Abstract
Purpose of Review
This review illustrates the incremental value of echocardiography as a bedsite tool for diagnosis and monitoring in critically ill patients with cardiopulmonary dysfunction. It provides practical guidance on the use of basic echocardiography in clinical scenarios frequently encountered in the ICU.
Recent Findings
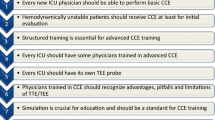
Echocardiography has become readily accessible to critical care physicians now and equipment is even been designed specifically for use in acute and critical care environments. The most important barrier to a more widespread implementation of this technique today, however, is the lack of training and experience. Indeed, proficiency is an absolute requirement for echo-based decision-making to positively impact on patient outcome.
Summary
Echocardiography has become an indispensable tool in the management of critically ill patients with severe cardiorespiratory conditions. It has the potential to become a game changer in ICU but current studies do not yet indicate a beneficial effect on outcome. It appears that structured training and certification in basic echocardiography are an absolute necessity to catalyze the widespread adoption and to guarantee the optimal use of ultrasound in the care of critically ill patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Echocardiography has acquired a central position in the daily care of critically ill patients. This non-invasive, mobile, safe, and relatively inexpensive imaging technique is ideally suited to provide real-time information on cardiac anatomy and function at the bedsite. Continuing investments in research and development of ultrasound (US)-based imaging have led recently to miniaturization of ultrasound equipment, the introduction of advanced imaging modalities, and an expansion of clinical applications, particularly in the field of perioperative medicine, emergency medicine, and critical care [1]. There are now a number of handheld ultrasound devices (HUD) that can be used to perform a basic cardiac ultrasound examination, with the ability to digitally store and upload images acquired on site. In a position statement of the European Association of Cardiovascular imaging, recommendations for the use of HUD, including nomenclature, appropriateness, indications, operators, clinical environments, data management and storage, educational needs, and training of potential users, were recently reviewed [2•]. The document also addresses current gaps in evidence, controversial issues, and future technological developments.
For the majority of patients in the ICU, transthoracic echocardiography is the preferred modality to perform a basic cardiac examination. Transesophageal echocardiography (TEE) is more invasive and is used when vital information can not be obtained via transthoracic windows or for specific indications [3]. Major complications due to insertion and manipulation of a transesophageal probe, such as esophageal perforation and severe bleeding, are rare but potentially lethal. A miniaturized, disposable TEE probe has been designed specifically for use in critical care settings. Insertion of this probe is less traumatic, and the device can be left indwelling for up to 72 h. However, the system is restricted to monoplane imaging with a limited set of views which do not meet the criteria outlined for a basic level echocardiography [4]. Its incremental value and its utility as a hemodynamic monitor in specific subgroups of critically ill patients are being investigated [5, 6].
The two primary indications for using echocardiography in the ICU are (1) life-threatening hemodynamic instability and (2) respiratory failure of unknown origin. It facilitates the differential diagnosis of shock, allowing faster identification and treatment of the underlying causes. With a limited set of imaging views, and a well-defined number of measurements, the majority of perioperative cardiovascular emergencies such as hypovolemia, pulmonary embolism (PE), myocardial ischemia, sepsis, and pericardial tamponade can be diagnosed through pattern recognition. In addition, basic echocardiography is increasingly being incorporated in routine practice as an extension of standard hemodynamic monitoring on the ICU.
Although numerous reports indicate the superior value of critical care echocardiography for cardiopulmonary assessment and diagnosis, beneficial effects on patient outcome are yet to be demonstrated [7]. In fact, the widespread adoption of ultrasound-based imaging outside traditional professional specialisms has raised concerns about potential harm associated with the lack of proficiency and inappropriate use of the technology. For this reason, high priority should be given to the implementation of training programs ensuring that learners are capable of demonstrating proficiency in echocardiographic image acquisition and interpretation in the clinical context of critical care and perioperative medicine [8,9,10].
A Systematic Approach to Cardiopulmonary Dysfunction
When life-threatening hemodynamic instability or respiratory failure occurs, the following approach may assist in ruling out the most prevalent causes:
-
1)
Check for the presence of pericardial fluid and look for external compression of any cardiac chamber to exclude cardiac tamponade
-
2)
Evaluate the right ventricle (RV) and left ventricle (LV): inspect chamber dimensions, wall thickness, atrial and interventricular septal position, and performance of both cardiac ventricles to exclude any form of cardiac dysfunction
-
3)
Check the volume status by evaluating chamber dimensions and assessing respiration-induced dynamic changes of the caval venous diameter
-
4)
Evaluate cardiac valves for stenosis and/or regurgitation. Valvular vegetations or prosthetic dysfunction should be addressed. If in doubt, call for advice from an expert in advanced echocardiography
-
5)
Look for additional pathologic structures such as thrombi (atrial or LV apex) and intimal flaps (aortic dissection), which need immediate treatment
Differential Diagnosis of Severe Hypotension Using a Simplified Algorithm (Fig. 1)
Echocardiography is able to improve diagnostic accuracy and efficiency in hemodynamically unstable patients and can reveal the etiology of unexplained hypotension in 48% of critically ill patients [12]. Again, a systematic and targeted approach may save time and various protocols have been suggested to achieve this. We recommend starting with a transgastric mid short axis (TG Mid SAX) or parasternal SAX view to estimate LV size and performance. Pericardial fluid can easily be detected in these views. The SAX views are useful to quickly assess volume status (LV End-diastolic area (EDA) or diameter (EDD)) and to quantify LV pump performance (measure LV End systolic area (ESA) or diameter (ESD)). From these variables, functional ejection parameters can be calculated with simple formulae as follows: fractional area change (FAC) = (EDA − ESA/EDA) and fractional shortening (FS) = (EDD − ESD/EDD). There are only a limited number of combinations in which the two variables (end-diastolic dimension and LV function) typically present and these are key to a rapid differential diagnosis of hypotension:
-
1)
Increased LV end-diastolic dimensions combined with decreased functional ejection parameters are indicative for LV failure. Etiologies for impaired left ventricular function are acute coronary syndrome and heart failure.
-
2)
Normal LV end-diastolic dimensions combined with increased or normal functional parameters suggest decreased systemic vascular resistance as the underlying cause of hypotension. These patients are likely to have sepsis as the underlying pathology.
-
3)
Decreased LV end-diastolic dimensions may result from 3 different conditions and prompt for further assessment of RV dimensions, as well as the position of the interventricular septum. For this purpose, the TG Mid SAX or left parasternal SAX and the 4-chamber views may be used. The following keys lead to further diagnosis:
-
3a) Normal or slightly decreased dimensions of the RV with neutral position of the interventricular septum suggests hypovolemia—by far the most prevalent cause of hypotension.
-
3b) Severely reduced dimensions of the RV with signs of displacement of the RV and right atrium are highly suggestive for tamponade. The diagnosis is confirmed when pericardial fluid can be visualized.
-
3c) Finally, increased RV dimensions and a leftward shift of the intraventricular septum indicate RV pressure overload, which in the perioperative setting is mostly caused by pulmonary arterial hypertension (PAH) or pulmonary embolus (PE).
-
Algorithm for the differentiation of hypotension. Modified from figure 22–8 in [11], with permission from McGraw-Hill Global Education Holdings, LLC. LV, left ventricle; LV EDA, left ventricular end-diastolic area; FS, fractional shortening; FAC, fractional area change; EF, ejection fraction; US, ultrasound; RV, right ventricle; RA, right atrium; IVS, interventricular septum
Other combinations may occasionally be seen but these are much less prevalent in the acute setting and have not been included in the algorithm to avoid complexity.
Common Causes of Hemodynamic Collapse in ICU Patients
Acute Coronary Syndrome
Echocardiography is extremely valuable in the intensive care setting for the fast diagnosis of acute coronary syndrome [12, 13]. The echocardiographic hallmark of myocardial ischemia is the presence of acute segmental wall motion abnormalities (SWMA). SWMA are defined as impaired systolic wall thickening and reduced endocardial inward motion in an ischemic coronary segment(s). The degree and extension of the wall motion abnormality depends on the severity and duration of ischemia and the location of the coronary artery occlusion. Global LV function should also be assessed in patients with acute myocardial ischemia. As a consequence of ischemic left ventricular dysfunction, dilatation of the mitral annulus combined with MV leaflet tethering often results in ischemic or functional MR [14]. The complete mitral valve apparatus should be assessed (leaflets, annulus, chordae, papillary muscles, and LV) to understand the underlying mechanism of an “ischemic” MR. In some patients, papillary muscle rupture or a ventricular septum defect can further complicate the clinical condition.
Heart Failure
LV dysfunction can be categorized into (a) systolic failure or pump dysfunction with the inability of the LV to generate adequate stroke volume and (b) diastolic dysfunction where adequate filling of the LV is not possible at low diastolic pressures [15]. Patients who exhibit heart failure with preserved EF frequently demonstrate abnormalities of LV diastolic function, i.e., impaired relaxation, increased stiffness, or a combination of both.
Global systolic function can be assessed by quantifying chamber dimensions (diameter, area, volume) and proportional changes in dimension over the cardiac cycle, i.e., fractional shortening, fractional area change, and ejection fraction at the uni-, bi-, or three-dimensional level respectively. Calculation of LV volumes and EF can be performed with 2D echo using Simpson’s method or with the use of three-dimensional echocardiography.
LV diastolic dysfunction is common in critically ill patients and is in fact an echocardiographic diagnosis [16]. Diastolic heart failure is present in about 50% of patients admitted with heart failure to the cardiology department where the diagnosis is confirmed when echocardiographic features of diastolic dysfunction are present in a symptomatic patient [17]. Patients with diastolic dysfunction often manifest signs of pulmonary congestion and dyspnea because the increased left atrial pressure or left ventricular diastolic pressure is transmitted backwards into the pulmonary circulation.
Echocardiography is considered the gold standard for the diagnosis of cardiac dysfunction and elevated filling pressures in critically ill patients. However, lung ultrasound may provide complementary information to diagnose interstitial syndrome or pulmonary edema [18]. Alveolar-interstitial syndrome is present when more than two B-lines are visible between two ribs at both sides of the anterior chest wall [19]. This pattern is also referred to as the B-profile. The presence of B-lines at the anterior chest wall indicates that filling pressures are high (pulmonary artery occlusion pressure > 18 mmHg) and that the origin of the dyspnea and/or hypotension is cardiac with a sensitivity and specificity of 93% [20]. In contrast, the presence of A-lines at the anterior chest wall (A-profile) indicates that left atrial pressures are low and fluid therapy can be initiated safely when deemed necessary [21••].
A simplified method can be used to categorize patients with diastolic dysfunction that may also assist with outcome prognostication. Tissue Doppler is used to quantify mitral annular plane peak velocities during early diastole (e′). A value of e′ < 10 cm/s is considered indicative for LV diastolic dysfunction. The ratio of peak mitral bloodflow velocity (E) and peak mitral annular plane velocity during early diastole, the E/e′ ratio, is used to grade diastolic dysfunction as follows: A ratio E/e′ < 8 indicates grade 1 diastolic dysfunction or a relaxation disorder, E/e′ between 9 and 12 indicates grade 2 diastolic dysfunction, and E/e′ > 13 indicates grade 3 or a restrictive pattern [22]. A higher E/e′ ratio is correlated to higher filling pressures and is significantly associated with weaning failure of critically ill patients [23, 24].
Hypovolemia and Fluid Responsiveness
Hypovolemia is a common cause of hypotension in the intensive care unit. It is typically associated with a small and hyperdynamic LV on echocardiography. The IVC diameter is small and varies with respiration [25]. Several techniques have been validated to objectively quantify LV chamber dimensions. However, these usually require several measurements of LV dimensions in short- and long-axis views to incorporate into a volume formula. This can be time consuming and probably adds little additional value over instant qualitative assessment or simple area measurements. The single best view for preload assessment is the TG SAX/parasternal SAX view to trace LV EDA. Normal LV EDA is typically 12 to 18 cm2 and < 12 cm2 is usually associated with hypovolemia. A 16% respiratory variation of LV EDA in SAX predicts fluid responsiveness in patients under mechanical ventilation [26, 27]. Another useful marker is ES cavity obliteration of the LV (i.e., kissing papillary muscles). However, 20% of cases with systolic cavity obliteration may occur in the setting of reduced afterload and/or increased ejection fraction (EF), in the absence of hypovolemia. Therefore, a keypoint is to evaluate both EDA and ESA since EDA is considered a sign of volume status while ESA is more indicative of changes in systemic vascular resistance. Furthermore, patients with chronic dilated cardiomyopathy may require more filling than patients with normal cardiac function, hence hypovolemia is more difficult to recognize in this situation. While LV EDA and ESA are obtained, FAC can be determined for the estimation of LV performance as hypovolemia is often associated with a hyperdynamic cardiac function.
Echocardiography is also helpful in predicting and optimizing the effects of volume replacement therapy. The variability of the IVC diameter in ventilated patients has been validated as a marker of fluid responsiveness [25, 27, 28]. A threshold of 12% change in diameter (maximum diameter − minimum diameter/mean diameter) is widely used as a positive predictor. Factors rendering this technique less reliable include inconsistent respiratory tidal volumes, cardiac arrhythmias, low lung compliance (as in ARDS), and open chest. An alternative test for fluid responsiveness is to observe the effect of a fluid bolus or passive leg raising (PLR) test on stroke volume and cardiac output (CO). During this test, the patient’s legs are raised from the supine position by which on average 300 ml of blood is transferred from the legs to the thorax. The effect of this fluid challenge on SV may be assessed by measuring LVOT velocity time integral (VTI) before and after leg raising. An increase of > 10% within a minute of performing the test is suggestive of fluid responsiveness. Importantly, echocardiography is the only technique that can rule out a false-positive diagnosis of fluid responsiveness when pulse pressure variation is due to RV failure [29•].
Cardiac Tamponade
Cardiac tamponade is a clinical syndrome caused by the accumulation of fluid in the pericardial space, resulting in reduced ventricular filling and hemodynamic compromise. The classical clinical signs of tamponade are those of hemodynamic shock combined with elevated systemic venous pressure, pulsus paradoxus, dyspnea, oliguria, and tachycardia.
Common causes of tamponade include iatrogenic lesions after cardiac surgery or intervention, trauma, ventricular rupture after acute myocardial infarction, aortic dissection, acute pericarditis, and malignancy.
The most sensitive echocardiographic manifestations of tamponade include early diastolic right ventricular collapse and late diastolic right atrial collapse in a patient who has a pericardial effusion. Obliteration of the LV cavity may be observed when ventricular filling is impaired. The presence of a large pericardial effusion may cause the heart to “swing” in the pericardial space. With the exception of postoperative cardiac surgical patients who may have loculated effusions or thrombi, the absence of demonstrable effusion on echocardiography excludes the diagnosis of tamponade. After cardiac surgery or in patients treated with an LV assist device, atypical findings are common, and tamponade should always be considered as a potential cause of hemodynamic instability [30, 31].
Pulmonary Embolism
A normal appearance of the heart on echocardiographic examination renders the possibility of acute PE extremely unlikely. Two important features of acute PE are (1) the presence of a thrombus in the right heart or pulmonary artery and (2) acute right ventricular dilatation and dysfunction. At least 30% obstruction of the pulmonary vasculature is required to produce RV dilation [32, 33]. Additionally, there is a variable increase in RV systolic pressure, as estimated by peak TR velocity with continuous wave Doppler. In most patients, TR gradients should be above 30 mmHg to indicate pulmonary arterial hypertension (PAH) due to PE. However, in the acutely failing RV, this pressure may only slightly be increased if cardiac output is low. High TR gradients > 45 mmHg may indicate chronic thromboembolic PAH, especially in the presence of right ventricular free wall hypertrophy which suggests long standing PAH. The inferior vena cava appears distended and shows no respiratory variation.
RV dilation may also result from cor pulmonale with PAH, RV infarction, or chronic PE. In addition, ventricular septal shift is commonly seen in acute PE and not in RV infarct [34]. A shift of the interventricular septum to the left, flattening the cross-section of the LV into a D-shape in SAX views, and paradoxical septal motion are important signs of acute RV pressure overload. The echocardiographic McConnell’s sign which describes a distinct regional wall motion abnormality with akinesia of the RV mid free wall with normal motion at the apex is particularly suggestive of PE [35]. Another sign is the 60/60 sign which indicates a tricuspid regurgitation (TR) pressure gradient less than 60 mmHg and a pulmonary acceleration time < 60 ms [36]. The coexistence of the McConnell sign together with the 60/60 sign appears to be a very useful echocardiographic criterion for right ventricular dysfunction due to PE [37].
Sepsis and Septic Shock
Sepsis is a leading cause of death in critically ill patients. Evaluation with TEE may be very useful in diagnosing sepsis and guiding fluid resuscitation as well as inotropic support. Adequately resuscitated patients with severe sepsis may present with a hyperdynamic circulation, a markedly reduced systemic vascular resistance, and high CO. Although CO may be normal or high in patients who have early septic shock, systolic function frequently is impaired. LV dysfunction defined as a LVEF of less than 45% was observed in about one-third of patients [38, 39]. Myocardial depression may become apparent only when afterload is restored with norepinephrine [40]. Diastolic dysfunction is also common in sepsis and is associated with increased mortality [41]. In patients who survive the episode of sepsis, cardiac dysfunction typically may resolve completely within 7–10 days. Sepsis-induced myocardial dysfunction is associated with poor outcomes, but the traditional measurement of LVEF does not directly correlate with prognosis. Global longitudinal strain utilizing speckle-tracking echocardiography seems to be a better marker of intrinsic LV function, reflecting myocardial deformation rather than displacement and volume changes. Lower values of global longitudinal strain are associated with higher mortality in patients with septic shock [42].
Endocarditis
Despite technical advances in TTE imaging techniques [43], TEE remains the preferred diagnostic test when there is a high clinical suspicion of infective endocarditis (IE) [44, 45]. IE may be suspected in a variety of clinical situations including heart failure, sepsis, cerebral embolism, pacemaker infection, a new regurgitant heart murmur, congenital heart disease, and new conduction abnormalities. All valves can be affected although pulmonary valve endocarditis is rare. The diagnosis of IE is based on the modified Duke criteria that integrate clinical, microbiologic, and echocardiographic data [46]. The presence of cardiac failure in a septic patient should raise the suspicion for the presence of IE. The echocardiographic hallmark of IE is a vegetation that usually is present on the upstream side of the affected cardiac valve. It may be difficult to differentiate vegetations from thrombi, Lambl’s excrescences, non-infective vegetations, and papillary fibroelastomas.
Left Ventricular Outflow Tract Obstruction (LVOTO)
LVOTO has been reported in 5–10% of hemodynamically unstable patients in the intensive care unit. It has been described in a number of clinical settings such as myocardial infarction, sepsis, cardiac tamponade, and post cardiac surgery. In susceptible patients, a decreased preload, decreased afterload, increased contractile state, and tachycardia may all lead to a dynamic LVOTO induced by a displacement of the anterior mitral valve. The decreased left ventricular outflow tract (LVOT) size and the higher velocity of blood flow through the LVOT may pull the anterior mitral valve leaflet into the outflow tract, causing systolic closure of the LV outlet and forcing blood backwards through the mitral valve. Hypovolemia and the use of inotropic support will often lead to refractory hypotension caused by this mechanism in susceptible patients. Anatomically susceptible patients are those with left ventricular hypertrophy and a large posterior leaflet of the mitral valve.
Measurements to predict LVOTO susceptibility are a posterior leaflet length > 15 mm, an anterior/posterior leaflet length ratio < 1,3, and a C-septal distance < 25 mm (distance between the systolic coaptation point and the most prominent part of the septum) [47, 48].
2D echocardiography will show the displacement of the anterior leaflet of the mitral valve in the apical/Mid-Esophageal (ME) 4- chamber view or in the left parasternal/ME Long-axis view. Color Doppler will reveal turbulent flow or flow acceleration in the LVOT and the presence of MR. A characteristic systolic late-peaking, dagger-shaped flow profile can be demonstrated by Continuous Wave (CW)-Doppler. The peak velocity can be used to calculate the maximum instantaneous pressure gradient across the LVOT. LVOTO is defined as an instantaneous peak Doppler LVOT pressure gradient of > 30 mmHg although higher gradients are often required to become hemodynamically important [49].
Mechanical Support: ECMO and LVAD
Echocardiography is an invaluable tool in the management and follow-up of patients treated with left ventricular assist devices (LVAD) or extra-corporeal membrane oxygenation (ECMO). Echocardiographic parameters and thresholds for successful ECMO weaning upon reduction of flows below 1.5 L/min include aortic VTI ≥ 10 cm, LVEF > 20–25%, and lateral mitral annulus peak systolic velocity > 6 cm/s [50]. A key element of LVAD physiology is the dynamic interplay between an unloaded left ventricle and the working, unassisted right ventricle. Echocardiography provides a direct window to this interaction and allows assessment of the RV while hemodynamic support is adjusted to optimize LVAD preload and systemic flows. Useful echocardiographic determinants of RV function include tricuspid annular plane systolic excursion (TAPSE), RV dimensions relative to LV size, and the position of the interventricular septum. The septum should remain in a neutral position or slightly deviated to the RV. More than moderate MR and an aortic valve that opens with every heartbeat are signs that are very suggestive for excessive LV preload and should prompt to increase the level of LVAD flow support [51••].
Conclusion
Echocardiography has become an indispensable tool in the management of critically ill patients with severe cardiorespiratory conditions. It provides point-of-care morphological and functional information of the cardiovascular system, superior to any standard hemodynamic monitor in the ICU. Recent data also confirm the diagnostic potential of lung ultrasound and recommend its use in conjunction with echocardiography. With basic imaging techniques and a limited set of views, echocardiography enables the rapid detection and differentiation of pathophysiological conditions causing hemodynamic and respiratory compromise. For advanced users, it provides a unique set of tools to perform detailed cardiovascular assessments to guide therapy and monitor its effect. If the benefits of echocardiography are to be translated into better patient outcomes on a widespread scale, formal comprehensive training is an absolute requirement. Indeed, the utility of echocardiography is directly related to operator proficiency and a lack of competence may even cause harm to patients if therapeutic decisions are based on erroneous echo diagnostics [7].
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Longobardo L, Zito C, Carerj S, Caracciolo G, Khandheria BK. Role of echocardiography in the intensive care unit: overview of the most common clinical scenarios. J Patient Cent Res Rev. 2018;5:239–43.
• Cardim N, Dalen H, Voigt J-U, Ionescu A, Price S, Neskovic AN, et al. The use of handheld ultrasound devices: a position statement of the European Association of Cardiovascular Imaging (2018 update). Eur Heart J Cardiovasc Imaging. 2019;20:245–52. A very important paper that addresses the most important aspects related to the use of handheld ultrasound devices. The authors provide guidance and recommendations as they recognize the potential benefit of partial focused ultrasound exams with these devices, but also caution against the drawbacks from inappropriate use of this technology.
Cheitlin MD, Armstrong WF, Aurigemma GP, et al. ACC/AHA/ASE 2003 guideline update for the clinical application of echocardiography--summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASE Committee to Update the 1997 Guidelines for the Clinical Application of Echocardiography). J Am Coll Cardiol. 2003;42:954–70.
Reeves ST, Finley AC, Skubas NJ, Swaminathan M, Whitley WS, Glas KE, et al. Basic perioperative transesophageal echocardiography examination: a consensus statement of the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr. 2013;26:443–56.
Hastie J, Panzer OPF, Weyker P, Flynn BC. Miniaturized echocardiography in the cardiac intensive care unit. J Cardiothorac Vasc Anesth. 2018;33:1540–7. https://doi.org/10.1053/j.jvca.2018.08.199.
Hlaing M, He J, Haglund N, Takayama H, Flynn BC. Impact of a monoplane hemodynamic TEE (hTEE) monitoring device on decision making in a heterogeneous hemodynamically unstable intensive care unit population: a prospective, observational study. J Cardiothorac Vasc Anesth. 2018;32:1308–13.
Singh K, Mayo P. Critical care echocardiography and outcomes in the critically ill. Curr Opin Crit Care. 2018;24:316–21.
Hernandez-Torres V, Prada G, Diaz-Gomez JL. Critical care echocardiography-embracing the future today. Int Anesthesiol Clin. 2019;57:75–88.
Cholley BP, Mayo PH, Poelaert J, et al. International expert statement on training standards for critical care ultrasonography. Intensive Care Med. 2011;37:1077–83.
Vieillard-Baron A, Mayo PH, Vignon P, et al. International consensus statement on training standards for advanced critical care echocardiography. Intensive Care Med. 2014;40:654–66.
Mathew J. Clinical manual and review of transesophageal echocardiography. Third Edition. New York: Mc Graw Hill; 2019. p. p591.
Shah BN, Ahmadvazir S, Pabla JS, Zacharias K, Senior R. The role of urgent transthoracic echocardiography in the evaluation of patients presenting with acute chest pain. Eur J Emerg Med. 2012;19:277–83.
Smith JS, Cahalan MK, Benefiel DJ, Byrd BF, Lurz FW, Shapiro WA, et al. Intraoperative detection of myocardial ischemia in high-risk patients: electrocardiography versus two-dimensional transesophageal echocardiography. Circulation. 1985;72:1015–21.
Poelaert JI, Bouchez S. Perioperative echocardiographic assessment of mitral valve regurgitation: a comprehensive review. Eur J Cardiothorac Surg. 2016;50:801–12.
Mebazaa A, Tolppanen H, Mueller C, Lassus J, DiSomma S, Baksyte G, et al. Acute heart failure and cardiogenic shock: a multidisciplinary practical guidance. Intensive Care Med. 2016;42:147–63.
Suarez JC, Lopez P, Mancebo J, Zapata L. Diastolic dysfunction in the critically ill patient. Med Int. 2016;40:499–510.
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF III, Dokainish H, Edvardsen T, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2016;17:1321–60.
Mojoli F, Bouhemad B, Mongodi S, Lichtenstein D. Lung ultrasound for critically ill patients. Am J Respir Crit Care Med. 2019;199:701–14.
Lichtenstein D, Mézière G, Biderman P, Gepner A, Barré O. The comet-tail artifact. Am J Respir Crit Care Med. 2012;156:1640–6.
Picano E, Pellikka PA. Ultrasound of extravascular lung water: a new standard for pulmonary congestion. Eur Heart J. 2016;37:2097–104.
•• Lichtenstein DA. Novel approaches to ultrasonography of the lung and pleural space: where are we now? Breathe. 2017;13:100–11. This review article updates the reader on the essential knowledge and skills required to practice lung ultrasound in the critically ill patient.
Swaminathan M, Nicoara A, Phillips-Bute BG, Aeschlimann N, Milano CA, Mackensen GB, et al. Utility of a simple algorithm to grade diastolic dysfunction and predict outcome after coronary artery bypass graft surgery. Ann Thorac Surg. 2011;91:1844–50.
Roche Campo F, Bedet A, Vivier E, Brochard L, Mekontso Dessap A. Cardiac function during weaning failure: the role of diastolic dysfunction. Ann Intensive Care. 2018;8:2.
de Meirelles Almeida CA, Nedel WL, Morais VD, Boniatti MM, de Almeida-Filho OC. Diastolic dysfunction as a predictor of weaning failure: a systematic review and meta-analysis. J Crit Care. 2016;34:135–41.
Barbier C, Loubières Y, Schmit C, Hayon J, Ricôme J-L, Jardin F, et al. Respiratory changes in inferior vena cava diameter are helpful in predicting fluid responsiveness in ventilated septic patients. Intensive Care Med. 2004;30:1740–6.
Cannesson M, Slieker J, Desebbe O, Farhat F, Bastien O, Lehot J-J. Prediction of fluid responsiveness using respiratory variations in left ventricular stroke area by transoesophageal echocardiographic automated border detection in mechanically ventilated patients. Crit Care. 2006;10:R171.
Charron C, Caille V, Jardin F, Vieillard-Baron A. Echocardiographic measurement of fluid responsiveness. Curr Opin Crit Care. 2006;12:249–54.
Vieillard-Baron A, Slama M, Cholley B, Janvier G, Vignon P. Echocardiography in the intensive care unit: from evolution to revolution? Intensive Care Med. 2008;34:243–9.
• Vignon P, Merz TM, Vieillard-Baron A. Ten reasons for performing hemodynamic monitoring using transesophageal echocardiography. Intensive Care Med. 2017;43:1048–51. This article pleads for a more liberal use of transesophageal echocardiography (versus the transthoracic or “surface” approach) in mechanically ventilated ICU patients. They list 10 convincing arguments to deviate from the formal indication (i.e., views not accessible, selective diagnostics) in this specific subgroup of patients where the potential (low) risk of a transesophageal approach is outweighed by the cited benefits.
Kronzon I, Cohen ML, Winer HE. Contribution of echocardiography to the understanding of the pathophysiology of cardiac tamponade. J Am Coll Cardiol. 1983;1:1180–2.
Fowler NO. Cardiac tamponade. A clinical or an echocardiographic diagnosis? Circulation. 1993;87:1738–41.
Wood KE. Major pulmonary embolism: review of a pathophysiologic approach to the golden hour of hemodynamically significant pulmonary embolism. Chest. 2002;121:877–905.
McIntyre KM, Sasahara AA. The hemodynamic response to pulmonary embolism in patients without prior cardiopulmonary disease. Am J Cardiol. 1971;28:288–94.
Kasper W, Geibel A, Tiede N, Bassenge D, Kauder E, Konstantinides S, et al. Distinguishing between acute and subacute massive pulmonary embolism by conventional and Doppler echocardiography. Br Heart J. 1993;70:352–6.
McConnell MV, Solomon SD, Rayan ME, Come PC, Goldhaber SZ, Lee RT. Regional right ventricular dysfunction detected by echocardiography in acute pulmonary embolism. Am J Cardiol. 1996;78:469–73.
Kurzyna M, Torbicki A, Pruszczyk P, Burakowska B, Fijałkowska A, Kober J, et al. Disturbed right ventricular ejection pattern as a new Doppler echocardiographic sign of acute pulmonary embolism. Am J Cardiol. 2002;90:507–11.
Kurnicka K, Lichodziejewska B, Goliszek S, Dzikowska-Diduch O, Zdończyk O, Kozłowska M, et al. Echocardiographic pattern of acute pulmonary embolism: analysis of 511 consecutive patients. J Am Soc Echocardiogr. 2016;29:907–13.
Vieillard-Baron A, Prin S, Chergui K, Dubourg O, Jardin F. Hemodynamic instability in sepsis: bedside assessment by Doppler echocardiography. Am J Respir Crit Care Med. 2003;168:1270–6.
Bouhemad B, Nicolas-Robin A, Arbelot C, Arthaud M, Féger F, Rouby J-J. Isolated and reversible impairment of ventricular relaxation in patients with septic shock. Crit Care Med. 2008;36:766–74.
Vieillard-Baron A, Caille V, Charron C, Belliard G, Page B, Jardin F. Actual incidence of global left ventricular hypokinesia in adult septic shock. Crit Care Med. 2008;36:1701–6.
Gonzalez C, Begot E, Dalmay F, et al. Prognostic impact of left ventricular diastolic function in patients with septic shock. Ann Intensive Care. 2016;6:36.
Sanfilippo F, Corredor C, Fletcher N, Tritapepe L, Lorini FL, Arcadipane A, et al. Left ventricular systolic function evaluated by strain echocardiography and relationship with mortality in patients with severe sepsis or septic shock: a systematic review and meta-analysis. Crit Care. 2018;22:183.
Reynolds HR, Jagen MA, Tunick PA, Kronzon I. Sensitivity of transthoracic versus transesophageal echocardiography for the detection of native valve vegetations in the modern era. J Am Soc Echocardiogr. 2003;16:67–70.
Habib G, Badano L, Tribouilloy C, et al. Recommendations for the practice of echocardiography in infective endocarditis. Eur J Echocardiogr. 2010;11:202–19.
Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Guyton RA, et al. 2014 AHA/ACC Guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:e521–643.
Durack DT, Lukes AS, Bright DK. New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Duke Endocarditis Service. Am J Med. 1994;96:200–9.
Maslow AD, Regan MM, Haering JM, Johnson RG, Levine RA. Echocardiographic predictors of left ventricular outflow tract obstruction and systolic anterior motion of the mitral valve after mitral valve reconstruction for myxomatous valve disease. J Am Coll Cardiol. 1999;34:2096–104.
Ibrahim M, Rao C, Ashrafian H, Chaudhry U, Darzi A, Athanasiou T. Modern management of systolic anterior motion of the mitral valve. Eur J Cardiothorac Surg. 2012;41:1260–70.
Slama M, Tribouilloy C, Maizel J. Left ventricular outflow tract obstruction in ICU patients. Curr Opin Crit Care. 2016;22:260–6.
Zhang Z. Echocardiography for patients undergoing extracorporeal cardiopulmonary resuscitation: a primer for intensive care physicians. J Intensive Care. 2017;5:15.
•• Bouchez S, Van Belleghem Y, De Somer F, De Pauw M, Stroobandt R, Wouters P. Haemodynamic management of patients with left ventricular assist devices using echocardiography: the essentials. Eur Heart J Cardiovasc Imaging. 2019;20:373–82. This article provides comprehensive instructions on the use of echocardiography as a base for decision-making in a challenging clinical context. The number of patients treated with mechanical support systems is increasing, yet there is very little supportive educational guidance in today’s scientific literature.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Stefaan Bouchez and Patrick F. Wouters declare they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Critical Care Anesthesia
Rights and permissions
About this article
Cite this article
Bouchez, S., Wouters, P.F. Echocardiography in the Intensive Care Unit. Curr Anesthesiol Rep 9, 360–367 (2019). https://doi.org/10.1007/s40140-019-00336-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-019-00336-x