Abstract
Purpose
Weak care cascade of diabetes from the time of screening, diagnosis, treatment initiation and attainment of optimal glycemic control is a public health challenge particularly in resource limited settings. We aimed to assess the diabetes care cascade in India and its determinants in the 15–49 age group.
Methods
We conducted a secondary data analysis of the National Family Health Survey (NFHS-5, 2019–2021), a nationally representative cross-sectional survey, including a total of 724,115 women and 101,839 men with mean (SD) age 30.6 (9.9) years.
Results
The prevalence of self-reported Diabetes Mellitus (DM) in the sample was 2.14% (n = 14,116, 95% CI: 2.06, 2.21) of which 55.13% (n = 6990, 95% CI: 53.37, 56.88) were currently undergoing anti-diabetes therapy. The net prevalence of DM including both old and new cases detected on screening was 2.9%. Poor glycemic control was observed in 52.43% (n = 3506, 95% CI: 50.69, 54.16) of patients with DM on anti-diabetes therapy. Patients from the richest wealth quintile (aOR = 5.17, 95% CI: 1.93, 13.84) had significantly higher odds of accessing private health facilities, while female patients with DM were less likely to be on anti-diabetes therapy.
Conclusion
The prevalence of self-reported DM in India has increased from 1.7% (NFHS-4, 2015-16) to 2.1% (NFHS-5, 2019-21) while more than half of existing patients continue to remain undiagnosed. Consequently, diabetes care cascade have major lacunae at every stage from screening to diagnosis, initiation of effective treatment, and achievement of safe blood glucose levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Abbreviations:
DM (Diabetes Mellitus), NFHS (National Family Health Survey), RBS (Random Blood Sugar), LMICs (Low- and Middle-Income Countries).
Introduction
Diabetes Mellitus (DM) is a chronic illness with a global burden of 537 million adults aged 20–79 years in 2021 [1]. These estimates are projected to increase several folds by 2030 (643 million), and by 2045 (783 million) primarily attributing to the ageing world population [1, 2]. The global prevalence of Type 2 DM is expected to increase to 7079 cases per 100,000 people by 2030 [3]. Diabetes has emerged in the list of top ten causes of death globally and is linked to severe complications such as neuropathy, kidney disease, cardiovascular diseases, foot amputations, etc. [4, 5].
Additionally, 10.6% of adults worldwide (~ 541 million individuals) have impaired glucose tolerance (IGT), a condition of raised glucose levels above the normal range while below the diabetic threshold [1]. Screening and diagnosis of undiagnosed asymptomatic patients with DM or IGT is essential for preventing the premature onset and progression of diabetes related vascular complications [6, 7]. India has the second highest prevalence (67.8 million) of DM after China whereas it ranks first in diabetes-related Disability Adjusted Life Years (DALYs) accounting for 11.2 million DALYs [8].
The rule of two-thirds in diabetes is well established in India which suggests only two in three people with DM are diagnosed, HbA1c is not assessed in two in three diagnosed patients, and of those assessed, two in three do not achieve target glycemic control. Furthermore, only two in three patients with DM adhere to anti-diabetes therapy while only one in three adhere to their exercise recommendations [9, 10]. A nationwide study from India above 12,000 households ascertained that among patients with DM, only 45.8% were aware of their condition, 36.1% were on anti-diabetes treatment, and just 15.7% achieved optimal glycemic control indicative of the high burden of undiagnosed cases, medication non-adherence and adverse patient outcomes [11]. A large nationally representative demographic and health survey from India (2015-16) in more than 2,00,000 household found that 42% of individuals with high glucose levels were unaware of their condition despite 45% of these undiagnosed patients having access to healthcare services suggestive of a combination of poor awareness and suboptimal health seeking behaviors [12]. Delayed initiation of treatment in new cases of DM with poor medication adherence contributes to persistent suboptimal glycemic control, complications and adverse patient outcomes with high burden of treatment costs straining healthcare sustainability particularly in resource challenged settings [13, 14].
Information from the updated round of the National Family Health Survey (2019-21) in India which involved universal screening of blood pressure and blood glucose levels of all participants aged 15–49 years can be utilized to assess the population level cascade of care in patients with DM.
The study aims to assess the diabetes care cascade in India and their determinants in the 15–49 age group constituting the largest economically productive age-group in whom a high burden of undiagnosed and untreated diabetes contributes to the early onset and progression of DM related complications with premature mortality and their associated social and health costs [6, 7].
The specific objectives were to estimate the prevalence of DM in India in the 15–49 age group and their determinants, ascertain the proportion of previously diagnosed DM cases initiated on treatment and assess treatment preferences, estimate the proportion of new (previously undiagnosed) DM cases, and estimate the glycemic control of patients with DM on anti-diabetes treatment. Furthermore, regional variation in the level of diabetes care across the states and union territories of India were also assessed. Findings from this analysis would also enable identifying gaps and strengthening of the National Program for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS) in India by identifying key priority areas and in the design and implementation of evidence-based interventions [15].
Methods
This study is a secondary data analysis from the fifth round of National Family Health Survey (NFHS-5), a nationally representative household survey, conducted from 17 to 2019 to 30 April 2021. Details of the sampling method and survey questionnaires are reported in detail elsewhere [16]. A total of 724,115 women and 101,839 men were interviewed using a structured interview schedule using Computer Assisted Personal Interviewing (CAPI). Along with survey questions, there were measurements of height, weight, random blood glucose and blood pressure in the participants.
Data Sources.
Men’s Recode dataset and Women’s Recode dataset was appended and then merged with the Household Recode dataset for the analysis. We considered both men and non-pregnant women aged 15 to 49 years for the analysis. All datasets used in the analysis were downloaded from DHS (http://www.dhsprogram.com/) after obtaining necessary permission.
Description of variables
Outcome variables
Treatment seeking behavior (public or private health facilities) and diabetes control were selected as the dependent variable in our regression models. Treatment seeking behavior was assessed in terms of whether a previously diagnosed patient with DM (defined as having awareness of person’s DM status as yes) is currently taking anti-diabetes medication to lower blood glucose or not, and the type of treatment facility accessed (public or private). “Other health facilities” was excluded in the regression models owing to a smaller number of observations in this category. Poor diabetes control was defined as participants who were currently taking prescribed medicine to lower their blood glucose but had random blood glucose levels > 180 mg/dL.
Explanatory variables
We examined how the control of diabetes and treatment seeking patterns are associated by the sociodemographic and socioeconomic variables including participant age, sex, education, marital status and wealth index. Other variables included in the regression models included body mass index, smoking status, alcohol consumption, dietary pattern and physical activity pattern representing the behavioral risk factors. For health system factors, we considered type of healthcare facility accessed, health insurance and Health Index [17] as a surrogate for health system performance as the relevant independent variables.
Operational definitions
Participants who answered “yes” to a question asking them if they were told they had high blood glucose on two or more occasions were categorized as previously diagnosed patients with diabetes mellitus (DM). New cases of DM were considered as those participants without a previous history of DM who were screened with Random Blood Sugar (RBS) > 200 mg/dL. High blood glucose levels suggestive of impaired glucose tolerance were considered as those participants without a previous history of DM screened with RBS > 160 < 200 mg/dL.
Wealth index score is derived from principal component analysis of scores based on household performances as per various indicators covered under various dimensions. Participants were categorized into 5 categories of wealth index: poorest, poor, middle, rich and richest.
For comorbidities, 3 categories were considered: (i) participants without any comorbidity having only diabetes mellitus, (ii) having both DM and hypertension, and (iii) having DM and any thyroid disorder, and/or heart disease and/or chronic kidney disease (without hypertension). Smoking status was categorized as smoker and non-smoker.
BMI was classified based on the WHO Pan Asian classification as underweight (< 18.5 kg/m2), normal weight (18.5–22.9 kg/m2), overweight/obese (≥ 23.0 kg/m2).
No information on physical activity was directly available in the NFHS-5 datasets. Hence, we employed occupation as a surrogate variable to measure the physical activity level. Physical activity was assessed on the basis of type of occupation of the respondent, wherein not working, clerical and sales jobs were classified as having inadequate physical activity, while other job types were considered to involve adequate physical activity. Dietary pattern was assessed based on the frequency of fruit and vegetable consumption. Never, weekly, occasionally consumption of both fruit and vegetable was considered as unhealthy, while daily consumption of these items was considered a healthy diet.
Health Index is a tool to assess performance for states and union territories (UTs) based on 24 indicators under ‘Health Outcomes’, ‘Governance and Information’ and ‘Key Inputs/Processes’ domains. Health Indices for each state and union territory of India was derived as per the government of India’s apex public policy think-tank NITI Aayog Round 4 (2019–2020). The indices were then categorized as Index score ≥ 62, Index score ≥ 48 and < 62 and Index score < 48 [15]. Since financing diabetes care may be more feasible in richer states as compared to poorer states of India, we considered each state’s/UTs gross domestic product (GDP) as an independent variable. State per capita income was categorized as high (≥ Rs. 3,00,000), medium (Rs. 1,00,000-Rs. 2,99,999) and low (< Rs. 1,00,000).
Statistical analysis
We have reported the summary statistics of the outcome variables including frequencies and proportions for categorical variables and where applicable, means along with standard deviations for continuous variables, accounting for the survey design and sampling weights. We expressed proportions with 95% Confidence Intervals (C.I.) after applying pre-specified sampling weights to account for the survey design. Bivariate analysis was conducted using the chi-square test and the variables found significantly associated (P < 0.05) were selected for the multivariate regression model. Further, any non-significant variable not selected for the multivariate model was added to the model one at a time in a stepwise manner along with the significant variables retained earlier. Model with the best fit (P > 0.05) was chosen as the final model for multivariate regression for determining associations between socio-demographic factors, lifestyle characteristics, and the treatment seeking behavior of patients with DM. All assumptions and prerequisites were checked for logistic regression analysis, including diagnostic methods to check for strong influential outliers in the model. Predictor variables were assessed for multicollinearity. Analysis was performed using Stata version 15.1 (StataCorp LLC, Texas, USA) and a P-value < 0.05 was considered statistically significant.
Ethics statement
The ethical approval for NFHS 5 survey was obtained from ethics review board of the International Institute of Population Sciences, Mumbai, India. Written and informed consent was obtained from each respondent before participating in the survey. The de-identified datasets were obtained after a written permission from the DHS which also approved the study proposal. Since the NFHS-5 dataset is an anonymous publicly available dataset with no identifiable information about the participants, no separate ethical approval is required for this secondary data analysis.
Results
We included 788,974 individuals aged 15–49 years (695,707 women and 93,267 men) in the analysis. Table 1 presents the socio-demographic and lifestyle characteristics of the participants. The mean (SD) age of the participants was 30.6 (9.9) years. Most of the participants were women (88.2%) while a majority (51.0%) had at least a secondary education. Almost 70% of the participants were currently married. More than half (58%) of the participants reported accessing public health facilities while nearly 70% of the participants were not covered under any health insurance. Overall, 8.3% and 3.3% of the participants reported tobacco smoking and alcohol consumption, respectively. Nearly one in four participants (24.5%) were overweight or obese. Not working, clerical and sales jobs with presumed low physical activity levels were observed in a majority (52.1%) of the participants.
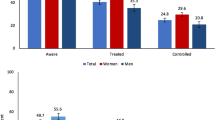
The prevalence of self-reported Diabetes Mellitus (DM) in the sample was 2.14% (n = 14,116, 95% CI: 2.06, 2.21) of which 55.13% (n = 6990, 95% CI: 53.37, 56.88) were currently undergoing anti-diabetes therapy (Fig. 1).
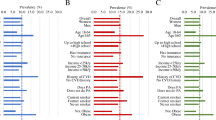
Factors that were associated with being on treatment status in previously diagnosed patients with DM included male compared to female gender (aOR = 2.76, 95% CI: 1.70, 4.51), middle-age compared to younger age-groups (aOR = 2.18, 95% CI: 0.73, 6.52), and overweight/obese compared to normal and underweight (aOR = 1.68, 95% CI: 0.75, 3.76) patients (Fig. 2, Table S1).
Distribution of Socio-demographic and lifestyle characteristics of previously diagnosed patients with Diabetes and their treatment status
Adjusted analysis to determine the factors associated with being on treatment status in previously diagnosed patients with DM (N = 14,116). Private health facilities comprise of private hospital, pharmacy/drugstore, clinic and AYUSH.
Among the patients on anti-diabetes therapy, high blood glucose resulting in poor glycemic control was observed in 52.43% (n = 3506, 95% CI: 50.69, 54.16) participants (Fig. 1). On adjusted analysis, middle-aged (aOR = 3.71, 95% CI: 1.83, 7.52) and overweight/obese participants (aOR = 1.90, 95% CI: 1.36, 2.64) had significantly higher odds of having uncontrolled blood glucose levels. Furthermore, participants with the richest wealth index were found to have significantly higher odds of having uncontrolled glucose levels (aOR = 2.33, 95% CI: 1.67, 3.26) (Fig. 3, Table S2).
Among participants without a prior history of DM (n = 735,277), the magnitude of newly diagnosed DM (RBS > 200 mg/dL) was 0.94% (n = 5656, 95% CI: 0.90, 0.99), and likely prediabetes (RBS ≥ 160 < 200 mg/dL) was 1.96% (n = 12,987, 95% CI: 1.90, 2.02). High blood glucose (RBS ≥ 160) was therefore cumulatively observed in 2.91% (n = 18,643, 95% CI: 2.84, 2.98) participants without previous history of DM on screening. On adjusted analysis, males compared to females (aOR = 1.37, 95% CI: 1.12, 1.66) and middle-aged compared to younger participants (aOR = 10.57, 95% CI: 7.17, 15.56) had significantly higher odds of being detected with high blood glucose levels. Furthermore, those having a higher education had comparatively lower odds of having high blood glucose levels (aOR = 0.90, 95% CI: 0.67, 1.21) as compared to those with secondary education (aOR = 1.26, 95% CI: 1.02, 1.55) and this difference was statistically significant (P = 0.03) (Fig. 4, Table S3).
Distribution of sociodemographic and lifestyle characteristics of participants detected with high blood glucose levels (without previous history of DM)
Adjusted analysis to determine the factors associated with high blood glucose levels (RBS ≥ 160 mg/dL) among participants without a prior history of DM (N = 735,277). Dietary pattern is based on consumption of fresh fruits and vegetables
The type of health facility accessed by participants who were on treatment for diabetes were also compared (Fig. 5, Table S4). Overweight/obese participants (aOR = 4.69, 95% CI: 1.16, 13.50), those with higher education (aOR = 1.04, 95% CI: 0.49, 2.19), those belonging to the richest wealth index (aOR = 5.17, 95% CI: 1.93, 13.84) and those comorbid or multimorbid (aOR = 1.66, 95% CI: 1.02, 2.73) were found to have significantly higher odds of accessing private compared to public facilities for treatment.
Distribution of factors associated with choice of treatment facility in patients with Diabetes
Adjusted analysis to determine the factors associated with choice of treatment facility in patients with DM. Public versus private facilities were compared for the logistic regression analysis. Other morbidities include any thyroid disorder; heart disease; and chronic kidney disease
Figure 6 assesses the regional variation in the care cascade of DM among the different states and union territories of India. Southern states report a higher proportion of newly diagnosed DM cases as compared to the northern states of the country. A majority of the states and UTs had more than 50% of patients living with diabetes, and having poor glycemic control despite being on anti-diabetes therapy.
Discussion
This large-cross sectional survey suggests that nearly one in two young and middle-aged patients with previously diagnosed DM in India were not on regular anti-diabetes treatment, and of those on treatment, nearly half had uncontrolled blood sugar levels. The net prevalence of DM was 2.9% while the prevalence of self-reported DM was 2.1% which is slightly higher than that observed in the previous round of NFHS (2015-16) (1.7%) [12] and in another national survey (2017) (1.8%) [18]. Our study suggests that 30.54% of the existing cases of DM in the country were undiagnosed which is nearly in agreement with the rule of two thirds [8] and consistent with previous round of the survey [12]. However, in comparison, to the ICMR-INDIAB study, the proportion of undiagnosed DM cases in this study is substantially lower (47.3%) [19]. Furthermore, the proportion of previously diagnosed patients with DM with controlled blood sugar levels was lower compared to the pooled estimate from previous Indian studies (56.4%) [20].
Our study found that treatment seeking behavior for DM increases proportionally with age, which is comparable to other studies conducted in Asia, including Nepal, China and Bangladesh [21,22,23]. Our analysis also indicated that men when diagnosed with DM are more likely to be on treatment. Poor treatment seeking behavior in women can be attributed to poor awareness and difficult treatment access signifying the need for engendering public health programs for DM management [11]. Furthermore, overweight/obese participants have higher odds of having uncontrolled glycaemia, a finding consistent with the “Investigation of the Glycosylated Hemoglobin on Therapy in Indian diabetics” (TIGHT) study [24]. Our analysis showed that age, education, BMI and wealth index are the most important risk factors associated with glycemic control in patients with DM, a finding consistent with previous studies [25]. The present study also corroborates sparse evidence that patients with DM in India having higher socioeconomic status do not necessarily achieve better glycemic control suggestive of differential medical adherence characteristics [26]. Our analysis also finds preference of private health facilities for treatment by the participants belonging to the richest wealth index, like the findings from a study in South Africa, suggesting of factor mediated to treatment affordability [27].
Southern states of India have a higher prevalence of DM than Northern India possibly due to correlation with their improved economic status, a finding consistent with another national ICMR-INDIAB study [19, 28]. Improved implementation of opportunistic and community screening processes recommended by the NPCDCS can improve screening yield, but that factor could not be assessed in this study [15]. Furthermore, we observed that in states with comparatively poor socioeconomic indicators known as the empowerment action group states such as Uttarakhand and Bihar, more than 50% of the previously diagnosed patients with DM had poor glycemic control despite being on anti-diabetes therapy. These findings are suggestive of the high burden of clinical inertia and medication non-adherence [29] that deleteriously affect diabetes care in low-resource settings. Consequently, strengthening the primary health systems in the country may translate into effective treatment cascade for diabetes care in India [30].
The strengths of this study include the large sample size ensuring adequate power and narrow confidence intervals of the study outcomes. Since the survey coverage was across all states of India, the study findings are representative of the population, and reflect high generalizability. Nevertheless, this study has certain limitations. First, the cross-sectional nature of this study does not permit the establishment of causal and temporal relationships. Second, since individual data on HbA1c and fasting blood glucose levels were unavailable in the public domain, we employed random blood glucose as a biomarker for diagnosis of DM which does not account for the presence or absence of symptoms which may cause less reliability of the disease burden estimate. Furthermore, the accuracy of glycemic control established through RBS will be much lower compared to HbA1c, which is the recommended gold standard [31]. Furthermore, we could not assess the implementation of adherence phenomenon such as frequency of missed dosing which is not captured in this survey. Moreover, there was no data to distinguish whether the treated patients were on insulin, or oral hypoglycemic agents alone, or both. Third, our analysis and findings are limited to 15–49-year-old non-pregnant women and men although the prevalence of DM and related complications will be significantly higher in the elderly population as observed in the Global Burden study [32]. Lastly, this study does not differentiate between Type 2 Diabetes and other variants of diabetes, such as Latent Autoimmune Diabetes of Adults (LADA), Type 1 diabetes, Post pancreatitis DM, etc. in which case the patients would be expected to be on insulin, and their BMI may not correlate with their glycemic control as a predictor, since these patients may be phenotypically ectomorphic or belong to low BMI category.
A slight reduction in proportion of adults remaining undiagnosed with DM although a large proportion still remains undiagnosed and exhibits poor treatment seeking behavior despite efforts in strengthening the NPCDCS [33]. Implementing community-wide screening, strengthening primary care and identifying high-risk groups through this programme is recommended. Our study results suggest that in India screening of a naïve population with RBS alone is expected to yield nearly one new patient of DM and another two cases of pre-diabetes every hundred participants screened. Early initiation of diabetes care in new cases, and lifestyle modifications in pre-diabetes cases can significantly reduce the burden of complications and disease burden while improving the quality of life with enhanced economic productivity. These findings may call for strengthening attention on non-communicable diseases during the monitoring and implementation of national health policies.
Our study has certain other important public health policy implications. First, a large subset of the population in India remains undiagnosed with DM indicative of lack of effective screening and missed opportunities in primary care outpatient settings despite the NPCDCS recommending both opportunistic screening by doctors and nurses, and community screening by frontline and community health workers. As none of the sociodemographic factors except education were linked to newly diagnosed DM in this study, hence future operational research should be directed towards identifying specific public health system barriers that reduce the efficiency and effectiveness of population-based screening for DM.
Second, in this study, glycemic control was negatively associated with high BMI. Consequently, physicians should provide enhanced focus on overweight/obese individuals with DM who are less likely to have control over their blood glucose levels that further accelerates their risk of disease progression. Third, there has been a significant improvement in the proportion of patients on anti-diabetes treatment (55.13%) compared to that in the NFHS-4 2015-16 (40.5%) [34] suggestive of improved drug accessibility that could be secondary to schemes such as the Pradhan Mantri Jan Aushadi Yojana (PMJAY) that promote people’s access to high quality generic medicines at affordable prices. Third, nearly one in two patients on anti-diabetes medication had random blood glucose < 180, suggestive of improved control reflecting the positive correlation between increased drug accessibility and drug adherence in the Indian context.
In conclusion, diabetes care cascade in younger and middle-aged groups in India have major lacunae at each stage from screening and diagnosis, initiation of effective anti-diabetic treatment, and achievement of safe blood glucose levels. Identification of high-risk groups for opportunistic screening, implementation of community-based screening, and strengthening primary care and sensitizing medical practitioners are urgently warranted.
Data availability
The NFHS-5 survey data is available free of charge on request from the International Institute of Population Sciences through the DHS program portal https://dhsprogram.com/data/.
References
IDF diabetes atlas- 10th Edition. International Diabetes Federation. ISBN: 978-2-930229-98-0., 2021. https://diabetesatlas.org/atlas/tenth-edition/. Accessed November 30, 2022.
World population ageing 2019. United Nations: Department of Economic and Social Affairs. Population Division., 2020. https://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2019-Highlights.pdf. Accessed November 30, 2022.
Khan MA, Hashim MJ, King JK, Govender RD, Mustafa H, Al Kaabi J. Epidemiology of type 2 diabetes–global burden of disease and forecasted trends. J Epidemiol global health 2020 Mar;10(1):107. https://doi.org/10.2991%2Fjegh.k.191028.001.
World Health Organization. (2020, December 9). The top 10 causes of death. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death. Accessed November 30, 2022.
Deshpande AD, Harris-Hayes M, Schootman. Epidemiology of diabetes and diabetes-related complications. M Phys Ther. 2008;88:1254–64. https://doi.org/10.2522/ptj.20080020.
Rao SS, Disraeli P, McGregor T. Impaired glucose tolerance and impaired fasting glucose. American family physician. 2004 Apr 15;69(8):1961–8.
Fowler MJ. Microvascular and macrovascular complications of diabetes. Clinical diabetes. 2008 Apr 1;26(2):77–82. https://doi.org/10.2337/diaclin.26.2.77.
Lin X, Xu Y, Pan X, Xu J, Ding Y, Sun X, Song X, Ren Y, Shan PF. Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025. Scientific reports. 2020 Sep 8;10(1):1–1. https://doi.org/10.1038/s41598-020-71908-9.
Kalra S, Saboo B, Sahay R, Khandelwal D, Talwar V, Unnikrishnan AG. The rule of two-thirds in diabetes epidemiology. Indian J Endocrinol Metabol. 2017 Jan;21(1):242. https://doi.org/10.4103/2230-8210.196027.
Mohan V, Shah SN, Joshi SR, Seshiah V, Sahay BK, Banerjee S, Wangnoo SK, Kumar A, Kalra S, Unnikrishnan AG, Sharma SK. Current status of management, control, complications and psychosocial aspects of patients with diabetes in India: results from the DiabCare India 2011 study. Indian J Endocrinol Metabol. 2014 May;18(3):370. https://doi.org/10.4103/2230-8210.129715.
Mathur P, Leburu S, Kulothungan V. Prevalence, awareness, treatment and control of diabetes in India from the countrywide National NCD Monitoring Survey. Front Public Health 2022 Mar 14;10:205. https://doi.org/10.3389/fpubh.2022.748157.
Claypool KT, Chung MK, Deonarine A, Gregg EW, Patel CJ. Characteristics of undiagnosed diabetes in men and women under the age of 50 years in the Indian subcontinent: the National Family Health Survey (NFHS-4)/Demographic Health Survey 2015–2016. BMJ Open Diabetes Research and Care. 2020 Feb 1;8(1):e000965. https://doi.org/10.1136/bmjdrc-2019-000965.
Aschner P, Gagliardino JJ, Ilkova H, Lavalle F, Ramachandran A, Mbanya JC, Shestakova M, Chantelot JM, Chan JC. Persistent poor glycaemic control in individuals with type 2 diabetes in developing countries: 12 years of real-world evidence of the International Diabetes Management Practices Study (IDMPS). Diabetologia. 2020 Apr;63:711–21. https://doi.org/10.1007/s00125-019-05078-3.
Kishore J, Kohli C, Gupta N, Kumar N, Sharma PK. Awareness, practices and treatment seeking behavior of type 2 diabetes mellitus patients in Delhi. Annals of medical and health sciences research. 2015 Jul 24;5(4):266 – 73. https://doi.org/10.4103/2141-9248.160184.
National Programme for Prevention & Control of Cancer, Diabetes, Cardiovascular Diseases & Stroke (NPCDCS). National Health Mission, Ministry of Health and Family Welfare, Government of India. (n.d.). https://nhm.gov.in/index1.php?lang=1&level=2&sublinkid=1048&lid=604.Accessed December 1, 2022.
International Institute for Population Sciences (IIPS) and ICF. National Family Health Survey (NFHS-5), 2019-21: India: volume I. Mumbai: IIPS; 2021.
Health Performance Index, Aayog NITI, National Institution for Transforming India., Government of India. (n.d.). https://social.niti.gov.in/hlt-ranking. Accessed December 1, 2022.
Nagarathna R, Bali P, Anand A, Srivastava V, Patil S, Sharma G, Manasa K, Pannu V, Singh A, Nagendra HR. Prevalence of diabetes and its determinants in the young adults indian population-call for yoga intervention. Front Endocrinol 2020 Dec 11;11:507064. https://doi.org/10.3389/fendo.2020.507064.
Anjana RM, Deepa M, Pradeepa R, Mahanta J, Narain K, Das HK, Adhikari P, Rao PV, Saboo B, Kumar A, Bhansali A. Prevalence of diabetes and prediabetes in 15 states of India: results from the ICMR–INDIAB population-based cross-sectional study. The lancet Diabetes & endocrinology. 2017 Aug 1;5(8):585 – 96. https://doi.org/10.1016/S2213-8587(17)30174-2.
Daniel RA, Mani K, Aggarwal P, Gupta SK. Treatment and control of diabetes in India: A systematic review and meta-analysis. Journal of Primary Care Specialties. 2022 Sep 1;3(3):69. https://doi.org/10.4103/jopcs.jopcs_10_22.
Gyawali B, Hansen MR, Povlsen MB, Neupane D, Andersen PK, McLachlan CS, Sandbæk A, Vaidya A, Kallestrup P. Awareness, prevalence, treatment, and control of type 2 diabetes in a semi-urban area of Nepal: findings from a cross-sectional study conducted as a part of COBIN-D trial. PloS one. 2018 Nov 2;13(11):e0206491. https://doi.org/10.1371/journal.pone.0206491.
Wang Q, Zhang X, Fang L, Guan Q, Guan L, Li Q. Prevalence, awareness, treatment and control of diabetes mellitus among middle-aged and elderly people in a rural Chinese population: A cross-sectional study. PloS one. 2018 Jun 1;13(6):e0198343. https://doi.org/10.1371/journal.pone.0198343.
Khan N, Oldroyd JC, Hossain MB, Islam RM. Awareness, treatment, and control of diabetes in Bangladesh: evidence from the Bangladesh Demographic and Health Survey 2017/18. International Journal of Clinical Practice. 2021 Jul 14;2022. https://doi.org/10.1155/2022/8349160.
Borgharkar SS, Das SS. Real-world evidence of glycemic control among patients with type 2 diabetes mellitus in India: the TIGHT study. BMJ Open Diabetes Research and Care. 2019 Jul 1;7(1):e000654. https://doi.org/10.1136/bmjdrc-2019-000654.
Rakhis Sr SA, AlDuwayhis NM, Aleid N, AlBarrak AN, Aloraini AA. Glycemic control for type 2 diabetes mellitus patients: A systematic review. Cureus. 2022 Jun 21;14(6). https://doi.org/10.7759/cureus.26180.
Ahsan KZ, Iqbal A, Jamil K, Haider MM, Khan SH, Chakraborty N, Streatfield PK. Socioeconomic disparities in diabetes prevalence and management among the adult population in Bangladesh. Plos one 2022 Dec 20;17(12):e0279228. https://doi.org/10.1371/journal.pone.0279228.
Mhlanga D, Hassan A. An investigation of the factors influencing the choice of healthcare facility in South Africa. Int J Res Bus Social Sci. 2022 Jun;5(4):2147–4478. https://doi.org/10.20525/ijrbs.v11i4.1765.
Ranasinghe P, Jayawardena R, Gamage N, Sivanandam N, Misra A. Prevalence and trends of the diabetes epidemic in urban and rural India: A pooled systematic review and meta-analysis of 1.7 million adults. Annals of epidemiology. 2021 Jun 1;58:128 – 48. https://doi.org/10.1016/j.annepidem.2021.02.016.
Basu S, Sharma N. Under-recognised ethical dilemmas of diabetes care in resource-poor settings. Indian J Med Ethics. 2018 Oct;3(4):324–6. https://doi.org/10.20529/IJME.2018.048.
Basu S, Sharma N. Diabetes self-care in primary health facilities in India-challenges and the way forward. World journal of diabetes. 2019 Jun 6;10(6):341. https://doi.org/10.4239/wjd.v10.i6.341.
American Diabetes Association Professional Practice Committee, American Diabetes Association Professional Practice Committee:. 6. Glycemic targets: standards of medical care in diabetes—2022. Diabetes Care. 2022 Jan;45(Supplement_1):S83-96. https://doi.org/10.2337/dc22-S006.
Tandon N, Anjana RM, Mohan V, Kaur T, Afshin A, Ong K, Mukhopadhyay S, Thomas N, Bhatia E, Krishnan A, Mathur P. The increasing burden of diabetes and variations among the states of India: the Global Burden of Disease Study 1990–2016. The Lancet Global Health. 2018 Dec 1;6(12):e1352-62. https://doi.org/10.1016/S2214-109X(18)30387-5.
Thakur JS, Paika R, Singh S. Burden of noncommunicable diseases and implementation challenges of National NCD Programmes in India. medical journal armed forces india. 2020 Jul 1;76(3):261-7. https://doi.org/10.1016/j.mjafi.2020.03.002.
Prenissl J, Jaacks LM, Mohan V, Manne-Goehler J, Davies JI, Awasthi A, Bischops AC, Atun R, Bärnighausen T, Vollmer S, Geldsetzer P. Variation in health system performance for managing diabetes among states in India: a cross-sectional study of individuals aged 15 to 49 years. BMC Med. 2019 Dec;17:1–2. https://doi.org/10.1186/s12916-019-1325-6.
Acknowledgements
We thank the IIPS for providing access to the datasets and permission to conduct this analysis.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Design, concepts: SB, PA.
Methodology: SB, VM, MM.
Formal analysis: VM, MM, SB.
Literature review: All authors.
Writing (First Draft): SB, VM.
Writing (Review and Editing): All authors.
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Basu, S., Maheshwari, V., Malik, M. et al. Diabetes care cascade and their predictors in young and middle-aged population in India: evidence from the National Family Health Survey (2019-21). J Diabetes Metab Disord 22, 1405–1415 (2023). https://doi.org/10.1007/s40200-023-01263-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-023-01263-9