Abstract
Background
Several clinical trials of dapagliflozin in patients with type 2 diabetes mellitus (T2DM) at elevated cardiovascular risk have observed reduced hospitalization for heart failure (HHF). Several studies have also suggested cardiovascular benefits for patients with HF regardless of whether or not they have T2DM.
Objective
This meta-analysis was conducted to evaluate the therapeutic effects of dapagliflozin in patients with HF.
Methods
The PubMed, Embase, Cochrane Library, and Web of Science databases were systematically searched from database inception to 15 February 2020. Clinical studies of dapagliflozin use in patients with HF were included. Data on HHF, all-cause mortality, cardiovascular death, major adverse cardiovascular events (MACE), systolic blood pressure, body weight, glycated hemoglobin (HbA1c), and adverse events were collected for analysis.
Results
Four randomized controlled trials involving 6738 patients with HF were included in this meta-analysis. Patients receiving dapagliflozin showed a significantly lower incidence of HHF [risk ratio (RR) 0.72; P < 0.00001], all-cause mortality (RR 0.83; P = 0.004), cardiovascular death (RR 0.86; P = 0.03), and MACE (RR 0.88; P = 0.03). Moreover, patients receiving dapagliflozin also showed significant improvements in systolic blood pressure and body weight. However, no statistical difference was observed in HbA1c. In addition, hypoglycemia, volume depletion, and renal impairment was not more frequent with dapagliflozin than with placebo.
Conclusion
This meta-analysis suggests that dapagliflozin could be a therapeutic strategy for patients with HF regardless of the presence or absence of T2DM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Heart failure (HF) is a common clinical syndrome that imposes substantial health and financial burdens worldwide [1, 2]. Patients with HF are characteristic for impaired left ventricular function, reduced quality of life, and increased mortality [3]. To date, multiple guideline-directed medical therapies have been proposed and applied to clinical practice, including β-blockers, renin–angiotensin–aldosterone system inhibitors, diuretics, and so forth [1]. Nevertheless, the burden of cardiovascular events in HF, particularly in HF with reduced ejection fraction (HFrEF; defined as left ventricular ejection fraction [LVEF] ≤ 40%), remains significant [4]. Therefore, a novel therapeutic strategy is required to improve symptoms, decrease mortality, and reduce hospitalization for patients with HF.
Dapagliflozin is a sodium-glucose co-transporter 2 inhibitor (SGLT2i) initially developed to treat type 2 diabetes mellitus (T2DM) by preventing glucose reabsorption in the proximal tubule and thereby lowering plasma glucose concentrations [5]. Recently, several clinical trials using dapagliflozin in patients with T2DM at elevated cardiovascular risk have demonstrated reduced rates of hospitalization for HF (HHF) [6,7,8]. In addition, several studies have suggested cardiovascular benefits with dapagliflozin in patients with HF regardless of the presence or absence of T2DM [9,10,11].
However, the overall effects of dapagliflozin in patients with HF remain poorly understood and are thus vigorously debated. Hence, a systematic review is required to summarize existing data and evaluate the protective effects of dapagliflozin against HF. We aimed to conduct a meta-analysis to comprehensively estimate the effects of dapagliflozin in patients with HF regardless of the presence or absence of T2DM.
2 Methods
2.1 Selection strategy
The literature search was conducted in the PubMed, Embase, Web of Science, and Cochrane Library electronic databases from inception to 15 February 2020. Detailed search strategies were used. For example, the following strategy was used in PubMed: (((sodium-glucose co-transporter [title/abstract]) OR SGLT2 [title/abstract]) OR dapagliflozin [title/abstract]) AND heart failure [title/abstract]. We also manually screened the reference lists of retrieved articles, previous meta-analyses, and reviewed articles to identify any related research.
2.2 Study design
Inclusion criteria were as follows: (1) randomized, double-blind, placebo-controlled clinical trials; (2) studies reporting efficacy or safety-related outcomes, including HHF, all-cause mortality, cardiovascular death, major adverse cardiovascular events (MACE; described as a composite of cardiovascular death, myocardial infarction, and ischemic stroke), and adverse events; and (3) full articles published in English in peer-reviewed journals. For multiple publications of the same trial, only the study containing the most data was included. Importantly, studies regarding the effects of dapagliflozin in patients with HF, regardless of LVEF, were considered, in order to capture the full spectrum of HF. We excluded animal studies, review articles, letters, case reports, articles lacking outcomes of interest/control group, and trials with follow-up of < 1 month). Two independent investigators (XD Zheng and XY Jiang) screened and reviewed article titles, abstracts, and full texts to assess eligibility. Any disagreements about eligibility were resolved via discussion with a third investigator (C Tang).
2.3 Data extraction and quality assessment
For each eligible study, data were extracted by two independent investigators (XD Zheng and Q Qu), with any discrepancy clarified through discussion with a third investigator (ZY Wang). Extracted characteristics included first author, publication year, follow-up period, drug dose, number of participants, patient demographic and clinical characteristics, and the following efficacy and safety outcomes: HHF, all-cause mortality, cardiovascular death, MACE, systolic blood pressure, body weight, glycated hemoglobin (HbA1c), and diverse adverse events.
We used the Cochrane Collaboration’s tool for assessing the risk of bias to assess the quality of the included studies [12] in terms of selection bias, performance bias, detection bias, attrition bias, reporting bias, and other bias. Two independent investigators (XD Zheng and ZY Wang) conducted this assessment, with any controversy settled by consensus with a third investigator (JY Sun).
2.4 Statistical Analysis
Categorical variables were presented as frequencies and risk ratios (RR) with corresponding 95% confidence intervals (CI), and continuous variables were presented as mean ± standard deviation. P values < 0.05 were considered statistically significant. The proportion of variance derived from between-study heterogeneity was quantified by I2, with a fixed-effects model applied when the I2 value was < 50% and a random-effects model adopted otherwise [13]. Baujat plot-based sensitivity analyses were performed to detect potential outliers and influence points that over-contributed to the overall heterogeneity and results [14], and influence analyses were conducted to identify whether any individual study distorted the pooled effects, as described by Viechtbauer and Cheung [15]. All analytical results were measured using Review Manager v5.3 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark), and sensitivity analyses were performed using R software v3.6.3 (R Foundation for Statistical Computing, Vienna, Austria). The analysis was carried out according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) guidelines [16].
3 Results
3.1 Study selection and quality assessment
As shown in Fig. 1, a total of 2249 articles were identified via initial database search, of which 878 duplicates and 1323 irrelevant studies were excluded after title and abstract screening. After the full texts of the remaining 48 studies were reviewed, four articles with 6738 patients were ultimately included for further analysis [11, 17,18,19] (Table 1). Of note, 4226 (62.7%) participants were diagnosed with T2DM, whereas 5210 (77.3%) participants had concomitant reduced LVEF. All included studies were high-quality randomized controlled trials, and the corresponding risks of bias are presented in Fig. 2.
3.2 Efficacy outcomes assessment
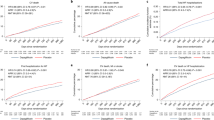
HHF, all-cause mortality, cardiovascular mortality, and MACE were documented to assess efficacy outcomes with dapagliflozin. Importantly, all the included studies reported the effect of dapagliflozin on HHF, and a fixed-effects model was applied to evaluate the difference. As shown in Fig. 3a, dapagliflozin treatment was associated with significantly reduced HHF compared with placebo (RR 0.72; 95% CI 0.63–0.82; P < 0.00001; I2 = 28%). Similarly, four studies reported all-cause mortality, with results indicating that dapagliflozin significantly decreased all-cause mortality (RR 0.83; 95% CI 0.74–0.94; P = 0.004; I2 = 0%; Fig. 3b). Cardiovascular mortality (RR 0.86; 95% CI 0.74–0.99; P = 0.03; I2 = 0%; Fig. 3c) and MACE (RR 0.88; 95% CI 0.78–0.99; P = 0.03; I2 = 12%; Fig. 3d) were also reduced in patients with HF receiving dapagliflozin compared with those receiving placebo.
Forest plot of a hospitalization for heart failure, b all-cause mortality, c cardiovascular mortality, and d major adverse cardiovascular events. Comparison of hospitalization for heart failure, all-cause mortality, cardiovascular mortality, and major adverse cardiovascular events between dapagliflozin and placebo group. CI confidence interval
3.3 Safety Outcomes Assessment
Multiple adverse events were evaluated, including hypoglycemia, volume depletion, and renal impairment, as were serious adverse events. Three studies enrolling 4751 patients reported no significant difference in hypoglycemia (RR 1.09; 95% CI 0.78–1.53; P = 0.60; I2 = 0%; Fig. 4a) or the occurrence of volume depletion (RR 1.10; 95% CI 0.91–1.34; P = 0.33; I2 = 0%; Fig. 4b) or renal impairment (RR 1.13; 95% CI 0.30–4.26; P = 0.86; I2 = 53%; Fig. 4c) between the two groups. Patients receiving dapagliflozin had a significantly lower incidence of serious adverse events than those receiving placebo (RR 0.90; 95% CI 0.84–0.96; P = 0.002; I2 = 0%; Fig. 4d).
3.4 Assessments of Other Indicators
Other indicators analyzed included systolic blood pressure, body weight, and HbA1c. Three studies involving 4751 participants reported results for systolic blood pressure, with the overall value significantly lower with dapagliflozin than with placebo [mean difference (MD) − 1.00; 95% CI − 1.86 to − 0.15; P = 0.02; I2 = 0%; Fig. 5a]. Similarly, Fig. 5b illustrates a significant negative correlation between dapagliflozin treatment and body weight compared with placebo (MD − 1.72; 95% CI − 3.36 to − 0.08; P = 0.04; I2 = 87%), but no significant difference was noted in HbA1c (MD − 0.23; 95% CI − 0.52–0.07; P = 0.13; I2 = 90%; Fig. 5c).
3.5 Sensitivity analysis
No research fell in the top-right quadrant of the Baujat plot (Fig. 6a), suggesting a significant lack of any individual study driving the observed results. Moreover, Fig. 6b shows the influence analyses comparing weight with overall heterogeneity, which reveals that the pooled estimated outcomes were robust and did not depend on a single study.
a Baujat plot using the dapagliflozin fixed-effects model. The x-axis represents the squared Pearson resident of each study, and the y-axis represents the standardized squared difference between the model-estimated effect for each study. Studies located in the upper-right corner of the Baujat plot contribute greatly to the overall heterogeneity and results. b Influences of overall heterogeneity in model studies. Study 1–4 refers to the study by Kato et al. [11], Kosiborod et al. [19], McMurray et al. [9], and Nassif et al. [10], respectively
4 Discussion
To the best of our knowledge, although previous studies have demonstrated cardiovascular protective effects with SGLT2i, this is the first meta-analysis to comprehensively evaluate the effects of dapagliflozin in patients with HF regardless of the presence or absence of T2DM. We systematically assessed 6738 patients with HF randomized to dapagliflozin or placebo from four randomized controlled trials. On one hand, the results indicated that dapagliflozin significantly reduced HHF, cardiovascular death, all-cause mortality, MACE, systolic blood pressure, and body weight. On the other hand, no significant differences were found in hypoglycemia, volume depletion, renal impairment, or serious adverse events. Generally, these findings reveal the efficacy and safety of dapagliflozin in patients with HF, regardless of the presence or absence of T2DM.
HF is a common syndrome that seriously threatens human health worldwide. Despite appreciable advances in therapeutic strategies, the cardiovascular outcomes, survival, and prognosis for patients with HF remain relatively poor, resulting in a persistently high risk of symptomatic progression and clinical deterioration. Therefore, a novel strategy against HF is required to complement current therapies as previously detailed. Additional cardiovascular protective effects beyond lowering plasma glucose have recently been reported for dapagliflozin [6,7,8], which has made it a research hotspot in HF treatment. This meta-analysis indicates that dapagliflozin can effectively reduce HHF, cardiovascular death, all-cause mortality, and MACE in patients with HF, findings that are consistent with those of previous studies [20,21,22,23]. Importantly, considering that more than three-quarters of the participants had reduced LVEF, these results may primarily reflect the effects of dapagliflozin in patients with HFrEF, which deserves paramount attention in clinical applications.
In terms of safety, this analysis showed no increased risk of hypoglycemia, volume depletion, renal impairment, or serious adverse events in patients receiving dapagliflozin. Dapagliflozin could inhibit renal glucose reabsorption, thus decreasing plasma glucose concentrations. Unlike other hypoglycemic agents, dapagliflozin can subsequently increase plasma glucagon concentrations and improve the production of endogenous glucose [24]. Therefore, although dapagliflozin could lower plasma glucose, it does not contribute to hypoglycemia in patients with HF without T2DM. Volume depletion is another major concern in patients receiving high doses of loop diuretics. Consistent with recent studies, this analysis showed no significant difference between dapagliflozin and placebo in volume depletion events [25, 26]. Interestingly, the vast majority of SGLT2i have been demonstrated as associated with a higher risk of volume depletion than placebo or other oral hypoglycemic agents [27, 28]. Furthermore, no significant reduction in cardiac biomarkers (natriuretic peptides) was reported in included studies, which further validates our results and contradicts the volume depletion hypothesis. Thus, we postulate that volume preservation can be partly explained by diuretic dose adjustments during trials; such a speculation was supported by the results of a recent clinical trial [29]. Regardless, these results suggest dapagliflozin has a reassuring safety profile.
Although several possible mechanisms for the cardiovascular protective benefits of SGLT2i have been proposed, the underlying biological mechanisms remain unclear. The protective effect was observed early after SGLT2i treatment, indicating that the possible mechanisms might be distinguished from other glucose-lowering therapies [9, 30]. In several clinical trials in patients with T2DM [31, 32], dapagliflozin lowered plasma volume and depressed systolic blood pressure without increasing heart rate, suggesting its potential as a promising therapeutic alternative in HF, particularly in HFrEF (e.g., β-blockers and bradycardia; renin–angiotensin–aldosterone system inhibitors and renal dysfunction/hyperkalemia). However, reduced systolic blood pressure could generate insufficient blood supply to the brain, heart, kidneys, and other organs and has been prominently correlated with an elevated risk of sudden cardiac death. Several clinical trials have corroborated the neutral or even detrimental role of antihypertensive drugs in established HF [33,34,35]. Hence, the clinical application of dapagliflozin might require combination with antihypotensive therapies. Of note, glycosuria could stimulate lipid oxidation to compensate for the loss of energy and further lead to weight loss and fat mass reduction [36, 37]. These changes may subsequently lighten both the preload and the afterload to the heart and eventually result in cardiovascular protective effects. Alongside a systemic hemodynamic and metabolic effect, direct cardiovascular effects have also been proposed as important drivers, including improved cardiac inflammation [38], oxidative stress [39], apoptosis [38], mitochondrial dysfunction [40], ionic dyshomeostasis [41], and so forth [42, 43].
Other studies have mainly evaluated the cardiovascular protection benefits of dapagliflozin in patients with T2DM with elevated cardiovascular risks, most of whom did not have established HF. Therefore, the cardiovascular benefits of dapagliflozin primarily corresponded to the prevention of HF. Clinical trials to evaluate protective effects in patients with HF, most of whom have reduced ejection fraction and T2DM, have only recently been conducted. The results from the DAPA-HF trial, which showed an association between dapagliflozin and improved HF-related prognosis regardless of baseline HbA1c, have led to dapagliflozin being recognized as a potential therapeutic strategy for HFrEF regardless of T2DM. In addition, several large ongoing trials are evaluating the clinical effects of SGLT2i in patients with HF with or without T2DM (NCT02653482, NCT03030235, NCT03057951, NCT03057977, and NCT03619213). These clinical trials may further demonstrate the effects of dapagliflozin in patients with HF, especially those with preserved ejection fraction.
Although this analysis adhered strictly to PRISMA guidelines, several limitations should be highlighted. First, the included studies did not provide enough relevant information to allow us to precisely define volume depletion, renal impairment, and serious adverse events. Second, the use of secondary outcomes (cardiovascular death, myocardial infarction, ischemic stroke) derived from DECLARE TIMI 58, a neutral trial on the original primary endpoint (MACE), may reduce the strength of this meta-analysis. There may also exist some selection bias induced by the inclusion criteria (e.g., exclusion of patients with symptomatic hypotension or systolic blood pressure < 95 mmHg at two of three measurements in visit 1 or 2 of the DAPA-HF trial) during the run-in phases of the included trials, which may cause unexpected signs of some estimators. Importantly, since 77.3% of participants involved in this meta-analysis had HFrEF, our findings might be mainly applicable to current HFrEF treatment. Moreover, since the included patients were characterized by a specific baseline (e.g., 62.7% of patients diagnosed with T2DM, 63.3% of patients with New York Heart Association class II disease, 73.1% males, and so forth), the generalizability of these findings to real-world HFrEF populations is debatable.
5 Conclusion
This meta-analysis predominantly strengthens the efficacy and safety of dapagliflozin in patients with HFrEF regardless of the presence or absence of T2DM, with some caveats. Importantly, whether benefits are observed regardless of LVEF remains to be established, and more randomized controlled trials are required to verify the effects of dapagliflozin in patients with HF.
References
Writing Committee M, Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128(16):e240–327.
Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation. 2019;139(10):e56–e528.
Bui AL, Horwich TB, Fonarow GC. Epidemiology and risk profile of heart failure. Nat Rev Cardiol. 2011;8(1):30–41.
Hillege HL, Nitsch D, Pfeffer MA, Swedberg K, McMurray JJ, Yusuf S, et al. Renal function as a predictor of outcome in a broad spectrum of patients with heart failure. Circulation. 2006;113(5):671–8.
DeFronzo RA, Norton L, Abdul-Ghani M. Renal, metabolic and cardiovascular considerations of SGLT2 inhibition. Nat Rev Nephrol. 2017;13(1):11–26.
Wanner C, Lachin JM, Inzucchi SE, Fitchett D, Mattheus M, George J, et al. Empagliflozin and clinical outcomes in patients with type 2 diabetes mellitus, established cardiovascular disease, and chronic kidney disease. Circulation. 2018;137(2):119–29.
Fitchett D, Butler J, van de Borne P, Zinman B, Lachin JM, Wanner C, et al. Effects of empagliflozin on risk for cardiovascular death and heart failure hospitalization across the spectrum of heart failure risk in the EMPA-REG OUTCOME(R) trial. Eur Heart J. 2018;39(5):363–70.
Fitchett D, Zinman B, Wanner C, Lachin JM, Hantel S, Salsali A, et al. Heart failure outcomes with empagliflozin in patients with type 2 diabetes at high cardiovascular risk: results of the EMPA-REG OUTCOME(R) trial. Eur Heart J. 2016;37(19):1526–34.
Docherty KF, Jhund PS, Anand I, Bengtsson O, Böhm M, de Boer RA, et al. Effect of dapagliflozin on outpatient worsening of patients with heart failure and reduced ejection fraction: a prespecified analysis of DAPA-HF. Circulation. 2020. https://doi.org/10.1161/CIRCULATIONAHA.120.047480.
Nassif ME, Windsor S, Tang F, Khariton Y, Husain M, Inzucchi SE, et al. Dapagliflozin effects on biomarkers, symptoms, and functional status in patients with heart failure with reduced ejection fraction: the DEFINE-HF Trial. Circulation. 2019;140(18):1463–76.
Kato ET, Silverman MG, Mosenzon O, Zelniker TA, Cahn A, Furtado RHM, et al. Effect of dapagliflozin on heart failure and mortality in type 2 diabetes mellitus. Circulation. 2019;139(22):2528–36.
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ (Clinical research ed). 2011;343:d5928.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
Baujat B, Mahé C, Pignon JP, Hill C. A graphical method for exploring heterogeneity in meta-analyses: application to a meta-analysis of 65 trials. Stat Med. 2002;21(18):2641–52.
Viechtbauer W, Cheung MW. Outlier and influence diagnostics for meta-analysis. Res Synth Methods. 2010;1(2):112–25.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ (Clinical research ed). 2009;339:b2535.
Anker SD, Butler J, Filippatos GS, Jamal W, Salsali A, Schnee J, et al. Evaluation of the effects of sodium-glucose co-transporter 2 inhibition with empagliflozin on morbidity and mortality in patients with chronic heart failure and a preserved ejection fraction: rationale for and design of the EMPEROR-Preserved Trial. Eur J Heart Fail. 2019;21(10):1279–87.
Jhund PS, Bengtsson O, Sjostrand M, Langkilde AM, Nassif ME, Windsor S, et al. Dapagliflozin effects on biomarkers, symptoms, and functional status in patients with heart failure with reduced ejection fraction: the DEFINE-HF Trial. N Engl J Med. 2019; 140(18):1463–76.
Kosiborod M, Gause-Nilsson I, Xu J, Sonesson C, Johnsson E. Efficacy and safety of dapagliflozin in patients with type 2 diabetes and concomitant heart failure. J Diabetes Complic. 2017;31(7):1215–21.
Usman MS, Siddiqi TJ, Memon MM, Khan MS, Rawasia WF, Talha Ayub M, et al. Sodium-glucose co-transporter 2 inhibitors and cardiovascular outcomes: a systematic review and meta-analysis. Eur J Prev Cardiol. 2018;25(5):495–502.
Verma S, McMurray JJV. SGLT2 inhibitors and mechanisms of cardiovascular benefit: a state-of-the-art review. Diabetologia. 2018;61(10):2108–17.
Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380(4):347–57.
Birkeland KI, Jorgensen ME, Carstensen B, Persson F, Gulseth HL, Thuresson M, et al. Cardiovascular mortality and morbidity in patients with type 2 diabetes following initiation of sodium-glucose co-transporter-2 inhibitors versus other glucose-lowering drugs (CVD-REAL Nordic): a multinational observational analysis. Lancet Diabetes Endocrinol. 2017;5(9):709–17.
Bonner C, Kerr-Conte J, Gmyr V, Queniat G, Moerman E, Thevenet J, et al. Inhibition of the glucose transporter SGLT2 with dapagliflozin in pancreatic alpha cells triggers glucagon secretion. Nat Med. 2015;21(5):512–7.
Weber MA, Mansfield TA, Cain VA, Iqbal N, Parikh S, Ptaszynska A. Blood pressure and glycaemic effects of dapagliflozin versus placebo in patients with type 2 diabetes on combination antihypertensive therapy: a randomised, double-blind, placebo-controlled, phase 3 study. Lancet Diabetes Endocrinol. 2016;4(3):211–20.
Araki E, Onishi Y, Asano M, Kim H, Yajima T. Efficacy and safety of dapagliflozin over 1 year as add-on to insulin therapy in Japanese patients with type 2 diabetes: the DAISY (Dapagliflozin Added to patients under InSulin therapY) trial. Diabetes Obes Metab. 2017;19(4):562–70.
Menne J, Dumann E, Haller H, Schmidt BMW. Acute kidney injury and adverse renal events in patients receiving SGLT2-inhibitors: a systematic review and meta-analysis. PLoS Med. 2019;16(12):e1002983.
Singh AK, Unnikrishnan AG, Zargar AH, Kumar A, Das AK, Saboo B, et al. Evidence-based consensus on positioning of SGLT2i in type 2 diabetes mellitus in Indians. Diabetes Ther Res Treat Educ Diabetes Relat Disord. 2019;10(2):393–428.
Jabbour S, Seufert J, Scheen A, Bailey CJ, Karup C, Langkilde AM. Dapagliflozin in patients with type 2 diabetes mellitus: a pooled analysis of safety data from phase IIb/III clinical trials. Diabetes Obes Metab. 2018;20(3):620–8.
Packer M, Anker SD, Butler J, Filippatos G, Zannad F. Effects of sodium-glucose cotransporter 2 inhibitors for the treatment of patients with heart failure: proposal of a novel mechanism of action. JAMA Cardiol. 2017;2(9):1025–9.
Mazidi M, Rezaie P, Gao HK, Kengne AP. Effect of sodium-glucose cotransport-2 inhibitors on blood pressure in people with type 2 diabetes mellitus: a systematic review and meta-analysis of 43 randomized control trials with 22 528 patients. J Am Heart Assoc. 2017;6(6):e004007.
Thomas MC, Cherney DZI. The actions of SGLT2 inhibitors on metabolism, renal function and blood pressure. Diabetologia. 2018;61(10):2098–107.
Cohn JN, Pfeffer MA, Rouleau J, Sharpe N, Swedberg K, Straub M, et al. Adverse mortality effect of central sympathetic inhibition with sustained-release moxonidine in patients with heart failure (MOXCON). Eur J Heart Fail. 2003;5(5):659–67.
Packer M, Carson P, Elkayam U, Konstam MA, Moe G, O'Connor C, et al. Effect of amlodipine on the survival of patients with severe chronic heart failure due to a nonischemic cardiomyopathy: results of the PRAISE-2 study (prospective randomized amlodipine survival evaluation 2). JACC Heart Fail. 2013;1(4):308–14.
Mehra MR, Vaduganathan M, Fu M, Ferreira JP, Anker SD, Cleland JGF, et al. A comprehensive analysis of the effects of rivaroxaban on stroke or transient ischaemic attack in patients with heart failure, coronary artery disease, and sinus rhythm: the COMMANDER HF trial. Eur Heart J. 2019;40(44):3593–602.
Lahnwong S, Chattipakorn SC, Chattipakorn N. Potential mechanisms responsible for cardioprotective effects of sodium-glucose co-transporter 2 inhibitors. Cardiovasc Diabetol. 2018;17(1):101.
Neeland IJ, McGuire DK, Chilton R, Crowe S, Lund SS, Woerle HJ, et al. Empagliflozin reduces body weight and indices of adipose distribution in patients with type 2 diabetes mellitus. Diab Vasc Dis Res. 2016;13(2):119–26.
Ye Y, Bajaj M, Yang HC, Perez-Polo JR, Birnbaum Y. SGLT-2 inhibition with dapagliflozin reduces the activation of the Nlrp3/ASC inflammasome and attenuates the development of diabetic cardiomyopathy in mice with type 2 diabetes. Further augmentation of the effects with saxagliptin, a DPP4 inhibitor. Cardiovasc Drugs Ther. 2017;31(2):119–32.
Lee TM, Chang NC, Lin SZ. Dapagliflozin, a selective SGLT2 Inhibitor, attenuated cardiac fibrosis by regulating the macrophage polarization via STAT3 signaling in infarcted rat hearts. Free Radic Biol Med. 2017;104:298–310.
Tanajak P, Sa-Nguanmoo P, Sivasinprasasn S, Thummasorn S, Siri-Angkul N, Chattipakorn SC, et al. Cardioprotection of dapagliflozin and vildagliptin in rats with cardiac ischemia-reperfusion injury. J Endocrinol. 2018;236(2):69–84.
Joubert M, Jagu B, Montaigne D, Marechal X, Tesse A, Ayer A, et al. The sodium-glucose cotransporter 2 inhibitor dapagliflozin prevents cardiomyopathy in a diabetic lipodystrophic mouse model. Diabetes. 2017;66(4):1030–40.
Baartscheer A, Schumacher CA, Wust RC, Fiolet JW, Stienen GJ, Coronel R, et al. Empagliflozin decreases myocardial cytoplasmic Na(+) through inhibition of the cardiac Na(+)/H(+) exchanger in rats and rabbits. Diabetologia. 2017;60(3):568–73.
Bertero E, Prates Roma L, Ameri P, Maack C. Cardiac effects of SGLT2 inhibitors: the sodium hypothesis. Cardiovasc Res. 2018;114(1):12–8.
Acknowledgements
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
Xiao-Dong Zheng, Qiang Qu, Xing-Yu Jiang, Zhong-Yuan Wang, Cheng Tang, and Jin-Yu Sun have no potential conflicts of interest that might be relevant to the contents of this manuscript.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Availability of Data and Material
Not applicable.
Rights and permissions
About this article
Cite this article
Zheng, XD., Qu, Q., Jiang, XY. et al. Effects of Dapagliflozin on Cardiovascular Events, Death, and Safety Outcomes in Patients with Heart Failure: A Meta-Analysis. Am J Cardiovasc Drugs 21, 321–330 (2021). https://doi.org/10.1007/s40256-020-00441-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-020-00441-x