Abstract
Purpose of Review
The use of neuraxial opioids (NAO) as a method for postoperative analgesia for patients undergoing total joint arthroplasty (TJA) is growing in popularity. Intrathecal morphine (ITM) remains the most commonly used NAO. The purpose of this article is to provide readers with an overview of ITM, as well as a comprehensive review of efficacy, dosing, side effects, complications, and adjuncts of ITM when used for TJA.
Recent Findings
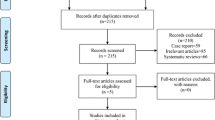
Recent randomized control trials and meta-analyses provide comprehensive evidence on the usefulness of ITM for TJA. Many of these publications demonstrate clear favorability regarding pain outcomes for TJA patients who receive ITM in the perioperative setting. Additional publications help explain the risk for adverse events and complications associated with routine use of ITM.
Summary
Intrathecal morphine is a safe and efficacious modality for providing postoperative analgesia in TJA. A universal approach to optimizing postoperative pain that includes routine use of ITM has yet to be established. Continued research is needed to more clearly define the role that ITM plays in a multi-approach pathway to postoperative analgesia in TJA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total joint arthroplasty (TJA) is growing in popularity and has been one of the most common procedures performed in the US operating rooms over the last several decades [1]. According to the American College of Rheumatology, approximately 790K knee arthroplasties (TKA) and 450K hip arthroplasties (THA) are performed annually [2]. It is widely accepted that postoperative pain following TJA contributes significantly to perioperative morbidity, hindered physical and pulmonary mobilization after surgery, chronic postsurgical pain, and patient dissatisfaction [3, 4]. Multi-approach modalities for optimizing postoperative analgesia are therefore relevant and crucial to patient-centric care. Oral opioid medications remain the mainstay method for controlling postoperative pain; however, the desire to hinder the recent opiate epidemic has led to anesthesiologists employing alternate strategies of pain control. The use of neuraxial opioids (NAOs) has drastically increased over the last 20 years due to their proven efficacy and low risk profile. Additionally, NAOs carry little risk of technical failure and reduce the undesirable side effects of systemic opioids [5]. More specifically, intrathecal morphine (ITM) for TJA has emerged in the literature as a safe, cost-effective, and efficacious method to provide postoperative analgesia [6•, 7•].
Overview of Intrathecal Morphine
Chemical Properties of Neuraxial Opioids
When administering opioid medications, it is important to understand how their chemical properties will impact the expected analgesic effect. These key factors include duration of action, propensity for cranial spread in the cerebral spinal fluid, and the potency of the opioid selected. Hydrophilic opioids, such as morphine and hydromorphone, bind with higher affinity to the opioid receptors of the dorsal horn of the spinal cord; thus, these opioids have higher potency and longer duration of action when compared to lipophilic counterparts such as fentanyl or alfentanil [5]. Morphine remains the most commonly used NAO due to its relative low cost, hydrophilicity, and proven efficacy, but this varies by region and hospital system.
Efficacy of Intrathecal Morphine in Total Joint Arthroplasty
NAOs are becoming more commonly used for postoperative pain control following TJA. There are many studies noting the efficacy of NAOs for this purpose. Spinal anesthesia with ITM has been shown to cause a significant reduction in rest pain at 8–12 h postoperatively when compared to opiate-free spinal anesthesia for TJA [8•]. Similarly, ITM has been proven to cause significantly reduced morphine consumption and pain scores at 4 h and 24 h when compared to placebo in patients undergoing TKA [9•]. When considered comprehensively, these studies show use of ITM affords patients favorable pain outcomes. Table 1, below, provides several relevant publications on the efficacy of ITM for TJA.
Dosing of Intrathecal Morphine
Since ITM was first introduced as a modality of postoperative analgesia in 1979, a wide range of ITM doses have been used [14]. Prior to the last 10 years, dosing for ITM has gone as high as 0.5 mg or higher, but anectodal effidence as well as several studies have noted that side effect concerns increase in a dose dependent manner without increasing analgesic efficacy past 0.4 mg. Several randomized controlled trials have recently been conducted to determine the optimal dose of ITM for TJA while minimizing opiate-related side effects. Thus far, these studies offer varying results. In studies comparing 0.2 to 0.1 mg ITM, 0.2 mg has been shown to provide both superior and comparable analgesia; however, 0.2 mg did carry a significantly higher risk of PONV and pruritis [10•, 11]. When comparing the analgesic efficacy of 0.1 mg, 0.2 mg, and 0.3 mg ITM, 0.2 mg and 0.3 mg ITM provided comparable levels of analgesia and were superior to that provided by 0.1 mg ITM, and all three dosages were associated with similar opiate-related side effects including PONV, pruritus, respiratory depression, or urinary retention [15]. When comparing lower doses of 0.1 mg vs 0.15 mg ITM in patients undergoing TJA, it has been shown that 0.15 mg resulted in superior analgesia and a comparable side effect profile of the 0.1 mg [16]. These studies highlight that while 0.1–0.3 mg is potentially a safe and effective dose range for ITM, further research into this topic is needed to optimize postoperative analgesia and minimize adverse effects. Despite these studies showing varying incidence of side effects associated with different dosages, all patient should be risk stratified and counseled on the potential to experience unpleasant side effects when ITM is used.
Adverse Effects
Nausea and Vomiting
Nausea and vomiting is one of the most common adverse effects associated with opioid medications and often contributes to patient dissatisfaction and longer hospital stays following the use of NAOs. Several studies have been conducted to determine the incidence of PONV in patients undergoing TJA under spinal anesthesia with ITM. One prospective study where ITM dosing varied (0.08–0.2 mg) amongst patients undergoing TJA revealed 46% of patients experienced PONV during the first three postoperative days, regardless of PONV prophylaxis [17]. Similarly, a retrospective review of patients who received < 0.3 mg, 0.3 mg, and > 0.3 mg ITM for TJA determined the incidence of PONV to be 56%, 53%, and 53%, respectively [18]. These studies emphasize that regardless of dosing used, the risk for nausea and vomiting following administration of ITM remains high. All patients should be counseled on the risk of PONV should they receive ITM as a part of their anesthetic care. The authors of this review recommend the use of ITM should be avoided in patients who are at high risk for PONV or who have a history of PONV.
Pruritus
Although the exact mechanism of opioid-induced pruritus remains unclear, it is another well-documented adverse effect of NAO that is distressing to patients. The risk of pruritus following ITM has been shown to increase with higher doses [10•, 19]. A retrospective review to determine the side-effect profile of ITM in patients undergoing TJA showed the incidence of pruritus was 35%, 48%, and 45% with ITM dosing of < 0.3 mg, 0.3 mg, and > 0.3 mg, respectively [18]. Likewise pruritus in patients who received ITM has been found to be as high as 38.8% [7•]. Unfortunately, the prevention and treatment of opioid-induced pruritus remain a challenge.
Urinary Retention
Several studies have been conducted to determine the incidence and risk factors for postoperative urinary retention (POUR) associated with ITM. In one retrospective study, authors found that 21% of patients developed POUR, and independent predictors included age over 65 and male gender [20]. Similar studies determined the overall incidence of POUR after hip or knee arthroplasties under spinal anesthesia with ITM to be 36% and 43.3% [21, 22]. The use of spinal anesthesia with ITM should therefore be considered carefully, and caution should be utilized when administering ITM in patients who are high-risk.
Respiratory Depression
Although delayed respiratory depression is a feared problem associated with ITM, it is fortunately a rare complication compared to the aforementioned side effects. In a systematic review of the efficacy and safety of ITM in TJA, authors found that the administration of ITM does not pose an increased risk of respiratory depression or hypoxemia [8•]. Furthermore, patients with diagnosed or suspected obstructive sleep apnea who are undergoing TJA can safely be administered low dose ITM (0.1 mg) without a higher risk of postoperative pulmonary complications, such as respiratory depression [23]. Other recent studies further emphasize the insignificance of respiratory depression following administration of low dose ITM [16, 18, 24].
Other Intrathecal Opiates and Medications
Fentanyl
Fentanyl is a commonly used opioid in subarachnoid block due to its rapid onset and relative potency. The use of fentanyl to supplement and decrease local anesthetic dose requirements has been demonstrated [25]. A subsequent study on intrathecal fentanyl shows less intraoperative hypotension [26]. However, additional authors failed to demonstrate a significant difference in surgical outcomes with intrathecal fentanyl administration including postoperative opioid consumption, readmission rates, or hospital length of stay [27]. Additionally, fentanyl has proven to be inferior to ITM comparing first 24-h pain scores and subsequent analgesic usage with no significant difference in rates of PONV [28]. Fentanyl has also been shown to have inferior pain control compared to morphine in intrathecal catheter infusion-based approaches [29].
Methadone, Buprenorphine, and Nalbuphine
Nalbuphine has been examined as an intrathecal adjunct medication with one group demonstrating faster onset of analgesia in the setting of total hip arthroplasty; however, the analgesic requirements after ITM were significantly lower in the first 24 h postoperatively [30]. In comparison, buprenorphine has been shown to be superior to nalbuphine in regard to visual analog scale scores and time to rescue medication [31]. The use of intrathecal methadone has been studied as well, with one author showing comparable analgesia in the first 4 h, after which morphine was superior with significantly fewer side effects [32].
Clonidine and Dexmedetomidine
While most commonly used as an antihypertensive, several authors have explored the use of neuraxial clonidine as modality of postoperative analgesia. One study comparing the addition of 25 mcg or 75 mcg of clonidine showed decreased postoperative morphine consumption when combined with ITM versus morphine alone. The authors noted increased postoperative hypotension in both clonidine groups with subsequent authors demonstrating comparable results [33, 34]. Though it should be noted that as a single agent combined with bupivacaine, ITM was superior to intrathecal clonidine with improved postoperative pain scores and opioid consumption [35]. Dexmedetomidine, an alternate α-2 agonist, has also been studied for intrathecal use. Similar to clonidine, dexmedetomidine demonstrated inferior postoperative analgesia when added to bupivacaine compared to ITM [36]. Additionally, other authors were not able to show benefit with intrathecal dexmedetomidine and morphine combined [37].
Adjuncts and Alternatives to Intrathecal Morphine
Peripheral Nerve Blockade
Peripheral nerve blockade (PNB) techniques have long been incorporated into enhanced recovery after surgery pathways for TJA due to being associated with reduced chronic postsurgical pain, opiate requirements, pain scores, and hospital length of stay, as well as improved mobilization following surgery [38,39,40,41]. The role of ITM for use in TJA when considered against PNB remains undefined. When compared in randomized control trials for use in TKA, ITM has failed to consistently provide superior analgesia over PNB. It has, however, shown to increase opiate-related side effects, reduce patient satisfaction, and increase postoperative bleeding complications [42,43,44,45]. Meta-analyses comparing ITM to PNB for TKA again offer mixed conclusions on analgesic benefit; however, the evidence of opiate-related side effects is once again demonstrated [12•, 46]. While PNB has shown to provide superior analgesia when used alone, several studies suggest that ITM is appropriate for use in combination with PNB [13•, 13]. ITM has showed more promising results when compared to PNB for THA. Randomized control trials have showed ITM provides superior analgesia when compared to lumbar plexus block and fascia iliaca plane block, with no difference in adverse effects or patient satisfaction [48, 49].
Local Infiltration Analgesia
Local infiltration analgesia (LIA) has been shown to be a beneficial technique for improving postoperative pain following TJA, and it has gained popularity due to requiring very little technical training, its cost effectiveness, and its ability to reduce hospital length of stay [50,51,52]. The literature lacks consensus on the efficacy of LIA compared to ITM for postoperative pain, and studies provide mixed conclusions on the difference in opiate-related side effects. Some authors have credited LIA with reducing postoperative morphine requirements, lowering pain scores, reducing hospital length of stay, and improving patient satisfaction when compared to ITM for TKA, while others found no difference in pain outcomes or incidence of opiate-related side effects for these patients [53,54,55,56,57]. Comprehensive evidence from recent meta-analyses supports the use of LIA over ITM for TJA due to improved pain scores, morphine requirements, length of hospital stay, and opiate-related side effects [58,59,60].
Evidence suggests LIA does not perform alone as well as it does in combination with additional techniques, so it is once more important to consider LIA and ITM as modalities within a multi-faceted approach to analgesia [61]. While acute postoperative pain is the primary outcome in most of these studies, it is important to note no significant difference has been appreciated in quality of life, functional outcomes, or chronic postsurgical pain between patients who received ITM or LIA at the time of surgery [54, 62].
Discussion and Conclusions
ITM is a safe and efficacious method for providing postoperative analgesia to patients undergoing TJA. Morphine is a low-cost medication, has favorable biochemical properties, and is associated with superior analgesic benefit compared to other intrathecally administered medications. Moving forward, the continuing trend that ITM will become increasingly incorporated into enhanced recovery after surgery pathways for total joint arthroplasty is supported, when combined with other analgesic modalities such as perphereal nerve blocks, or ITM alone. ITM is not completely benign as it does carry the risk of unpleasant side effects such as nausea, vomiting, and pruritus, as well as the rather uncommon but dangerous side effect of respiratory depression or sedation. Due to the considerations of recognizing unwanted sequala of ITM, it is recommended that post injection monitoring is in place for at least 24 h [63]. When preparing a plan for adding ITM to a post operative analgesic regimen, the biggest point of contention in recent literature continues to be dosing. While the general consensus is side effects increase in a dose dependent manner without considerable analgesic efficacy with dosing past 0.4 to 0.5 mg, there is wide variability in the risk/reward profile with doses between 0.1 and 0.3 mg. The authors of this review recommend that the comorbidities and surgical circumstances be taken into consideration for each patient before administering ITM. Future research is needed to determine and to clearly define ITM dosage and its role in a multi-approach pathway to postoperative analgesia for TJA.
Data Availability
No datasets were generated or analysed during the current study.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Fingar KR, Stocks C, Weiss AJ, Steiner CA. Most frequent operating room procedures performed in U.S. hospitals, 2003–2012. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD): Agency for Healthcare Research and Quality (US). Statistical Briefs # 186; 2006.
American College of Rheumatology. https://rheumatology.org/patients/joint-replacement-surgery.
Freys SM, Pogatzki-Zahn E. Pain therapy to reduce perioperative complications. Innov Surg Sci. 2019;4(4):158–66.
van Boekel RLM, Warle MC, Nielen RGC, Vissers KCP, van der Sande R, Bronkhorst EM, et al. Relationship between postoperative pain and overall 30-day complications in a broad surgical population: an observational study. Ann Surg. 2019;269(5):856–65.
Rawal N. Intrathecal opioids for the management of post-operative pain. Best Pract Res Clin Anaesthesiol. 2023;37(2):123–32.
Cheah JW, Sing DC, Hansen EN, Aleshi P, Vail TP. Does intrathecal morphine in spinal anesthesia have a role in modern multimodal analgesia for primary total joint arthroplasty? J Arthroplasty. 2018;33(6):1693–8. within 5 years and compressive discussion on topic.
Wang LM, Zhang Z, Yao RZ, Wang GL. The role of intrathecal morphine for postoperative analgesia in primary total joint arthroplasty under spinal anesthesia: a systematic review and meta-analysis. Pain Med. 2021;22(7):1473–84. within 2 years and compressive discussion on topic.
Gonvers E, El-Boghdadly K, Grape S, Albrecht E. Efficacy and safety of intrathecal morphine for analgesia after lower joint arthroplasty: a systematic review and meta-analysis with meta-regression and trial sequential analysis. Anaesthesia. 2021;76(12):1648–58. within 2 years and compressive discussion on topic.
AbdelQadir YH, Nabhan AE, Abdelghany EA, Mohamed AG, Tokhey ASE, Elmegeed AA, et al. Efficacy and safety of intrathecal morphine in total knee arthroplasty: a systematic review and meta-analysis. J Opioid Manag. 2021;17(5):405–16. within 2 years and compressive discussion on topic.
Vitola E, Buraka N, Erts R, Golubovska I, Miscuks A. Effect of different low doses of intrathecal morphine (0.1 and 0.2 mg) on pain and vital functions in patients undergoing total hip arthroplasty: a randomised controlled study. BMC Anesthesiol. 2022;22(1):377. within 1 year and compressive discussion on topic.
Pathonsamit C, Onklin I, Hongku N, Chaiyakit P. Randomized double-blind controlled trial comparing 0.2 mg, 0.1 mg, and no intrathecal morphine combined with periarticular injection for unilateral total knee arthroplasty. Arthroplast Today. 2021;7:253–9. within 2 years and compressive discussion on topic.
Tang Y, Tang X, Wei Q, Zhang H. Intrathecal morphine versus femoral nerve block for pain control after total knee arthroplasty: a meta-analysis. J Orthop Surg Res. 2017;12(1):125. comprehensive meta analysis on topic.
Sundarathiti P, Thammasakulsiri J, Supboon S, Sakdanuwatwong S, Piangjai M. Comparison of continuous femoral nerve block (CFNB/SA) and continuous femoral nerve block with mini-dose spinal morphine (CFNB/SAMO) for postoperative analgesia after total knee arthroplasty (TKA): a randomized controlled study. BMC Anesthesiol. 2016;16(1):38. prospective comprehensive analysis of topic.
Wang JK, Nauss LA, Thomas JE. Pain relief by intrathecally applied morphine in man. Anesthesiology. 1979;50(2):149–51.
Hassett P, Ansari B, Gnanamoorthy P, Kinirons B, Laffey JG. Determination of the efficacy and side-effect profile of lower doses of intrathecal morphine in patients undergoing total knee arthroplasty. BMC Anesthesiol. 2008;8:5.
Sibanyoni M, Biyase N, Motshabi CP. The use of intrathecal morphine for acute postoperative pain in lower limb arthroplasty surgery: a survey of practice at an academic hospital. J Orthop Surg Res. 2022;17(1):323.
Moraitis A, Hultin M, Wallden J. Risk of postoperative nausea and vomiting in hip and knee arthroplasty: a prospective cohort study after spinal anaesthesia including intrathecal morphine. BMC Anesthesiol. 2020;20(1):242.
Hess SR, Lahaye LA, Waligora AC, Sima AP, Jiranek WA, Golladay GJ. Safety and side-effect profile of intrathecal morphine in a diverse patient population undergoing total knee and hip arthroplasty. Eur J Orthop Surg Traumatol. 2019;29(1):125–9.
Murphy PM, Stack D, Kinirons B, Laffey JG. Optimizing the dose of intrathecal morphine in older patients undergoing hip arthroplasty. Anesth Analg. 2003;97(6):1709–15.
Dana E, Ben-Zur O, Dichtwald S, Feigin G, Brin N, Markushevich M, et al. Postoperative urinary retention following hip or knee arthroplasty under spinal anaesthesia with intrathecal morphine: a retrospective cohort study. Singapore Med J. 2023.
David M, Arthur E, Dhuck R, Hemmings E, Dunlop D. High rates of postoperative urinary retention following primary total hip replacement performed under combined general and spinal anaesthesia with intrathecal opiate. J Orthop. 2015;12(Suppl 2):S157–60.
Griesdale DEG, Neufeld J, Dhillon D, Joo J, Sandhu S, Swinton F, Choi PT. Risk factors for urinary retention after hip or knee replacement: a cohort study. Can J Anaesth. 2011;58(12):1097–104. https://doi.org/10.1007/s12630-011-9595-2.
Bai JW, Singh M, Short A, Bozak D, Chung F, Chan VWS, et al. Intrathecal morphine and pulmonary complications after arthroplasty in patients with obstructive sleep apnea: a retrospective cohort study. Anesthesiology. 2020;132(4):702–12.
Albrecht E, Bayon V, Hirotsu C, Al Ja’bari A, Heinzer R. Intrathecal morphine and sleep apnoea severity in patients undergoing hip arthroplasty: a randomised, controlled, triple-blinded trial. Br J Anaesth. 2020;125(5):811–7.
Hitka T, O'Sullivan J, Szucs S, Iohom G. Determination of the initial minimum effective dose of 0.5% bupivacaine with 20 mug of fentanyl for an operative fixation of fractured neck of femur: a prospective, observational trial. Minerva Anestesiol. 2021;87(7):766–73.
Martyr JW, Stannard KJ, Gillespie G. Spinal-induced hypotension in elderly patients with hip fracture. A comparison of glucose-free bupivacaine with glucose-free bupivacaine and fentanyl. Anaesth Intensive Care. 2005;33(1):64–8.
Kelly M, Turcotte J, Aja J, MacDonald J, King P. Impact of intrathecal fentanyl on hospital outcomes for patients undergoing primary total hip arthroplasty with neuraxial anesthesia. Arthroplast Today. 2021;8:200–3.
Kilickaya R, Orak Y, Balci MA, Balci F, Unal I. Comparison of the effects of intrathecal fentanyl and intrathecal morphine on pain in elective total knee replacement surgery. Pain Res Manag. 2016;2016:3256583.
Niemi L, Pitkanen MT, Tuominen MK, Rosenberg PH. Comparison of intrathecal fentanyl infusion with intrathecal morphine infusion or bolus for postoperative pain relief after hip arthroplasty. Anesth Analg. 1993;77(1):126–30.
Fournier R, Van Gessel E, Macksay M, Gamulin Z. Onset and offset of intrathecal morphine versus nalbuphine for postoperative pain relief after total hip replacement. Acta Anaesthesiol Scand. 2000;44(8):940–5.
Kaushal S, Kamlakar M, Baburao JP. Intrathecal nalbuphine vs. buprenorphine as an adjuvant in lower limb orthopedic surgeries: a prospective randomized controlled study. Med Gas Res. 2021;11(4):126–30.
Jacobson L, Chabal C, Brody MC, Ward RJ, Wasse L. Intrathecal methadone: a dose-response study and comparison with intrathecal morphine 0.5 mg. Pain. 1990;43(2):141–8.
Sites BD, Beach M, Biggs R, Rohan C, Wiley C, Rassias A, et al. Intrathecal clonidine added to a bupivacaine-morphine spinal anesthetic improves postoperative analgesia for total knee arthroplasty. Anesth Analg. 2003;96(4):1083–8.
Grace D, Bunting H, Milligan KR, Fee JP. Postoperative analgesia after co-administration of clonidine and morphine by the intrathecal route in patients undergoing hip replacement. Anesth Analg. 1995;80(1):86–91.
Fogarty DJ, Carabine UA, Milligan KR. Comparison of the analgesic effects of intrathecal clonidine and intrathecal morphine after spinal anaesthesia in patients undergoing total hip replacement. Br J Anaesth. 1993;71(5):661–4.
Wasinwong WS-TM, Rujirojindakul P, Oofuwong M, Dilokrattanaphichit N, Thongtip B. Postoperative analgesic effect of intrathecal dexmedetomidine compared to morphine in Bupivacaine spinal block. J Med Assoc Thail. 2019;102(1):42–9.
Omara AF, Mohsen HH, Mohammed Abo Hagar A, Abdelrahman AF. Intrathecal morphine versus morphine-dexmedetomidine combination for postoperative pain control after total knee replacement: a randomized controlled trial. Local Reg Anesth. 2023;16:113–22.
Curatolo M. Adding regional analgesia to general anaesthesia: increase of risk or improved outcome? Eur J Anaesthesiol. 2010;27(7):586–91.
Guay J, Kopp S. Peripheral nerve blocks for hip fractures in adults. Cochrane Database Syst Rev. 2020;11(11):CD001159.
Hebl JR, Dilger JA, Byer DE, Kopp SL, Stevens SR, Pagnano MW, et al. A pre-emptive multimodal pathway featuring peripheral nerve block improves perioperative outcomes after major orthopedic surgery. Reg Anesth Pain Med. 2008;33(6):510–7.
Memtsoudis SG, Poeran J, Cozowicz C, Zubizarreta N, Ozbek U, Mazumdar M. The impact of peripheral nerve blocks on perioperative outcome in hip and knee arthroplasty-a population-based study. Pain. 2016;157(10):2341–9.
Frassanito L, Vergari A, Zanghi F, Messina A, Bitondo M, Antonelli M. Post-operative analgesia following total knee arthroplasty: comparison of low-dose intrathecal morphine and single-shot ultrasound-guided femoral nerve block: a randomized, single blinded, controlled study. Eur Rev Med Pharmacol Sci. 2010;14(7):589–96.
Janiak M, Kowalczyk R, Gorniewski G, Olczyk-Miiller K, Kowalski M, Nowakowski P, Trzebicki J. Efficacy and side effect profile of intrathecal morphine versus distal femoral triangle nerve block for analgesia following total knee arthroplasty: a randomized trial. J Clin Med. 2022;11(23).
Sites BD, Beach M, Gallagher JD, Jarrett RA, Sparks MB, Lundberg CJF. A single injection ultrasound-assisted femoral nerve block provides side effect-sparing analgesia when compared with intrathecal morphine in patients undergoing total knee arthroplasty. Anesth Analg. 2004;99(5):1539–43.
Alvarez NER, Ledesma RJG, Hamaji A, Hamaji MWM, Vieira JE. Continuous femoral nerve blockade and single-shot sciatic nerve block promotes better analgesia and lower bleeding for total knee arthroplasty compared to intrathecal morphine: a randomized trial. BMC Anesthesiol. 2017;17(1):64.
Li XM, Huang CM, Zhong CF. Intrathecal morphine verse femoral nerve block for pain control in total knee arthroplasty: a meta-analysis from randomized control trials. Int J Surg. 2016;32:89–98.
Olive DJ, Barrington MJ, Simone SA, Kluger R. A randomised controlled trial comparing three analgesia regimens following total knee joint replacement: continuous femoral nerve block, intrathecal morphine or both. Anaesth Intensive Care. 2015;43(4):454–60.
Souron V, Delaunay L, Schifrine P. Intrathecal morphine provides better postoperative analgesia than psoas compartment block after primary hip arthroplasty. Can J Anaesth. 2003;50(6):574–9.
Kearns R, Macfarlane A, Grant A, Puxty K, Harrison P, Shaw M, et al. A randomised, controlled, double blind, non-inferiority trial of ultrasound-guided fascia iliaca block vs. spinal morphine for analgesia after primary hip arthroplasty. Anaesthesia. 2016;71(12):1431–40.
Kerr DR, Kohan L. Local infiltration analgesia: a technique for the control of acute postoperative pain following knee and hip surgery: a case study of 325 patients. Acta Orthop. 2008;79(2):174–83.
Seangleulur A, Vanasbodeekul P, Prapaitrakool S, Worathongchai S, Anothaisintawee T, McEvoy M, et al. The efficacy of local infiltration analgesia in the early postoperative period after total knee arthroplasty: a systematic review and meta-analysis. Eur J Anaesthesiol. 2016;33(11):816–31.
Rostlund T, Kehlet H. High-dose local infiltration analgesia after hip and knee replacement—what is it, why does it work, and what are the future challenges? Acta Orthop. 2007;78(2):159–61.
McCarthy D, McNamara J, Galbraith J, Loughnane F, Shorten G, Iohom G. A comparison of the analgesic efficacy of local infiltration analgesia vs. intrathecal morphine after total knee replacement: a randomised controlled trial. Eur J Anaesthesiol. 2019;36(4):264–71.
Essving P, Axelsson K, Aberg E, Spannar H, Gupta A, Lundin A. Local infiltration analgesia versus intrathecal morphine for postoperative pain management after total knee arthroplasty: a randomized controlled trial. Anesth Analg. 2011;113(4):926–33.
Tammachote N, Kanitnate S, Manuwong S, Yakumpor T, Panichkul P. Is pain after TKA better with periarticular injection or intrathecal morphine? Clin Orthop Relat Res. 2013;471(6):1992–9.
Kuchalik J, Granath B, Ljunggren A, Magnuson A, Lundin A, Gupta A. Postoperative pain relief after total hip arthroplasty: a randomized, double-blind comparison between intrathecal morphine and local infiltration analgesia. Br J Anaesth. 2013;111(5):793–9.
Rikalainen-Salmi R, Forster JG, Makela K, Virolainen P, Leino KA, Pitkanen MT, et al. Local infiltration analgesia with levobupivacaine compared with intrathecal morphine in total hip arthroplasty patients. Acta Anaesthesiol Scand. 2012;56(6):695–705.
Jia XF, Ji Y, Huang GP, Zhou Y, Long M. Comparison of intrathecal and local infiltration analgesia by morphine for pain management in total knee and hip arthroplasty: a meta-analysis of randomized controlled trial. Int J Surg. 2017;40:97–108.
Cai AL, Liu SJ, Wu B, Liu G. Intrathecal versus local infiltration analgesia for pain control in total joint arthroplasty. J Orthop Surg Res. 2020;15(1):110.
Qi BC, Yu J, Qiao WS. Comparison of intrathecal morphine versus local infiltration analgesia for pain control in total knee and hip arthroplasty: a meta-analysis. Medicine (Baltimore). 2020;99(36):e21971.
Toolyodpun S, Laoruengthana A, Kositanurit I, Podjanasupawun S, Saenghirunvattana C, Pongpirul K. Effect of multiple analgesic pathways including local infiltration analgesia, peripheral nerve blocks, and intrathecal morphine for controlling pain after total knee arthroplasty. Eur J Orthop Surg Traumatol. 2023;33(5):2129–35.
Kuchalik J, Magnuson A, Lundin A, Gupta A. Local infiltration analgesia: a 2-year follow-up of patients undergoing total hip arthroplasty. J Anesth. 2017;31(6):837–45.
Desousa K, Chandran R. Intrethecal Morphine for post operative analgesia: current trends. World J Anesthesia. 2014;3(3):191–202.
Author information
Authors and Affiliations
Contributions
P.P. wrote, reviewed and prepared main manuscript and tables and responded to revisions J.A. wrote, reviewed and prepared main manuscript and tables A.B. wrote, reviewed and prepared main manuscript and tables C.P. wrote and prepared main manuscript contributions.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Piennette, P., Ahn, J., Braun, A.S. et al. Current Review of the Use of Intrathecal Morphine for Postoperative Analgesia in Total Joint Arthroplasty. Curr Anesthesiol Rep 14, 83–89 (2024). https://doi.org/10.1007/s40140-023-00598-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-023-00598-6