Abstract
Background
The current study aimed to investigate the Superoxide dismutase, Glutathione Peroxidase activity, Advanced oxidation Protein products levels, Malondialdehyde levels, Baseline Conjugated Diene concentration, and 8-Isoprostaglandin F2α (8-IPG-F2α) quantification in diabetic and non-diabetic senile cataract patients to find out the pathomechanism of early onset of cataract in diabetic patients.
Methods
This case–control study was performed on 184 subjects undergoing cataract surgery. For 8-IPG-F2α quantification, 35 diabetics and non-diabetic lenses and the entire study included 22 patients with diabetic senile cataracts and non-diabetic senile cataracts of aqueous humor age ≥ 40 years. Ninety-two patients with diabetic senile cataract and non-diabetic senile cataract lenses aged ≥ 40 years were incorporated for all other studies. The student’s t-test was used for statistical analysis.
Results
From the study population, the mean age was 63.82 ± 0.6, and 75% of them were female. Higher female prevalence in both groups was observed. The results revealed that the superoxide dismutase and glutathione peroxidase activity were significantly reduced in diabetic patients compared to non-diabetic patients (p < 0.001) in both lenses and aqueous humor. Malondialdehyde, conjugated diene, and 8-IPG-F2α levels significantly increased in diabetic patients when compared to non-diabetic (p < 0.01), and advanced oxidation protein products levels also significantly increased in diabetic patients when compared to non-diabetics in both lenses and aqueous humor (p < 0.001).
Conclusion
The current study revealed that oxidative stress and Lipid per-oxidation have an imperative role in the diabetic-related complication, specifically in the lens, may have a responsibility in the pathomechanism of early onset of cataracts coupled with diabetes mellitus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cataract is a multifactorial process in which there is a combination of a linked process such as post-translational modifications, aggregation, fragmentation, and precipitation of lens proteins leading to opacification of the lens [1]. Morphologically it can be defined as the disturbance of the optical homogeneity, which can cover the lens partially or wholly, leading to blindness [2].
It is one of the most important causes of unavoidable blindness globally, accounting for 51% of all-cause blindness [3, 4]. The estimation of the first worldwide blindness by the World Health Organization (WHO) in 1972 was about 10–15 million, and they also estimated that about 1–2 million become blind every year [1].
The pathogenesis of cataracts is known to be inclined by several factors, including oxidative stress. The lens is exposed to light throughout the lifetime and prone to oxidative attack induced by reactive oxygen/ nitrogen species (ROS/RNS) [5, 6]; it is equipped with an efficient antioxidant system for shielding this oxidative/nitrosative stress. The primary enzymatic antioxidants in the lens are superoxide dismutase [7], Catalase [8], glutathione peroxidase [9], glutathione reductase, glutathione-S-transferase [10], thioredoxin system. [11] Moreover, non-enzymatic antioxidants are reduced glutathione [12], ascorbic acid, Vitamin A, E [13,14,15,16]. A decline in the activity of all these enzymes and molecules is reported in cataract formation [17, 18]. Aging, hypertension, diabetes mellitus, smoking, renal disease, malnutrition contribute to cataracts [19, 20].
Diabetes mellitus (DM) is significant metabolic anarchy differentiated by a disturbance in glucose metabolism and impaired carbohydrate, lipid, and protein metabolism, leading to long-term difficulties. The prevalence of DM has augmented dramatically over the past two decades and persists in increasing [21]. Multiple mechanisms have been concerned with cataract development progress in DM, such as excessive tissue sorbitol concentrations, abnormal glycosylation of lens proteins, and increased free radical production in the intraocular region [22]. Ocular complications are common in diabetes, and cataract becomes the primary cause of blindness in those patients [23]. The epidemiological studies revealed the fivefold increased prevalence of cataracts in diabetic subjects compared with the non-diabetic population. Growing evidence indicates that both duration of diabetes and quality of glycemic control is the most critical risk factors for diabetic cataract formation [24].
Surgical removal of cloudy/opaque lenses and replacement with a synthetic intraocular lens is the only available treatment for cataracts [25]. In developed countries, the surgical rate has been increased above the WHO anticipated range (3000/million people/year to 7000 – 11,000/ million people) [26,27,28,29]. Even though surgery is a successful measure for cataract blindness, significant risks are associated with post-surgery, such as inflammation in the eye, retinal detachment, infection in the eye, glaucoma, secondary cataract [30].
A cataract is a degenerative protein disorder, and its irreversible nature directs vision researchers in the track of preventive measures for the management of blindness. The current study focused on investigating the relationship between oxidative stress, lipid peroxidation, and diabetes to prevent the early onset of cataracts in diabetic patients by quantifying the levels of antioxidative enzymes and lipid peroxidation products in diabetic cataract patients in contrast to the non-diabetic.
Materials and methods
Patients and samples
This comparative case–control observational study was carried out at Sri Ramachandra Medical Center on subjects who had undergone cataract surgery between March 2018 to April 2019. The control group was non-diabetic patients who had cataract extraction during the study period. Diabetic cataract (study group) patients had a previous history of type 2 diabetes mellitus, and the diagnosis was based on random blood sugar > 200 mg/dl within one week of the surgery. All subjects underwent a complete eye examination in the ophthalmic OPD, and cataract was diagnosed using slit-lamp and fundus examination, which had severe visual disturbances and visual acuity of below 0.3. The study was approved by the Institutional Ethical Committee (IEC-NI/15/OCT49/61), and all participants provided written informed consent the day before the surgery. In this current study for 8-Isoprostaglandin F2α(8-IPG-F2α) quantification, 35 diabetic (study group) and 35 non-diabetic lenses (control group) were included, and for all other studies, 92 patients with diabetic senile cataract and 92 patients with non-diabetic senile cataract were incorporated. For the entire study, 22 patients with diabetic senile cataracts and 22 patients with non-diabetic senile cataracts of aqueous humor were incorporated in this study.
Inclusion Criteria
Patients having cataracts with diabetes mellitus (study group) and cataracts without diabetes mellitus (control group) in both groups aged ≥ 40 years were included in this study.
Exclusion Criteria
The study expelled smoking history, glaucoma, eye infections, eye diseases, and antioxidant therapy patients.
Sample preparations
Cataract lens was obtained after Extracapsular cataract extraction, and Small Incision cataract surgery procedure and 0.15 ml of aqueous humor were aspirated from the anterior eye chamber with a 27-gauge needle connected to a tuberculin syringe, immediately stored in an icebox and transferred to central research lab within two hours of extraction and stored at -80 °C. The stored lens was thawed, the tissue was sliced into parts, and tissue homogenization was done according to the Assay Kit protocol. 0.2 mM Butylated hydroxytoluene (BHT) was added during homogenization to prevent auto-oxidation. Aqueous humor was diluted with PBS buffer to measure superoxide dismutase, glutathione peroxidase, conjugated diene, malondialdehyde, advanced oxidation protein products, and ELISA buffer for 8-IPG-F2α and further proceeded for the assay.
Activity of Superoxide Dismutase (SOD)
SOD activity is standardized using the Cytochrome C, and Xanthine oxidase coupled assay. The Cayman Chemical Assay Kit for SOD was purchased from Synergy Scientific Services (Catalog number: 706002), and the procedure is followed according to the manufacturer's protocol. The tissue was homogenized in 5–10 ml of cold 20 mM HEPES buffer, pH 7.2, containing 1 mM EGTA, 210 mM mannitol, and 70 mM sucrose per gram tissue, centrifuged at 1,500 × g for 5 min at 4 °C. The supernatant was removed for assay and stored on ice, and the SOD activity was calculated using the equation obtained from the standard curve's linear regression, substituting the linearized rate for each sample. The following equation was used to quantify the SOD level. One unit is defined as the amount of enzyme needed to exhibit 50% dismutation of the superoxide radical.
Measurement of glutathione peroxidase (GPx)
The Cayman Chemical Assay Kit for GPx was purchased from Everon Life Sciences (Catalog number: 703102), and the procedure was followed according to the manufacturer's protocol. The tissue was homogenized in 5–10 ml of cold buffer (i.e., 50 mM Tris–HCl, pH 7.5, 5 mM EDTA, and 1 mM DTT) per gram tissue and centrifuged at 10,000 × g for 15 min at 4 °C. The supernatant was removed and stored on ice. The reaction rate at 340 nm was determined using the NADPH extinction coefficient of 0.00373 µM-1. One unit is defined as the amount of enzyme that will cause the oxidation of 1.0 nmol of NADPH to NADP + per minute at 25 °C. The following equation measures GPx activity.
Measurement of Advanced oxidation Protein products (AOPP)
AOPP concentrations are expressed as µmol/L of chloramine-T equivalents. AOPP quantified as described by Witko-Sarsat et al.,[31]. The sample was diluted in 1:5 phosphate-buffered saline into each well of a 96-well microplate and added 20 µl of acetic acid to each well. For the standards, 10 µl of 1.16 M potassium iodide was added to 200 µl of chloramine-T solution (0 to 100 µmol/L) in a well and then added 20 µl of acetic acid. The absorbance was immediately read at 340 nm against a blank consisting of 200 µl of phosphate-buffered saline, 10 µl of 1.16 M potassium iodide, and 20 µl of acetic acid.
Estimation of Malondialdehyde (MDA)
The Cayman Chemical Assay Kit for MDA was purchased from Synergy Scientific Services (Catalog number: 10009055), and the procedure is followed according to the manufacturer's protocol. Approximately 25 mg of tissue was weighed into a 1.5 ml centrifuge tube, and 250 μl of RIPA Buffer containing protease inhibitors was added. The tissue was homogenized on ice and centrifuged at 1,600 × g for 10 min at 4 °C. The supernatant was used for analysis. Absorbance was measured at 540 to 530 nm, and the values of MDA were calculated from the given formula.
Measurement of baseline Conjugated Diene (CD) concentration
Baseline CD concentration was measured by the method detailed by Chajes et al. (1996) [32]. The sample was mixed with 0.5 ml of water, and lipids were extracted following the addition of 1.5 ml of chloroform–methanol mixture 2:1 (v/v) with butylated hydroxytoluene (5 mg/100 ml), vortex mixed, further separated by centrifuging for 5 min at 2000 × g (4 °C). The lower layer was evaporated under a stream of nitrogen until dry. The lipid residue was redissolved in 1 ml of cyclohexane, and the absorbance was measured at 234 nm. The results were presented as relative optical density units (OD 234).
Quantification of 8-IPG-F2α
The Cayman Chemical ELISA Kit for 8-IPG-F2α was purchased from Everon Life Sciences (Catalog number: 516351), and the procedure is followed according to the manufacturer's protocol. 1 ml of Homogenization Buffer (0.1 M phosphate buffer, pH 7.4 containing 1 mM EDTA and 0.005% BHT) was added per 100 mg of tissue. The sample was homogenized and centrifuged at 8,000 × g to pellet particulate matter for ten minutes; the supernatant was transferred to a clean tube. Before the assay, sample purification was done using solid-phase extraction purchased from Phenomenex. Strata C18-E, reverse phase, silica-based with a sorbent mass of 200 mg was used. The absorbance of samples and standards was measured at the 420-405 nm wavelengths.
Statistical Analysis
Statistical analysis was carried out with Graph Pad Prism 7 software. The Shapiro–Wilk test was used to find the normality distribution, and logarithmic transformation was done when needed. The Student's t-test was used to find the differences between the means of the two continuous variables, and Pearson's Chi-square test compared the categorical variables. Data are expressed as mean with standard deviation for continuous variables, and number (percentage) for categorical variables and p-value < 0.05 were considered statistically significant.
Results
Demographical and clinical characteristics
The demographic data and clinical characteristics of the two study groups are represented in Table 1. The mean age was similar in both the study groups, and there is a female preponderance in both the study population. The prevalence of females was higher in the diabetic cataract group, and males were dominant in the non-diabetic cataract group. The average mean wet weight of lens was higher in diabetic cataract lenses. As expected, random blood sugar was significantly higher in the diabetic cataract group. Most of the diabetic cataract patient lenses were dark brown and light brown, whereas the non-diabetic group had a light brown color.
Activity of antioxidative enzymes in lenses and aqueous humour
The activity of SOD and GPx of cataract lenses is represented in Table 2. In the study group, significantly lower superoxide dismutase and glutathione peroxidase activity was observed in the lenses of diabetes compared to the control group.
The activity of SOD and GPx of aqueous humor is represented in Table 2. In aqueous humor, the SOD and GPx activity was significantly decreased in diabetic cataracts compared to non-diabetic cataract patients.
Concentration of advanced oxidation protein products in lens and aqueous humour
The level of AOPP in lens and Aqueous humor was represented in Table 2. The concentration of AOPP was significantly higher in the lenses of cataract patients with diabetes. In parallel to lens AOPP concentration, the aqueous humor levels in diabetic cataracts were significantly increased compared to the non-diabetic cataract patients.
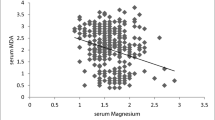
Levels of lipid peroxidation products (malondialdehyde, conjugated diene, and 8-isoprostaglandin-f2α) in lens and aqueous humour
The estimation of MDA and CD in lenses was represented in Table 2. The concentration of MDA and CD was significantly higher in the lenses of cataract patients with diabetes than in the control group.
The estimation of MDA and CD in Aqueous humor are represented in Table 2. The concentration of MDA and CD was significantly increased in cataract patients with diabetes compared to the control group.
The estimation of 8-IPG-F2α in lenses and Aqueous humor are represented in Table 2. In contrast to the control group, the concentration of 8-IPG-F2α was significantly higher in both the lenses and aqueous humor of cataract patients with diabetes.
Discussion
Patients with diabetes mellitus are two to three times more likely to develop cataracts than their non-diabetic counterparts [33]; this risk may reach 15–25 times in people with diabetes less than 40 years of age. [34] Even impaired fasting glucose (IFG), a pre-diabetic condition, has been considered a risk factor for developing cortical cataracts [35].
Oxidative stress is assumed to play a significant role in cataract formation and diabetic complications. The glycometabolic imbalance is a vital cataractogenic aspect in people with diabetes. Several pathogenetic mechanisms have been projected to elucidate the accelerated cataractogenesis in diabetes. These mechanisms include the increased glycation and browning of lens crystallins and increased sorbitol-pathway activity [36]
The standard lens is fully equipped with antioxidants to endeavor against oxidative stress, and it has been well recognized that free radicals damage proteins, lipids, and DNA under oxidative stress. Enzymatic antioxidants, namely SOD and GPx, battle the toxic effects of reactive oxygen species [37]. SOD activity was considerably decreased in lenses of diabetes patients, which supports the previous study done by Ozmen B et al. (2002) [38], which suggests that decreased SOD activity occurs as a result of glycation due to hyperglycemia[39] Concurrently in aqueous humor, we have found decreased SOD activity in DM patients.
Glutathione (GSH), identified to react with glycation mixture extensively, prevents the formation of sugar-mediated protein–protein cross-linking in vitro. While GSH is the primary substrate of the enzyme GPx, the enzyme activity may be reduced in the lenses of diabetes patients. The results of our study revealed a significant decrease in glutathione peroxidase level in diabetic cataract lenses and aqueous humor in contrast to non-diabetic cataracts. These results are consistent with the previous study by Emre et al. [40], (2010). At the same time, GPx inactivates the H2O2 (well-known ROS), which is usually present in aqueous humor. The lens becomes more vulnerable to oxidative injury in the presence of pentose phosphate pathway deficiency [41]. In case of any oxidative stress, the pentose phosphate pathway is proficient at amplifying the nicotinamide adenine dinucleotide phosphate (NADPH) supply, which the GSH protective system needs. GPx reduces the oxidative damage at a cellular level caused under physiological conditions [42], and it can fight the toxic effects of hydroperoxides [43]. Further decrease in SOD level increases the superoxide radicals (O2‾), inactivating the enzyme GPx [44].
Our results are reliable with the previous study reports, and the exact mechanism can be implied. Inactivation of SOD and GPx enzymes may result in an elevation of the H2O2 and O2‾ levels in the lens, which may be accountable for the oxidative alteration of lens protein. These results additionally support the idea that the inactivation of antioxidative enzymes may be significant for the progress of diabetic complications [42, 45].
Elevated protein oxidation markers have been linked with cataractogenesis [46]. Increased AOPP in diabetic cataract patients supports the idea that the frequency of protein damage is higher in cataract patients with diabetes than those without diabetes. These products may promote the progression of microvascular damage in diabetes and alter the blood-ocular barrier. An increase in AOPP is also due to glucose oxidation and non-enzymatic glycation of proteins in diabetic patients. In our study, increased AOPP was observed in both lens and aqueous humor of diabetic patients compared to senile cataracts. The result supports the previous study done in serum by Yildrim et al. (2009) [47]. Higher concentrations of AOPP have been observed in diabetes and intensified by the glycoxidation process and oxidant-antioxidant imbalance. Concurrently AOPP has also been increased in the aqueous humor of hyperglycemic rabbits [48]. There is a prospect of leakage of protein adducts from the lens into the aqueous humor, increasing the level in diabetes cataract patients.
Lipid peroxidation is increased in diabetes. Malondialdehyde, the breakdown product of polyunsaturated fatty acids under peroxidation conditions, is the standard marker for lipid peroxidation and has been significantly increased in diabetic cataract lenses. The reason may be hypothesized that there is overproduction of oxidants in the lens in a hyperglycemic state due to glucose oxidation. MDA levels in diabetic cataracts significantly increased compared to non-diabetic cataracts in both lens and aqueous humor. Hashim et al. (2006) [49, 50] demonstrated a higher MDA level in the lenses and plasma of diabetic patients than in non-diabetic cataract patients. Simultaneously, Donma et al. (2002) [51] showed an increased MDA level in the lenses of diabetic cataract group when compared to non-diabetic cataract groups, which are concurrent with our study corroborated the confirmation of a role for free radical-induced lipid peroxidative damage in the pathomechanism of diabetic cataract. Studies recommend that high blood levels of MDA in patients with diabetes reflect similar increases at the aqueous humor level. Costagliola et al. (1988) [52] established that MDA levels in the lenses of patients with diabetes were approximately twice as high as controls.
Many studies have found a distinct accumulation of conjugated diene in the lenses of cataract patients. Babizhayav (1989) [53] and Chang et al. (2013) [54] have reported elevated accumulation of conjugated diene in the lenses and serum of cataract patients, respectively. CD levels were high in the early progressive stage of cataract, and this diene act as an initiating factor that later propagates and affects the lens [55]. In our study, the levels of CD were found to be higher in diabetic cataracts than senile cataracts in both samples lens and aqueous humor. Mooradian D (1991) [58], in a study on diabetes mellitus, determined that CD may have a pathogenetic role in diabetes-related difficulties. The excess of glucose causes overproduction of oxidants in the lens, mainly in auto-oxidative reactions and overloaded mitochondria [56], and intensifies the Lipid peroxidation as confirmed by higher levels of conjugated diene [57].
F2-isoprostanes are prostaglandin derivatives, and these are formed by free-radical-catalyzed peroxidation of arachidonic acid, which resides on the cell membrane of phospholipids. These compounds are bioactive and may be accountable for the unfavorable effects of oxidative stress. 8-IPG-F2α is a primary F2- isoprostane; presently, it is one of the most reliable in vivo lipid peroxidation and oxidative stress [59]. Levels of isoprostanes have an extensive daily difference in their secretion in plasma, creatinine, and aqueous humor in humans. These compounds are found in augmented concentrations in different pathophysiological states [60].
The current study revealed that the levels of 8-IPG-F2α were significantly increased in the diabetic cataract patients as contrasted to non-diabetic cataract patients in both lens and aqueous humor due to the interaction of the polyol pathway with other metabolic pathways resulting in an increase in the enzyme Phospholipase A2 and further damage to lens structures. Due to phagocytic changes in hyper mature cataracts, there is a leakage from the lens to aqueous humor leading to the increased production of 8-IPG-F2α in diabetic cataract subjects. These results corroborate the evidence of a role for free radical encouraged lipid peroxidative damage in the pathophysiology of diabetic cataracts. It is in harmony with the study performed by Montuschi et al. [61], in which it was revealed that the mean concentration of 8-IPG-F2α in aqueous humor from patients with exfoliation syndrome and cataracts was approximately five times higher than that deliberated in the aqueous humor from control cataract patients.
The ability of 8-IPG-F2α to alter the integrity of neurotransmitter pools contributes pathways and new potential target sites for the treatment of degenerative ocular diseases. Isoprostanes can elicit both inhibitory and excitatory effects on norepinephrine (NE) release from sympathetic nerves in isolated mammalian iris ciliary bodies, and its effect is blocked by the thromboxane receptor (TP) antagonist SQ-29548, considering that TP receptors mediate the mechanisms of 8-IPG-F2α [62]. In contrast, isoprostanes attenuate dopamine release from the in-vitro mammalian neural retina, suggesting that these novel arachidonic acid metabolites exhibit a biphasic regulatory effect on glutamate release from the retina. They can regulate amino acid neurotransmitter metabolism without inducing cell death in the retina [63].
Diabetes mellitus considerably impacts the cornea's metabolic, morphological, physiological, and clinical properties. The corneal abnormalities, generally termed diabetic keratopathy, are present in more than 70% of diabetic patients [64] and include clinically detectable changes such as increased epithelial fragility and recurrent erosions [65], reduced corneal sensitivity,[66,67,68,69], increased autofluorescence, [70] impaired wound healing [71], altered epithelial and endothelial barrier functions [72], and predisposition to corneal edema [73] and infectious ulcers [65,66,67,68].
It has been reported that a higher percentage of cortical opacities in people with diabetes in contrast to non-diabetic as documented by Scheimpflug photography and densitometric analysis [74]. It has been found that a twofold higher incidence of cortical cataracts in subjects with diabetes mellitus over five years and posterior subcapsular cataracts were more frequent in diabetic patients [35].
Hyperglycemia is the main reason for transient refractive changes in diabetic patients. The refractive changes observed during periods of unstable blood sugar are related to both morphologic and functional changes in the crystalline lens [75].
In our study, the Superoxide dismutase and Glutathione Peroxidase activity were significantly reduced in diabetic patients compared to non-diabetic patients in both lenses and aqueous humor. Malondialdehyde, Conjugated Diene, and 8-IPG-F2α levels significantly increased in diabetic patients compared to non-diabetic, and advanced oxidation protein product levels also significantly increased in diabetic patients compared to non-diabetics in both lenses and aqueous humor. The current study suggested that oxidative stress and Lipid per-oxidation have an imperative role in the diabetic-related complication, specifically in the lens, may have a responsibility in the pathomechanism of early onset of cataracts coupled with diabetes mellitus.
The study's main limitation is that a cataract-free control group is not included, which limits the study of the pathomechanism of senile cataracts in diabetic patients. This current study only included cataract patients with age group ≥ 40 years. So there may be a chance to avoid limitations for the early onset of diabetic cataracts.
Conclusion
In conclusion, our findings specify that free radical action jointly with a depleted antioxidant defense system may represent significant molecular mechanisms in developing diabetic cataracts. Future research is necessary to advance understanding these mechanisms to clarify the pathogenesis of diabetic cataracts as the first step towards developing precise treatment approaches in the future.
Data availability statement
The data supporting this study's findings are available from the corresponding author upon reasonable request.
References
Baynes JW, Thorpe SR. Role of oxidative stress in diabetic complications: a new perspective on an old paradigm. Diabetes. 1999;48(1):1–9.
Thylefors B, Négrel AD, Pararajasegaram R, Dadzie KY. Global data on blindness. Bull World Health Organ. 1995;73(1):115.
Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol. 2012;96(5):614–8.
Bourne RR, Stevens GA, White RA, Smith JL, Flaxman SR, Price H, Pesudovs K. Causes of vision loss worldwide, 1990–2010: a systematic analysis. Lancet Glob Health. 2013;1(6):e339–49.
Babizhayev MA, Deyev AI, Linberg LF. Lipid peroxidation as a possible cause of cataract. Mech Ageing Dev. 1988;44:69–89.
Inomata M, Hayashi M, Shumiya S, Kawashima S, Ito Y. Involvement of inducible nitric oxide synthase in cataract formation in Shumiya cataract rat (SCR). Curr Eye Res. 2001;23:307–11.
Varma SD, Ets TK, Richards RD. Protection against superoxide radicals in rat lens. Ophthalmol Res. 1977;9:875–80.
Bhuyan KC, Bhuyan DK. Catalase in ocular tissue and its intracellular distribution in corneal epithelium. Am J Ophthalmol. 1970;69:147–53.
Pirie A. Glutathione peroxidase in lens and a source of hydrogen peroxide in aqueous humour. Biochem J. 1965;96:244–53.
Rao GN, Sadasivudu B, Cotlier E. Studies on glutathione S-transferase, glutathione peroxidase and glutathione reductase in human normal and cataractous lenses. Ophthalmic Res. 1983;15:173–9.
Yegorova S, Yegorov O, Lou MF. Thioredoxin induced antioxidant gene expressions in human lens epithelial cells. Exp Eye Res. 2006;83:783–92.
Giblin FJ. Glutathione: a vital lens antioxidant. J Ocul Pharmacol Ther. 2000;16:121–35.
Heath H. The distribution and possible functions of ascorbic acid in the eye. Exp Eye Res. 1962;1:362–7.
Jacques PF, Hartz SC, Chylack LT Jr, McGandy RB, Sadowski JA. Nutritional status in persons with and without senile cataract: blood vitamin and mineral levels. Am J Clin Nutr. 1988;48:152–8.
Yeum KJ, Taylor A, Tang G, Russell RM. Measurement of carotenoids, retinoids, and tocopherols in human lenses. Invest Ophthalmol Vis Sci. 1995;36:2756–61.
Bernstein PS, Khachik F, Carvalho LS, Muir GJ, Zhao DY. Katz NB Identification and quantitation of carotenoids and their metabolites in the tissues of the human eye. Exp Eye Res. 2001;72:215–23.
Kisic B, Miric D, Zoric L, Ilic A, Dragojevic I. Antioxidant capacity of lenses with age-related cataract. Oxid Med Cell Longev. 2012;2012:467130.
Stamenkovic M, Radic T, Stefanovic I, Coric V, Sencanic I, Pljesa-Ercegovac M, et al. Glutathione S transferase omega-2 polymorphism-Asn142Asp modifies the risk of age related cataract in smokers and subjects exposed to ultraviolet irradiation. Clin Exp Ophthalmol. 2014;42:277–83.
Resnikoff S, Pascolini D, Etya’Ale D, Kocur I, Pararajasegaram R, Pokharel GP, Mariotti SP. Global data on visual impairment in the year 2002. Bull World Health Organ. 2004;82:844–51.
Murthy GVS, Gupta SK, John N, Vashist P. Current status of cataract blindness and Vision 2020: the right to sight initiative in India. Indian J Ophthalmol. 2008;56(6):489.
Diagnosis ADA, Classification of Diabetes Mellitus,. Oxidative stress is recognized as one of the major contributors to the increased risk of several diseases. Diabetes Care. 2006;29(Suppl 1):S43–8.
Aksoy H, Keles S, Kocer I, Akcay F. Diabetic cataract and the total antioxidant status in aqueous humor. Clin Chem Lab Med. 2001;39(2):143–5.
Klein R, Klein BE, Moss SE. Visual impairment in diabetes. Ophthalmology. 1984;91(1):1–9.
Kim SI, Kim SJ. Prevalence and risk factors for cataracts in persons with type 2 diabetes mellitus. Korean J Ophthalmol. 2006;20(4):201–4.
Arnold AC. Basic Principles of Ophthalmic Surgery. USA: American Academy of Ophthalmology; 2006.
World Health Organization. Global initiative for elimination of avoidable blindness. World Health Organization; 2000.
Taylor HR, Vu HT, Keeffe JE. Visual acuity thresholds for cataract surgery and the changing Australian population. Arch Ophthalmol. 2006;124(12):1750–3.
Behndig A, Montan P, Stenevi U, Kugelberg M, Lundström M. One million cataract surgeries: Swedish National Cataract Register 1992–2009. J Cataract Refract Surg. 2011;37(8):1539–45.
Gollogly HE, Hodge DO, Sauver JL, Erie JC. Increasing incidence of cataract surgery: population-based study. Journal of Cataract & Refractive Surgery. 2013;39(9):1383–9.
Chan E, Mahroo OA, Spalton DJ. Complications of cataract surgery. Clin Exp Optom. 2010;93:379–89.
Witko-Sarsat V, Friedlander M, Capeillère-Blandin C, Nguyen-Khoa T, Nguyen AT, Zingraff J, Descamps-Latscha B. Advanced oxidation protein products as a novel marker of oxidative stress in uremia. Kidney Int. 1996;49(5):1304–13.
Chajès V, Sattler W, Stultschnig M, Kostner GM. Photometric evaluation of lipid peroxidation products in human plasma and copper oxidized low density lipoproteins: correlation of different oxidation parameters. Atherosclerosis. 1996;121(2):193–203.
Klein BE, Klein R, Moss SE. Incidence of cataract surgery in the Wisconsin Epidemiologic Study of Diabetic Retinopathy. Am J Ophthalmol. 1995;119:295–300.
Bernth-Peterson P, Bach E. Epidemiologic aspects of cataract surgery. Frequencies of diabetes and glaucoma in a cataract population. Acta Ophthalmol. 1983;61:406–16.
Saxena S, Mitchell P, Rochtchina E. Five-year incidence of cataract in older persons with diabetes and pre-diabetes. Ophthalm Epid. 2004;11:271–7.
Lyons TJ, Silvestri G, Dunn JA, Dyer DG, Baynes JW. Role of glycation in modification of lens crytallins in diabetic and nondiabetic senile cataract. Diabetes. 1991;40:1010–5.
Obara Y. The oxidative stress in the cataract formation. Nippon Ganka Gakkai Zasshi. 1995;99(12):1303–41.
Özmen B, Özmen D, Erkin E, Güner İ, Habif S, Bayındır O. Lens superoxide dismutase and catalase activities in diabetic cataract. Clin Biochem. 2002;35(1):69–72.
Kowluru RA, Chan PS. Oxidative stress and diabetic retinopathy. Exp Diabetes Res. 2007;4:43603.
Emre S, Ateş B, Taşar A, Doğanay S. Lens Capsular Glutathione Level and Glutathione Peroxidase Activity Among Diabetic Patients. Journal of Inonu University Medical Faculty. 2010;15(3):139–43.
Ganea E, Harding JJ. Glutathione-related enzymes and the eye. Curr Eye Res. 2006;31(1):1–11.
Harding JJ. Free and protein-bound glutathione in normal and cataractous human lenses. Biochemical Journal. 1970;117(5):957–60.
Giblin FJ, Reddan JR, Schrimscher L, Dziedzic DC, Reddy VN. The relative roles of the glutathione redox cycle and catalase in the detoxification of H2O2 by cultured rabbit lens epithelial cells. Exp Eye Res. 1990;50(6):795–804.
Blum J, Fridovich I. Inactivation of glutathione peroxidase by superoxide radical. Arch Biochem Biophys. 1985;240(2):500–8.
Mileva M, Bakalova R, Zlateva G. Low-intensity laser irradiation does not affect the oxidative stress in experimental cataract. Med Laser Appl. 2004;19(3):150–4.
Garland D. Role of site-specific, metal-catalyzed oxidation in lens aging and cataract: a hypothesis. Exp Eye Res. 1990;50(6):677–82.
Yildirim Z, Yildirim F, Ucgun NI, Kilic N. The evaluation of the oxidative stress parameters in nondiabetic and diabetic senile cataract patients. Biol Trace Elem Res. 2009;128(2):135.
Gumieniczek A, Owczarek B, Pawlikowska B. Oxidative/nitrosative stress and protein damages in aqueous humor of hyperglycemic rabbits: effects of two oral antidiabetics, pioglitazone and repaglinide. Exp Diabetes Res. 2012;2012.
Kesavulu MM, Giri R, Rao K, Apparao CH. Lipid peroxidation and antioxidant enzyme levels in type 2 diabetics with microvascular complications. Diabetes & Metabolism. 2000;26(5):387–92.
Hashim Z, Zarina S. Antioxidant markers in human senile and diabetic cataractous lenses. J Coll Physicians Surg Pak. 2006;16(10):637–40.
Donma O, Yorulmaz EÖ, Pekel H, Suyugül N. Blood and lens lipid peroxidation and antioxidant status in normal individuals, senile and diabetic cataractous patients. Curr Eye Res. 2002;25(1):9–16.
Costagliola C, Iuliano G, Menzione M, Nesti A, Simonelli F, Rinaldi E. Systemic human diseases as oxidative risk factors in cataractogenesis. Ophthalmic Res. 1988;20(5):308–16.
Babizhayev MA. Accumulation of lipid peroxidation products in human cataracts. Acta Ophthalmol. 1989;67(3):281–7.
Chang D, Zhang X, Rong S, Sha Q, Liu P, Han T, Pan H. Serum antioxidative enzymes levels and oxidative stress products in age-related cataract patients. Oxidative Med Cell Longev. 2013;2013.
Kisic B, Miric D, Zoric L, Ilic A. Role of lipid peroxidation in the pathogenesis of age-related cataract. InLipid peroxidation 2012 Aug 29. IntechOpen.
Kyselova Z, Stefek M, Bauer V. Pharmacological prevention of diabetic cataract. J Diabetes Complicat. 2004;18:129–40.
Miric DJ, Kisic BB, Zoric LD, Mitic RV, Miric BM, Dragojevic IM. Xanthine oxidase and lens oxidative stress markers in diabetic and senile cataract patients. J Diabetes Complications. 2013;27(2):171–6.
Mooradian AD. Increased serum conjugated dienes in elderly diabetic patients. J Am Geriatr Soc. 1991;39(6):571–4.
Basu S. F2-isoprostanes in human health and diseases: from molecular mechanisms to clinical implications. Antioxid Redox Signal. 2008;10:1405–34.
Basu S, Helmersson J. Factors regulating isoprostane formation in vivo. Antioxid Redox Signal. 2005;7(1–2):221–35.
Montuschi P, Barnes PJ, Roberts LJ. Isoprostanes: markers and mediators of oxidative stress. FASEB J. 2004;18:1791–800.
Awe SO, Opere CA, Harris LC, Uketui AJ, Ohia SE. Effect of isoprostanes on sympathetic neurotransmission in the human isolated iris-ciliary body. Neurochem Res. 2000;25:491–6. https://doi.org/10.1023/A:1007560025570.
Njie-Mbye YF, Chitnis MK, Opere CA, Ohia SE. Lipid peroxidation: pathophysiological and pharmacological implications in the eye. Front Physiol. 2013;4:366.
Didenko TN, Smoliakova GP, Sorokin EL, Egorov VV. Clinical and pathogenetic features of neurotrophic corneal disorders in diabetes. Vestn Oftalmol. 1999;115:7–11.
Saini JS, Khandalavla B. Corneal epithelial fragility in diabetes mellitus. Can J Ophthalmol. 1995;30:142–6.
Sanchez-Thorin JC. The cornea in diabetes mellitus. Int Ophthalmol Clin. 1998;38:19–36.
Herse PR. A review of manifestations of diabetes mellitus in the anterior eye and cornea. Am J Optom Physiol Opt. 1988;65:224–30.
McNamara NA, Brand RJ, Polse KA, Bourne WM. Corneal function during normal and high serum glucose levels in diabetes. Invest Ophthalmol Vis Sci. 1998;39:3–17.
Touzeau O, Levet L, Borderie V, Bouchard P, Laroche L. Anterior segment of the eye and diabetes mellitus. J Fr Ophthalmol. 2004;27:859–70.
Stolwijk TR, van Best JA, Oosterhuis JA, Swart W. Corneal autofluorescence, an indicator of diabetic retinopathy. Invest Ophthalmol Vis Sci. 1992;33:92–7.
Schultz RO, Van Horn DL, Peters MA, Klewin KM, Schutten WH. Diabetic keratopathy. Trans Am Ophthalmol Soc. 1981;79:180–99.
Gekka M, Miyata K, Nagai Y, Nemoto S, Sameshima T, Tanabe T, et al. Corneal epithelialbarrier function in diabetic patients. Cornea. 2004;23:35–7.
Saini JS, Mittal S. In vivo assessment of corneal endothelial function in diabetes mellitus. Arch Ophthalmol. 1996;114:649–53.
Schäfer C, Lautenschläger C, Struck HG. Cataract types in diabetics and non-diabetics: a densitometric study with the Topcon-Scheimpflug camera. Klin Monatsbl Augenheilkd. 2006;223:589–92.
Saito Y, Ohmi G, Kinoshita S, Nakamura Y, Ogawa K, Harino S, et al. Transient hyperopia with lens swelling at initial therapy in diabetes. Br J Ophthalmol. 1993;77:145–8.
Funding
The author(s) received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Govindaswamy, S., C, U.R. & Prabhakar, S. Evaluation of antioxidative enzymes levels and lipid peroxidation products levels in diabetic and non diabetic senile cataract patients. J Diabetes Metab Disord 21, 697–705 (2022). https://doi.org/10.1007/s40200-022-01033-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-022-01033-z