Abstract
Objectives
Research is lacking on the impacts of exposure to particulate matter (PM) and air pollution on patients with chronic obstructive pulmonary disease (COPD) or asthma. Therefore, we investigate the effects of various air pollution factors on hospitalization for asthma and COPD.
Methods
We obtained data on pollutants—PM10, PM2.5, carbon monoxide (CO), ozone (O3), nitrogen dioxide (NO2), and sulfur dioxide (SO2)—in Gyeonggi-do, South Korea. We also extracted data from Korean National Health Insurance records and investigated asthma and COPD attacks that required hospitalization from January 2007 through February 2018. We used generalized additive models with Poisson distribution and log transformation to calculate adjusted risk. A time-stratified case-crossover design was used, and conditional logistic regression was performed to analyze these data.
Results
Per-unit increases in concentrations of PM10, PM2.5, SO2, NO2, CO, and O3 on different best lag days were associated with increased risks for hospital admission for COPD and asthma. SO2 had the strongest effect on hospital admission for asthma (odds ratio [OR], 1.535; 95 % confidence interval [CI], 1.450–1.619). SO2 also had the strongest effect on hospital admission for COPD (OR, 1.659; 95 % CI, 1.541–1.786). Subgroup analyses showed that these relationships were stronger in seniors (≥ 65 years old) and women with asthma than in men and nonseniors with COPD.
Conclusions
Short-term exposure to PM10, PM2.5, CO, O3, NO2, and SO2 may result in hospitalization for asthma and COPD. Of these pollutants, SO2 has the strongest effects. Therefore, patients with COPD and asthma should be cautioned against performing outdoor activities when SO2 levels are high.
Similar content being viewed by others

Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In many epidemiological studies, negative health effects of air pollution have been observed [1, 2]. In 2010, surrounding particulate matter (PM) pollution has resulted in approximately 3.1 million deaths worldwide [3]. In Asia, air pollution has increased for decades with rapid industrialization and urbanization, and Asian cities are one of the most polluted cities in the world. Thus, ambient air pollution has become a major health concern for the general population.
Short-term effects of air pollution increase the risk of hospitalization, including admission for stroke [4], congestive heart failure [5], pneumonia and chronic obstructive pulmonary disease (COPD) [6], and other cardiovascular and respiratory diseases [7]. However, studies on the relationship between air pollution and morbidity are limited in Asia. Because of the lack of local studies, studies from other regions have been used to estimate the health effects of air pollution in Asia. However, the characteristics of air pollution and the characteristics of other areas vary from place to place and need to be investigated in other areas. South Korea, like many Asian countries, is experiencing rapid economic development with increased industrialization and increased air pollution.
Asthma and COPD are common respiratory diseases in increasing worldwide. Air pollution can have a detrimental effect on patients with lung diseases such as COPD [6, 7]. Recent studies in South Korea have shown that concentrations of air pollution are associated with asthma [8,9,10], acute bronchitis, and acute rhinitis hospitalizations [11]. However, most air pollution studies in South Korea have investigated on asthma or cardiovascular disease [12,13,14], and there was no study have been investigated the effects of air pollution on patients with both asthma and COPD. Updated information on air pollution effect on patients with asthma and COPD is pivotal to urging health care professionals and policymakers to take effective actions to alleviate these adverse effects in South Korea. Therefore, we extracted data from Korean National Health Insurance records and assessed the effects of ambient air pollutants on hospital admissions for asthma and COPD in Gyeonggi-do, South Korea, from January 2007 through February 2018.
Methods
Environmental monitoring data on air pollutants were investifated hourly at each of the monitoring stations. Concentrations of PM10, PM2.5, carbon monoxide (CO), ozone (O3), nitrogen dioxide (NO2), and sulfur dioxide (SO2) are indicators of air quality in South Korea, and data on these pollutants were collected from January 1, 2007, through December 31, 2018. Air pollutions datas from monitoring stations in the main urban area of Gyeonggi-do, South Korea, were collected from reports published by the Institute of Health and Environment. Hourly data were used to calculate 24 h mean values (except for O3, for which the 8 h maximum value was calculated). Meteorological and hourly data on 24 h mean temperature (°C), humidity (%), and atmospheric pressure (hPa) at sea level were obtained from the Korea Meteorological Administration.
We obtained data from January 2007 through February 2018 from the National Health Information Database (NHIS-2019-1-270) of the National Health Insurance Service (NHIS). Study patients were selected from those who were hospitalized with asthma or COPD. We corrected monthly separation claim data by applying the medical treatment attributed to the nature of the claim. Analyses were conducted according to the age and sex of each patient. In subgroup analyses, patients with asthma were classified as preschoolers (0–5 years old), adolescents (6–17 years), adults (18–64 years), or seniors (≥ 65 years). Patients with COPD were classified as adults or seniors.
We used a time-stratified case-crossover design [15] to evluate the acute effects of daily ambient air pollution levels on asthma or COPD hospitalizations. This case-crossover study design required exposure data for only cases, as it was a special type of case-control study in which each case served as its own control. This design is used in environmental epidemiologic research, and one advantage of it is that confounding effects due to individual characteristics that do not vary by age, sex, physical condition, and time are removed.
Data analyses
The relationships between asthma or COPD hospitalizations and concentrations of outdoor air pollutants (PM10, PM2.5, SO2, NO2, O3, and CO) on current and lag days were examined with a time-stratified, case-crossover, generalized additive model [16]. The effects of PM10, PM2.5, SO2, NO2, O3, and CO on asthma or COPD hospitalizations were analyzed for single-lag days and multi-lag days, respectively [17]. The effect of the concentration of each pollutant was included in the single-day models for only that specific day (lag 0, lag 1, lag 2, etc.). In the multi-lag day models, we investigated the combined effect of multiple days (e.g., from lag 0 to lag 7) by including the concentrations of each pollutant.
Lag time 0 (i.e., lag 0) was defined as same-day exposure to PM10, PM2.5, SO2, NO2, O3, or CO. For example, lag 0 means that the effect of the pollutant was observed on the current day, lag 1 means that the effect was observed on the previous day, and lag 7 means that the effect was observed 7 days prior. Lags between consecutive days were calculated as intervals. This was done because conventional research indicates that adequate time is needed for air pollution to affect health. In addition to exposure data for the air pollutants, a statistical model were adjusted to include data for mean temperature, humidity, and atmospheric pressure at sea level.
In all models, relative risk was estimated on the basis of an increase of 1 unit of the air pollutant, with correction for temperature, relative humidity, and atmospheric pressure at sea level. P < 0.05 was considered statistically significant. All data were analyzed with R version 3.6.3 (R Foundation for Statistical Computing, http://cran.r-project.org).
Results
Table 1 showed general characteristics of asthma (n = 290,464) and COPD (n = 85,301) exacerbations hospitalizations due to air pollutants. The 24 h mean concentrations of PM10, PM2.5, SO2, NO2, and CO as well as the 8 h mean concentration of O3 are shown in Table 2. The daily mean concentrations of PM10, PM2.5, SO2, NO2, O3, and CO were 54.32 ± 29.89 µg/m3, 26.32 ± 14.41 µg/m3, 50.71 ± 20.43 ppb, 283.90 ± 105.14 ppb, 229.90 ± 112.62 ppb, and 57.29 ± 20.98 (100ppb), respectively. Table 3 shows correlations between air pollutants and meteorological variables. PM10 and PM2.5 were strongly correlated (r = 0.776, P < 0.01).
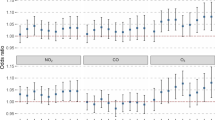
Table 4 summarizes the results of the single-pollutant model for hospital admission due to asthma after we controlled for meteorological variables. Per-unit increases in concentrations of PM10, PM2.5, SO2, NO2, CO, and O3 were associated with increased risk for hospital admission for asthma on different best lag days. These per-unit increases in PM10 were significantly positively associated with hospital admission for asthma on lag 2, lag 3, lag 5, lag 6, lag 7, lag 0–5, lag 0–6, and lag 0–7. Per-unit increases in PM2.5 were significantly positively associated with hospital admission for asthma on lag 1, lag 2, lag 3, lag 6, lag 7, lag 0–1, lag 0–2, lag 0–3, lag 0–4, lag 0–5, lag 0–6, and lag 0–7. Per-unit increases in SO2 were significantly positively associated with hospital admission for asthma on lag 1, lag 2, lag 3, lag 4, lag 0–2, lag 0–3, lag 0–4, lag 0–5, and lag 0–6. Per-unit increases in NO2 were significantly positively associated with hospital admission for asthma on lag 3, lag 4, and lag 5. Per-unit increases in O3 were significantly positively associated with hospital admission for asthma on lag 1, lag 2, lag 6, lag 7, lag 0–1, and lag 0–2. Per-unit increases in CO were significantly positively associated with hospital admission for asthma on lag 3, lag 4, lag 5, and lag 0–5. SO2 had the strongest effect on hospital admission for asthma (OR, 1.535; 95 % CI, 1.450–1.619). Lag 0–4 was determined to be the best lag for SO2, followed by effect estimates for PM2.5 on lag 0–7, PM10 on lag 2, O3 on lag 1, NO2 on lag 4, and CO on lag 3.
Table 5 summarizes the results of the single-pollutant model for hospital admission due to COPD after we controlled for meteorological variables. Per-unit increases in concentrations of PM10, PM2.5, SO2, NO2, CO, and O3 were associated with increased risk for hospital admission for COPD on different best lag days. Per-unit increases in PM10 were significantly positively associated with hospital admission for COPD on lag 2, lag 3, lag 5, lag 6, and lag 7. Per-unit increases in PM2.5 were significantly positively associated with hospital admission for COPD on lag 1, lag 2, lag 3, lag 6, lag 7, lag 0–1, lag 0–2, lag 0–3, lag 0–4, lag 0–5, lag 0–6, and lag 0–7. Per-unit increases in SO2 were significantly positively associated with hospital admission for COPD on lag 2, lag 3, lag 4, lag 0–2, lag 0–3, lag 0–4, and lag 0–5. Per-unit increases in NO2 were significantly positively associated with hospital admission for COPD on lag 3 and lag 5. Per-unit increases in O3 were significantly positively associated with hospital admission for COPD on lag 6 and lag 7. Per-unit increases in CO were significantly positively associated with hospital admission for COPD on lag 3, lag 4, and lag 5. SO2 had the strongest effect on hospital admission for COPD (OR, 1.659; 95 % CI, 1.541–1.786), with lag 0–3 indicated as the best lag, followed by effect estimates for PM2.5 on lag 0–7, O3 on lag 7, NO2 on lag 5, PM10 on lag 6, and CO on lag 3.
The results of the multiple-pollutant models are shown in Tables 6 and 7. SO2 had the highest OR for hospital admission due to asthma (OR, 1.604; 95 % CI, 1.553–1.656) compared to those for NO2, O3, and CO. SO2 also had the highest OR for hospital admission due to COPD (OR, 2.169; 95 % CI, 2.03–2.319) compared to those for O3, NO2, and CO.
The effects of air pollutants on reason for hospitalization, sex, and age are shown in Table 8. The ORs for each per-unit increase in PM10, PM2.5, SO2, NO2, and CO were higher in patients with asthma and women with COPD. Higher effect estimates for exposure to PM10, PM2.5, SO2, NO2, and CO were observed in patients with asthma and seniors with COPD.
Discussion
Our study gives showed that exposure to air pollutants exacerbates the risk for hospitalization for asthma and COPD. The positive correlation between hospitalization for asthma and COPD and concentrations of PM10, PM2.5, SO2, NO2, and CO suggests that increases in concentrations of these pollutants may increase the number of hospitalizations due to asthma and COPD. Our subgroup analyses of sex- and age-specific effects on the association between exposure to air pollutants and risk for hospitalization showed that women and seniors had more hospitalizations than men and non-seniors.
Our study findings are similar to the findings of other studies [18, 19]. In our study, six pollutants (PM10, PM2.5, SO2, NO2, O3, and CO) were associated with asthma or COPD hospitalization, and SO2 had stronger associations with hospitalization due to asthma or COPD as its concentration increased. The main anthropogenic sources of PM are transportation, power generation, and other combustion processes [16]. The main sources of SO2 in the developed countries are primary emissions from energy production and industrial processes [17], and NO2 and CO are mainly emitted from fossil fuel combustion in urban environments [20]. O3 is a secondary pollutant formed by a photochemical reaction between sunlight and precursors of pollutants such as nitrogen oxides and volatile organic compounds [21].
Many studies have showed that air pollution from O3, SO2, NO2, and PM may asthma exacerbation [22]. Air pollution may be associated with exacerbation of asthma via oxidative stress, airway remodeling and inflammation, and sensitization to aeroallergens [21, 23]. Specifically, exposure to O3 causes airway inflammation, airway hyperresponsiveness, and decreased lung function, whereas SO2 mainly leads to bronchoconstriction [24]. NO2, as a precursor of O3, likely triggers bronchial inflammation [25]. However, exposure to PM, alone or in combination with allergic sensitization, can cause oxidative stress, airway hyperresponsiveness, and airway remodeling [15].
Different sizes of PM are found in the atmosphere. The coarse fraction (PM2.5–10) can penetrate the airways, but the fine fraction (PM1–2.5) may deposit in the lungs, in particular in the alveoli, and may pass into systemic circulation [22]. Besides the size of the PM, its chemical composition is very important to understanding health effects. There are also differences in individuals’ susceptibility to air pollutants. According to a number of meta-analyses [24, 26, 27], air pollutants are associated with increased incidence and prevalence of asthma, as well as increased asthma hospitalization and worsening of asthma symptoms.
Regarding the short-term effects of air pollutants, three studies have found an association between PM, NO2, SO2, CO, and O3 and exacerbation or worsening of symptoms [28, 29].
A proposed mechanism by which air pollutants affect respiratory health is the production of large amounts of reactive oxygen species in the respiratory tract by exogenous oxidants. These oxygen species can cause epithelial damage and cause the inflammatory processes involved in asthma and COPD attacks. In addition to these direct effects on people with asthma and COPD, air pollutants interactively regulate the bioavailability of allergens in the air and therefore people with allergic asthma to outdoor allergens.
A recent meta-analysis showed that exposure to air pollutions were associated with increased COPD or asthma hospitalizations in East Asia [29]. The statistically significant risk for hospital utilization and general hospital admission for COPD associated with air pollutants ranged from 1.007 (for patients of all ages exposed to SO2) to 1.028 (for patients of all ages exposed to O3), and the risk for emergency room admission for COPD ranged from 1.011 (for patients of all ages exposed to SO2) to 1.028 (for patients of all ages exposed to O3). The majority of the summary estimates of risk for hospitalization due to COPD ranked O3 as having the highest risk, followed by PM2.5, NO2, PM10, and SO2.
For patients with asthma, the significant risk for hospital utilization ranged from 1.013 (for patients of all ages exposed to PM10) to 1.141 (for children exposed to CO). For general hospital admission, risk ranged from 1.010 (for patients of all ages exposed to PM10) to 1.141 (for children exposed to CO); for emergency room admission, risk ranged from 1.009 (for patients of all ages exposed to SO2) to 1.040 (for children exposed to NO2). Pooled estimates, which were not statistically significant, were mainly for emergency room admission due to asthma for patients ages 15–64 years.
The Air Pollution and Health: A European Approach (APHEA) project found that daily emergency room admission for COPD was significantly positively associated with NO2 and O3 in the whole population and that daily emergency room admission for asthma was significantly positively associated with NO2 in children [29]. Regarding emergency room admission for asthma among patients ages 15–64 years, the results for SO2 and O3 are consistent with those of APHEA, but these associations have since been determined to be statistically nonsignificant in both studies (36). However, according to APHEA, the risks for hospitalization due to NO2 and PM10 were 1.007 (95 % CI, 1.002–1.013) and 1.011 (95 % CI, 1.003–1.018), respectively [30]. Another multi-city study conducted in 14 U.S. cities (The National Morbidity, Mortality, and Air Pollution Study) reported an increase in hospital admission for COPD of 1.98 % (95 % CI, 1.49–2.47 %) in an elderly population [25].
Our study strengths were include the use of a time-stratified case-crossover design, which could minimize the effects of long-term seasonal trends, and the use of serial autocorrelation of the data to allow full adjustment for multiple variables confoundings. We adjusted for the possible effects of seasonal and long-term trends in air pollutant levels and for hospitalization due to asthma or COPD. We collected data to investigate the effects of air pollutants on hospitalization on different lag days. We found an association between air pollutants and hospitalization due to asthma or COPD. Of the pollutants, SO2 was significantly associated with hospitalization for asthma or COPD among persons living in Gyeonggi-do, South Korea. Therefore, patients with COPD and asthma should be cautioned against performing outdoor activities when PM levels (in particular those of SO2) are high.
References
Dominici F, Peng RD, Bell ML, et al. Fine particulate air pollution and hospital admission for cardiovascular and respiratory diseases. JAMA. 2006;295:1127–34.
Künzli N, Kaiser R, Medina S, et al. Public-health impact of outdoor and traffic-related air pollution: a European assessment. Lancet. 2000;356:795–801.
Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–60.
Oudin A, Strömberg U, Jakobsson K, et al. Estimation of short-term effects of air pollution on stroke hospital admissions in southern Sweden. Neuroepidemiology. 2010;34:131–42.
Wellenius GA, Schwartz J, Mittleman MA. Particulate air pollution and hospital admissions for congestive heart failure in seven United States cities. Am J Cardiol. 2006;97:404–8.
Ni L, Chuang CC, Zuo L. Fine particulate matter in acute exacerbation of COPD. Front Physiol. 2015;6:294.
Jo YS, Lim MN, Han YJ, et al. Epidemiological study of PM(2.5) and risk of COPD-related hospital visits in association with particle constituents in Chuncheon, Korea. Int J Chron Obstruct Pulmon Dis. 2018;13:299–307.
Lee JT, Son JY, Cho YS. Benefits of mitigated ambient air quality due to transportation control on childhood asthma hospitalization during the 2002 summer Asian games in Busan, Korea. J Air Waste Manag Assoc. 2007;57:968–73.
Lee JT, Kim H, Song H, et al. Air pollution and asthma among children in Seoul Korea. Epidemiology. 2002;13:481–4.
Kim SY, O’Neill MS, Lee JT, et al. Air pollution, socioeconomic position, and emergency hospital visits for asthma in Seoul, Korea. Int Arch Occup Environ Health. 2007;80:701–10.
Jo EJ, Lee WS, Jo HY, et al. Effects of particulate matter on respiratory disease and the impact of meteorological factors in Busan, Korea. Respir Med. 2017;124:79–87.
Lee JT, Kim H, Cho YS, et al. Air pollution and hospital admissions for ischemic heart diseases among individuals 64 + years of age residing in Seoul, Korea. Arch Environ Health. 2003;58:617–23.
Park JW, Lim YH, Kyung SY, et al. Effects of ambient particulate matter on peak expiratory flow rates and respiratory symptoms of asthmatics during Asian dust periods in Korea. Respirology. 2005;10:470–6.
Hwang SH, Lee JY, Yi SM, et al. Associations of particulate matter and its components with emergency room visits for cardiovascular and respiratory diseases. PLoS One. 2017;12:e0183224.
Stanek LW, Brown JS, Stanek J, et al. Air pollution toxicology–a brief review of the role of the science in shaping the current understanding of air pollution health risks. Toxicol Sci. 2011;120(Suppl 1):8–27.
Falcon-Rodriguez CI, Osornio-Vargas AR, Sada-Ovalle I, et al. Aeroparticles, composition, and lung diseases. Front Immunol. 2016;7:3.
Guarnieri M, Balmes JR. Outdoor air pollution and asthma. Lancet. 2014;383:1581–92.
Amâncio CT, Nascimento LF. Asthma and ambient pollutants: a time series study. Rev Assoc Med Bras (1992) 2012;58:302-7.
Park M, Luo S, Kwon J, et al. Effects of air pollution on asthma hospitalization rates in different age groups in metropolitan cities of Korea. Air Qual Atmos Health. 2013;6:559–65.
Masiol M, Agostinelli C, Formenton G, et al. Thirteen years of air pollution hourly monitoring in a large city: potential sources, trends, cycles and effects of car-free days. Sci Total Environ. 2014;494–495:84–96.
Auerbach A, Hernandez ML. The effect of environmental oxidative stress on airway inflammation. Curr Opin Allergy Clin Immunol. 2012;12:133–9.
Brugha R, Grigg J. Urban air pollution and respiratory infections. Paediatr Respir Rev. 2014;15:194–9.
Esposito S, Tenconi R, Lelii M, et al. Possible molecular mechanisms linking air pollution and asthma in children. BMC Pulm Med. 2014;14:31.
Bowatte G, Lodge C, Lowe AJ, et al. The influence of childhood traffic-related air pollution exposure on asthma, allergy and sensitization: a systematic review and a meta-analysis of birth cohort studies. Allergy. 2015;70:245–56.
Samet JM, Zeger SL, Dominici F, et al. The national morbidity, mortality, and air pollution study. Part II: Morbidity and mortality from air pollution in the United States. Res Rep Health Eff Inst. 2000;94:5–70 discussion 1–9.
Gasana J, Dillikar D, Mendy A, et al. Motor vehicle air pollution and asthma in children: a meta-analysis. Environ Res. 2012;117:36–45.
Barone-Adesi F, Dent JE, Dajnak D, et al. Long-term exposure to primary traffic pollutants and lung function in children: cross-sectional study and meta-analysis. PLoS One. 2015;10:e0142565.
Zheng XY, Ding H, Jiang LN, et al. Association between air pollutants and asthma emergency room visits and hospital admissions in time series studies: a systematic review and meta-analysis. PLoS One. 2015;10:e0138146.
Zhang S, Li G, Tian L, et al. Short-term exposure to air pollution and morbidity of COPD and asthma in East Asian area: A systematic review and meta-analysis. Environ Res. 2016;148:15–23.
Sunyer J, Spix C, Quénel P, et al. Urban air pollution and emergency admissions for asthma in four European cities: the APHEA Project. Thorax. 1997;52:760–5.
Author information
Authors and Affiliations
Contributions
All authors contributed conception, analysis, interpretation, revising, and final approval of the manuscript. CH Han served as a principal investigator and had full access to all of the data in the study. JH Chung take responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflict of interest
This work was supported by the National Health Insurance Ilsan Hospital grant (NHIMC-2019-11-019).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Chang Hoon Han and Haeyong Pak contributed equally to this work as co-first authors.
Rights and permissions
About this article
Cite this article
Han, C.H., Pak, H. & Chung, J.H. Short-term effects of exposure to particulate matter and air pollution on hospital admissions for asthma and chronic obstructive pulmonary disease in Gyeonggi-do, South Korea, 2007–2018. J Environ Health Sci Engineer 19, 1535–1541 (2021). https://doi.org/10.1007/s40201-021-00709-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40201-021-00709-7