Abstract
Venous thromboembolism is the third most common cardiovascular disease and a major cause of inpatient mortality as over 50 % of deep vein thrombosis and pulmonary embolism are undetected in medically treated patients. Several agents are approved for thromboprophylaxis, including warfarin, unfractionated heparin, low molecular-weight heparins, fondaparinux, and target-specific oral anticoagulants. The purpose of this literature review is to discuss the increased risk of venous thromboembolism in medically ill patients and the literature surrounding the efficacy and tolerability of low molecular-weight heparins and target-specific oral anticoagulants for this indication. PubMed, MEDLINE, EBSCOhost, and clinicaltrials.gov were used as search engines in the literature review. Search limits included articles containing human subjects, scholarly (peer-reviewed) journals written in English, and publication dates from 2004 to 2014. Animal studies, non-English articles, and publications dated prior to 2004 were excluded. Recurrent venous thromboembolism remains an ongoing problem affecting thousands of people in the non-surgical population annually. With limited data, it is not likely that target-specific oral anticoagulants will soon replace low molecular-weight heparins or even be considered an alternative until efficacy and tolerability have been established. Until further evidence is disclosed, low molecular-weight heparins and fondaparinux (in the absence of renal dysfunction and low body weight) should continue to be utilized as first-line agents for thromboprophylaxis in medically ill patients. The use of apixaban and rivaroxaban is discouraged for thromboprophylaxis in medically ill patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A major gap remains in clinical trials and in the overall body of evidence discussing thromboprophylaxis in medically ill patients. |
Low molecular-weight heparins continue to be first-line therapy for thromboprophylaxis in medically ill patients. |
Rivaroxaban is the only target-specific oral anticoagulant to show favorable efficacy in medically ill patients for thromboprophylaxis, but at an increased risk of bleeding. |
1 Introduction
Approximately 350,000–600,000 individuals in the USA alone experience venous thromboembolism (VTE), comprising deep vein thrombosis (DVT) and pulmonary embolism (PE). VTE is the third most common cardiovascular disease and a major cause of inpatient mortality, as over 50 % of DVT and PE are undetected in medically treated patients [1, 2]. Annually, at least 100,000 deaths are related to these disease states [3]. National Hospital Discharge Surveys have shown that over 230,000 individuals are hospitalized for VTE each year in the USA [4].
Venous thromboembolism is the formation of a thrombus in a vein. A thrombus is the final step of the coagulation cascade (Fig. 1), where a mix of aggregated platelets and cross-linked fibrin proteins form a blood clot. Once the thrombus relocates, it is called an embolus. The most common sites an embolus typically settles are the deep veins of the legs and the lungs [5]. In hospitalized medically ill patients, acute medical illnesses, cancer, immobility, obesity, and inherited or acquired thrombophilia are some of the many risk factors for VTE (Table 1). The more risk factors present, the higher the risk of VTE. Numerous complications may arise from a DVT or PE, and the risk of these events increase with every subsequent VTE. In medically ill patients, these complications include, but are not limited to, recurrent VTE, post-thrombotic syndrome (PTS), and chronic thromboembolic pulmonary hypertension (CTEPH) [6].
Several agents are approved for the treatment and prevention of VTE, including warfarin, unfractionated heparin (UFH), low molecular-weight heparins (LMWHs), fondaparinux, and target-specific oral anticoagulants (TSOACs) (Table 2). Although the mechanisms of action of these medications differ, they all have the same endpoint of inhibiting the formulation of fibrin (or blood clot). Warfarin has been part of the mainstay of VTE treatment and thromboprophylaxis for decades. Warfarin inhibits the synthesis of vitamin K-dependent clotting factors II (also known as thrombin), VII, IX, and X, thereby blocking several sites in the coagulation cascade [7]. Before warfarin, UFH was the sole anticoagulant used to treat and prevent VTE, and is still one of the most commonly used agents within the inpatient setting. UFH inactivates the activated forms of factors II and X via antithrombin III. It also inhibits the activation of factor XIII, the fibrin stabilizing factor [8]. LMWHs work similarly to UFH by enhancing the inhibition of activated factors X and II via antithrombin III [9, 10]. The most commonly used LMWHs are enoxaparin and dalteparin. These agents have a lower affinity for antithrombin due to a smaller polysaccharide chain structure compared with UFH, with the advantage of more predictable anticoagulation effects (Table 3). Fondaparinux, a synthetic analog of the pentasaccharide chain in heparin and LMWHs, is another anticoagulant that selectively binds to antithrombin III and inhibits activated factor X, but does not affect activated factor II [11]. Finally, our most recently approved anticoagulant agents are the TSOACs, consisting of rivaroxaban and apixaban. These agents directly inhibit activated factor X (Fig. 1) [12, 13].
For the past decade, LMWHs have been replacing UFH as initial VTE therapy and prevention for medically ill patients because of a more predictable pharmacokinetic profile and the allowance of out-of-hospital management for uncomplicated VTE [14]. Target-specific oral anticoagulants are a new class of medication for VTE prophylaxis that offer several advantages over LMWH, such as an oral route of administration, a more predictable pharmacokinetic profile, and no risk of heparin-induced thrombocytopenia (HIT). Similar to LMWH, these agents have few drug–drug and drug–food interactions and do not require routine monitoring and fast onset of action.
The purpose of this review is to discuss the increased risk of VTE in medically ill patients and the literature surrounding the efficacy and tolerability of LMWHs and TSOACs for thromboprophylaxis.
2 Literature Search Methods
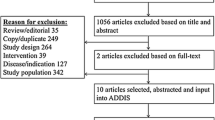
PubMed, MEDLINE, EBSCOhost, and clinictrials.gov were used as search engines in the literature review. The inclusion criteria of the search limits included articles containing human subjects, scholarly (peer-reviewed) journals written in English, and publication dates from 2004 to 2014. The exclusion criteria included animal studies, non-English articles, publications dated prior to 2004. An exception to the exclusion criteria was articles prior to 2004 that were deemed necessary to include for historical reference. Keywords searched were venous thromboembolism, VTE, thromboprophylaxis, deep vein thrombosis, DVT, pulmonary embolism, PE, low molecular weight heparin, LMWH, enoxaparin, dalteparin, target-specific oral anticoagulant, TSOAC, novel oral anticoagulant, NOAC, dabigatran, rivaroxaban, apixaban, and anticoagulation.
3 Discussion
Venous thromboembolism continues to be an ongoing issue in the medically ill population. In the absence of thromboprophylaxis, 5–15 % of hospitalized medical patients develop VTE. Furthermore, it has been shown that PE occurs more frequently in hospitalized medical patients than non-medical patients [15]. Approximately one-third of VTE patients will have a recurrent episode within 10 years, and up to 30 % will die within 1 month of diagnosis [16]. The American College of Chest Physicians (ACCP) suggests the use of thromboprophylaxis in any acutely ill hospitalized medical patients who are at increased risk of thrombosis and are not bleeding or at a high risk of bleeding [17]. LMWHs are recommended as first-line treatment, including dalteparin and enoxaparin. Relatively lackluster results with TSOACs have been shown. The current ACCP guidelines provide no recommendation supporting or discouraging the use of TSOACs for VTE prevention due to a lack of strong evidence with neither having a US FDA-approved indication for thromboprophylaxis at the time of publication [17].
3.1 Risk Factors
Balancing the risk of VTE with bleeding can be a daunting task in acutely ill medical patients. Studies have shown that, even with guidelines recommending the use of VTE prophylaxis in medically ill patients at risk of thrombosis, it may be underutilized [18]. The IMPROVE VTE (International Medical Prevention Registry on Venous Thromboembolism) study examined thromboprophylaxis in clinical practice. Looking at over 15,000 patients, it found that approximately 60 % of the patients who were considered eligible and would have benefited from pharmacological therapy actually received it [18].
Using the data from IMPROVE VTE, several risk calculators were developed in order to predict the development of VTE and bleeding risk. Spyropoulos et al. [19] developed a weighted VTE risk score derived from seven clinical factors for medically ill hospitalized patients. The following factors were identified as independently associated with the development of VTE (and points for VTE risk): previous VTE (3 points), known thrombophilia (2 points), cancer (2 points), age greater than 60 years (1 point), lower-limb paralysis (2 points), immobilization for at least 7 days (1 point), and admission to an intensive care unit (ICU) or coronary care unit (CCU) (1 point). A score of ≥2 was associated with a high risk of 3-month VTE mortality. Of the 184 patients observed, a score of 2 or 3 resulted in a 1.5 % VTE risk compared with 5.7 % for a score of ≥4 [19]. This risk assessment model (RAM) was later reviewed in the VTE-VALOURR (External Validation of a Risk Assessment Model for Venous Thromboembolism in the Hospitalised Acutely-ill Medical Patient) study, the first external validation of any evidence base-derived RAM in medically ill patients. In this large retrospective cohort, the seven independent risk factors of the aforementioned study were identified and separated patients in low (score of 0 or 1), moderate (score of 2 or 3), and high (score of 4 or more) VTE risk categories. The area under the receiver-operator characteristics curve was 0.7731, showing good discrimination and calibration of the three-tiered RAM point system [20].
Looking at bleeding risk, Decousus et al. [21] assessed the incidence of major and clinically relevant bleeding. The strongest independent risk factors (and points that were assigned to each factor) were the presence of an active gastroduodenal ulcer (4.5 points), prior bleeding 3 months before admission (4 points), and a platelet count of <50 × 109 cells/L (4 points). Other factors (and their scores) included age older than 84 years (3.5 points), international normalized ratio (INR) above 1.5 (2.5 points) or glomerular filtration ratio (GFR) below 30 mL/min/m2 (2.5 points), ICU or CCU stays (2.5 points), central venous catheter use (2 points), rheumatic disease (2 points), active cancer (2 points), male sex (1 points), and GFR between 30 and 59 mL/min/m2 (1 point). A score of ≥7 showed an exponentially increased risk of bleeding. More than 50 % of all major bleeding events occurred in 10 % of medically ill hospitalized patients for whom a score of ≥7 was established. Additionally, a mean score of 8.6 signified death due to bleeding [21]. A validated RAM for bleeding or a tool validating the overall risk-to-benefit ratio is the next step in research, as we move into this new era of VTE prevention in medically ill inpatients [22].
Other RAMs such as the Padua Prediction score and Geneva score are used to assess VTE risk. The Padua Prediction score combines patient-specific and disease-specific risk factors in patients admitted to internal medicine departments [22]. This assessment tool is used to classify patients as having a high or low risk of VTE according to the following criteria (and point scale): active cancer (3 points), previous VTE (3 points), bedrest for at least 3 days (3 points), already known thrombophilic condition (3 points), trauma and/or surgery within the last month (2 points), age ≥70 years (1 point), heart and/or respiratory failure (1 point), acute myocardial infarction or ischemic stroke (1 point), acute infection and/or rheumatologic disorder (1 point), body mass index (BMI) of ≥30 (1 point), and ongoing hormonal therapy (1 point). A score of ≥4 denotes a high risk of VTE [23]. Barbar et al. [23] first tested the use of this tool. The primary outcome, the risk of VTE in high-risk patients who had adequate thromboprophylaxis while inpatient compared with those who did not and compared with low-risk patients who received thromboprophylaxis, was analyzed. In the high-risk group, VTE occurred in 2.2 % of patients who received prophylaxis and in 11 % of those who did not (hazard ratio [HR] 0.13; 95 % confidence interval [CI] 0.04–0.40). In the low-risk group, VTE occurred in 0.3 % of those who were given thromboprophylaxis (HR 32; 95 % CI 4.1–251.0) [23]. The Padua Prediction Score helped further discriminate between medically ill patients at high and low risk of VTE and is utilized by the current ACCP antithrombotic guidelines, although it has not been validated in non-critically ill patients to date [17, 23]. The Geneva Risk Score’s algorithm was first evaluated in patients with high, intermediate, or low probability of PE admitted to the emergency department [24]. It was found that eight predictors showed a significant association with PE: recent surgery (odds ratio [OR] 4.6; 95 % CI 2.6–8.3; p < 0.001; point score +2), previous thromboembolic event (OR 3.0; 95 % CI 2.1–4.4; p < 0.001; point score +2), age between 60 and 79 years (OR 1.9; 95 % CI 1.3–2.7; p = 0.002; point score +1), age >80 (OR 2.8; 95 % CI 1.8–4.4; p < 0.001; point score +2), hypocapnia (OR 2.9; 95 % CI 1.9–4.4; p < 0.001; point score +2), hypoxemia (OR 7.2; 95 % CI, 3.2–15.8; p < 0.001; point score +4), tachycardia (OR 1.6; 95 % CI 1.1–2.2; p = 0.008; point score +1), band atelectasis (OR 1.9; 95 % CI 1.3–2.9; p = 0.001; point score +1), or elevation of a hemidiaphragm on chest X-ray (OR 1.6; 95 % CI 1.1–2.4; p = 0.02; point score +1), All levels of hypocapnia and hypoxemia were significantly associated with PE, but point scores varied based on degree of severity [24]. A cut-off score of ≤4 classified patients as low risk, 5–8 as intermediate risk, and ≥9 as high risk. Of the 1090 patients analyzed, 10 % were categorized as low risk and developed a PE, 38 % as intermediate risk and developed a PE, and 81 % as high risk score and developed a PE [24]. These RAMs were subsequently validated by the ESTIMATE (Explicit Assessment of Thromboembolic Risk and Prophylaxis for Medical Patients in Switzerland) trial, where the Geneva Risk Score was compared with the Padua Prediction Score in distinguishing between low- and high-risk patients while looking at symptomatic VTE or VTE-related death at 90 days as the primary endpoint [25]. This endpoint was shown in 3.2 % (95 % CI 0.022–0.046) of high-risk patients versus 0.6 % (95 % CI 0.002–0.019) in low-risk patients when utilizing the Geneva Risk Score, compared with 3.5 % (95 % CI 0.023–0.053) for high-risk patients and 1.1 % (95 % CI 0.006–0.023) in low-risk patients when using the Padua Prediction Score. The authors concluded that, amongst hospitalized medically ill patients, the Geneva Risk Score predicted VTE and VTE-mortality similarly to the Padua Prediction Score and was especially useful in identifying low-risk patients who may not require thromboprophylaxis [25]. Once the risk-to-benefit ratio of thromboprophylaxis versus bleeding is assessed, several pharmacological options can be chosen.
3.2 Dalteparin
The literature surrounding dalteparin in the medically ill is lacking, with only a few major clinical trials and post hoc analyses describing its efficacy and safety in VTE prevention. PREVENT (Prospective Evaluation of Dalteparin Efficacy for Prevention of VTE in Immobilized Patients Trial) looked at the efficacy and tolerability of dalteparin for thromboprophylaxis in low-risk medically ill patients [26]. Dalteparin was shown to significantly decrease the risk of VTE by 45 % compared with placebo (4.96 % in the placebo group vs. 2.77 % in the dalteparin group; absolute risk reduction [ARR] of 2.19 %; relative risk [RR] 0.55; 95 % CI 0.38–0.80; p = 0.0015). This benefit was shown to extend for at least 3 months. Additionally, there was an overall low risk of bleeding (0.49 % of patients receiving dalteparin and 0.16 % of those receiving placebo; p = 0.15) and thrombocytopenia observed [26].
Although dalteparin is not highly protein bound, in clinical practice it is suggested that prophylactic doses be increased in morbidly obese patients, defined as a BMI >40 kg/m2 [27]. This recommendation comes from subgroup analyses of obese and elderly hospitalized patients from PREVENT [27–29]. In these subgroups, a composite of symptomatic VTE, fatal PE, sudden death, or asymptomatic proximal DVT was reduced with dalteparin without an increased risk in major hemorrhage (obese patients 0 vs. 0.7 % placebo; p > 0.99; elderly patients 1.1 vs. 0.7 %; p = 0.12). In obese patients, the primary outcome showed a non-significant trend towards dalteparin compared with placebo (2.8 % of the dalteparin and 4.3 % of the placebo groups; RR 0.64; 95 % CI 0.32–1.28). In non-obese patients, the primary outcome was significantly decreased in the dalteparin group (RR 0.53; 95 % CI 0.34–0.82). Similarly, in individuals aged 75 years or older, the primary endpoint occurred significantly less in the dalteparin group (RR 0.52; 95 % CI 0.31–0.87) [28]. Patients with acute and chronic heart failure (HF), respiratory failure, infectious disease, rheumatological disorders, and varicose veins were also assessed, and no difference was found in thromboprophylaxis benefit between groups. The RR was 0.73 in patients with HF, 0.72 in those with respiratory failure, 0.46 in those with infectious disease, and 0.97 in those with rheumatological disorders. The RR was 0.52 in patients aged ≥75 years, 0.64 in obese patients, 0.34 for patients with varicose veins, and 0.71 in patients with chronic HF. No subgroup had a significantly different response from any other [29]. This suggests that VTE prevention with dalteparin should be used in a wide range of acutely ill hospitalized medical patients [29]. However, it is important to consider that, in disease states such as chronic kidney disease, the half-life of dalteparin can be increased. Therefore, in patients with a creatinine clearance (CrCl) of <30 mL/min, the manufacturer suggests using the recommended daily dose of 5000 units while obtaining anti-Xa levels [30].
The PROTECT (Prophylaxis for Thromboembolism in Critical Care Trial) is a unique study in that medical and surgical patients with any degree of renal function or dysfunction were included [31]. This phase III randomized, double-blinded study tested the superiority of dalteparin 5000 units daily versus UFH 5000 units twice daily in regards to the primary outcome, the prevention of proximal leg DVT. A total of 76 % of admissions were medically treated patients. The primary outcome occurred in 5.1 % of patients receiving dalteparin and in 5.8 % in those receiving UFH (HR 0.92; 95 % CI 0.68–1.23; p = 0.57). Of note, PE developed significantly less in the dalteparin group (1.3 %) compared with the UFH group (2.3 %) (HR 0.51; 95 % CI 0.30–0.88; p = 0.01). The rate of any VTE or VTE-related death did not differ between groups (HR 0.89; 95 % CI 0.79–1.01; p = 0.07). Major bleeding was also not significantly different between groups (HR 1.00; 95 % CI 0.75–1.34; p = 0.98) [31].
Advantages of dalteparin are its pharmacokinetics and low incidence of adverse effects. Dalteparin has a high bioavailability, allowing for once-daily administration. Additionally, a low incidence of HIT and osteopenia with long-term use has been demonstrated [32]. Dalteparin’s low affinity for plasma proteins makes it a useful agent in the morbidly obese and elderly populations. Also, severe adverse events have only been shown to occur rarely. However, it is important to keep in mind that HIT, anaphylactic reactions, skin necrosis, alopecia, rash, retroperitoneal, gastrointestinal, and intracranial hemorrhage, and spinal or epidural hematoma are uncommon, but possible and dalteparin should be avoided in patients with a history of any of the aforementioned [9].
3.3 Enoxaparin
Throughout the 1990s and early 2000s, clinical trials demonstrated that enoxaparin was as efficacious and safe as UFH in medically ill patients needing thromboprophylaxis [33–37]. Subsequently, a real-world comparison of the clinical and economic advantages of enoxaparin and UFH thromboprophylaxis in acute medically ill patients, including those with circulatory disorders, respiratory disorders, infectious diseases, or neoplasms, was performed [38]. A 74 % risk reduction in VTE among patients receiving enoxaparin prophylaxis versus UFH was established (RR 0.26; p < 0.001). Also, the occurrence of side effects, length of stay (10 days with enoxaparin vs. 10.26 days with UFH; p = 0.348), and total costs ($US18,777 vs. $US17,602; p = 0.463) were similar between the two groups [38].
In an attempt to define the level of thromboembolic risk in acutely ill medical patients the MEDENOX (Prophylaxis in Medical Patients with Enoxaparin) trial examined the risk–benefit ratio of 20 or 40 mg enoxaparin daily compared with placebo. The primary outcome, occurrence of documented VTE between days 1 and 14 of admission, was found to be significantly lower in the enoxaparin 40 mg group than in the placebo group (RR 0.37; 95 % CI 0.22–0.63; p < 0.001). No significant difference was observed between the enoxaparin 20 mg and placebo groups [39]. Further analysis of this study revealed independent factors related to an increased risk of VTE. Age older than 75 years (RR 1.51; 95 % CI 1.03–2.20; χ 2 4.22; p < 0.04), cancer (RR 1.74; 95 % CI 1.13–2.68; χ 2 5.46; p < 0.02), and previous VTE (RR 1.84; 95 % CI 1.15–2.94; χ 2 5.29; p < 0.02), were found to have a significantly high association with an increased risk of VTE. An acute infectious disease was the only acute medical illness found to significantly increase VTE risk (RR 1.47; 95 % CI 1.47–2.14; χ 2 3.59; p < 0.05). Acute respiratory failure (RR 0.63; 95 % CI 0.43–0.91; χ 2 5.72; p < 0.02) and chronic respiratory disease (RR 0.60; 95 % CI 0.42–0.88; χ 2 6.64; p < 0.01) showed a significant yet lower risk of VTE compared with other factors [40].
In order to examine the risk and benefits of long-term LMWH prophylactic therapy in acutely ill and immobile patients, the EXCLAIM (Extended Clinical prophylaxis in Acutely Ill Medical patients) study compared the incidence of VTE and safety using enoxaparin versus placebo [41]. After receiving open-label enoxaparin for an initial 10 ± 4 days, patients were randomized to receive extended-duration enoxaparin or placebo for an additional 28 ± 4 days. This extended-duration enoxaparin group reduced VTE incidence compared with placebo [2.5 vs. 4 %; absolute risk (AR) difference favoring enoxaparin –1.53 %; 95 % CI –2.54 to –0.52], but with an increase in major bleeding events (0.8 vs. 0.3 %; AR difference favoring placebo 0.51 %; 95 % CI 0.12–0.89). The benefits of extended-duration enoxaparin seemed to be restricted to women, patients aged >75 years, and those with level 1 immobility (total bed rest or sedentary state). A criticism of this trial is that a planned, blinded interim analysis was performed, which suggested the study was unlikely to show statistical significance of enoxaparin compared with placebo. As a result, the inclusion criteria were redefined to focus on enrollment of patients with a high risk of VTE. Of note, almost half of the patients were enrolled at this time [41]. Nevertheless, this study helps support the use of enoxaparin in several subgroups of medically ill patients in need of VTE prevention.
The LIFENOX (Mortality reduction of Enoxaparin in Hospitalized Acutely Ill Medical patients Receiving Enoxaparin) study aimed to find an association between mortality and thromboprophylaxis using enoxaparin compared with placebo [42]. Patients hospitalized due to acute decompensated HF, severe systemic infection with at least one risk factor for VTE, or active cancer were examined for the rate of death from any cause at 30 days. The primary safety outcome was the rate of major bleeding during and up to 48 h after the treatment period. Results showed that the rate of death from any cause at day 30 was 4.9 % in those receiving enoxaparin as compared with 4.8 % in those receiving placebo (RR 1.0; 95 % CI 0.8–1.2; p = 0.83) without an increased rate of major bleeding (0.4 % in the enoxaparin group and 0.3 % in the placebo group; RR 1.4; 95 % CI 0.7–3.1; p = 0.35). The composite of the incidence of sudden death or PE did not significantly differ between groups at 30 days (RR 1.0; 95 % CI 0.6–1.7; p = 0.97). In conclusion, enoxaparin thromboprophylactic therapy was not associated with a reduction in the rate of death from any cause among hospitalized acutely ill medical patients compared with placebo [42].
Similar to dalteparin, bleeding complications and HIT are possible with enoxaparin therapy. Elevations in serum aminotransferases, local injection site reactions, nausea, anemia, ecchymosis, edema, and peripheral edema have also been reported [10]. Enoxaparin has been well tolerated in pregnancy and in the elderly. The manufacturer suggests that anti-factor Xa levels in geriatric patients with low body weight (<45 kg) should be monitored. In morbidly obese patients with a BMI ≥40 kg/m2, it is suggested that the prophylactic dose of enoxaparin should be increased by 25 % and anti-factor Xa levels should be obtained. Anti-factor Xa monitoring is suggested in these patient populations because of the uncertainty surrounding the balance between sub-therapeutic levels and bleeding risk. Anti-factor Xa levels should be obtained 4 h after injection and monitored based on laboratory-specific goal ranges [27, 43]. In patients with severe renal dysfunction (CrCl <30 mL/min), enoxaparin concentration is significantly increased as it is renally excreted; therefore, dose adjustments are recommended with anti-factor Xa monitoring [10, 43].
A meta-analysis for thromboprophylaxis in medically ill patients compared LMWHs (including fondaparinux) with UFH and with placebo regarding thromboprophylaxis [44]. This analysis evaluated nine randomized controlled trials; it found DVT was significantly reduced in patients receiving LMWH compared with those receiving placebo (OR 0.60; 95 % CI 0.47–0.75; p < 0.001) and similarly with UFH (OR 0.92; 95 % CI 0.56–1.52). No significant difference in PE was observed amongst the LMWH, UFH, and placebo groups. Major bleeding was also comparable between all groups (LMWH/fondaparinux vs. placebo, OR 1.65; 95 % CI 0.8–3.4; LMWH/fondaparinux vs. UFH, OR 0.69; 95 % CI 0.29–1.68; LMWH/fondaparinux vs. UFH or placebo, OR 1.16; 95 % CI 0.66–2.04). Minor bleeding was increased in the LMWH and fondaparinux groups compared with placebo (OR 1.64; 95 % CI 1.18–2.29; p = 0.003). This investigation showed that LMWH, fondaparinux, and UFH are similar in effectiveness for the prevention of DVT, but not PE, with similar risks in bleeding [44].
Enoxaparin and dalteparin are both widely utilized agents for thromboprophylaxis that are supported by current guidelines and clinicians. However, a disadvantage of LWMH agents is the lack of reversal agents for bleeding events. Protamine sulfate, an effective antidote for UFH-related bleeding, has only been shown to neutralize the anti-Xa activity of these agents at a maximum of 60 % [10]. Choosing between enoxaparin and dalteparin can be cumbersome, as these medications are extremely similar in efficacy and safety. However, once an agent has been chosen it is important to consider that dalteparin and enoxaparin cannot be used interchangeably with UFH or each other as they differ in anti-Xa: anti-IIa ratio: UFH 1:1, dalteparin 2:1, enoxaparin 3:1 [8–10]. Each agent also differs in manufacturing process, molecular weight distribution, units and dosages [10]. Dalteparin may be more favorable in patients with renal dysfunction and allows for once-daily administration. Enoxaparin can be given as a 40 mg once-daily dose. Dose reduction to 30 mg once daily is recommended in medically ill patients with a CrCl <30 mL/min [10]. On the other hand, enoxaparin has been more extensively studied in special populations such as obesity, pregnancy, and elderly, but also in the medically ill population. Institution-specific formularies and protocol must also be considered when choosing between LMWH agents.
3.4 Fondaparinux
ACCP guidelines endorse the use of fondaparinux as a first-line agent for thromboprophylaxis in medically ill patients [17]. Less than a handful of case reports have described an occurrence of HIT with fondaparinux, which has a mechanism similar to that of LMWH [45–47]. It is indicated for the treatment of DVT or PE when administered in conjunction with warfarin [11]. The missing indication of prophylaxis in medically ill patients is based on the limited number of clinical trials showing benefit in this patient population.
ARTEMIS (Arixtra for Thromboembolism Prevention in a Medical Indications Study) was a major clinical trial focusing on medically ill patients [48]. This study examined thromboprophylaxis in elderly hospitalized medically ill patients receiving fondaparinux compared with placebo. Any VTE (e.g., DVT, PE, symptomatic DVT, fatal PE, non-fatal PE) was detected in 5.6 % of the fondaparinux treatment arm and in 10.5 % of the placebo arm [relative risk reduction (RRR) 46.7 %; 95 % CI 0.077–0.6983] with significantly less symptomatic VTE in the fondaparinux group (p = 0.029). Five fatal PEs occurred in the placebo group as opposed to none in the fondaparinux group. No difference in major bleeding or death was observed at follow-up. These results indicated that fondaparinux is effective for the prevention of VTE with a safety profile similar to that of placebo [48].
Like the LMWHs, the most common adverse reaction from fondaparinux is bleeding. Other less common side effects include injection site reactions, anemia, insomnia, hypokalemia, dizziness, hypotension, confusion, bullous eruption, hematoma, and purpura. Fondaparinux is renally eliminated and therefore should be avoided in patients with renal dysfunction (CrCl <30 mL/min) and with a low body weight (<50 kg), as the concentration of this medication will accumulate in the body, increasing the risk of bleeding. It has few drug–drug interactions, but caution should be taken in patients on medications that increase the risk of bleeding. Similarly, patients with bleeding disorders should also use this agent with caution, as protamine sulfate and other reversal agents are not effective when neutralizing this agent during bleeding occurrence [11].
3.5 Rivaroxaban
Rivaroxaban is one of the two direct factor Xa inhibitors that has recently been FDA approved for thromboprophylaxis following an initial 6 months of treatment for DVT and/or PE. In medically ill patients, the MAGELLAN (Multicenter, Randomized, Parallel Group Efficacy and Safety Study for the Prevention of Venous Thromboembolism in Hospitalized Acutely Ill Medical Patients Comparing Rivaroxaban with Enoxaparin) trial showed that extended-duration rivaroxaban was non-inferior to standard of care (enoxaparin) for the prevention of VTE (RR with rivaroxaban 0.97; 95 % CI 0.71–1.31; p = 0.003 for non-inferiority), but at the cost of an increased rate of bleeding events (RR 2.3; 95 % CI 1.63–3.17; p < 0.001) [49]. Patients were hospitalized for an acute medical illness and received either oral rivaroxaban 10 mg for 35 ± 4 days and subcutaneous placebo for 10 ± 4 days or subcutaneous enoxaparin 40 mg for 10 ± 4 days and oral placebo for 35 ± 4 days. The patient population included those with acute infectious or inflammatory diseases, including rheumatic diseases, acute HF, acute respiratory insufficiency, acute ischemic stroke, and active cancer. The primary efficacy endpoints were the composite of asymptomatic proximal DVT, symptomatic DVT, symptomatic non-fatal PE, and VTE-related death at days 10 and day 35. The primary safety outcome was the composite of treatment-emergent major and non-major clinically relevant bleeding events. At day 10, the primary efficacy endpoint occurred at the same rate in both treatment arms (2.7 vs. 2.7 %, p = 0.0025 for non-inferiority). At day 35, the primary efficacy endpoint occurred in 4.4 % of patients in the rivaroxaban group and in 5.7 % of patients in the enoxaparin followed by placebo group (p = 0.0211 for superiority). Rates of clinically relevant bleeding events were significantly higher in 2.8 % of patients receiving rivaroxaban than in 1.2 % of patients receiving enoxaparin (RR 2.3; 95 % CI 1.63–3.17; p < 0.001). Rates of other adverse events, including liver and cardiovascular events, and all-cause mortality were similar between treatment regimens [49].
Bleeding events, including fatal intracranial bleeding, and non-fatal intracranial, gastrointestinal, retroperitoneal, intraocular, or organ bleeding, have been reported in >1 % of patients treated with rivaroxaban. Dyspepsia, toothache, fatigue, sinusitis, and urinary tract infections have also been reported [12].
3.6 Apixaban
In 2014, the FDA approved apixaban for the treatment of DVT and PE, and for the reduction in risk of recurrent DVT and PE following initial therapy after 6 months of treatment for DVT or PE [13, 50]. Approval was based on the results shown in the AMPLIFY (Apixaban for the Initial Management of Pulmonary Embolism and Deep-Vein Thrombosis as First-Line Therapy) and AMPLIFY-EXT (Apixaban after the Initial Management of Pulmonary Embolism and Deep Vein Thrombosis with First-Line Therapy–Extended Treatment) studies that focused on treatment for symptomatic DVT and/or PE patients [51, 52]. AMPLIFY demonstrated non-inferiority to enoxaparin/warfarin regarding recurrent symptomatic VTE or VTE-related death over 6 months of therapy (RR 0.84; 95 % CI 0.60–1.18; p < 0.001) [51]. AMPLIFY-EXT showed apixaban was superior to placebo in recurrent VTE or all-cause death [52]. The AMPLIFY trial was associated with significantly less bleeding in the apixaban treatment arm (RR 0.31; 95 % CI 0.17–0.55; p < 0.001), whereas the rate of major bleeding did not significantly differ in AMPLIFY-EXT (RR 0.49; 95 % CI 0.09–2.64 and RR 0.25; 95 % CI 0.03–2.24 for apixaban 2.5 mg vs. placebo and apixaban 5 mg vs. placebo, respectively) [51, 52].
The ADOPT (Apixaban Dosing to Optimize Protection from Thrombosis) trial compared the efficacy and safety of long-term thromboprophylaxis in acutely ill patients who had CHF, respiratory failure, or other medical disorders and at least one additional risk factor for VTE receiving apixaban 2.5 mg twice daily versus enoxaparin 40 mg daily [53]. Results showed that the primary efficacy endpoint of composite death related to VTE, PE, symptomatic DVT, or asymptomatic proximal-leg DVT occurred in 2.71 % of the apixaban-treated patients and 3.06 % in the enoxaparin group (relative risk with apixaban 0.87; 95 % CI 0.62–1.23; p = 0.44). Over a timeframe of 1 month, major bleeding had occurred in 0.47 % of the patients receiving apixaban and 0.19 % of patients receiving enoxaparin (relative risk 2.58; 95 % CI 1.02–7.24; p = 0.04). Therefore, apixaban was not superior to enoxaparin therapy and was found to have significantly more bleeding events [53]. Interestingly, these results are very dissimilar to the results found in patients with symptomatic DVT/PE.
Bleeding events, including epistaxis, hematuria, hematoma, and gingival bleeding, have been reported in <4 % of patients treated with apixaban. Confusion has also been reported as a rare side effect [13].
As mentioned earlier, the lack of drug–drug and drug–food interactions, elimination of coagulation testing, and fast onset of action makes the TSOACs desirable. However, in patients with a history of non-adherence to medications, this class of medication may be less attractive as their duration of action requires good compliance in order to gain optimal coverage against VTE [12, 13]. Additionally, there is no reversal agent for rivaroxaban or apixaban when bleeding events occur. However, ongoing phase II and III trials are investigating the safety and effectiveness of promising agents such as andexanet alfa (PRT064445), a factor Xa inhibitor antidote [54, 55]. Rivaroxaban and apixaban have yet to show superior effectiveness and safety compared with conventional therapy for thromboprophylaxis in the medically ill population. The rationale is unknown, as these agents have the same mechanism of action and very similar pharmacokinetic and pharmacodynamic profiles. Criticisms surrounding the design of the ADOPT trial that may provide some explanation is that the trial was underpowered, making it difficult for conclusions to be drawn. Also, compression ultrasonography was used to screen for VTE at the time of hospital discharge, which is not typically performed in routine medically hospitalized patients. Despite the results shown in the ADOPT trial, the event rates of VTE compared with those in the EXCLAIM and MAGELLAN trials were similar at 30 days, with 3, 5, and 6 % in the ADOPT, EXCLAIM, and MAGELLAN trials, respectively. Regarding bleeding risks, the more recent MAGELLAN and ADOPT trials highlight that major bleeding rates appear to be lower with enoxaparin use compared with older trials, such as EXCLAIM, demonstrating that enoxaparin is an ideal comparator when comparing novel treatment options and standard treatment for VTE prevention in medically ill patients.
3.7 Current Clinical Guideline Recommendations
Recommendations for acutely ill hospitalized medical patients can be found in the ACCP or International Union of Angiology (IUA) journals [17, 56]. The ACCP guidelines recommend the implementation of thromboprophylaxis with LMWH daily, UFH twice daily, UFH thrice daily, or fondaparinux daily (grade 1B) in patients with an increased risk of thrombosis. On the other hand, if a patient is at low risk of thrombosis, the use of pharmacologic prophylaxis or mechanical prophylaxis is not suggested (grade 1B). Additionally, in patients who are actively bleeding or at a high risk for bleeding, thromboprophylaxis is not recommended (grade 1B). However, in patients actively bleeding, or at a high risk for bleeding and at an increased risk of thrombosis, mechanical thromboprophylaxis with graduated compression stockings or intermittent pneumatic compression is recommended (grade 2C). If the bleeding risk decreases over time, pharmacologic thromboprophylaxis should be employed (grade 2B). The duration of the initial course of therapy should not extend beyond the period of immobilization or hospital stay (grade 2B) [17].
The IUA guidelines echo the ACCP recommendations in stating that, in acutely ill medical patients, prophylaxis with UFH 5000 units thrice daily or LMWH (enoxaparin 40 mg once daily or dalteparin 5000 units once daily) is recommended in all patients who are deemed to require thromboprophylaxis (grade A). In patients with suspected or proven hemorrhagic stroke and in those with ischemic stroke where the risks of prophylactic anticoagulant therapy are perceived to outweigh the benefits, graduated compression stockings or intermittent pneumatic compression is recommended (grade B). These guidelines also highlight that patients aged ≥40 years with acute medical illness and/or reduced mobility should be considered for prophylaxis if they also have one of the following morbidities: acute HF New York Heart Association (NYHA) class III/IV, respiratory disease (respiratory failure with or without ventilation or exacerbation of respiratory disease), active cancer requiring therapy, acute infective disease including severe infection and sepsis, rheumatic disease, ischemic stroke, or acute myocardial infarction. Patients with acute medical illness with reduced mobility should also be considered for prophylaxis if they also have one of the following risk factors: history of VTE, malignant disease, or age over 75 years [56].
4 Future Outlooks
Information regarding the effectiveness and safety of thromboprophylaxis in medically ill bedridden patients is severely lacking, with enoxaparin providing the most data. With contrary results for rivaroxaban and apixaban, studies analyzing the medically ill patient population are desperately needed for TSOACs in thromboprophylaxis. Overall, there exists a major ‘hole’ in the present body of evidence for LMWH and TSOAC for VTE treatment or thromboprophylaxis in the acutely medically ill population. To date, there is one completed, unpublished phase III clinical trial looking at the efficacy and safety of thromboprophylaxis with certoparin, an LMWH, compared with UFH in acutely ill non-surgical patients. This study is investigating the incidence of DVT-, PE-, or VTE-related death over a 10-day treatment period. Hemorrhage and thrombocytopenia are also being evaluated [57]. This may help shed more light on the use of LMWHs for thromboprophylaxis in medically ill patients.
Pipeline medication, semuloparin (AVE5026, Mulsevo®; Sanofi), is part of a new generation of heparins called the ultra-low-molecular-weight heparins (molecular weight 2000–3000 Da). It is hemisynthetic and exhibits novel anti-thrombotic properties, resulting in high affinity against factor Xa and minimal activity against factor IIa. Pharmacokinetic studies have shown that the agent’s half-life is between 16 and 20 h, allowing for once-daily subcutaneous administration. Similar to fondaparinux, it is renally eliminated and not affected by the antidote, protamine sulfate. Presently, only one trial, SAVE-CEMED (Evaluation of AVE5026 in the Prevention of Venous Thromboembolism in Acutely Ill Medical Patients with Restricted Mobility), has attempted to examine this agent in medically ill patients. Unfortunately, this trial was terminated early before recruitment was completed [58].
In clinical practice, underutilization of thromboprophylaxis has been a problem amongst the medically ill population. The utilization of RAMs such as the Padua Prediction Score, Geneva Risk Score, and the IMPROVE-VTE risk calculator are part of a new shift in the medical field to better understand the risk-to-benefit ratio between the development of VTE and bleeding, and to identify patients who should be pharmacologically managed. For the first time, clinical trials are implementing RAMs to identify high-risk medical patients [22]. The MARINER (Medically Ill Patient Assessment of Rivaroxaban Versus Placebo in Reducing Post-Discharge Venous Thrombo-Embolism Risk) study is a phase III randomized, double-blinded trial investigating the efficacy and safety of rivaroxaban 10 mg or 7.5 mg compared with placebo in the prevention of symptomatic VTE and VTE-related death in post-hospital-discharge, high-risk, medically ill patients [59]. ‘High risk’ is defined in this study as a score of >3 using the IMPROVE-VTE risk score. The co-primary outcomes include time from randomization to the first occurrence of symptomatic VTE and VTE-related death up to day 45 and time from randomization to the first occurrence of major bleeding up to day 45 [59]. The APEX (Acute Medically Ill VTE Prevention with Extended Duration Betrixaban) study is a phase III randomized, double-blinded trial evaluating whether extended thromboprophylaxis with betrixaban 80 mg daily for 35–42 days is superior for the prevention of VTE in hospitalized medically ill patients compared with enoxaparin 40 mg daily for 10 days ± 4 days [60]. High-risk patients are included in this study and are identified using elements of the Padua Prediction Score. The primary outcome is the composite of VTE and VTE death through 35 days [60]. The results of these trials are expected to emerge between June and September 2015.
5 Conclusion
This review article focused on the evidence-based medical literature that has been produced in the last decade regarding the use of LMWHs and TSOACs for thromboprophylaxis in medically ill patients. A major gap remains in clinical trials and in the overall body of evidence discussing thromboprophylaxis in medically ill patients. This is unfortunate, since recurrent VTE remains an ongoing problem affecting thousands of people annually in the non-surgical population. LMWHs continue to be first-line therapy for thromboprophylaxis in medically ill patients. Rivaroxaban is the only TSOAC to show favorable efficacy in medically ill patients for thromboprophylaxis, but at the risk of bleeding. With limited data, it is not likely that TSOACs will soon replace LWMHs or even be considered an alternative until efficacy and tolerability have been established. Until further evidence is disclosed, LMWHs and fondaparinux (in the absence of renal dysfunction and low body weight) as well as UFH should continue to be utilized as first-line agents for thromboprophylaxis in medically ill patients.
References
Deitcher SR, Carman TL. Deep venous thrombosis and pulmonary embolism. Curr Treat Opt Cardiovasc Med. 2002;4:223–38.
Bergmann JF, Kher A. Venous thromboembolism in the medically ill patient: a call to action. Int J Clin Pract. 2005;59:555–61.
Surgeon General’s Call to Action To Prevent Deep Vein Thrombosis and Pulmonary Embolism. U.S. Department of Health and Human Services (HHS) under the direction of the Office of the Surgeon General and the National Heart, Lung, and Blood Institute (NHLBI) of the National Institutes of Health. Washington, DC; 2008.
Centers for Disease Control and Prevention (CDC). Venous thromboembolism in adult hospitalizations—United States, 2007–2009. MMWR Morb Mortal Wkly Rep. 2012;61:401–4.
National Institute for Health and Clinical Excellence. National Clinical Guideline Centre—Acute and Chronic Conditions (UK). Venous thromboembolism: reducing the risk and venous thromboembolism (deep vein thrombosis and pulmonary embolism) in patients admitted to hospital. NICE: London; 2010.
Fanikos J, Piazza G, Zayaruzny M, et al. Long-term complications of medical patients with hospital-acquired venous thromboembolism. Thromb Haemost. 2009;102:688–93.
Coumadin® [package insert]. Princeton: Bristol-Myers Squibb Co.; 2011.
Heparin sodium injection [package insert]. New York, NY; Pfizer, Inc.; 2013.
Fragmin® [package insert]. New York: Pfizer, Inc.; 2010.
Lovenox® [package insert]. Bridgewater: Sanofi-Aventis, LLC.; 2013.
Arixtra® [package insert]. Research Triangle Park, NC; GlaxoSmithKline Co.; 2013.
Xarelto® [package insert]. Titusville: Janssen Pharmaceuticals, Inc.; 2014.
Eliquis® [package insert]. Princeton: Pfizer, Inc.; 2014.
Weitz JL. Management of venous thromboembolism: present and future. Circulation. 2004;110:1–2.
Jaffer AK, Amin AN, Brotman DJ, et al. Prevention of venous thromboembolism in the hospitalized medical patient. Cleveland Clin J Med. 2008;75(Suppl 3):S7–16.
Center for Disease Control and Prevention. Deep vein thrombosis (DVT)/pulmonary embolism (PE)—blood clot forming in a vein. Updated 8 June 2012. http://www.cdc.gov/ncbddd/dvt/data.html. Accessed 30 Aug 2014.
Guyatt GH, Akl EA, Crowther M, et al. Antithrombotic therapy and prevention of thrombosis, 9th edition: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(Suppl):7S–47S.
Tapson VF, Decousus H, Pini M, et al. Venous thromboembolism prophylaxis in acutely ill hospitalized medical patients: findings from the International Medical Prevention Registry on Venous Thromboembolism. Chest. 2007;132:936–45.
Spyropoulos AC, Anderson FA, Fitzgerald G, et al. Predictive and associative models to identify hospitalized medical patients at risk for VTE. Chest. 2011;140:706–14.
Mahan CE, Liu Y, Turpie AG, et al. External validation of a risk assessment model for venous thromboembolism in the hospitalised acutely-ill medical patient (VTE-VALOURR). Thromb Haemost. 2014;112:692–9.
Decousus H, Tapson VF, Bergmann JF, et al. Factors at admission associated with bleeding risk in medical patients: findings from the IMPROVE investigators. Chest. 2011;139:69–79.
Squizzato A, Ageno W. A new era for venous thromboembolism prevention in medical inpatients. Thromb Haemost. 2014;112:627–8.
Barbar S, Noventa F, Rossetto V, et al. A risk assessment model for the identification of hospitalized medical patients at risk for venous thromboembolism: the Padua Prediction Score. J Thromb Haemost. 2010;8:2450–7.
Wicki J, Perneger TV, Junod AF, et al. Assessing clinical probability of pulmonary embolism in the emergency ward. Arch Intern Med. 2001;161:92–7.
Nendaz M, Spirk D, Kucher N, et al. Multicentre validation of the Geneva Risk Score for hospitalised medical patients at risk of venous thromboembolism. Explicit Assessment of Thromboembolic Risk and Prophylaxis for Medical Patients in Switzerland (ESTIMATE). Thromb Haemost. 2014;111:531–8.
Leizorovicz A, Cohen AT, Turpie AG, et al. Randomized, placebo-controlled trial of dalteparin for the prevention of venous thromboembolism in acutely ill medical patients. Circulation. 2004;110:874–9.
Nutescu EA, Spinler SA, Wittkowsky A, et al. Low-molecular-weight heparins in renal impairment and obesity: available evidence and clinical practice recommendations across medical and surgical settings. Ann Pharmacother. 2009;43:1064–83.
Kucher N, Leizorovicz A, Vaitkus PT, et al. Efficacy and safety of fixed low-dose dalteparin in preventing venous thromboembolism among obese or elderly hospitalized patients: a subgroup analysis of the PREVENT trial. Arch Intern Med. 2005;165:341–5.
Cohen AT, Turpie AG, Leizorovicz A, et al. Thromboprophylaxis with dalteparin in medical patients: which patients benefit? Vasc Med. 2007;12:123–8.
Pincus KJ, Hynicka L. Prophylaxis of thromboembolic events in patients with nephrotic syndrome. Ann Pharmacother. 2013;47:725–34.
Cook D, Meade M, Guyatt G, et al. Dalteparin versus unfractionated heparin in critically ill patients. N Engl J Med. 2011;364:1305–14.
Pineo GF, Hull RD. Dalteparin: pharmacological properties and clinical efficacy in the prophylaxis and treatment of thromboembolic diseases. Eur J Med Res. 2004;9:215–24.
Bergmann JF, Neuhart E. A multicenter randomized double blind study of enoxaparin compared with unfractionated heparin in the prevention of venous thromboembolic disease in elderly in-patients bedridden for an acute medical illness. Thromb Haemost. 1996;76:529–34.
Harenberg J, Kallenbach B, Martin U, et al. Randomized controlled study of heparin and low-molecular weight heparin for prevention of deep vein thrombosis in medical patients. Thromb Res. 1990;59:639–50.
Harenberg J, Roebruck P, Heene DL. Subcutaneous low-molecular-weight heparin versus standard heparin and the prevention of thromboembolism in medical inpatients. Haemostasis. 1996;26:127–39.
Lechler E, Schramm W, Flosbach CW, et al. The venous thrombotic risk in non-surgical patients: epidemiological data and efficacy/safety profile of a low-molecular weight heparin (enoxaparin). Haemostasis. 1996;26(Suppl 2):49–56.
Kleber FX, Witt C, Vogel G, et al. Randomized comparison of enoxaparin with unfractionated heparin for the prevention of venous thromboembolism in medical patients with heart failure or severe respiratory disease. Am Heart J. 2003;145:614–21.
McGarry LJ, Stokes ME, Thompson D. Outcomes of thromboprophylaxis with enoxaparin vs unfractionated heparin in medical inpatients. Thromb J. 2006;4:17.
Samama MM, Cohen AT, Darmon JY, et al. A comparison of enoxaparin with placebo for the prevention of venous thromboembolism in acutely ill medical patients: prophylaxis in Medical Patients with Enoxaparin Study Group. N Engl J Med. 1999;341:793–800.
Alikhan R, Cohen AT, Combe S, et al. Risk factors for venous thromboembolism in hospitalized patients with acute medical illness: analysis of the MEDENOX study. Arch Intern Med. 2004;164:963–8.
Hull RD, Schellong SM, Tapson VF, et al. Extended-duration venous thromboembolism prophylaxis in acutely ill medical patients with recently reduced mobility: a randomized trial. Ann Intern Med. 2010;153:8–18.
Kakker AK, Cimminiello C, Goldhaber SZ, et al. Low-molecular weight heparin and mortality in acutely ill medical patients. N Engl J Med. 2011;365:2463–72.
Shogbon A, Marshall J. Utilization of low molecular weight heparins in special populations: renal impairment and obesity. ASHP: New Practitioners Forum. 2011.
Kanaan AO, Silva MA, Donovan JL, et al. Meta-analysis of venous thromboembolism prophylaxis in medically ill patients. Clin Ther. 2007;29:2395–405.
Warkentin TE, Maurer BT, Aster RH. Heparin-induced thrombocytopenia associated with fondaparinux. N Engl J Med. 2007;356:2653–5.
Rota E, Bazzan M, Fantino G. Fondaparinux-related thrombocytopenia in a previous low-molecular-weight heparin (LMWH)-induced heparin-induced thrombocytopenia (HIT). Thromb Haemost. 2008;99:779–81.
Burch M, Cooper B. Fondaparinux-associated heparin-induced thrombocytopenia. Proc (Bayl Univ Med Cent). 2012;25:13–5.
Cohen AT, Davidson BL, Callus AS, et al. Efficacy and safety of fondaparinux for the prevention of venous thromboembolism in older acute medical patients: randomized placebo controlled trial. BMJ. 2006;7537:325–9.
Cohen AT, Spiro TE, Buller HR, et al. Rivaroxaban for thromboprophylaxis in acutely ill medical patients. N Engl J Med. 2013;368:513–23.
US FDA Approves Eliquis (apixaban) for the Treatment of Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE), and for the Reduction in the Risk of Recurrent DVT and PE Following Initial Therapy [press release]. http://www.pfizer.com/news/press-release/press-release-detail/u_s_fda_approves_eliquis_apixaban_for_the_treatment_of_deep_vein_thrombosis_dvt_and_pulmonary_embolism_pe_and_for_the_reduction_in_the_risk_of_recurrent_dvt_and_pe_following_initial_therapy. Accessed 29 Aug 2014.
Agnelli G, Buller HR, Cohen A, et al. Oral apixaban for the treatment of acute venous thromboembolism. N Engl J Med. 2013;369:799–808.
Agnelli G, Buller HR, Cohen A, et al. Apixaban for extended treatment of venous thromboembolism. N Engl J Med. 2013;368:699–708.
Goldhaber SZ, Leizorovicz A, Kakkar AK, et al. Apixaban versus enoxaparin for thromboprophylaxis in medically ill patients. N Engl J Med. 2011;365:2167–77.
Crowther M, Kitt M, Lorenz T, et al. A phase 2 randomized, double-blind, placebo-controlled trial of PRT4445, a novel, universal antidote for direct and indirect Factor Xa inhibitors. In: Presented at the International Society on Thrombosis and Haemostasis Congress. Amsterdam; 2013.
Lu G, DeGuzman FR, Hollenbach SJ, et al. A specific antidote for reversal of anticoagulation by direct and indirect inhibitors of coagulation factor Xa. Nat Med. 2013;19:446–51.
Nicolaides AN, Fareed J, Kakkar AK, et al. Prevention and treatment of venous thromboembolism. International Consensus Statement (guidelines according to scientific evidence). Int Angiol. 2006;25:101–61.
Efficacy and safety of low-molecular weight heparin for thromboprophylaxis in acutely ill medical patients. http://clinicaltrials.gov/show/NCT00311753. Accessed 30 Aug 2014.
Evaluation of AVE5026 in the prevention of venous thromboembolism in acutely ill medical patients with restricted mobility. http://clinicaltrials.gov/ct2/show/results/NCT00714597. Accessed 31 Aug 2014.
A study of rivaroxaban (JNJ-39039039) on the venous thromboembolic risk in post-hospital discharge patients (MARINER). https://clinicaltrials.gov/ct2/show/NCT02111564. Accessed 8 Feb 2015.
Acute medically ill VTE prevention with extended duration betrixaban study (The APEX Study). https://clinicaltrials.gov/ct2/show/study/NCT01583218. Accessed 8 Feb 2015.
Pradaxa® [package insert]. Ridgefield: Boehringer Ingelheim Pharmaceuticals, Inc.; 2015.
Savaysa® [package insert]. Parisippany: Daiichi Sankyo, Co.; 2015.
Betrixaban: FXa inhibitor. http://www.portola.com/clinical-development/betrixaban-fxa-inhibitor/ Accessed 8 Feb 2015.
Compliance with ethical standards
Drs. Genevieve Hale and Michael Brenner do not have any conflicts of interest or funding to disclose. No internal or external sources of financial assistance were used to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hale, G., Brenner, M. Risks and Benefits of Low Molecular-Weight Heparin and Target-Specific Oral Anticoagulant Use for Thromboprophylaxis in Medically Ill Patients. Am J Cardiovasc Drugs 15, 311–322 (2015). https://doi.org/10.1007/s40256-015-0122-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-015-0122-7