Abstract
Background
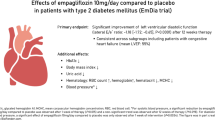
Sodium glucose co-transporter2 (SGLT2) inhibitors have exhibited cardioprotective properties in diabetes patients. The aim of this study was to investigate the effect of Empagliflozin on changes in echocardiographic parameters.
Methods
This was a post hoc analysis of the EMPA-CARD trial which was a multicenter, triple-blind randomized controlled trial. Type 2 diabetes mellitus patients with concomitant history of coronary artery disease were randomized on a 1:1 ratio into two groups receiving either 10 mg/day Empagliflozin or placebo. Patients with a history of heart failure (NYHA class 3–4) and ejection fraction (EF) < 40% were excluded. Trans-thoracic echocardiography was performed at baseline and at 26 weeks of intervention.
Results
A total of 69 (Empagliflozin = 39 and placebo = 30) patients underwent echocardiography. Significant changes were observed for left ventricular ejection fraction [standard error (SE) = 0.76; beta (95% correlation interval (CrI)] = -5.558 (-7.25; -4.18) and left ventricular end-systolic volume (SE = 1.38; beta (95% CrI) = 3.915 (1.2; 0.66). Other echocardiographic parameters relating to right ventricular or atrial function did not change significantly.
Conclusion
Empagliflozin can have cardioprotective benefits in subjects without HF. Further studies are required to determine the effect of Empagliflozin in non-HF patients.
Trial registration
The original EMPA-CARD study has been registered in Iranian Registry of Clinical Trials. www.IRCT.ir, Identifier: IRCT20190412043247N2. Registration Date: 6/13/2020. Registration timing: prospective.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with diabetes have an elevated risk of developing heart failure (HF), coupled with an increased likelihood of HF-related mortality and hospitalization [1]. Sodium glucose co-transporter 2 (SGLT2) inhibitor, recognized as antihyperglycemic agents, exhibit substantial cardioprotective properties beyond merely reducing glycemic levels [2]. Notably, in various large-scale trials, empagliflozin, a specific SGLT2 inhibitor, has consistently demonstrated a capacity to alleviate left ventricular (LV) remodeling in HF [3, 4] and has shown to improve cardiomyocyte stiffness as well [5]. Patients with acute coronary syndrome (ACS) are more predisposed to neurohormonal activation and LV remodeling, therefore there is a greater burden of HF after myocardial infarction (MI) [6].
While the EMPA-CARD trial has unraveled the cardiovascular benefits of empagliflozin, highlighting reductions in oxidative stress and pro-inflammatory responses, the precise mechanisms underlying these advantages have been explored. To investigate whether these molecular alterations translate into changes in echocardiographic parameters, we have conducted this post hoc study to assess the effect of empagliflozin on cardiac performance.
Methods
Study design and population
This study constitutes a post hoc analysis derived from the EMPA-CARD trial [7], with a fully disclosed study protocol [8]. Conducted between 2020 and 2021 in Zanjan, Iran, this multicenter, double-blind, randomized placebo-controlled trial (RCT) explored the impacts of empagliflozin (10 mg/day) versus placebo in individuals with both Type 2 Diabetes (T2DM) and confirmed Coronary Artery Disease (CAD) across four clinical centers. Ethical approval from the Zanjan University of Medical Sciences Ethics Committee was obtained, and the trial was prospectively registered at the Iranian Registry of Clinical Trials (www.IRCT.ir; Identifier: IRCT20190412043247N2). Informed consent was secured from eligible patients meeting inclusion criteria, including T2DM, documented CAD through angiography, age between 40 and 75 years, serum HbA1c levels of 6.5 to 9.5%, and a history of standard oral anti-diabetic/anti-ischemic medication use for the past three months. CAD diagnosis required evidence of at least one vessel with ≥ 50% stenosis in coronary angiographies. Exclusion criteria comprised various factors such as pregnancy, SGLT2-inhibitor allergies, BMI exceeding 40 kg/m2, heart failure (NYHA class 3–4), EF < 40%, and recent cardiovascular events or interventions. Eligible patients underwent interviews and a randomization process, with stratification based on gender, age, and HbA1c. The allocation into study arms utilized block stratified randomization generated by Winpepi software (version 11.6) and concealed through sealed envelopes. Throughout the study duration, healthcare providers, recruited patients, and researchers remained blinded to the assigned treatment.
Intervention procedures
Baseline characteristics were gathered through interviews, and patients were randomly assigned to receive either a placebo or 10 mg/day empagliflozin (Dr. Abidi Co, Iran) for 26 weeks, in addition to their prescribed antidiabetic drugs. A single cardiologist conducted trans-thoracic echocardiography (Vivid S6, GE, Germany) before and after the 26-week Empagliflozin treatment.
The primary outcomes were defined as changes in echocardiography parameters in the intervention group compared to the placebo after 26 weeks of Empagliflozin.
Statistical considerations
Given the post-hoc nature of the analysis, the sample size was not pre-determined. However, echocardiographic parameter changes were outlined as a sub-study exploratory outcome in the published study protocol [8]. Results, expressed as mean ± standard deviation (SD) for quantitative variables, were analyzed using the per-protocol method. Bayesian regression models, particularly mixed-effects models, were applied to account for baseline differences. The R3.4.1 environment, along with the Rstan and ggplot packages, was used for statistical analysis. An association was considered significant if the 95% credible interval (CrI) did not include zero.
Results
In this current analysis from the 95 recruited patients in the trial, the transthoracic echocardiography data of a total of 69 patients were available. The overall average age was 63.44 and 44.15% were men. The empagliflozin group consisted of 39 patients with an average age of 64.22 ± 6.69 years and the placebo arm had 30 participants whose mean age was 62 ± 9.06 years. The baseline echocardiography parameters of both groups are in Table 1.
By adjusting the parameters to their baseline value in each arm via Bayesian regression model, the change in EF was significant for patients receiving Empagliflozin [SE = 0.76; beta (95% CrI) = -5.558 (-7.25; -4.18)]. Additionally, according to this model, when using the mixed-effect model, LVESV in Empagliflozin group decreased significantly [(SE = 1.38; beta (95% CrI) = 3.915 (1.2; 0.66)]. Other echocardiographic variables did not change significantly. Changes in echocardiographic variables in Empagliflozin arm compared to placebo with the regression model are shown in Table 2.
Discussion
In this post hoc study, patients treated with empagliflozin exhibited a notable increase in EF and decrease in LVESV after a 26-week duration. Considering that increased LVESV is regarded as predictor of new-onset heart failure in HF patients with preserved EF, the results of our study suggest that Empagliflozin can improve cardiac function in subjects with T2DM and CAD. This aligns with the results of EMMY-trial, which demonstrated echocardiographic and structural benefits of empagliflozin in patients with acute MI and T2DM [9]. Similarly, the SUGAR-DM-HF trial illustrated positive effects on LV volume parameters in diabetic or prediabetic individuals with heart failure with reduced EF (HFrEF) [10]. The sub-study of the EMPIRE HF trial also reported modest reductions in LV volumes. Although, unlike our study, the two latter trials investigated the effect of Empagliflozin on HF patients [11]..
However, we have observed no significant changes in other echocardiographic parameters. Similar to our findings, the sub-study of the EMPA-HEART trial on patients with diabetes have observed no significant changes in LV diastolic parameters despite reduced LV mass index [12]. Moreover, the study of Rau et al. in Germany has found the same results among patients with T2DM [13]. However, no between-group difference was seen in the changes for LV global longitudinal strain and LVEF in an observational study [14]. Additionally, we did not document significant improvements in echocardiographic parameters related to RV function. Likewise, in the study of Sarak et al.. 6 months treatment with empagliflozin had no impact on RV volumes [15].
A meta-analysis suggests that echocardiographic improvements related to LV function primarily observed in the HF population [16]. This attenuative effect on LV functional capacity was even observed in non-diabetic patients with HF with reduced EF (HFrEF) independent of their glycemic status [3]. This pronounces the dominant beneficial effect of empagliflozin on patients with HFrEF. These data suggest that the ameliorated risk of cardiovascular events of SGLT2 inhibitors in CANVAS [17] and EMPA-REG OUTCOME [18] trials may not be subsequent to the changes in echocardiographic parameters. Moreover, the findings of Verma et al. were indicative that reverse LV remodeling with regressed LV mass can be the logic behind the reduction in HF hospitalization in these studies [19]. The favorable role of SGLT2 inhibitors in HF is believed to be subsequent to both the osmotic diuresis and load independent effect of these drugs [20]. This bolsters the hypothesis that the effect of SGLT2 inhibitors on cardiac function corresponds to the degree and presence of HF. As this study included diabetic patients with normal EF and no history of HF, our results can propose the ameliorating effect of LV remodeling with Empagliflozin even in cases with normal or near normal EF. Inhibition of ventricular remodeling can reduce readmission rate and mortality in diabetes [21].
This study has several strengths. The randomized design of the EMPA-CARD trial, based on HbA1C and age, enhances the accuracy of our sub-study results. Additionally, this study comprehensively assessed nearly all systolic and diastolic echocardiographic parameters. The analysis was performed by a single echocardiography cardiologist who remained blinded to the assigned patient groups throughout.
Despite these strengths, certain limitations are acknowledged. The study lacked a specific sample-size estimation, as it was conducted as a post hoc exploratory analysis. Moreover, EMPA-CARD was not primarily designed to investigate cardiac functional parameters, potentially rendering the study underpowered to detect changes on echocardiography. The use of the per protocol method might have impacted the results.
Conclusion
In conclusion, this post hoc analysis reveals significant changes in LVEF and LVESV after 26 weeks of treatment with 10 mg empagliflozin. The outcomes suggest the potential protective effect of empagliflozin on cardiac function in individuals without heart failure. Further randomized controlled trials are warranted to elucidate the impact of empagliflozin on cardiac hemodynamics in diabetic individuals without heart failure.
Data availability
The data/information supporting this study is available from the corresponding author upon reasonable request.
References
Rosano GM, Vitale C, Seferovic P. Heart failure in patients with diabetes mellitus. Cardiac Fail Rev. 2017;3(1):52.
Novo G, Guarino T, Di Lisi D, Biagioli P, Carluccio E. Effects of SGLT2 inhibitors on cardiac structure and function. Heart Fail Rev. 2022:1–11.
Santos-Gallego CG, Vargas-Delgado AP, Requena-Ibanez JA, Garcia-Ropero A, Mancini D, Pinney S, et al. Randomized trial of empagliflozin in nondiabetic patients with heart failure and reduced ejection fraction. J Am Coll Cardiol. 2021;77(3):243–55.
Santos-Gallego CG, Requena-Ibanez JA, San Antonio R, Garcia-Ropero A, Ishikawa K, Watanabe S, et al. Empagliflozin ameliorates diastolic dysfunction and left ventricular fibrosis/stiffness in nondiabetic heart failure: a multimodality study. Cardiovasc Imaging. 2021;14(2):393–407.
Hsu J-C, Wang C-Y, Su M-YM, Lin L-Y, Yang W-S. Effect of empagliflozin on cardiac function, adiposity, and diffuse fibrosis in patients with type 2 diabetes mellitus. Sci Rep. 2019;9(1):1–9.
Bhatt AS, Ambrosy AP, Velazquez EJ. Adverse remodeling and reverse remodeling after myocardial infarction. Curr Cardiol Rep. 2017;19(8):1–10.
Gohari S, Reshadmanesh T, Khodabandehloo H, Karbalaee-Hasani A, Ahangar H, Arsang-Jang S, et al. The effect of EMPAgliflozin on markers of inflammation in patients with concomitant type 2 diabetes mellitus and coronary ARtery disease: the EMPA-CARD randomized controlled trial. Diabetol Metab Syndr. 2022;14(1):1–13.
Gohari S, Reshadmanesh T, Khodabandehloo H, Fathi M, Ahangar H, Arsang-Jang S, et al. Study rationale and design of a study of EMPAgliflozin’s effects in patients with type 2 diabetes mellitus and coronary ARtery disease: the EMPA-CARD randomized controlled trial. BMC Cardiovasc Disord. 2021;21(1):1–11.
von Lewinski D, Kolesnik E, Tripolt NJ, Pferschy PN, Benedikt M, Wallner M, et al. Empagliflozin in acute myocardial infarction: the EMMY trial. Eur Heart J. 2022;43(41):4421–32.
Lee MM, Brooksbank KJ, Wetherall K, Mangion K, Roditi G, Campbell RT, et al. Effect of empagliflozin on left ventricular volumes in patients with type 2 diabetes, or prediabetes, and heart failure with reduced ejection fraction (SUGAR-DM-HF). Circulation. 2021;143(6):516–25.
Omar M, Jensen J, Ali M, Frederiksen PH, Kistorp C, Videbæk L, et al. Associations of empagliflozin with left ventricular volumes, mass, and function in patients with heart failure and reduced ejection fraction: a substudy of the empire HF randomized clinical trial. JAMA Cardiol. 2021;6(7):836–40.
Bami K, Gandhi S, Leong-Poi H, Yan AT, Ho E, Zahrani M, et al. Effects of empagliflozin on left ventricular remodeling in patients with type 2 diabetes and coronary artery disease: echocardiographic substudy of the EMPA-HEART CardioLink-6 randomized clinical trial. J Am Soc Echocardiogr. 2020;33(5):644–6.
Rau M, Thiele K, Hartmann N-UK, Schuh A, Altiok E, Möllmann J, et al. Empagliflozin does not change cardiac index nor systemic vascular resistance but rapidly improves left ventricular filling pressure in patients with type 2 diabetes: a randomized controlled study. Cardiovasc Diabetol. 2021;20(1):1–12.
Lan NS, Yeap BB, Fegan PG, Green G, Rankin JM, Dwivedi G. Empagliflozin and left ventricular diastolic function following an acute coronary syndrome in patients with type 2 diabetes. Int J Cardiovasc Imaging. 2021;37(2):517–27.
Sarak B, Verma S, David Mazer C, Teoh H, Quan A, Gilbert RE, et al. Impact of empagliflozin on right ventricular parameters and function among patients with type 2 diabetes. Cardiovasc Diabetol. 2021;20(1):1–11.
Yu Y-W, Zhao X-M, Wang Y-H, Zhou Q, Huang Y, Zhai M, et al. Effect of sodium–glucose cotransporter 2 inhibitors on cardiac structure and function in type 2 diabetes mellitus patients with or without chronic heart failure: a meta-analysis. Cardiovasc Diabetol. 2021;20(1):1–17.
Neal B, Perkovic V, Mahaffey KW, De Zeeuw D, Fulcher G, Erondu N, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377(7):644–57.
Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–28.
Verma S, Garg A, Yan AT, Gupta AK, Al-Omran M, Sabongui A, et al. Effect of empagliflozin on left ventricular mass and diastolic function in individuals with diabetes: an important clue to the EMPA-REG OUTCOME trial? Diabetes Care. 2016;39(12):e212–e3.
Connelly KA, Zhang Y, Desjardins J-F, Nghiem L, Visram A, Batchu SN, et al. Load-independent effects of empagliflozin contribute to improved cardiac function in experimental heart failure with reduced ejection fraction. Cardiovasc Diabetol. 2020;19(1):1–11.
Chen Y, Peng D. New insights into the molecular mechanisms of SGLT2 inhibitors on ventricular remodeling. Int Immunopharmacol. 2023;118:110072.
Acknowledgements
We would like to express our thanks to Dr. Ahmad Jalilvand, Dr. Zarei for their consultations. We thank all the patients and collaborators for their patience and cooperation through the study.
Funding
The original EMPA-CARD study received a non-restricted financial grant from Zanjan University of Medical Sciences and a non-restricted non-financial (Medication and placebo) from Dr. Abidi Pharmaceutical Company. The company had no role in the development of the protocol, process of the study, or preparation of this manuscript. The Original EMPA-CARD study was funded by Dr. Abidi Pharmaceutical Company® and Zanjan University of Medical Sciences (Grant Number: 1602001000).
Author information
Authors and Affiliations
Contributions
SAM G: Conceptualization, main investigator, Outcome assessor. SEP G, TR: Study design, Patients follow-up, Conceptualization, Drafting manuscript, Revision. SAJ: Statistical Analysis, data curation. FIB: Supervision, study design, Revision. MM: Manuscript draft, Revision, Conceptualization. HC: Revision. MD and AA: patient follow up. HA: Project Administration, supervision, resource, manuscript editing, patient follow up.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics committee of Zanjan university of Medical Sciences (ID: IR.ZUMS.REC.1398.278). Moreover, the study protocol of the original study was prospectively registered on the Iranian Registry of Clinical Trials (www.IRCT.ir, Identifier: IRCT20190412043247N2). All patients provided with written informed consent prior to the recruitment.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Role of Dr. Abidi pharmaceutical company
The company supplied the medication and placebo for the original study. The company had no role in the development of the protocol, process of the study, or preparation of this manuscript.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ghanbari, S., Gohari, S., Reshadmanesh, T. et al. Empagliflozin improves left ventricular ejection fraction and end systolic volume in patients with type 2 diabetes mellitus and coronary artery disease: a post-hoc analysis of EMPA-CARD trial. J Diabetes Metab Disord 23, 1107–1111 (2024). https://doi.org/10.1007/s40200-024-01393-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-024-01393-8