Abstract
Background
Obesity is a complicated phenomenon which is a combination of genetic, environmental, and psychological factors. Genetic factors of obesity play an important role in individual risk. It is well known that obese children have disturbed puberty timing. To the best of our knowledge, no study has been performed to investigate the association between MC4R gene mutation and puberty timing.
Methods
This study was performed as a cross-sectional study evaluating the near MC4R rs17782313 variation in 60 obese children and 98 healthy non obese children. Weight, height, BMI ( Body Mass Index ), BMI z-score (BMIz), family history of diabetes mellitus and obesity, the age of the obesity onset, overeating behavior, type of obesity (central or general) and puberty stage were evaluated in 60 obese children.
Results
The average age of the participants was 14.87 (+/- 1.3) years, with average weight and BMI of 90.77 (+/-12.2) Kg and 31.72 (+/-4.35) Kg/m2, respectively. Compared to healthy non obese patients, those with C-T genotype (C-T Vs. T-T and C-C) had higher odds of obesity than those with T-T and C-C genotype (p < 0.0001) while genotype TT showed significant protective effect (p = 0.0007). The heterozygote individuals (CT) have a higher BMIz than homozygote ones (CC and TT) (2.8 vs. 2.5 Kg/m2, p = 0.04).
Conclusions
children with CT genotype have 5.1 increased risk of obesity. While genotype TT showed significant obesity protective effect. We did not find association of this polymorphism with either childhood eating disorders or puberty. It is recommended to perform a cohort study in a larger sample.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is a complicated phenomenon with the contribution of all genetic, environmental, and psychological factors. Excessive calorie intake and insufficient physical activity are important factors involved in obesity; however, the role of genetic elements is gaining much attention recently [1]. The environment, diet, and physical activity cause the gene to be expressed; furthermore, genes affect the dietary and food choose habit [2]. Genetic factors of obesity play an important role in individual risk [3]. Children obesity has a growing incidence; in 2013, the estimated rate of obese or overweight children was 43 million, which has been reached over 60 million in 2020 [4].
Like other developing countries, the prevalence of childhood obesity is increasing in Iran [5, 6]. Genome-wide association studies (GWAS) are performed to determine the associated genetic variants with obesity [1]. These findings imply that obesity-related genes affect energy intake and expenditure [7]. Working on mammals, Doulla et al[8], El-Sabrout [9], and Aykut et al[10] found that Melanocortin 4 receptor (MC4R), a protein produced by the MC4R gene, can control appetite and satiety, as well as affect feeding intake, body weight, and sexual desire behavior in humans and rabbits. Furthermore, MC4R gene variants have been associated to inherited human obesity[11].
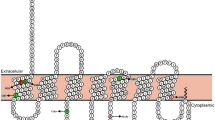
MC4R protein that produced by MC4R gene is a member of G protein coupled receptors in some region of brain such as hypothalamus.[12]. MC4R is a component of the leptin system, expressing in the central nervous system, including the hypothalamus, cerebral cortex, brain stem, and spinal cord [13]. This 332-amino-acid receptor is encoded by a single exon on the 18q22 chromosome [14]. MC4R mutations are associated with energy hemostasis perturbation, food intake, metabolic rate, and weight gain [15].
Single nucleotide polymorphisms (SNPs) near the MC4R gene (including rs17782313, rs571312, rs17700144 and rs2331842) have a strong association with obesity, regardless of age [16]. The MC4R rs17782313 variant has been indicated to be more frequent than other variants associated with obesity [7]. We have previously indicated the association of childhood obesity with puberty timing perturbations [17]. To the best of our knowledge, no study has been performed to investigate the association between MC4R gene mutation and puberty timing. The objective of this study is to evaluate the relationship between MC4R rs17782313 variant and Body mass index (BMI), and delayed or early puberty in boys and girls.
Materials and methods
Study design and data collection
This study was performed as a cross-sectional study evaluating the MC4R rs17782313 variation in 60 children with obesity ( with age mean : 14.87 and weight mean : 90.77, 26 person was female ) and 98 healthy subjects with Body mass index (BMI) of less than 25 kg/m2. Weight, height, BMI, BMI z-score (BMIz), birth weight, family history of diabetes mellitus and obesity, the age of the obesity onset, presence of overeating behavior (including bulimia, excessive hunger and night eating), type of obesity (central or general) and puberty stage were evaluated in 60 obese children. Children with a positive past medical history for all type of disease, positive drug history, and positive family history of delayed or early puberty were excluded from the study. Central obesity was considered as abdominal obesity, while general obesity was considered as truncal obesity [18]. For children whose puberty was initiated, the stage of puberty, based on the Tanner staging [19], was recorded. The presence of breast buds in girls and penile and testicular changes (> 2.5 cm testicular length or > 4ml testicular volume) in boys are considered as the signs of puberty initiation. The presence of breast buds before eight and after 13 years of age was considered as the early and delayed puberty in girls respectively. The presence of penile and testicular size change before nine years, and after 14 years of age was considered early and delayed puberty in boys respectively. All examinations were performed by a single experienced pediatric endocrinologist.
Genetic analysis of the MC4R gene
DNA isolation : Genomic DNA was extracted from peripheral blood leukocytes by the phenol-chloroform method. The DNA concentration was determined using a nanodrop at a wavelength of 260 nm. All DNA templates were adjusted to 50 ng/µL concentration. The DNA samples were stored at ‑80˚C until required for genotyping.
PCR amplification was performed in a volume of 20 µL reaction the mixture containing 7 µL Red Master Mix (2X) (Thermo Scientific), 1 µL of the genomic DNA, 0.5 µL for each 10 pmol/ul primer, The region encompassing MC4R gene were amplified by PCR with following primers, MC4R; Forward primer: 5′-AAGTTCTACCTACCATGTTCTTGG-3′ Reverse primer: 5′-TTCCCCCTGAAGCTTTTCTTGTCATT-3′ (Amplicon size: 137 bp).
The PCR cycle included an initial DNA denaturation for MC4R at 95 °C for 5 min, followed by 29 cycles of DNA denaturation at 95 °C for 30 s, annealing at melting temperature (TM) set for 30 s, extension at 72 °C for 10 min, and a final extension period of 5 min at 72 °C.
All PCR products were visualized on 2% agarose gel electrophoresis.
Restriction endonuclease digestion was carried out in a 10 µL reaction solution for rs17782313 (MC4R) polymorphism containing, 3 µL of PCR products, 3.5 µL of distilled water, 1 µL of the 10X Buffer G, and 2.5 µL of BclI enzyme (Thermo Fisher) (Waltham, Massachusetts, United States) Incubate at 55 °C for 1 h. Mutant genotype (CC), heterozygote genotype (CT), and wild genotype (TT) consisted of fragments (137 bp), (137, 107 bp), and (107 bp) respectively. All digested fragments were analyzed by 3% agarose gel electrophoresis and viewed with UV transillumination.
Ethical considerations
The study protocol has been approved by the ethical committee of our institution- Tehran University of Medical Sciences (approval number: IRTUMSVCRCC.1397.284). Full written informed consent was obtained from all parents before recruitment in the study.
Statistical analysis
All data were analyzed using SPSS version 22. Descriptive analyses were expressed as mean (+/- standard deviation) and number (percent). The t-test was used for normally distributed variables; otherwise, the Mann- Whitney was used. The chi-square tests and odds ratios (OR) were used to compare the proportions of the group in different part. The p-value below 0.05 was considered statistically significant.
Results
Sixty obese children were enrolled in the current study. The average age of the participants in obese group was 14.87 (± 1.3) years, with an average weight and BMI of 90.77 (± 12.2) Kg and 31.72 (± 4.35) Kg/m2, respectively. The BMIz ranged from 1.8 to 5.3, with an average of 2.7 (± 0.57). Twenty-six (43.3%) were female. The average birth weight of the participants was 3380.19 (± 479.75) g. Parental consanguinity was positive for 16 (6.7%) children. Positive family history of obesity and diabetes mellitus was found in 50 (83.3%) and 34 (56.7%) individuals. The age of obesity onset was 5–10 years in 34(56.7%) (Table 1). Six (10%) children had abnormal puberty timing (5 had delayed, and one had early-onset puberty). Forty-five (75%) had a history of overeating behavior, and 56 (93.3%) had general, and 4 (6.7%) had central obesity.
The genetic evaluations were done for all enrolled participants (sixty children with obesity, 98 healthy subjects with less than 25 kg/m2 as controls that came for routine evaluations). The age, gender, and other clinical characteristics were not significantly different between cases and controls (P > 0.05). Chi-square analysis for genotype frequency differences between cases and controls showed significant differences (P = 0.003). Compared to healthy patients, those with C-T genotype (C-T Vs. T-T and C-C) had higher odds of obesity than those with T-T and C-C genotype (p < 0.0001, OR = 5.1, 95% CI: 3.2–11.0); While genotype TT showed significant protective effect (p = 0.0007, OR; 0.28, 95%CI = 0.12–0.62) (Table 2). None of the overeating behaviors (excessive hungry, bulimia, and night eating) were associated with the MC4R rs17782313 variants (P > 0.05). There was also no correlation between MC4R rs17782313 variants and birth weight (p = 0.985). The heterozygote individuals (CT) have a higher BMIz than homozygote ones (CC and TT) (2.8 vs. 2.5 Kg/m2, p = 0.04).
There was no difference between obese males and females regarding the early puberty (p-value = 0.098) but delayed puberty was significantly higher among obese males (p-value = 0.029). Early and delayed puberty was not significantly different between obese children (p = 0.678, 0.305). The genetic condition (CC, TT, and CT) was not correlated with early (p = 0.427) or delayed puberty (p = 0.462). The presence of the T allele could not predict the occurrence of early (p = 0.502) or delayed puberty (p = 0.281), as same as the C allele (p = 0.464, 0.095). The genotype of C-T could not predict the occurrence of early (p = 0.284) and delayed puberty (p = 0.875); The genotype of C-C and C-T could not also predict the occurrence of either early (p = 0.464) and delayed puberty (p = 0.095). Normal or abnormal puberty stage was not associated with the presence of T allele (p = 0.590), C allele (p = 0.320), CT genotype (p = 0.320), and CC plus TT genotype (p = 0.689).
Discussion
This study was performed to assess the association between genetic mutations and puberty onset. The results of the current study indicate that subjects with the CT genotype are at an increased risk of early-onset obesity. We found no association between abnormal eating behaviors and MC4R rs17782313 variants. There was also no correlation between the MC4R rs17782313 variant and delayed or early puberty.
Previous studies have demonstrated that the common variants near the MC4R are associated with increased risk of obesity;[17, 18] nevertheless, the mechanism of these variants is not fully understood. Metabolic and eating disorders, such as hyperphagia and increased fat intake, have been shown to be associated with MC4R deficiency by some animal studies [20, 21]. Qi et al. showed that the MC4R C allele is associated with higher energy, fat, and protein intake; interestingly, they also found that the MC4R rs17782313 variant is associated with higher BMI independent of the dietary intake [22]. The MC4R rs17782313 polymorphism is associated significantly with childhood obesity in European countries [23]. The MC4R variations are associated with higher BMI [7, 24]. The BMI in individuals with risk allele (CC or CT) was higher compared to others without risk allele (TT). Despite their results, Asian studies done by Hotta et al. [25], Liem et al. [26], Ng et al. [27], and Grant et al. [28] showed no association between the presence of risk allele and BMI. The findings of the current study showed that individuals with CT genotype are at five times higher risk of early-onset obesity; with TT genotype was protective against it. In 2016, Garcia-Solis et al. investigated the MC4R and FTO polymorphism in 580 Mexican children. Obesity was found in 19.1% of these children, and the MC4R risk allele (allele C) was present in 9.8%. They concluded that there is a significant association between MC4R and FTO risk alleles and obesity in children [29]. In line with our findings, Mejía-Benítez et al. found a significant association between MC4R rs17782313 variant and obesity risk in children (OR 1·4; 95% CI 1·06, 1·83) [30]. In 2018, Almeida et al. studied the association between LEPR, FTO, MC4R, and PPARG-2 polymorphisms and obesity in the school-age children. 352 children were evaluated for MC4R rs17782313, they indicated that MC4R rs17782313 is positively associated with obesity, however they declared that this SNP has a very rare contribution in school-age children with obesity [31]. Loose et al. also indicated that the BMI of 8859 7-11-year-old children had a strong positive association with each additional copy of the polymorphic allele [11]. Similar to our findings, Tang et al. in 2017 on a meta-analysis indicated that MC4R rs17782313 increases the childhood obesity risk and the BMIz in different inheritable models [32]. They also concluded that the MC4R rs17782313 T allele causes the promotor hyper methylation and decreased MCR4 expression which contribute to childhood onset obesity [32]; in contrast to the mentioned study, we found that TT genotype is protective against early-onset obesity.
This gene may cause obesity by promoting overeating behaviors; however, Yilmaz et al. found no association between MC4R polymorphism and disordered eating despite a significant association between BMI and MC4R polymorphism [21]. In accordance with the previous study, we did not find a significant association between overeating behavior and the MCR4 rs17782313 variant. Interestingly, in 2016, Park et al. indicated that individuals with MC4R minor alleles have increased intake of fat and decreased intake of fruits, and those with minor alleles had also increased mental stress [16]. However, in contrast to our findings, the association between MCR4 rs17782313 variant and disturbed eating behavior have been shown in Chilean adults and children [33, 34]. Rana et al. evaluated the MCR4 rs17782313 variant in Pakistani females; they reported that females with CT and CC genotype have 1.55 and 2.43 times increased the risk of obesity [35]. We found that children with the CT genotype has 5.1 times increased risk for obesity, which is similar to the previous study. Rana et al. also could not find a significant association between MCR4 rs17782313 variant and obesity-related metabolic, physical, and behavioral characteristics except random eating timings [35]. The similar results of the Rana et al. study and our study could probably be attributed to similar race and genome of people of Pakistan and Iran [35].
It is well known that obesity affects puberty timing via various mechanisms, including increased insulin resistance and hyperinsulinism, hyperandrogenic state, and leptin alteration [17]. In fact, excessive adipose tissue in the childhood period results in growth and pubertal disturbances. Furthermore, the genetics and race is another factor affecting the puberty timing [17]. In the present study, we evaluated the direct association of the puberty timing and the MCR4 rs17782313 variant in 60 Iranian children with obesity. To the best of our knowledge, this is the first study evaluating the MC4R rs17782313 and puberty. The results of our study found no significant association between the MCR4 rs17782313 variant and the occurrence of either early or delayed puberty. The human genome differs from one population to another; therefore, Studies investigating the genetic causes and their associations in different populations help us identify which variant or loci is involved in obesity. In conclusion, children with CT have 5.1 times increased risk of obesity; while those TT have lower risk (OR = 0.28). We did not find the association of this polymorphism with childhood eating disorders and puberty, but performing a cohort study with larger sample size is recommended.
References
Wang J, Mei H, Chen W, Jiang Y, Sun W, Li F, et al. Study of eight GWAS-identified common variants for association with obesity-related indices in Chinese children at puberty. Int J Obes. 2012;36(4):542–7.
Risso DS, Giuliani C, Antinucci M, Morini G, Garagnani P, Tofanelli S, et al. A bio-cultural approach to the study of food choice: The contribution of taste genetics, population and culture. Appetite. 2017;114:240–7.
Cefalu WT, Bray GA, Home PD, Garvey WT, Klein S, Pi-Sunyer FX, et al. Advances in the science, treatment, and prevention of the disease of obesity: reflections from a diabetes care editors’ expert forum. Am Diabetes Assoc; 2015.
Lazopoulou N, Gioka E, Ntalla I, Pervanidou P, Magiakou A-M, Roma-Giannikou E, et al. The combined effect of MC4R and FTO risk alleles on childhood obesity in Greece. Hormones. 2015;14(1):126–33.
Hosseini M, Yousefifard M, Baikpour M, Motlagh ME, Heshmat R, Qorbani M, et al. Age-Period-Cohort Analysis of Abdominal Obesity in Iranian Children and Adolescents: The CASPIAN Study. International Journal of Endocrinology and Metabolism. 2020;18(1).
Jenabi E, Khazaei S. Trends in obesity among iranian children and adolescents: 2000–2016. J Tehran Univ Heart Cent. 2020;15(1):41–2.
Mozafarizadeh M, Mohammadi M, Sadeghi S, Hadizadeh M, Talebzade T, Houshmand M. Evaluation of FTO rs9939609 and MC4R rs17782313 polymorphisms as prognostic biomarkers of obesity: A population-based cross-sectional study. Oman Med J. 2019;34(1):56.
Doulla M, McIntyre AD, Hegele RA, Gallego PH. A novel MC4R mutation associated with childhood-onset obesity: A case report. Paediatr Child Health. 2014;19(10):515–8.
El-Sabrout K, Aggag S. Association of Melanocortin (MC4R) and Myostatin (MSTN) genes with carcass quality in rabbit. Meat Sci. 2018;137:67–70.
Aykut A, Özen S, Gökşen D, Ata A, Onay H, Atik T, et al. Melanocortin 4 receptor (MC4R) gene variants in children and adolescents having familial early-onset obesity: genetic and clinical characteristics. European journal of pediatrics. 2020:1.
Loos RJ, Lindgren CM, Li S, Wheeler E, Zhao JH, Prokopenko I, et al. Common variants near MC4R are associated with fat mass, weight and risk of obesity. Nat Genet. 2008;40(6):768–75.
Hinney A, Volckmar A-L, Knoll N. Melanocortin-4 receptor in energy homeostasis and obesity pathogenesis. Prog Mol Biol Transl Sci. 2013;114:147–91.
Srinivasan S, Lubrano-Berthelier C, Govaerts C, Picard F, Santiago P, Conklin BR, et al. Constitutive activity of the melanocortin-4 receptor is maintained by its N-terminal domain and plays a role in energy homeostasis in humans. J Clin Investig. 2004;114(8):1158–64.
Razquin C, Marti A, Martinez JA. Evidences on three relevant obesogenes: MC4R, FTO and PPARγ. Approaches for personalized nutrition. Mol Nutr Food Res. 2011;55(1):136–49.
Balthasar N, Dalgaard LT, Lee CE, Yu J, Funahashi H, Williams T, et al. Divergence of melanocortin pathways in the control of food intake and energy expenditure. Cell. 2005;123(3):493–505.
Park S, Daily JW, Zhang X, Jin HS, Lee HJ, Lee YH. Interactions with the MC4R rs17782313 variant, mental stress and energy intake and the risk of obesity in Genome Epidemiology Study. Nutr metabolism. 2016;13(1):38.
Mohsenipour R, Abbasi F, Setoodeh A, Sayarifard F, Rostami P, Moinfar Z, et al. Early and delayed puberty among Iranian children with obesity. Minerva Endocrinologica. 2020.
Esmaillzadeh A, Azadbakht L. Major dietary patterns in relation to general obesity and central adiposity among Iranian women. J Nutr. 2008;138(2):358–63.
Tanner JM, Whitehouse RH. Clinical longitudinal standards for height, weight, height velocity, weight velocity, and stages of puberty. Arch Dis Child. 1976;51(3):170–9.
Srisai D, Gillum MP, Panaro BL, Zhang X-M, Kotchabhakdi N, Shulman GI, et al. Characterization of the hyperphagic response to dietary fat in the MC4R knockout mouse. Endocrinology. 2011;152(3):890–902.
Yilmaz Z, Davis C, Loxton NJ, Kaplan AS, Levitan RD, Carter JC, et al. Association between MC4R rs17782313 polymorphism and overeating behaviors. Int J Obes. 2015;39(1):114–20.
Qi L, Kraft P, Hunter DJ, Hu FB. The common obesity variant near MC4R gene is associated with higher intakes of total energy and dietary fat, weight change and diabetes risk in women. Hum Mol Genet. 2008;17(22):3502–8.
Thorleifsson G, Walters GB, Gudbjartsson DF, Steinthorsdottir V, Sulem P, Helgadottir A, et al. Genome-wide association yields new sequence variants at seven loci that associate with measures of obesity. Nat Genet. 2009;41(1):18–24.
Speliotes EK, Willer CJ, Berndt SI, Monda KL, Thorleifsson G, Jackson AU, et al. Association analyses of 249,796 individuals reveal 18 new loci associated with body mass index. Nat Genet. 2010;42(11):937–48.
Hotta K, Nakamura M, Nakamura T, Matsuo T, Nakata Y, Kamohara S, et al. Association between obesity and polymorphisms in SEC16B, TMEM18, GNPDA2, BDNF, FAIM2 and MC4R in a Japanese population. J Hum Genet. 2009;54(12):727–31.
Liem ET, Vonk JM, Sauer PJ, van der Steege G, Oosterom E, Stolk RP, et al. Influence of common variants near INSIG2, in FTO, and near MC4R genes on overweight and the metabolic profile in adolescence: the TRAILS (TRacking Adolescents’ Individual Lives Survey) Study. Am J Clin Nutr. 2010;91(2):321–8.
Ng MC, Tam CH, So WY, Ho JS, Chan AW, Lee HM, et al. Implication of genetic variants near negr1, sec16b, tmem18, etv5/dgkg, gnpda2, lin7c/bdnf, mtch2, bcdin3d/faim2, sh2b1, fto, mc4r, and kctd15 with obesity and type 2 diabetes in 7705 Chinese. J Clin Endocrinol Metabolism. 2010;95(5):2418–25.
Grant SF, Bradfield JP, Zhang H, Wang K, Kim CE, Annaiah K, et al. Investigation of the locus near MC4R with childhood obesity in Americans of European and African ancestry. Obesity. 2009;17(7):1461–5.
García-Solís P, Reyes-Bastidas M, Flores K, García OP, Rosado JL, Méndez-Villa L, et al. Fat mass obesity-associated (FTO)(rs9939609) and melanocortin 4 receptor (MC4R)(rs17782313) SNP are positively associated with obesity and blood pressure in Mexican school-aged children. Br J Nutr. 2016;116(10):1834–40.
Mejía-Benítez A, Klünder-Klünder M, Yengo L, Meyre D, Aradillas C, Cruz E, et al. Analysis of the contribution of FTO, NPC1, ENPP1, NEGR1, GNPDA2 and MC4Rgenes to obesity in Mexican children. BMC Med Genet. 2013;14(1):21.
Almeida SM, Furtado JM, Mascarenhas P, Ferraz ME, Ferreira JC, Monteiro MP, et al. Association between LEPR, FTO, MC4R, and PPARG-2 polymorphisms with obesity traits and metabolic phenotypes in school-aged children. Endocrine. 2018;60(3):466–78.
Tang Y, Jin B, Zhou L, Lu W. MeQTL analysis of childhood obesity links epigenetics with a risk SNP rs17782313 near MC4R from meta-analysis. Oncotarget. 2017;8(2):2800–6.
Obregón A, Oyarce K, Santos J, Valladares M, Goldfield G. Association of the melanocortin 4 receptor gene rs17782313 polymorphism with rewarding value of food and eating behavior in Chilean children. J Physiol Biochem. 2017;73(1):29–35.
Vega JA, Salazar G, Hodgson MI, Cataldo LR, Valladares M, Obregón AM, et al. Melanocortin-4 receptor gene variation is associated with eating behavior in Chilean adults. Annals of Nutrition and Metabolism. 2016;68(1):35–41.
Rana S, Rahmani S, Mirza S. MC4R variant rs17782313 and manifestation of obese phenotype in Pakistani females. RSC Adv. 2018;8(30):16957–72.
Acknowlegment
Research reported in this publication was supported by Elite Researcher Grant Committee under award number 957,994 from the National Institute for Medical Research Development (NIMAD ), Tehran, Iran.
Funding
This research was done under support of Endocrinology and Metabolism Research Center Institute, Tehran University of Medical sciences, Tehran, Iran.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
None.
Study limitation
Our limitation was small sample size that will be solved if we continue to collect sample in future.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mohsenipour, R., Rabbani, A., amoli, M.M. et al. Relationship between a near Melanocortin-4 receptor gene variant and puberty timing in children is vague unlike obesity. J Diabetes Metab Disord 21, 1255–1260 (2022). https://doi.org/10.1007/s40200-022-01011-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-022-01011-5