Abstract
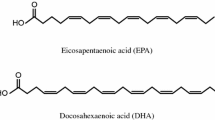
Icosapent ethyl (Vascepa®) is a high-purity ethyl ester of eicosapentaenoic acid (EPA) that is de-esterified to EPA following oral administration. Both EPA and docosahexaenoic acid (DHA) are long-chain omega-3 fatty acids that have been associated with triglyceride (TG)-lowering. However, DHA has been associated with increased low-density lipoprotein cholesterol (LDL-C) levels. Icosapent ethyl contains ≥96 % of the EPA ethyl ester, does not contain DHA, and is approved in the USA for use as an adjunct to diet to lower TG levels in adult patients with severe (≥500 mg/dL [≥5.65 mmol/L]) hypertriglyceridemia. In a pivotal phase III trial, oral icosapent ethyl 4 g/day significantly decreased the placebo-corrected median TG levels by 33.1 %. It did not increase LDL-C, had favorable effects on other lipid parameters, and had a tolerability profile similar to that of placebo. Therefore, icosapent ethyl is an effective and well-tolerated agent for the treatment of severe hypertriglyceridemia in adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
An omega-3 fatty acid product that predominantly contains eicosapentaenoic acid ethyl ester, and does not contain docosahexaenoic acid |
Significantly reduces triglyceride (TG) levels and has favorable effects on other lipid parameters |
Well tolerated in clinical trials with the numerical incidence of adverse events in patients taking icosapent ethyl similar to that of patients on placebo; only arthralgia was reported as occurring more often with icosapent ethyl than with placebo |
The only prescription omega-3 fatty acid product available in the USA that reduces TG levels without increasing low-density lipoprotein cholesterol levels |
1 Introduction
Hypertriglyceridemia, a condition of elevated serum triglyceride (TG) levels of >150 mg/dL (>1.7 mmol/L), affects approximately 31–33 % of adults in the United States [1–3]. Hypertriglyceridemia can stem from various familial disorders, but it is also associated with obesity and other secondary causes such as type II diabetes mellitus and various drugs [4, 5]. The National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) classifies fasting TG levels of <150 mg/dL (<1.7 mmol/L) as desirable, 150–199 mg/dL (1.7–2.3 mmol/L) as borderline high, 200–499 mg/dL (2.3–5.6 mmol/L) as high, and ≥500 mg/dL (≥5.6 mmol/L) as very high [5, 6]. According to data from the National Health and Nutrition Examination Survey (NHANES) in US adults, one in five has a TG level of ≥200 mg/dL and one in fifty has a TG level of ≥500 mg/dL [7].
High levels of TGs have been associated with a higher risk of cardiovascular death, cardiovascular events, myocardial infarction, and all-cause mortality [3, 8]. In addition, very high levels of TGs have been associated with acute pancreatitis [2, 3]. A meta-regression analysis of large, controlled fibrate trials demonstrated an association between TG lowering and the reduced risk of major cardiovascular events [8]. Eicosapentaenoic acid (EPA), an omega-3 fatty acid, significantly reduced the risk of major coronary events when added to statin therapy, in Japanese patients with low high-density lipoprotein cholesterol (HDL-C) levels and TG levels ≥150 mg/dL, as compared with statin monotherapy [9]. In the AIM-HIGH study of extended-release niacin, a trend toward cardiovascular risk reduction was seen in a sub-analysis of patients with low HDL-C levels and TG levels ≥198 mg/dL [10]. However, a significant reduction in the risk of major vascular events was not seen in an exploratory analysis of the HPS2-THRIVE study in which extended-release niacin-laropiprant was added to statin-based cholesterol-lowering therapy in patients with low HDL-C levels and TG levels >151 mg/dL [11]. Although a large, randomized trial examining the cardiovascular outcomes of lowering TG levels in high-risk, statin-treated patients with hypertriglyceridemia is currently underway (Sect. 8), no large-scale, randomized trial has provided conclusive evidence yet of the link between lowering TGs and reducing the risk of cardiovascular diseases [8]. However, recent studies suggest that raised levels of remnant cholesterol, marked by raised TGs, are a causal risk factor for cardiovascular disease and all-cause mortality [8].
The NCEP ATP III [5], the US Endocrine Society [6], and the American Heart Association [2] recommend intensive lifestyle changes (i.e., diet, weight reduction, and exercise) as first-line therapy for patients with borderline high TG levels. TG-lowering drugs (i.e., fibrates, niacin, long-chain omega-3 fatty acids, statins, and ezetimibe [2]) should be considered as additional treatment options in patients with TG levels ≥200 mg/dL [3, 5, 6]. In patients with borderline high or high TG levels, lowering low-density lipoprotein cholesterol (LDL-C) is the primary goal, while in those with very high TG levels, TG-lowering is the primary goal in order to prevent acute pancreatitis [5].
Comparing the efficacy of TG-lowering treatments when used as monotherapy, fibrates produce the greatest reduction in TG levels (30–50 %), followed by immediate-release niacin (20–50 %), omega-3 ethyl esters (20–50 %), extended release niacin (10–30 %), statins (10–30 %), and ezetimibe (5–10 %) [2]. Although fibrates and niacin are effective TG-lowering drugs, their use has been limited mainly due to concerns related to tolerability and drug interactions [4]. Omega-3 fatty acids offer a well-tolerated and effective treatment alternative to fibrates and niacin in lowering TG levels [7].
Of the three major long-chain omega-3 fatty acid components, the TG-lowering effects of omega-3 fatty acids have been attributed to the docosahexaenoic acid (DHA) and EPA components [7]. In addition to lowering TG levels, both DHA and EPA are thought to improve vascular and cardiac hemodynamics as well as cardiovascular endpoints [12]. For instance, DHA may reduce the risk of atrial fibrillation, fatal coronary heart disease, and sudden death. On the other hand, EPA may reduce the risk of congestive heart failure and nonfatal coronary syndromes [12]. However, mixed preparations of DHA and EPA, as well as DHA alone, have been found to increase LDL-C levels, especially in patients with very high TG levels [4]. This can compromise therapeutic interventions aimed at lowering LDL-C levels [4, 7]. There is a need for a well-tolerated product that lowers TG levels without raising levels of LDL-C [7] or apolipoprotein (Apo) B, a surrogate marker for atherogenic particles in the circulation [2, 13].
Icosapent ethyl (Vascepa®; formerly AMR101) is a high-purity prescription form of EPA ethyl ester [14]. It contains ≥96 % EPA ethyl ester, does not contain DHA, and therefore, would not be expected to increase LDL-C levels [4]. Icosapent ethyl was approved by the FDA in 2012 as an adjunct to diet to reduce levels of TGs in adult patients with severe (≥500 mg/dL) hypertriglyceridemia [14]. This article provides a narrative review of the pharmacologic properties of icosapent ethyl relevant to TG lowering, and its efficacy and tolerability in the treatment of severe hypertriglyceridemia.
2 Pharmacodynamic Properties
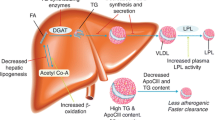
Icosapent ethyl is an ethyl ester of EPA, a long-chain omega-3 fatty acid [14, 15]. EPA is thought to reduce TG levels by enhancing the clearance of TGs from circulating very-low-density lipoprotein (VLDL) particles and by reducing hepatic VLDL-TG synthesis and/or secretion [14]. Potential mechanisms of action include inhibition of acyl-CoA:1,2-diacylglycerol acyltransferase (DGAT), increased beta-oxidation, increased plasma lipoprotein lipase activity, and decreased hepatic lipogenesis [14].
Previous human studies showed that omega-3 fatty acids decrease VLDL-TG, LDL-Apo B, and VLDL-Apo B formation [16, 17]. Animal studies indicated that purified EPA inhibits VLDL-TG secretion by reducing cellular TG synthesis, and that EPA reduces DGAT activity [16, 17]. In an animal study in which high fat diet-fed hamsters were administered highly purified EPA and DHA separately, EPA was found to have no apparent effect on LDL-C, while DHA was found to increase LDL-C [18].
An exploratory analysis of the MARINE study (see Table 1 for trial design details) that examined the effects of icosapent ethyl on lipoprotein particle sizes and concentrations in patients with baseline TG levels ≥500 and ≤2,000 mg/dL concluded that icosapent ethyl 4 g/day significantly decreased VLDL particle size and decreased particle concentrations of total HDL, small LDL, total LDL, and large VLDL compared with placebo (Table 2) [19]. A separate analysis (abstract plus poster) indicated that icosapent ethyl 4 g/day also significantly decreased remnant-like particle cholesterol (RLP-C) levels compared with placebo in the MARINE study (Table 2), with the greatest reductions among patients with baseline TG levels >750 mg/dL [20]. RLP-C levels were reduced to a significant extent in both statin-treated patients and patients not receiving statins [20].
Another exploratory analysis of the MARINE study examining the effect of icosapent ethyl on plasma and red blood cell (RBC) fatty acid profiles concluded that icosapent ethyl significantly raised EPA plasma and RBC concentrations in a dose-dependent and linear manner, caused beneficial changes in the fatty acid profile, decreased the arachidonic acid/EPA ratio significantly in plasma and RBCs, and significantly increased DPA n-3 (metabolite of EPA) (Table 3) [21]. A separate study on icosapent ethyl also showed a dose-dependent and linear increase in EPA plasma and RBC concentrations compared with baseline [22, 23].
A follow-up analysis assessing the effect of icosapent ethyl compared with placebo on inflammatory markers linked with atherosclerosis and cardiovascular disease in patients who received icosapent ethyl 4 g/day in the MARINE study showed a significant decrease in the high-sensitivity C-reactive protein level, in addition to the lipoprotein associated phospholipase A2 (Lp-PLA2) level (Table 2), but no significant change in the levels of intercellular adhesion molecule-1, oxidized LDL, or interleukin-6 [24].
An additional follow-up analysis (abstract plus poster) of the MARINE study showed a significant reduction in Apo C-III levels with icosapent ethyl 4 g/day compared with placebo (Table 2) [25].
Other potential benefits of icosapent ethyl, which are outside the scope of this review, include anti-inflammatory effects, endothelial protective effects, antidysrhythmic effects, the lowering of heart rate and blood pressure, and beneficial alterations in other atherogenic lipids and lipoproteins [4, 7].
3 Pharmacokinetic Properties
3.1 Absorption and Distribution
Following oral administration, icosapent ethyl is de-esterified to the active metabolite EPA [14]. EPA is absorbed in the small intestine and enters the systemic circulation primarily through the thoracic duct lymphatic system. Food effect studies have not been performed, but icosapent ethyl was given with food or following a meal in all clinical studies. Icosapent ethyl exhibits a linear and dose-dependent relationship with plasma EPA concentrations and does not affect plasma DHA levels [21]. Peak plasma EPA concentrations (Cmax) were attained approximately 5 hours after administration, and steady state was attained by day 14 [14, 26]. Following the administration of icosapent ethyl 4 g/day for 28 days, the steady-state EPA Cmax was 347 µg/mL and the area under the EPA plasma concentration–time curve (AUC) from time zero to 24 h (AUC24) was 6,519 µg·h/mL. The majority of circulating EPA in plasma is incorporated in cholesteryl esters, triglycerides, and phospholipids, with <1 % present as the unesterified fatty acid. More than 99 % of the unesterified EPA is bound to plasma proteins. At steady state, the mean volume of distribution of EPA is approximately 88 L [14, 26].
3.2 Metabolism and Elimination
EPA is metabolized predominantly by beta-oxidation in the liver [14]. EPA is also known to be metabolized by cytochrome P450 (CYP) enzymes, cyclo-oxygenases, and lipoxygenases [27]. However, EPA is not expected to interfere with CYP-mediated pathways because CYP-mediated metabolism is only a minor pathway for EPA elimination [14, 15].
At steady state, the total plasma clearance of EPA is 684 mL/h [14, 26]. EPA has a plasma elimination half-life of approximately 89 h [14, 26]. Icosapent ethyl does not undergo renal excretion [14].
4 Drug Interactions
Long-chain omega-3 fatty acids have the potential for antithrombotic effects [15]. However, when co-administered with racemic warfarin 25 mg in healthy adult patients, icosapent ethyl did not alter the anti-coagulation pharmacodynamics of the drug [14, 15]. No serious bleeding events were reported, supporting previous findings that omega-3 fatty acids do not increase bleeding risk [15]. However, the periodic monitoring of patients receiving icosapent ethyl together with other drugs affecting coagulation (e.g. anti-platelet drugs) is recommended [14].
No pharmacokinetic drug–drug interactions were seen with icosapent ethyl 4 g/day and typical CYP substrates in healthy adult subjects [14]. Icosapent ethyl 4 g/day did not significantly alter the steady-state Cmax or AUC for omeprazole and atorvastatin, or the single dose Cmax or AUC of rosiglitazone and warfarin [14, 15, 28–30]. Some studies are available as abstracts [28, 29].
5 Therapeutic Efficacy
The TG-lowering efficacy of icosapent ethyl in adult patients with very high (≥500 and ≤2,000 mg/dL [≥5.6 and ≤22.4 mmol/L]) fasting TG levels was assessed in the phase III, randomized, double-blind, placebo-controlled, multinational MARINE study [13], which is the focus of this section. Table 1 summarizes key design features and baseline characteristics for the 12-week study. The baseline demographics were similar across all treatment groups [13].
Following a 4- to 6-week lead-in period, during which patients’ diet, medication and lifestyle were stabilized, patients (n = 229) with average fasting TG levels ≥500 and ≤2,000 mg/dL were randomized to therapy with oral icosapent ethyl 1 or 2 g or placebo twice daily, for 12 weeks [13]. The duration of the lead-in period was 4 weeks in untreated patients and those taking permitted lipid-altering drugs, and 6 weeks in those discontinuing prohibited lipid-altering therapy (see Table 1). The primary endpoint was the placebo-corrected median percentage change in TG level from baseline to week 12 in the modified intent-to-treat (mITT) population, defined as all randomized patients with a baseline efficacy measurement, who received at least one dose of the study drug, and who had at least one post-randomization efficacy measurement. Additional efficacy endpoints included changes from baseline to 12 weeks in other lipid components. Although the trial included an icosapent ethyl 2 g/day treatment arm, the 2 g/day dosage was less effective than the 4 g/day dosage [13] and is not an approved dosage [14]. Therefore, only the results for the approved 4 g/day dosage are discussed.
Oral icosapent ethyl 4 g/day significantly reduced from baseline the placebo-corrected median TG level by 33.1 % (see Table 2) [13]. Results were consistent in the per-protocol population (defined as all patients in the mITT population who completed the 12-week treatment period with no major protocol deviations) [13].
Improvements from baseline to week 12 in other lipid parameters assessed as secondary and exploratory efficacy endpoints showed that icosapent ethyl 4 g/day significantly decreased the placebo-corrected median levels of non-HDL-C, total cholesterol (TC), VLDL-C, VLDL-TG, Apo B, and Lp-PLA2 (see Table 2) [13]. A noteworthy finding was that icosapent ethyl did not significantly increase LDL-C. Subgroup analyses of patients receiving icosapent ethyl 4 g/day in the mITT population showed significant reductions in placebo-corrected median TG levels from baseline to week 12 in statin-treated patients (65 % reduction in placebo-corrected median TG levels; p = 0.0001) and patients with baseline TG levels >750 mg/dL (45.4 % reduction in placebo-corrected median TG levels; p = 0.0001) [13].
6 Tolerability
This section focuses on tolerability data from the phase III study [13] discussed in Sect. 5, supplemented by data from the US prescribing information [14].
Treatment-emergent adverse events in the study were experienced by 35 % of patients receiving icosapent ethyl 4 g/day and 37 % of patients receiving placebo [13]. The incidence and severity of adverse events were descriptively similar between all treatment groups. Gastrointestinal treatment-emergent adverse events were the most common, having a numerically higher incidence with placebo than with icosapent ethyl 4 g/day (16 vs. 2 %). Diarrhea and nausea occurred in 7 and 5 % of patients, respectively, in the placebo group compared with 1 % each in the icosapent ethyl 4 g/day group [13].
Treatment-emergent adverse events were mostly mild to moderate in severity, and most were deemed unrelated to the study drug [13]. One serious adverse event (coronary artery disease) occurred in the icosapent ethyl 4 g/day group, but investigators who were unaware of the treatment groups determined that it was not related to the study drug. No deaths occurred during the study, and there were no significant changes in the icosapent ethyl 4 g/day group with respect to AST, ALT and creatine kinase levels, electrocardiographic parameters, and vital signs. In addition, icosapent ethyl 4 g/day did not significantly alter fasting plasma glucose levels compared with placebo [13].
In a phase III, randomized, double-blind, placebo-controlled, multicenter study (the ANCHOR study), which was an investigational (off-label) study of icosapent ethyl in statin-treated patients with high (≥200 to <500 mg/dL) TG levels, only arthralgia occurred in more patients receiving icosapent ethyl (1.7 % for 4 g/day and 3.4 % for 2 g/day) than in patients receiving placebo (0.4 %) [14, 31]. The US prescribing information also states that oropharyngeal pain was an additional adverse reaction [14].
7 Dosage and Administration
Icosapent ethyl is approved in the US for use as an adjunct to diet for the reduction of TG levels in adult patients with severe (≥500 mg/dL) hypertriglyceridemia [14]. Prior to commencing icosapent ethyl therapy, patients should have a lipid-lowering diet and an exercise regimen in place. The recommended dosage of icosapent ethyl is two 1 g capsules twice daily (4 g/day) orally with food. The capsules should be swallowed whole and should not be broken open, chewed, crushed, or dissolved [14].
Adequate and well-controlled studies have not been conducted in pregnant women [14]. In addition, the safety and efficacy of icosapent ethyl has not been established in pediatric patients. Although greater sensitivity cannot be ruled out in the geriatric population, overall variations in response have not been identified between elderly and younger patients. Icosapent ethyl has not been studied in patients with hepatic or renal impairment. AST and ALT levels should be monitored periodically in patients with liver impairment, and icosapent ethyl should be used with caution in patients with fish or shellfish allergies [14].
Local prescribing information should be consulted for detailed information, including contraindications, precautions, drug interactions, and use in special patient populations.
8 Current Status of Icosapent Ethyl in Hypertriglyceridemia
Icosapent ethyl is currently one of more than three FDA-approved prescription omega-3 fatty acid products indicated as an adjunct to diet for TG-lowering in adults with severe (≥500 mg/dL) hypertriglyceridemia [14, 32–35]. Unlike omega-3 acid ethyl esters (Lovaza®, Omtryg®, and generics), which contain ethyl esters of EPA and DHA, and omega-3 carboxylic acids (Epanova®), which contains free fatty acid forms of EPA and DHA, icosapent ethyl contains a highly purified form of EPA ethyl ester without any DHA [7, 23, 34, 35]. In a well-controlled clinical trial, icosapent ethyl 4 g/day was shown to significantly (p < 0.0001) lower TG levels without increasing LDL-C levels (Sect. 5). Icosapent ethyl was also shown to be well tolerated (Sect. 6).
The primary goal of therapy for patients with very high TGs is avoiding acute pancreatitis, and the secondary goal is preventing cardiovascular disease [4, 5]. Although icosapent ethyl reduces TG levels effectively, its effect on the risk of cardiovascular mortality and morbidity and pancreatitis in patients with severe hypertriglyceridemia has not been determined [14].
However, the ongoing, large, phase III trial, REDUCE-IT, in high-risk, statin-treated patients with persistent hypertriglyceridemia, is assessing the efficacy of icosapent ethyl 4 g/day in preventing a first major cardiovascular event [7, 36]; results are expected in 2018 [37].
In conclusion, icosapent ethyl is a novel omega-3 fatty acid agent that lowers TG levels without significantly altering LDL-C levels. It is an effective and well-tolerated adjunct to diet in patients with TG ≥500 mg/dL.
Data selection sources:
Relevant medical literature (including published and unpublished data) on icosapent ethyl (Vascepa®) was identified by searching databases including MEDLINE (from 1946) and EMBASE (from 1996) [searches last updated November 15, 2014], bibliographies from published literature, clinical trial registries/databases and websites. Additional information was also requested from the company developing the drug.
Search terms: Icosapent ethyl, Vascepa, hypertriglyceridaemia, hypertriglyceridemia.
Study selection: Studies in patients with severe hypertriglyceridemia who received icosapent ethyl (Vascepa®). When available, large, well designed, comparative trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
References
Jacobson TA, Glickstein SB, Rowe JD, et al. Effects of eicosapentaenoic acid and docosahexaenoic acid on low-density lipoprotein cholesterol and other lipids: a review. J Clin Lipidol. 2012;6(1):5–18.
Miller M, Stone NJ, Ballantyne C, et al. Triglycerides and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2011;123(20):2292–333.
Murad MH, Hazem A, Coto-Yglesias F, et al. The association of hypertriglyceridemia with cardiovascular events and pancreatitis: a systematic review and meta-analysis. BMC Endocr Disord. 2012. doi:10.1186/1472-6823-12-2.
Jacobson TA. Perspectives on a new prescription omega-3 fatty acid, icosapent ethyl, for hypertriglyceridemia. Clin Lipidol. 2014;9(2):149–61.
American Heart Association. Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) final report. Circulation. 2002;106(25):3143–421.
Berglund L, Brunzell JD, Goldberg AC, et al. Evaluation and treatment of hypertriglyceridemia: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2012;97(9):2969–89.
Bradberry JC, Hilleman DE. Overview of omega-3 fatty acid therapies. PT. 2013;38(11):681–91.
Nordestgaard BG, Varbo A. Triglycerides and cardiovascular disease. Lancet. 2014;384(9943):626–35.
Saito Y, Yokoyama M, Origasa H, et al. Effects of EPA on coronary artery disease in hypercholesterolemic patients with multiple risk factors: sub-analysis of primary prevention cases from the Japan EPA Lipid Intervention Study (JELIS). Atherosclerosis. 2008;200(1):135–40.
Guyton JR, Slee AE, Anderson T, et al. Relationship of lipoproteins to cardiovascular events: the AIM-HIGH trial (Atherothrombosis intervention in metabolic syndrome with low HDL/high triglycerides and impact on global health outcomes). J Am Coll Cardiol. 2013;62(17):1580–4.
The HPS2-THRIVE Collaborative Group. Effects of extended-release niacin with laropiprant in high-risk patients. N Engl J Med. 2014;371(3):203–12.
Mozaffarian D, Wu JH. (n-3) fatty acids and cardiovascular health: are effects of EPA and DHA shared or complementary? J Nutr. 2012;142(3):614S–25S.
Bays HE, Ballantyne CM, Kastelein JJ, et al. Eicosapentaenoic acid ethyl ester (AMR101) therapy in patients with very high triglyceride levels (from the Multi-center, plAcebo-controlled, Randomized, double-blINd, 12-week study with an open-label Extension [MARINE] trial). Am J Cardiol. 2011;108(5):682–90.
US FDA. Vascepa (icosapent ethyl) capsules: US prescribing information. 2013. http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/202057s009lbl.pdf. Accessed 14 Nov 2014.
Braeckman RA, Stirtan WG, Soni PN. Phase 1 study of the effect of icosapent ethyl on warfarin pharmacokinetic and anticoagulation parameters. Clin Drug Investig. 2014;34(7):449–56.
Rustan AC, Nossen JØ, Christiansen EN, et al. Eicosapentaenoic acid reduces hepatic synthesis and secretion of triacylglycerol by decreasing the activity of acyl-coenzyme A:1,2-diacylglycerol acyltransferase. J Lipid Res. 1988;29(11):1417–26.
Harris WS, Bulchandani D. Why do omega-3 fatty acids lower serum triglycerides? Curr Opin Lipidol. 2006;17(4):387–93.
Ishida T, Ohta M, Nakakuki M, et al. Distinct regulation of plasma LDL cholesterol by eicosapentaenoic acid and docosahexaenoic acid in high fat diet-fed hamsters: participation of cholesterol ester transfer protein and LDL receptor. Prostaglandins Leukot Essent Fatty Acids. 2013;88(4):281–8.
Bays HE, Braeckman RA, Ballantyne CM, et al. Icosapent ethyl, a pure EPA omega-3 fatty acid: effects on lipoprotein particle concentration and size in patients with very high triglyceride levels (the MARINE study). J Clin Lipidol. 2012;6(6):565–72.
Ballantyne CM, Bays H, Braeckman R, et al. Icosapent ethyl (eicosapentaenoic acid ethyl ester): effects on remnant-like particle cholesterol from the MARINE and ANCHOR studies [abstract no. 16803 plus poster]. In: AHA Scientific Sessions; 2014; Chicago, IL.
Braeckman RA, Manku MS, Bays HE, et al. Icosapent ethyl, a pure EPA omega-3 fatty acid: effects on plasma and red blood cell fatty acids in patients with very high triglyceride levels (results from the MARINE study). Prostaglandins Leukot Essent Fatty Acids. 2013;89(4):195–201.
Braeckman RA, Bays HE, Ballantyne CM, et al. Pharmacokinetic and triglyceride-lowering pharmacodynamic effects of icosapent ethyl (eicosapentaenoic acid ethyl ester) across clinical studies [abstract no. 19343 (plus poster 2016)]. In: 86th Annual Scientific Sessions of the American Heart Association; Nov 19 2013; Dallas, TX.
Weintraub HS. Overview of prescription omega-3 fatty acid products for hypertriglyceridemia. Postgrad Med. 2014;126(7):7–18.
Bays HE, Ballantyne CM, Braeckman RA, et al. Icosapent ethyl, a pure ethyl ester of eicosapentaenoic acid: effects on circulating markers of inflammation from the MARINE and ANCHOR studies. Am J Cardiovasc Drugs. 2013;13(1):37–46.
Ballantyne CM, Bays HE, Braeckman RA, et al. Icosapent ethyl (eicosapentaenoic acid ethyl ester): effects on apolipoprotein C-III in patients from the MARINE and ANCHOR studies [abstract no. 122 plus poster]. J Clin Lipidol. 2014;8(3):313–4.
Braeckman RA, Stirtan WG, Soni PN. Pharmacokinetics of eicosapentaenoic acid in plasma and red blood cells after multiple oral dosing with icosapent ethyl in healthy subjects. CPDD. 2014;3(2):101–8.
Arnold C, Konkel A, Fischer R, et al. Cytochrome P450-dependent metabolism of omega-6 and omega-3 long-chain polyunsaturated fatty acids. Pharmacol Rep. 2010;62(3):536–47.
Braeckman R, Soni P, Stirtan W. Phase 1 study of the effect of icosapent ethyl on atorvastatin pharmacokinetics in healthy subjects [abstract no. 156]. J Clin Lipidol. 2013;7(3):269–70.
Braeckman R, Stirtan W, Soni P. Effects of icosapent ethyl (eicosapentaenoic acid ethyl ester) on pharmacokinetic parameters of rosiglitazone in healthy subjects [abstract no. T-755-P]. In: Annual Obesity Week meeting; Nov 11–16 2013, Atlanta, GA.
Braeckman RA, Stirtan WG, Soni PN. Effect of icosapent ethyl (eicosapentaenoic acid ethyl ester) on omeprazole plasma pharmacokinetics in healthy adults. Drugs RD. 2014;14(3):159–64.
Ballantyne CM, Bays HE, Kastelein JJ, et al. Efficacy and safety of eicosapentaenoic acid ethyl ester (AMR101) therapy in statin-treated patients with persistent high triglycerides (from the ANCHOR study). Am J Cardiol. 2012;110(7):984–92.
US FDA. Lovaza (omega-3-acid ethyl esters) capsules: US prescribing information. 2014. http://www.accessdata.fda.gov/drugsatfda_docs/label/2014/021654s041lbl.pdf. Accessed 14 Nov 2014.
US FDA. Epanova (omega-3-carboxylic acids) capsules: US prescribing information. 2014. http://www.accessdata.fda.gov/drugsatfda_docs/label/2014/205060s000lbl.pdf. Accessed 14 Nov 2014.
US FDA. Omtryg (omega-3-acid ethyl esters A) capsules: US prescribing information. 2014. http://www.accessdata.fda.gov/drugsatfda_docs/label/2014/204977s000lbl.pdf. Accessed 14 Nov 2014.
US National Library of Medicine. Omega-3-acid ethyl esters capsules: US prescribing information. 2014. http://dailymed.nlm.nih.gov/dailymed/getFile.cfm?setid=2423ae12-e70e-40db-bf9b-b7597a911413&type=pdf&name=2423ae12-e70e-40db-bf9b-b7597a911413. Accessed 14 Nov 2014.
Amarin Pharma Inc. A study of AMR101 to evaluate its ability to reduce cardiovascular events in high risk patients with hypertriglyceridemia and on statin. The primary objective is to evaluate the effect of 4 g/day AMR101 for preventing the occurrence of a first major cardiovascular event (REDUCE-IT) [ClinicalTrials.gov Identifier NCT01492361] US National Institutes of Health, ClinicalTrials.gov. 2013. http://clinicaltrials.gov/ct2/show/NCT01492361. Accessed 16 July 2014.
Amarin Corporation. Amarin reaffirms its mission to improve patient care with commitment to completing REDUCE-IT cardiovascular outcomes study. 2014. http://investor.amarincorp.com/releasedetail.cfm?ReleaseID=870953. Accessed 22 Sept 2014.
Disclosure
The preparation of this review was not supported by any external funding. During the peer review process, the manufacturer of the agent under review was offered an opportunity to comment on this article. Changes resulting from comments received were made by the authors on the basis of scientific and editorial merit. Esther S. Kim and Paul L. McCormack are salaried employees of Adis/Springer.
Author information
Authors and Affiliations
Corresponding author
Additional information
The manuscript was reviewed by: J. C. Bradberry, School of Pharmacy and Health Professions, Creighton University, Omaha, NE, USA; D. C. F. Chan, Medicine and Pharmacology RPH Unit, The University of Western Australia, Crawley, WA, Australia; A. Sethi, Department of Medicine, Rosalind Franklin University of Medicine and Sciences, North Chicago, IL, USA.
Rights and permissions
About this article
Cite this article
Kim, E.S., McCormack, P.L. Icosapent Ethyl: A Review of Its Use in Severe Hypertriglyceridemia. Am J Cardiovasc Drugs 14, 471–478 (2014). https://doi.org/10.1007/s40256-014-0099-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-014-0099-7