Abstract
Iran, as an in-transition country, tackled communicable diseases and now is confronting emerging challenges of non-communicable diseases (NCDs) in the path to reach health for everyone at all ages by 2030. Across Iran, death-averting treatments of NCDs have been expanded recently which might cause a shift toward a greater share of years lived with disability (YLDs) compared to years of life lost (YLLs) in the disability-adjusted life years of NCDs. Since the management of disability differs from the reduction of mortality in terms of public health policies, depicting the current picture of the burden of NCDs is principal for policymakers in achieving health for all. In this communication, we briefly reviewed our current knowledge about the burden of NCDs in Iran and found that burdens of cardiovascular diseases and asthma are shifting toward greater YLDs than YLLs. In addition to expanding preventive measures and maintenance of the current system, this profile calls policymakers for the development of more rehabilitation centers for patients with ischemic heart disease, stroke, and respiratory diseases to mitigate their disabilities. The consistent increase in the age-standardized YLD rate of neoplasms necessitates providing rehabilitation centers as well. Morbidity and mortality of diabetes have increased robustly which warrant extensive preventive and control measures. It should be noted that the estimates of the Global Burden of Disease study offer us invaluable insights on the burden of diseases in Iran; nonetheless, efforts for gathering nationally-representative data, e.g., National and Subnational Burden of Diseases, Injuries, and Risk Factors study, are strongly encouraged in the future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2015, all United Nations Member States adopted sustainable development goals (SDGs) of which target 3 signifies providing health for everyone at all ages by 2030 [1]. Tracking our path toward this target necessitates a better understanding of the burden of diseases not only in the global scale [2] but also at national and even subnational levels. Iran, as an in-transition country, tackled communicable diseases in recent decades, mainly by the extensive infrastructure of primary health centers, and now is confronting emerging challenges of non-communicable diseases (NCDs) [3].
Across Iran, death-averting treatments of NCDs including percutaneous coronary intervention for ischemic heart disease [4, 5], novel oral agents and insulin for diabetes [6], and screening programs, radiotherapy, chemotherapy and modern imaging modalities for cancers [7] have been expanded in recent decades. These improvements might cause a shift toward years lived with disability (YLDs) compared to years of life lost (YLLs) in the disability-adjusted life years (DALYs) of NCDs. From the perspective of policymakers, this shift is of utmost importance given that management of disabilities differs from management of deaths in terms of public health policies and resource allocation. Therefore, investigating the burden of NCDs, as the main challenge of the health system of Iran, is principal for future policies to achieve SDG target 3. In this narrative review, we aimed to briefly review our current knowledge about the burden of NCDs in Iran with emphasis on four main NCDs (Cardiovascular Diseases, Diabetes, Neoplasms, and Respiratory Diseases) considered by the World Health Organization [8]. We are going to explore the epidemiological trends of these diseases to provide future perspectives.
Search strategy and selection criteria
In this study, we searched online databases via PubMed, Scopus, and Web of Knowledge up to December 15, 2019. The following keywords and other related terms were employed: Iran, Non-communicable Disease, Cardiovascular Diseases, Diabetes, Neoplasms, Asthma, Chronic Obstructive Pulmonary Disease, DALY, YLL, YLD, Mortality, Death, and Disability. We restricted our search to articles in English and excluded conference abstracts and correspondences. Studies that investigated epidemiological trends of NCDs in Iran were included. Titles/abstracts and full-texts were screened by two reviewers and discrepancies were resolved upon discussion.
Overview
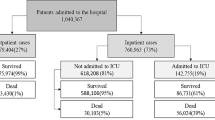
According to the results of the Global Burden of Disease Study 2017 (GBD 2017), the proportion of deaths attributable to NCDs steadily increased from 50% in 1990 and reached 82% in 2017 in Iran [9, 10]. The count of YLLs attributed to NCDs rose by 16% from 1990 to 2013 and reduced by 4% afterward until 2017 [10]. Moreover, the absolute number of YLDs and DALYs of NCDs grew by 98% and 48%from 1990 to 2017, accordingly [2, 11,12,13]. Noticeably, age-standardized rates of YLL and DALY diminished by 35% and 19%, respectively; nevertheless, the age-standardized rate of YLD increased by 3% in this period [2, 10,11,12,13]. These changes imply that the health system effectively prevented deaths from NCDs and the burden of NCDs shifted toward YLDs. In this study, in addition to the GBD, we employed results from the National and Subnational Burden of Diseases, Injuries, and Risk Factors (NASBOD) study 2015 as the nationally-representative data to demonstrate the trend of the mortality of NCDs [14,15,16,17,18,19,20,21].
Cardiovascular diseases
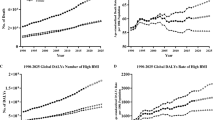
Ischemic heart disease (IHD) is the most prevalent cause of YLL [22] and DALY [12] attributed to NCDs from the early 2000s. Although the observed-to-expected ratio of YLL, predicted based on the socio-demographic index, for most of the causes was less than one, it was 1.21 for IHD in 2015 [22]. According to the results of the GBD, age-standardized YLL, YLD, and DALY rates of IHD decreased from 1990 to 2017; nonetheless, population growth led to increased counts of these measures [2, 10,11,12,13]. These trends were almost similar between males and females. It should be noted that the reduction of age-standardized YLL is more pronounced than age-standardized YLD (46% vs 7%). Furthermore, the increase in the number of YLLs is less prominent than the increase in the number of YLDs (41% vs 150%) (Fig. 1) [2, 10,11,12,13].
Results from the NASBOD study 2015 indicate that the age-standardized mortality rate (ASMR) of stroke after growing from 1990 to 2001–2002, started to decrease; however, the absolute number of deaths increased [23]. In contrast with IHD, ASMR of both types of stroke, ischemic, and hemorrhagic and other non-ischemic, have been reduced from 1990 to 2015 [23]. Trends of the age-standardized and absolute number of measures of the burden for stroke are quite similar to the IHD scenario. The age-standardized rates of YLL, YLD, and DALY decreased by 47%, 5%, and 42%, respectively (Fig. 1) [2, 10,11,12,13]. Similarly, there was no remarkable sex disparity for stroke.
Diabetes
The prevalence of diabetes has been doubled from 5% in 1980 to 10% in 2014 [24] which is mostly attributed to the increased prevalence of obesity amongst adults in the last decades [25]; however, other factors including abdominal obesity and low levels of serum 25-hydroxy vitamin D contributed to this increase [26]. According to the NASBOD study 2015, the ASMR of diabetes increased from 1990 to 2007–2009 and decreased afterward; however, the ASMR in 2015 was 128% greater than in 1990 [27]. Absolute counts of YLLs, YLDs, and DALYs of diabetes have increased by 225%, 277%, and 254%, respectively, from 1990 to 2017 [2, 10, 11]. In this period, age-standardized rates of YLL, YLD, and DALY grew by 40%, 55%, and 48%, respectively (Fig. 1) [2, 10, 11]. These trends were almost similar between both sexes.
Neoplasms
The GBD demonstrated that the absolute counts of YLLs, YLDs, and DALYs due to neoplasms increased steadily by 96%, 294%, and 99%, respectively, from 1990 to 2017 [2, 10, 11, 28]. Although age-standardized rates of YLL and DALY decreased overall by 4% and 3%, respectively, during this period, it should be noted that this reduction was not consistent and followed a sinus pattern, a decrease followed by an increase and another decrease afterward [2, 10]. In contrast, age-standardized YLD increased consistently by 72% from 1990 to 2017 (Fig. 1) [11]. There was no remarkable sex disparity regarding these trends.
Respiratory diseases
Results from the NASBOD study 2015 demonstrated that ASMR of asthma decreased from 2001 to 2015, in contrast with chronic obstructive pulmonary disease (COPD) which experienced a rise [29]. The GBD 2017 showed that the count of YLLs and YLDs attributed to asthma decreased and increased, respectively, from 1990 to 2017, while the count of DALYs fairly remained constant. Although the age-standardized YLL and DALY rates of asthma were reduced by 70% and 46%, respectively, the age-standardized YLD rate decreased just by 5% during this period (Fig. 1). The absolute number of YLLs, YLDs, and DALYs due to COPD rose from 1990 to 2017. Furthermore, age-standardized YLL decreased by 4% and age-standardized YLD and DALY grew by 10% and 2%, respectively; nevertheless, these changes were not consistent in the study period (Fig. 1) [2, 10, 11].
Other NCDs
In 2017, mental disorders, musculoskeletal disorders, and substance use disorders caused most of the YLDs in Iran [11, 13]. In 2017, musculoskeletal disorders including rheumatoid arthritis, osteoarthritis, low back pain, neck pain, and gout were responsible for 15.1% of total YLDs in Iran [11, 13, 30]. Mental disorders and substance use disorders accounted for 17.9% and 12.8% of Iranian disabilities in 2017 [11, 13]. The growth pattern of mental and substance use disorders is alarming [13, 22] and encouraged researchers to investigate their trends [14, 31]. In contrast with mental and musculoskeletal disorders, the burden of substance use disorders includes mortality as well as morbidity, especially for men which necessitates appropriate interventions [11, 13, 22].
In 2017, neurological disorders including Alzheimer’s disease and other dementias, Parkinson’s disease, epilepsy, multiple sclerosis, motor neuron disease, and headache disorders contributed to 10.9% of total YLDs in Iran [11, 13]. The National Elderly Health Survey demonstrated that about 8% of individuals aged ≥60 years have dementia in Iran. Noticeably, dementia is a disease of aging and our country is going to have an old population pyramid due to the low fertility rate and increased life expectancy [32]. Therefore, we might expect a greater burden of dementia soon.
Results from the NASBOD study 2015 demonstrated that ASMR of liver cirrhosis increased from 1990 to 2002 and decreased afterward which can be ascribed to the national vaccination program for hepatitis B [33]. Furthermore, the ASMR of liver cancer rose from 1990 to 2010 followed by a slight decrease. Given that no screening program is recommended for this neoplasm, the focus must be on its prevention. Vaccination for hepatitis B and the treatment of hepatitis C are appropriate targets for the prevention of liver cancer, since they are collectively responsible for 71% of liver cancer mortality in Iran [34].
Perspectives
We found that the YLD to YLL ratio for IHD, stroke, and asthma has increased from 1990 to 2017. This profile implies that patients with these diseases are less likely to die and more likely to be disabled nowadays compared to 30 years ago. These findings call policymakers for the development of more rehabilitation centers, in addition to maintenance of the current death averting measures for these diseases.
Diabetes showed a distinct profile with increasing numbers and age-standardized rates of YLL, YLD, and DALY. From 1990 to 2017, attributed YLD grew faster than YLL (55% versus 40%) which implies that we are going towards a greater share of morbidity of diabetes than its mortality, similar to IHD, stroke, and asthma; however, this alarming profile demonstrates that the preventive and control measures [6] were not successful in the reduction of either morbidity or mortality of diabetes. It is forecasted that diabetes will impose a greater burden on the Iranian health system in the near future given the increased prevalence of overweightness and obesity amongst children and adolescents recently [35]. Therefore, policymakers should provide appropriate action plans that may include national awareness-raising campaigns and systematic screening programs.
Contrary to IHD, stroke, and asthma, given the sinus pattern of the trends of age-standardized rates of YLL and DALY of neoplasms, we cannot firmly attribute this pattern to increased survival and disability of patients with neoplasms. If the diminishing trend of age-standardized YLL and DALY continues in the next years, then we can infer a shift toward YLDs in the burden of neoplasms. Policymakers should continue and extend the preventive measures including screening programs and management of risk factors, and treatments of neoplasms. Furthermore, the consistent increase in the age-standardized YLD of neoplasms necessitates providing rehabilitation centers.
We found that the ASMR of COPD has increased from 1990 to 2017. Given that air pollution is a risk factor of COPD [36], the increase in ASMR of COPD may be attributed to the deteriorating quality of air in the capital cities and probably other urban regions in recent years [37, 38]. Moreover, the long-term exposure of Iranian people with ambient particulate matter <2.5 μm has increased from 1990 to 2016 by 63% and COPD experienced the greatest increase in mortality attributable to these matters during this period [38]. Notably, the increasing trend in mortality of COPD may not arise from the tobacco smoking pattern due to its relatively stable prevalence [39]. These findings warrant policies aimed at the reduction of air pollution to reverse this trend. Moreover, increases in the age-standardized rate of YLD of COPD signifies the importance of rehabilitation centers for the disease.
Undoubtedly, the GBD estimates offer us invaluable insights on the burden of diseases in Iran; however, these results always can be more accurate if the real data are available. Hence, efforts for gathering nationally-representative data are strongly encouraged. The Non-Communicable Diseases Research Center took the initiative to provide fatal and non-fatal estimates for 290 diseases and about 60 risk factors in the NASBOD study. To the best of our knowledge, it is the first and the only project dedicated to addressing this gap in the country of which methodological details have been published previously [14,15,16,17,18,19]. It should be noted that the methods are being updated regularly by recognizing and addressing previous drawbacks [20, 21], and the results and updates are available online [27]. Further efforts are warranted to produce accurate and consistent data on the burden of NCDs in Iran.
The share of morbidity and mortality in the burden of a disease has insightful policymaking implications. Our findings indicate the importance of monitoring fatal and non-fatal estimates of NCDs to help policymakers in implementing more effective actions and resource allocation. Although we reviewed these trends for Iran, it may be a ground for other countries to depict their epidemiological picture of NCDs to achieve SDG target 3. The Iranian success story on implementing the NASBOD nationwide survey encourages other countries to produce nationally-representative estimates rather than relying on the GBD estimates.
Conclusion
In this communication, we reviewed the trends of main NCDs in Iran to demonstrate the current epidemiological picture of the biggest challenge of the Iranian health system. We can infer that the burden of the main NCDs is shifting toward greater YLDs than YLLs. In addition to expanding preventive measures and maintenance of the current system, this profile calls policymakers for the development of more rehabilitation centers for patients with IHD, stroke, and respiratory diseases to decrease their disabilities. The consistent increase in the age-standardized YLD rate of neoplasms necessitates providing rehabilitation centers as well. Furthermore, the alarming profile of diabetes necessitates extensive preventive and control measures.
References
UN. Sustainable development goal 3. https://sustainabledevelopment.un.org/sdg3. Accessed Dec 8, 2019.
Kyu HH, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392(10159):1859–922. https://doi.org/10.1016/S0140-6736(18)32335-3.
Danaei G, Farzadfar F, Kelishadi R, Rashidian A, Rouhani OM, Ahmadnia S, et al. Iran in transition. Lancet. 2019;393(10184):1984–2005. https://doi.org/10.1016/S0140-6736(18)33197-0.
Kassaian SE, Masoudkabir F, Sezavar H, Mohammadi M, Pourmoghaddas A, Kojuri J, et al. Clinical characteristics, management and 1-year outcomes of patients with acute coronary syndrome in Iran: the Iranian project for assessment of coronary events 2 (IPACE2). BMJ Open. 2015;5(12):e007786. https://doi.org/10.1136/bmjopen-2015-007786.
Poorhosseini H, Abbasi SH. The Tehran Heart Center. Eur Heart J. 2018;39(29):2695–6. https://doi.org/10.1093/eurheartj/ehy369.
Esteghamati A, Larijani B, Aghajani MH, Ghaemi F, Kermanchi J, Shahrami A, et al. Diabetes in Iran: Prospective Analysis from First Nationwide Diabetes Report of National Program for Prevention and Control of Diabetes (NPPCD-2016). Sci Rep. 2017;7(1):13461. https://doi.org/10.1038/s41598-017-13379-z.
Azizi MH, Bahadori M, Azizi F (2013) History of cancer in Iran. Archives of Iranian medicine. 16(10):613–22. doi:0131610/aim.0015.
WHO. https://www.who.int/features/factfiles/noncommunicable_diseases/en/. Accessed Dec 8, 2019.
Sheidaei A, Gohari K, Kasaeian A, Rezaei N, Mansouri A, Khosravi A et al. (2017) National and Subnational Patterns of Cause of Death in Iran 1990–2015: Applied Methods. Archives of Iranian medicine. 20(1):2–11. doi:0172001/aim.003
Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392(10159):1736–88. https://doi.org/10.1016/S0140-6736(18)32203-7.
James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392(10159):1789–858. https://doi.org/10.1016/S0140-6736(18)32279-7.
Sepanlou SG, Parsaeian M, Krohn KJ, Afshin A, Farzadfar F, Roshandel G, et al. Disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE) in Iran and its neighboring countries, 1990-2015: findings from global burden of disease study 2015. Archives of Iranian medicine. 2017;20(7):403–18.
Djalalinia S, Saeedi Moghaddam S, Moradi-Lakeh M, Shahraz S, Naghavi M, Murray CJL, et al. Prevalence and years lived with disability of 310 diseases and injuries in Iran and its neighboring countries, 1990-2015: findings from global burden of disease study 2015. Archives of Iranian medicine. 2017;20(7):392–402.
Naserbakht M, Djalalinia S, Tayefi B, Gholami M, Eftekhar Ardabili M, Shariat SV et al. (2014) National and sub-national prevalence, trend, and burden of mental disorders and substance abuse in Iran: 1990–2013, study protocol. Archives of Iranian medicine. 17(3):182–8. doi:0141703/aim.008
Farzadfar F, Delavari A, Malekzadeh R, Mesdaghinia A, Jamshidi HR, Sayyari A et al. (2014) NASBOD 2013: design, definitions, and metrics. Archives of Iranian medicine. 17(1):7–15. doi:0141701/aim.004
Mohammadi Y, Parsaeian M, Farzadfar F, Kasaeian A, Mehdipour P, Sheidaei A et al. (2014) Levels and trends of child and adult mortality rates in the Islamic Republic of Iran, 1990–2013; protocol of the NASBOD study. Archives of Iranian medicine. 17(3):176–81. doi:0141703/aim.007
Hassannia T, Farzadfar F, Noori A, Moradi-Lakeh M, Delavari F, Jamshidi HR et al. (2014) National and sub-national prevalence, trend, and burden of end stage renal diseases (ESRD) in Iran 1990–2013; the study protocol. Archives of Iranian medicine. 17(12):800–3. doi:0141712/aim.004
Salimzadeh H, Ardeshir Larijani F, Abedian S, Kalantar Motamedi SM, Malekzadeh MM, Mohaghegh H et al. The trend of national and sub-national burden of gastrointestinal and liver diseases in Iran 1990 to 2013; study protocol. Archives of Iranian medicine. 2014;17(1):33–53. doi:0141701/aim.008.
Shoaee S, Ghasemian A, Najafi B, Kasaeian A, Farzadfar F, Hessari H (2014) National and sub-national burden of oral diseases in Iran: 1990–2013, study protocol. Archives of Iranian medicine. 17(3):159–68. doi:0141703/aim.005
Modirian M, Rahimzadeh S, Cheraghi Z, Khosravi A, Salimzadeh H, Kompani F et al. (2014) Quality evaluation of national cancer registry system in Iran: study protocol. Archives of Iranian medicine. 17(3):193–7. doi:0141703/aim.0010
Niakan Kalhori SR, Tayefi B, Noori A, Mearaji M, Rahimzade S, Zandian E et al. (2014) Inpatient data, inevitable need for policy making at national and sub-national levels: a lesson learned from NASBOD. Archives of Iranian medicine. 17(1):16–21. doi:0141701/aim.005
Moradi-Lakeh M, Sepanlou SG, Karimi SM, Khalili N, Djalalinia S, Karimkhani C, et al. Trend of socio-demographic index and mortality estimates in Iran and its neighbors, 1990-2015; findings of the global burden of diseases 2015 study. Archives of Iranian medicine. 2017;20(7):419–28.
Djalalinia S, Saeedi Moghaddam S, Rezaei N, Rezaei N, Mansouri A, Abdolhamidi E, et al. National and sub-national patterns of mortality from stroke in the Iranian population (1990-2015): complementary results from the NASBOD study. International journal of stroke : official journal of the International Stroke Society. 2018;1747493018799974. https://doi.org/10.1177/1747493018799974.
Zhou B, Lu Y, Hajifathalian K, Bentham J, Di Cesare M, Danaei G, et al. Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016;387(10027):1513–30. https://doi.org/10.1016/S0140-6736(16)00618-8.
Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. The Lancet. 2016;387(10026):1377–96. doi:https://doi.org/10.1016/S0140-6736(16)30054-X.
Ramezankhani A, Harati H, Bozorgmanesh M, Tohidi M, Khalili D, Azizi F, et al. Diabetes mellitus: findings from 20 years of the Tehran lipid and glucose study. International journal of endocrinology and metabolism. 2018;16(4 Suppl):e84784. https://doi.org/10.5812/ijem.84784.
NCDRC. https://vizit.report/panel/nasbod/en/main.html. Accessed Dec 8, 2019.
Modirian M, Rahimzadeh S, Cheraghi Z, Saeedi Moghaddam S, Rezaei N, Tohidinik HR et al. (2015) Burden of Cancers in Iran from 1990 to 2010: findings from the Global Burden of Disease study 2010. Archives of Iranian medicine. 18(10):629–37. doi:0151810/aim.004
Varmaghani M, Kebriaeezadeh A, Sharifi F, Sheidaei A, Rashidian A, Moradi-Lakeh M, et al. Death-specific rate due to asthma and chronic obstructive pulmonary disease in Iran. Clin Respir J. 2018;12(6):2075–83. https://doi.org/10.1111/crj.12776.
Moradi-Lakeh M, Forouzanfar MH, Vollset SE, El Bcheraoui C, Daoud F, Afshin A, et al. Burden of musculoskeletal disorders in the eastern Mediterranean region, 1990-2013: findings from the global burden of disease study 2013. Ann Rheum Dis. 2017;76(8):1365–73. https://doi.org/10.1136/annrheumdis-2016-210146.
Sharifi V, Amin-Esmaeili M, Hajebi A, Motevalian A, Radgoodarzi R, Hefazi M et al. (2015) Twelve-month prevalence and correlates of psychiatric disorders in Iran: the Iranian Mental Health Survey, 2011. Archives of Iranian medicine. 18(2):76–84. doi:015182/aim.004
Sharifi F, Fakhrzadeh H, Varmaghani M, Arzaghi SM, Alizadeh Khoei M, Farzadfar F et al. (2016) Prevalence of Dementia and Associated Factors among Older Adults in Iran: National Elderly Health Survey (NEHS). Archives of Iranian medicine. 19(12):838–44. doi:0161912/aim.005
Rezaei N, Asadi-Lari M, Sheidaei A, Khademi S, Gohari K, Delavari F, et al. Liver cirrhosis mortality at national and provincial levels in Iran between 1990 and 2015: a meta regression analysis. PLoS One. 2019;14(1):e0198449. https://doi.org/10.1371/journal.pone.0198449.
Rezaei N, Farzad Far F, Khademiureh S, Sheidaei A, Gohari K, Delavari F, et al. Liver Cancer mortality at national and provincial levels in Iran between 1990 and 2015: a Meta regression analysis. Hepat Mon. 2018;18(1):e62009. https://doi.org/10.5812/hepatmon.62009.
Kelishadi R, Haghdoost AA, Sadeghirad B, Khajehkazemi R (2014) Trend in the prevalence of obesity and overweight among Iranian children and adolescents: a systematic review and meta-analysis. Nutrition (Burbank, Los Angeles County, Calif). 30(4):393–400. doi:https://doi.org/10.1016/j.nut.2013.08.011
Kelly FJ, Fussell JC. Air pollution and airway disease. Clinical and experimental allergy : journal of the British Society for Allergy and Clinical Immunology. 2011;41(8):1059–71. https://doi.org/10.1111/j.1365-2222.2011.03776.x.
Jamaati H, Attarchi M, Hassani S, Farid E, Seyedmehdi SM, Pormehr PS. Investigating air quality status and air pollutant trends over the Metropolitan Area of Tehran, Iran over the past decade between 2005 and 2014. Environ Health Toxicol. 2018;33(2):e2018010-e. https://doi.org/10.5620/eht.e2018010.
Shamsipour M, Hassanvand MS, Gohari K, Yunesian M, Fotouhi A, Naddafi K, et al. National and sub-national exposure to ambient fine particulate matter (PM2.5) and its attributable burden of disease in Iran from 1990 to 2016. Environ Pollut. 2019;255:113173. https://doi.org/10.1016/j.envpol.2019.113173.
Ghasemian A, Rezaei N, Saeedi Moghaddam S, Mansouri A, Parsaeian M, Delavari A et al. (2015) Tobacco Smoking Status and the Contribution to Burden of Diseases in Iran, 1990–2010: findings from the Global Burden of Disease Study 2010. Archives of Iranian medicine. 18(8):493–501. doi:015188/aim.006
Availability of data and material
Not applicable.
Code availability
Not applicable.
Author information
Authors and Affiliations
Contributions
AA prepared the first manuscript. NF, SA, EM, KJ, MR, and SMF helped in the process of literature review and data interpretation. NR, SN, FF, and BL reviewed and commented on the final manuscript. All authors approved the final manuscript. NR and BL were the corresponding authors and supervised all stages of manuscript preparation and publication.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aminorroaya, A., Fattahi, N., Azadnajafabad, S. et al. Burden of non-communicable diseases in Iran: past, present, and future. J Diabetes Metab Disord (2020). https://doi.org/10.1007/s40200-020-00669-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40200-020-00669-z