Abstract
Purpose
Prevalence of osteoporosis reported as high as 50% in thalassemia major patients. We compared bone density (BMD) of our patients with results of bone densitometry of participants of a national study, to find if BMD diagnosis is ethnicity sensitive or not.
Methods
In 177 adult beta thalassemia major patients and 490 normal subjects of 20–39 y/o range, dual-energy X-ray absorptiometry of the spine and femur performed. Normal subjects participated in Iranian Multi-center Osteoporosis Study (IMOS). Mean and standard deviation of normal ones achieved and Z-score of patients re-calculated based on normal Iranians. As BMD of normal participants and patients performed by devices of different brands, analyses done based on calculated standard BMD of all participants.
Results
BMD of patients was significantly lower than normal participants (P value <0.001). Frequency of Z-score ≤−2 found in 52% and 56% of patients in femur and spine regions, respectively. New Z-score of patients according to Iranian normal populations calculated. Frequency of this new Z-score ≤−2 found in 16% and 72% of patients in femur and spine regions, respectively.
Conclusions
We think in secondary osteoporosis, may be other cut-off points, especially according to BMD of normal population of that geographical region are needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is the most prevalent metabolic bone disease and is a known risk factor for pathologic fracture [1, 2] that leads to significant morbidity and mortality. Currently, dual-energy X-ray absorptiometry (DXA) is the gold standard for the diagnosis of osteoporosis. According to the World Health Organization (WHO), postmenopausal osteoporosis is defined as a bone mineral density (BMD) T-score of 2.5 or more below the mean for young women [3].
Furthermore, the International Society for Clinical Densitometry (ISCD) suggested that in younger females and males (premenopausal females and males aged <50 years), a Z-score of −2.0 or lower is considered to be “below the expected range for age.” [4]
The different criteria for osteoporosis in younger individuals have been carefully considered. For example, young patients with osteoporosis are mainly affected by chronic illnesses and characterized by a short stature and delayed puberty [5, 6]. The use of the Z-score by the ISCD as the main parameter for diagnosis of low bone mass in younger patients has many advantages; however, there are some disadvantages, particularly in case of endemic diseases. Some questions concerning the use of this parameter remain unanswered, e.g., “Does ethnicity affect the interpretation of DXA results in chronic diseases?” or “Do chronically ill patients in different countries require a different cut-off for BMD for predicting pathologic fracture?” One approach to answer these questions is to follow-up with chronically ill patients in different geographical regions until the first pathologic fractures occurs and define the cut-off point of BMD for pathologic fracture. However, this is costly and time-consuming and may not be possible in every region or country. Another approach is to compare the patient-derived values with region-specific normal BMD values. This may help define the differences between Z-scores or T-scores when using a default device reference range or a region- or ethnicity-specific reference range. If there is no significant variation between the results, it appears, at least theoretically, that the affected patients will follow the natural course of the pathologic fracture, as followed by the healthy population of the country of origin of the device.
Iran is an endemic area of thalassemia major, a disease that is a known risk factor for secondary osteoporosis [7]. Therefore, diagnosis, monitoring, and treatment of secondary osteoporosis are crucial. Beta-thalassemia major, a type of anemia, is caused by disorders in the synthesis of beta-globin chains and is an endemic disease in the Mediterranean region and Iran. Features of this disease include hemolysis and impaired erythropoiesis [8]. Bone destruction and mechanical interruption of bone formation, which are known complications of the disease, result from ineffective erythropoiesis. Bone marrow expansion leads to cortical attenuation of bones [9]. Chronic transfusion is essential for patients, and iron overload and hemochromatosis occur due to hypertransfusion [10, 11]. It seems ferric iron from hyper-transfusion has dangerous effects on osteoblasts in these patients [12]. Genetic factors also must be remembered. Polymorphism of genes like COL1A1 and TGF-β1 gene and VDR reported effective on bone strengths in thalassemics [13].
Alterations in the growth hormone/insulin-like growth factor I (GH/IGF-I) axis in patients with thalassemia and genetic factors play important roles in thalassemia-induced osteoporosis [14].
Other endocrinopathies that are by themselves risk factors for low BMD, found to be more prevalence in thalassemic patients than in normal [15,16,17,18].
Although not all thalassemia studies report a very high prevalence of osteoporosis [19], they do report a prevalence of 40%–50%, even using different methods of bone densitometry [20], which are not always in agreement [21]. Even in well-managed patients [22], osteoporosis is a significant comorbidity in this population [23]. Routine BMD and ethical monitoring in pediatric and adult patients with thalassemia to investigate bone density may provide a unique opportunity to elucidate a model for the natural course of secondary osteoporosis [24]. As we said above we are here to find “Does ethnicity affect the interpretation of DXA results in chronic diseases?” At least we want to find the answers about thalassemia major patients in Iran.
Methods
Subjects
177 Thalassemia major Patients (20–39 y/o) selected from Special Medical Center of Charity Foundation for Special Disease of Iran (SMC of CFFSD) BMD center. Special Medical Center is a reference center for major thalassemic patients that cases from all around Iran refer to it and do their work-up with no charge. They did not use osteoporosis medication.
For control subjects, data used in this study were obtained from the IMOS study [25]. Age- and sex-matched, 490 healthy men and women aged 20 to 39 years that were chosen from 843 healthy people that selected based on randomized clustered sampling of all regions of Tehran-Iran. To confirm inclusion of healthy participants to the study, subjects with the following diseases or conditions were excluded before densitometry: known history or evidence of rheumatoid arthritis, thyroid, parathyroid or adrenal disease, hepatic or renal failure, metabolic bone disease, type I diabetes mellitus, sterility, oligomenorrhea, malignancy, malabsorption, immobility for more than one week, pregnancy, lactation, smoking more than 10 cigarettes per day, alcoholism, and medications influencing bone metabolism [25].
Bone mineral density measurement
Bone mineral density at the lumbar spine (L2-L4; anteroposterior view) and femoral neck of patients were measured by dual-energy X-ray absorptiometry with a Norland XR-46 densitometer. All measurements were made on the same machine at Tehran Special Medical Center, the medical branch of Charity Foundation for Special Diseases).
Bone mineral density at the same BMD regions of healthy Iranian population measured by DXA method with a Lunar DPX-MD machine.
Calculations
The mean and standard deviation (SD) of healthy population and the Z-score of patients was recalculated based on those of normal Iranians. New Z-scores of patients according to normal Iranian populations were calculated based on the following formula:
As the BMD of the healthy population and patients with thalassemia was measured using different brands of devices, analyses were performed based on a calculated standard BMD for all participants. The standard BMD (sBMD) was calculated according to the formula [26]:
Statistical analyses
Continuous parameters are reported as means, standard deviations, and ranges. Categorical parameters are reported as simple percentages. Normality was graphically assessed for the healthy population. The two independent samples tests used to compare the means of the 2 groups. Significance was determined as α (or P value)=.05 and statistical analyses were performed with SPSS software (SPSS: An IBM Company, version 16.0, IBM Corporation, Armonk, NY, USA).
Results
DXA of the spine and femur was performed in 177 adult patients with beta-thalassemia major aged 20–39 years. Patients had no medical history of other diseases and were not taking drugs affecting bone metabolism. The female-to-male ratio was 86/91. Mean of age was 25.1 ± 4.7.
Our results were compared with those of 490 age- and sex-matched healthy population in the Iranian Multi-Center Osteoporosis Study who were randomly selected from a normal Iranian population, and the female-to-male ratio was 229/261. Mean of age was 27.3 ± 5.4.
The BMD of the patients was significantly lower than that of the healthy population (P<0.001) in the femoral and spinal regions (mean of 0.787 g/m2 vs 1.109 g/m2 in the femoral region and 0.763 g/m2 vs 1.203 g/m2 in the spinal region).
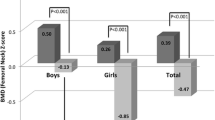
In normal population the mean ± SD of the femoral and spinal Z-scores according to the original reference range (American) of the device was −0.06 ± 1.11 and−0.04 ± 1.08, respectively.
When American reference (the original reference range of the device) used, the mean ± SD of the femoral and spinal Z-scores according to was −1.89 ± 1.12 and−2.09 ± 0.901, respectively. The frequency of Z-score ≤−2 was found in 52% (93 cases) and 56% (100 cases) of patients with thalassemia for the femoral and spinal regions, respectively.
When Iranian reference (new reference range) used, the mean ± SD of femoral and spinal Z-scores were−1.12 ± 1.107 and−2.80 ± 1.23, respectively. The frequency of low BMD Z-scores ≤ −2 was found in 16% (29 cases) and 72% (129 cases) of patients with thalassemia for the femoral and spinal regions.
The mean Z-score in adult Iranian patients with thalassemia was significantly different (higher in the femur and lower in the spine) when using the Iranian reference range (P<0.05).
More detailed results can be found in Table 1.
Discussion
The present study aimed to determine whether ethnicity was a determining factor in the diagnosis of low BMD in patients with chronic disease. Our study showed that the mean Z-score in adult Iranian patients with thalassemia was significantly different when using the Iranian reference range. In a recent study, we found that using T-score≤−2.5 as osteoporosis criteria in adults gave a better prediction power than using Z-score ≤−2 in children [27] and that femoral Z-score of −1 in children was a better cut-off for predicting femoral low bone mass in adults [28]. Another finding from our previous study showed that the odds of Z-score ≤−2 in patients aged 21 years and>22 years in the femoral region was 13 and 8 times greater than that in younger patients, respectively. Although such a cut-off point was found in the present study, we could not explain the scientific reason for this [29]. We also could not find a formula or measurement for adjusting BMD in adult patients with chronic illness; therefore, we decided to examine the role of ethnicity in the interpretation of BMD results in adult patients with thalassemia major. This disease is a representative of bone-deteriorating chronic illnesses. Although our study showed that the mean Z-score in adult Iranian patients with thalassemia was significantly different (higher in the femur and lower in the spine) when using the Iranian reference range, the mean Z-score for normal Iranian participants was not significantly different from that calculated using devices according to its American reference range.
We also found that the mean Z-score of the spine was lower than that of the femur. Their difference is so high that any region drops in different category of low BMD diagnosis. However, there was discordance between the diagnoses in the two regions. In general, diagnostic discordance for osteoporosis includes the observation that the T-score of an individual patient varies from one key measurement site to another and falls into two different diagnostic categories identified by the WHO classification system [30]. Recently, Z-score discordance has been focused on due to the importance of idiopathic low BMD in healthy men and younger patients [31]. It is also a hot topic for assessing low BMD in chronic diseases because patients with chronic disease are generally young, and a Z-score ≤−2 is used as a criterion for low BMD. The reason for this discordance is unclear. Soliman et al. described significant retardation in size observed in general stature and sitting height in patients with thalassemia [32]. Some studies have shown that the spinal vertebrae of patients with thalassemia are shorter [33]. It is known that shorter and smaller bones show lower BMD using DXA. This discordance was not previously reported, and this may be due to fewer studies investigating both sites (femoral and spinal regions) [34].
Why this discordance is more prominent in Iranian patients with thalassemia in comparison to normal Iranians is unknown, but this may be due to a higher mean spine BMD in the Iranian population compared with that in other countries [35].
The present study has some limitations. Data for the BMD Z-score of pediatric patients with thalassemia in comparison to healthy Iranian children would make our results more comprehensive. Furthermore, determining the interference of anthropometric and endocrine parameters compared with the results of BMD in normal Iranians and Iranian patients with thalassemia may improve the interpretation of our results.
In summary, in secondary osteoporosis, other cut-off points, such as the BMD of healthy individuals within a specific geographical region or ethnicity, may help to explain the natural course of pathologic fracture in chronically ill patients.
Change history
23 December 2019
The article ‘The role of using different reference population in the prevalence of low BMD in the thalassemia patients’, written by Mohammad Reza Mohajeri-Tehrani, Najmeh Darvishian, Faezeh Arab, Sedigheh Salemkar, Fariba Mohseni, Bagher Larijani and Zohreh Hamidi, was originally published.
References
World Health Organization Study Group. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Technical report series no. 843. Geneva: WHO; 1994.
Eastell R. Treatment of postmenopausal osteoporosis. N Engl J Med. 1998;338:736–46. https://doi.org/10.1056/NEJM199803123381107.
Kanis JA, Delmas P, Burckhardt P, Cooper C, Torgerson D. Guidelines for diagnosis and management of osteoporosis. The European Foundation for osteoporosis and bone disease. Osteoporos Int. 1997;7:390–406.
Bishop N, Braillon P, Burnham J, et al. Dual-energy X-ray aborptiometry assessment in children and adolescents withdiseases that may affect the skeleton: the 2007 ISCD pediatric official positions. J Clin Densitom. 2008;1:29–42.
van Kuijk C. Pediatric bone densitometry. Radiol Clin N Am. 2010;48:623–7. https://doi.org/10.1016/j.rcl.2010.02.017.
Schonau E. Problems of bone analysis in childhood and adolescence. Pediatr Nephrol. 1998;12:420–42.
Bogunovic LD, Vogiatzi SM, MG. Measurement of bone density in the pediatric population. Curr Opin Pediatr. 2009;21:77–82. https://doi.org/10.1097/MOP.0b013e32831ec338.
Muncie HL Jr, Campbell J. Alpha and Beta thalassemia. Am Fam Physician. 2009;80:339–44.
Voskaridou E, Terpos E. New insights into the pathophysiology and management of osteoporosis in patients with β thalassaemia. Br J Haematol. 2004;127:127–39.
Perera NJ, Lau NS, Mathews S, Waite C, Ho PJ, Caterson ID. Overview of endocrinopathies associated with beta-thalassaemia major. Intern Med J. 2010;40:689–96. https://doi.org/10.1111/j.1445-5994.2010.02254.x.
Mohseni F, Mohajeri-Tehrani MR, Larijani B, Hamidi Z. Relation between BMD and biochemical, transfusion and endocrinological parameters in pediatric thalassemic patients. Arch Osteoporos. 2014;9:174–6. https://doi.org/10.1007/s11657-014-0174-3.
Lertsuwan K, Nammultriputtar K, Nanthawuttiphan S, Phoaubon S, Lertsuwan J, Thongbunchoo J, et al. Ferrous and ferric differentially deteriorate proliferation and differentiation of osteoblast-like UMR-106 cells. Biometals. 2018;31:873–89.
Gaudio A, Morabito N, Catalano A, Rapisarda R, Xourafa A, Lasco A. Pathogenesis of Thalassemia Major-Associated Osteoporosis: Review of the Literature and Our Experience. J Clin Res Pediatr Endocrinol. 2019;28:110–17.
Angelopoulos NG, Katounda E, Rombopoulos G, et al. Evaluation of bone mineral density of the lumbar spine in patients with b-thalassemia major with dual-energy X-ray absorptiometry and quantitative computed tomography, a comparison study. J Pediatr Hematol Oncol. 2006;28:73–8. https://doi.org/10.1007/s11657-014-0174-3.
Najafipour F, Aliasgarzadeh A, Aghamohamadzadeh N, Bahrami A, Mobasri M, Niafar M, et al. A cross-sectional study of metabolic and endocrine complications in beta-thalassemia major. Ann Saudi medicine. 2008;28:361.
Kanbour I, Chandra P, Soliman A, De Sanctis V, Nashwan A, Abusamaan S, et al. Severe liver Iron concentrations (LIC) in 24 patients with β-thalassemia major: correlations with serum ferritin, liver enzymes and endocrine complications. Mediterr J Hematol Infect Dis. 2018;10:e2018062.https://doi.org/10.4084/MJHID.2018.062.
Cario H, Holl RW, Debatin KM, Kohne E. Insulin sensitivity and beta-cell secretion in thalassaemia major with secondary haemochromatosis: assessment by oral glucose tolerance test. Eur J Pediatr. 2003;162:139–46.
Hamidi Z, Mohajeri-Tehrani M, Hamidieh AA, Naghghash A, Behfar M, Alimoghaddam K, et al. How thalassemia affects endocrinological, BMD and bone metabolism parameters - a cross sectional study. Ann Clin Lab Res. 2019;7:293.
Hamidieh AA, Hamidi Z, Nedaeifard L, et al. Bone mineral density in ex-thalassemic pediatric patients. Hematol Oncol Stem Cell Ther. 2012;5:70–1.
Argentiero A, Neglia C, Peluso A, et al. The ability of lumbar spine DXA and phalanx QUS to detect previous fractures in young Thalassemic patients with Hypogonadism, hypothyroidism, diabetes, and hepatitis-B: a 2-year subgroup analysis from the Taranto area of Apulia region. J Pediatr Hematol Oncol. 2013;35:e260–4.
Hamidi Z, Sedaghat M, Mortaz Hejri S, Larijani B. Defining cut-off values for the diagnosis of osteoporosis in postmenopausal women by quantitative ultrasonography of the phalanx. Gynecol Endocrinol. 2008;24:546–8.
Hamidieh AA, Hamidi Z, Nedaeifard L, et al. Changes of bone density in pediatric patients with-thalassemia major after Allogenic hematopoietic stem cell transplantation. Arch Iran Med. 2013;16:88–92.
Gaudio A, Morabito N, Xourafa A, et al. Role of genetic pattern on bone mineral density in thalassemic patients. Clin Biochem. 2010;43:805–7.
Hamidi Z. Osteoporosis, What we learn from bone complication in conjenital disease, thalassemia, an example. Intech. 2012. https://www.researchgate.net/publication/222715466_What_We_Learn_from_Bone_Complications_in_Congenital_Diseases_Thalassemia_an_Example.
Correlation between bone mineral density and osteoporosis With Ca and vitamin D intake (In Farsi). Javadi E., Hossein-nezhad A., Khalili-Fard AR., Adibi H., Maghbooli Z., Larijani B. Tabib_e_sharg, 2003, 5: 1-11. https://www.sid.ir/fa/journal/ViewPaper.aspx?ID=15750
Genant, H K. Grampp, S. Gluer, C C. Faulkner, K G. Jergas, M. Engelke, K. et al. Universal standardization for dual x-ray absorptiometry: patient and phantom cross-calibration results. Journal of bone and mineral research, 1994. 9, 1503-14.
Mohseni F, Mohajeri-Tehrani MR, Larijani B, Hamidi Z.: Correlation between criteria of diagnosis of low bone mineral density in adult and pediatric thalassemic patients: a prospective study. Minerva Pediatr. 2015; Nov 19. PMID: 26583453.
Hamidi Z, Mohseni F , Mohajeri -Tehrani MR, Pajouhi M, Larijani B. Examining Z-score lower than -2 as a cut-off point for low BMD in children with chronic disease: Thalassemia an example. Osteoporos Int. 2015; 26 (Suppl 2):S445.
MOHSENI F, MOHAJERI-TEHRANI MR, LARIJANI B, HAMIDI Z. Bone density changes in thalassemic patients with age and time. HK J Paediatr (new series) 2016; 21 :257-261 .
Moayyeri A, Soltani A, Tabari NK, Sadatsafavi M, Hossein-Neghad A, Larijani B. Discordance in diagnosis of osteoporosis using spine and hip bone densitometry. BMC Endocr Disord. 2005 ; 11;5(1):3.
Park KH, Lim JS, Kim KM, Rhee Y, Lim SK. Z-score discordance and contributing factors in healthy premenopausal women with low bone mineral density: the Korean National Health and Nutrition Examination Survey 2008-9. J Bone Miner Metab. 2015 Oct 7.
Soliman, AT. Khalafallah, H. Ashour, R. Growth and factors affecting it in thalassemia major. Hemoglobin. 2009.;33:S116-S126.https://doi.org/10.3109/03630260903347781.
Vogiatzi MG, Macklin EA, Fung EB, et al. Bone disease in thalassemia: a frequent and still unresolved problem. J Bone Miner Res. 2009. 24:543-57. https://doi.org/10.1359/jbmr.080505.
Mamtani M, Kulkarni H. Bone recovery after zoledronate therapy in thalassemia-induced osteoporosis: a meta-analysis and systematic review. Osteoporos Int. 2010; 21:183-7. https://doi.org/10.1007/s00198-009-0875-4
Larijani B, Moayyeri A, Keshtkar AA, et al. Peak bone mass of Iranian population: the Iranian Multicenter Osteoporosis Study. J Clin Densitom. 2006 Jul-Sep;9(3):367-74.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Declarations of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised due to a retrospective Open Access cancellation.
Rights and permissions
About this article
Cite this article
Mohajeri-Tehrani, M.R., Darvishian, N., Arab, F. et al. The role of using different reference population in the prevalence of low BMD in the thalassemia patients. J Diabetes Metab Disord 19, 431–435 (2020). https://doi.org/10.1007/s40200-019-00455-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-019-00455-6