in the safety net period. The poorest adherence is in the GNSN group, which faces a co-payment of around AUS$30 per script for all scripts. Thus, adherence levels for the two groups, which face similar co-payments for their purchases, were broadly similar.
Table 3 allows us to explore whether the adherence of individuals changes on reaching the safety net, and the degree to which the results in Table 2 are due to these individual changes. It shows that those who were not adherent prior to reaching the safety net are highly likely (over 75%) to become adherent once facing the lower prices. However, it also shows that the largest group who are adherent on reaching the safety net were also adherent prior to reaching the threshold. The other important factor, as in Table 2, is that the majority of patients do not reach the safety net.
3.1.1 Cost-Related Variables
Table 4 reports on logistic regressions of adherence for each category. The variables that reflect total costs show mixed patterns. Total MBS co-payments (including specialist and diagnostic testing services and in-hospital private medical services) are significantly positively related to adherence for all categories except the CSN. However, the number of GP visits per year show few significant values, and these are not consistent between categories. To ensure that the MBS and GP consultation variables were not interacting, models were rerun without each of them and the patterns were unchanged. Income effects vary across categories, with those on lower incomes more adherent for the CSN, less adherent for the GNSN category and relationships not significant for the other categories.
While adherence is positively related to the purchase of mainstream over-the-counter medications for all groups, it is significant only for the non-safety net groups. Purchasing complementary medicines has an inconsistent pattern, while adherence is significantly higher among those reporting higher numbers of different prescription medications used for all categories.
3.1.2 Demographic and Social Variables
Adherence broadly increases across age groups with only GSN not showing significance, while this is also the only category with significant sex effects. One of the strongest relationships in all studies is the negative role of speaking a language other than English at home. People in regional areas were significantly more adherent than those in major cities except for remote areas. Adherence is significantly higher for those holding private health insurance, while working is associated with lower levels of adherence than not working. Being a regular smoker is uniformly associated with poorer adherence, as is having a Kessler mental health score reflecting greater than ‘low’ levels of distress. After allowing for other financial and sociodemographic factors, both having a partner and having poorer self-assessed health are mostly associated with lower adherence.
3.2 Monthly Analysis
Table 5 shows the average total PBS co-payments and average statin co-payments per person-month within categories for those using and not using statins. As outlined in Sect. 2.5, the GNSN category is excluded. Table 5 suggests that statins were purchased in addition to other medications with no reduction in other medications, when statins were purchased.
4 Discussion
Estimated statin adherence levels are somewhat higher in this study than those reported elsewhere [9, 18]. Differences arise because we base the calculation on person-years for people taking statins, while other studies are based on persons and commence when statin taking commences and conclude at different times depending on their rules. Further, we exclude those person-years with big gaps and few scripts as we cannot tell if they were caused clinically, while others tend to allow gaps and few scripts, and some allow long periods beyond the final purchase, assuming that ceasing to purchase reflects poor adherence.
Our primary question was why relatively high proportions of Australians reported they could not afford pharmaceuticals when supported by the PBS. To address this question, we have not only included economic variables but classified our sample depending on whether people have reached the PBS safety net. This enables us to track behaviour before and after reaching the safety net, to clarify the association of price with adherence to statins, and also to show which of the social and health correlates of adherence are significant within the safety net/non-safety net categories.
While the reported proportion of patients who could not afford prescribed pharmaceuticals in Australia is large relative to other countries, it is not large in absolute terms (9–23% in different studies) [1,2,3]. The strongest cost-related association is that patients with lower government-set co-payments are most likely to adhere to prescribed patterns of use of statins and those paying AUS$30 or more per prescription least likely. This observation can be interpreted economically as a downward sloping demand curve with higher prices creating barriers to purchasing medications, and our transition analysis supports this view, although it also shows the majority of those adherent on the safety net were also previously adherent, emphasising the need for careful targeting of any policy intervention.
The role of income further reinforces the interpretation of price impacting on demand for some people, as does the transition from non-adherence to adherence by those reaching the safety net. For those facing zero marginal cost (CSN), those with lower income and poorer average health have higher levels of adherence, while those facing the highest marginal cost (GNSN) have poorer adherence with lower income, despite health being worse in the lower income groups. Hence, the group with the poorest adherence is the low-income sector of the GNSN category.
The association of adherence with our measures of health costs is less clear. The number of different prescription medications reported in the survey was positively related to adherence, which could be owing to the “healthy adherer bias” [19], which suggests there are people who look after their health across the range of risk factors with exercise and medication [7]. Similarly, the higher adherence associated with more MBS co-payments could be seen to align with the healthy adherer bias. The monthly data show that purchasing of non-statin scripts is broadly the same whether or not statins are purchased, which also suggests that on average a healthy adherer bias may apply.
The non-cost variables showing strong effects in both this study and previous studies [9, 10] include patient age, language spoken at home, smoking and mental stress. While these modelling results reflect associations within categories and not causality, they may facilitate targeting of measures to improve adherence within the PBS. The results for self-assessed health and having a partner are inconsistent with previous studies [9]. These differences arise from the inclusion of more economic variables in the modelling and the more refined categories based on safety nets (established in detailed analysis not included in this report). If the self-assessed health result, which suggests the less healthy are also generally less adherent (cause and effect are not at all clear in this association) applies across other medications, it leads to a question of whether a more graduated system of co-payments may improve adherence to medications and hence community health.
These associations point to population groups to which GPs should pay particular attention in supporting patients to adhere to medications. In the case of languages, this may suggest a broader need for information in different languages. The negative association of smoking may reflect the negative side of the “healthy adherer bias” [19], which may be compounded by the costs of smoking.
The conclusion, therefore, is that statin adherence is responsive to out-of-pocket costs, particularly for the GNSN group facing the highest cost. While the categories facing AUS$5–$6 co-payments have lower adherence than the CSN group, there are no significant income effects nor clear patterns.
The safety net analysis shows the association of price and adherence, and gives a clearer view of the role of control variables. The study shows inconsistency in the potential impact of other health costs on statin purchases, but suggests that there may be a ‘healthy adherer bias’ within parts of the Australian community, and flags other groups likely to be poorly adherent.
Given the main group of people failing to adhere to their medications is the low-income GNSN patients, the issue becomes how to best support this group. Australia has a one of the most highly targeted welfare system and tax systems in the world [20], and its health system is similarly targeted. While the current structures ensure support is targeted to the neediest, people near the thresholds may be no less needy than those just reaching the thresholds. The barriers to purchasing statins for low-income GNSN patients could be addressed by reducing the effect of the general safety net threshold, by reducing the threshold, changing the definition of concessional patients or by considering a more stepped set of categories with different co-payments and thresholds.
4.1 Limitations
While at the time covered by this study statins were relatively expensive, since the ending of patents for the major statins this is no longer true. With lower prices, it is not clear whether the policy measures suggested would impact on statin adherence. However, similar patterns may apply to other medications in long-term use for chronic conditions that do not have immediate impact on symptoms. This is to be tested in a subsequent paper.
The main constraint on the analysis of purchasing of PBS medications is that prescriptions priced below the co-payment are not recorded. While this has minimal impact on statin purchases in 2011 and earlier or on concessional patients, it does impact materially on the costs of non-statin pharmaceuticals for general patients. Patient categories are precisely defined for each script dispensed, but for monthly or annual analysis, patients who move between categories must be allocated according to somewhat arbitrary rules. Sensitivity analyses suggest the results of this allocation are stable to variations in the rules. While PBS data can be tracked through time, material collected in the survey such as use of complementary medications relates to a point of time only, and is used to provide a perspective of patient characteristics.
5 Conclusions
We have used statins as an initial focus to help understand why survey responses show many Australian patients fail to purchase medications because of costs, and then to identify for which groups costs may be a problem. Previous Australian studies have not addressed cost per se, and we provide clear support for the view that some patients fail to fill prescriptions because of costs, as the least adherent group are low-income patients facing the highest costs, and over 75% of non-adherent patients become adherent on reaching the safety net. The result may, in part, reflect the binary nature of the concession card eligibility, and the nature of a system with a single safety net threshold for each of concessional and general patients. There are many Australians who are ineligible for a concession card who have very modest incomes. For this group, the general safety net threshold may be a barrier to adherence. While this study relates to a single medication, it is part of wider project exploring the impact of costs on adherence to a range of medications. If the wider study confirms these conclusions, policy solutions could focus on introducing additional financial protections for non-concessional patients on modest incomes by considering reducing the relevant co-payment or safety net threshold (potentially with a stepped structure), or more generous concession card eligibility criteria.
References
Menzies Centre for Health Policy. 2008 Menzies Nous Australian Health Survey, Report 2 Financial Stress and Health. 2008.
Schoen C, Osborn R, Squires D, Doty MM, Pierson R, Applebaum S. How health insurance design affects access to care and costs, by income, in eleven countries. Health Aff (Millwood). 2010;29(12):2323–34. doi:10.1377/hlthaff.2010.0862.
Australian Bureau of Statistics. Health experience survey 2015–2916. Canberra (ACT): Australian Bureau of Statistics; 2016.
Eaddy MT, Cook CL, O’Day K, Burch SP, Cantrell CR. How patient cost-sharing trends affect adherence and outcomes: a literature review. P T. 2012;37(1):45–55.
Hynd A, Roughead EE, Preen DB, Glover J, Bulsara M, Semmens J. The impact of co-payment increases on dispensings of government-subsidised medicines in Australia. Pharmacoepidemiol Drug Saf. 2008;17(11):1091–9. doi:10.1002/pds.1670.
Schafheutle EI, Hassell K, Noyce PR, Weiss MC. Access to medicines: cost as an influence on the views and behaviour of patients. Health Soc Care Community. 2002;10(3):187–95.
Briesacher BA, Gurwitz JH, Soumerai SB. Patients at-risk for cost-related medication nonadherence: a review of the literature. J Gen Intern Med. 2007;22(6):864–71. doi:10.1007/s11606-007-0180-x.
Laba TL, Brien JA, Jan S. Understanding rational non-adherence to medications: a discrete choice experiment in a community sample in Australia. BMC Fam Pract. 2012;13:61. doi:10.1186/1471-2296-13-61.
Warren JR, Falster MO, Fox D, Jorm L. Factors influencing adherence in long-term use of statins. Pharmacoepidemiol Drug Saf. 2013;22(12):1298–307. doi:10.1002/pds.3526.
Warren JR, Falster MO, Tran B, Jorm L. Association of continuity of primary care and statin adherence. PLoS One. 2015;10(10):e0140008. doi:10.1371/journal.pone.0140008.
Department of Social Services. Demographic, December 2015.
Banks E, Redman S, Jorm L, Armstrong B, Bauman A, Beard J, et al. Cohort profile: the 45 and up study. Int J Epidemiol. 2008;37(5):941–7. doi:10.1093/ije/dym184.
Johar M, Savage E. Healthcare expenditure profile of older Australians: evidence from linked survey and health administrative data. Econ Pap. 2012;31(4):451–63.
Mealing NM, Banks E, Jorm LR, Steel DG, Clements MS, Rogers KD. Investigation of relative risk estimates from studies of the same population with contrasting response rates and designs. BMC Med Res Methodol. 2010;10:26. doi:10.1186/1471-2288-10-26.
LuizaVL, Chaves LA, SilvaRM, Emmerick ICM, ChavesGC, Fonseca deAraújo SC et al. Pharmaceutical policies: effects of cap and co-payment on rational use of medicines. 2015 Contract No.: Art. No.: CD007017.
Dawda P, McRae IS, Yen L, Islam MM, Bagheri N, Jowsey T, et al. Does it matter who organises your health care? Int J Integr Care. 2015;15:e022.
Andrews G, Slade T. Interpreting scores on the Kessler Psychological Distress Scale (K10). Aust N Z J Public Health. 2001;25(6):494–7.
Chowdhury R, Khan H, Heydon E, Shroufi A, Fahimi S, Moore C, et al. Adherence to cardiovascular therapy: a meta-analysis of prevalence and clinical consequences. Eur Heart J. 2013;34(38):2940–8. doi:10.1093/eurheartj/eht295.
Shrank WH, Patrick AR, Alan Brookhart M. Healthy user and related biases in observational studies of preventive interventions: a primer for physicians. J Gen Intern Med. 2011;26(5):546–50. doi:10.1007/s11606-010-1609-1.
Whiteford P. Tales of Robin Hood (part 1): welfare myths and realities in the United Kingdom and Australia Australian Review of Public Affairs. Digest, September 2015.
Acknowledgements
This research was completed using data collected through the 45 and Up Study (http://www.saxinstitute.org.au). The 45 and Up Study is managed by the Sax Institute in collaboration with its major partner, Cancer Council New South Wales; and partners: the National Heart Foundation of Australia (New South Wales Division); New South Wales Ministry of Health; New South Wales Government Family and Community Services—Carers, Ageing and Disability Inclusion; and the Australian Red Cross Blood Service. The linked Medicare Benefits Scheme and Pharmaceutical Benefits Scheme data were supplied to the 45 and Up Study by the Commonwealth Department of Human Services. We thank the many thousands of people participating in the 45 and Up Study.
Author information
Authors and Affiliations
Contributions
IM developed the initial design of the project based on an idea of LY. JH and KG assisted in finalising the design. IM undertook the analysis and the initial drafting. All authors contributed to the editing, redrafting and finalising of the paper.
Corresponding author
Ethics declarations
Funding
The research was funded by the Research in the Finance and Economics of Primary Health Care Centre of Research Excellence (ReFinE-PHC) under the Australian Primary Health Care Research Institute’s Centres of Research Excellence funding scheme, which is supported by a grant from the Australian Government Department of Health. The article does not necessarily reflect the views of the Australian Primary Health Care Research Institute or the Australian Government.
Conflict of interest
Ian McRae, Kees van Gool, Jane Hall and Laurann Yen have no conflicts of interest directly relevant to the contents of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
McRae, I., van Gool, K., Hall, J. et al. Role of Cost on Failure to Access Prescribed Pharmaceuticals: The Case of Statins. Appl Health Econ Health Policy 15, 625–634 (2017). https://doi.org/10.1007/s40258-017-0336-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-017-0336-8