Abstract
Purpose of Review
Since healthcare costs have continued to rise, health-economic approaches in perioperative medicine tend to create potential benefits. However, a review of the perioperative literature reveals that there are only few published economic analyses. The aim of the present review is to explore the health-economic researches in the field of perioperative medicine.
Recent Findings
In perioperative medicine, cost-effectiveness is the most represented method of health-economic analysis. The recent CHEERS statement enables a critical appraisal of health-economic papers. Conducting systematic reviews of economic evaluations has been also reviewed. Costs and costing methods according to the type of approach retained, along with the three important steps in costing, have evolved. The costing principles and costing process, as well as the gross costing and microcosting approaches are becoming more detailed. Between the top-down and bottom-up approaches, several methods of measuring the costs have been proposed, considering the level of accuracy of the cost measurement. The “outside –In” approach, combining the two former approaches, has been newly introduced. The methods available to calculate the cost of an act either consider the accuracy in identifying the resources or the accuracy of valorizing the resources.
Summary
Important costs are attached to the perioperative period. Thus, a health-economic approach is particularly valuable in this context. Health-economic analysis provides tools to orient decision-making in order to better use the available resources. Anesthesiologists should seize the health-economic concepts and methods to better guide their medical decision and orient their policymaking in the domain of perioperative medicine.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Perioperative medicine describes the medical care of patients from the preoperative period, through the operative period to full recovery [1, 2•]. Although it does not include the surgery procedure itself, it includes patient prepared for surgical care, having and recuperating from surgery. The surgeon, anesthesiologist, intensivist, and medical consultant work together. The medical knowledge necessary to this field includes preoperative risk, operating risk and complications, looking for patient at risk, developing methods to reduce the risk, detecting and reporting outcome rates of complications, and harmonizing specific management of medical illness during this time period [3, 4]. Methods supporting best practices in perioperative medicine are expanding as well as standardizing outcomes measures [5••, 6•]. Since important costs are attached to the perioperative period, a health-economic approach is thus particularly valuable in this context [7••, 8••].
The importance of considering conditions which may impact perioperative medicine can be illustrated for instance by patients presenting with chronic kidney disease (CKD). As a matter of fact, CKD should not only be regarded as a marker of increased perioperative risk of morbidity. It is also a key indicator for perioperative medicine as a preventive translational specialty [9]. Mases et al. recently added consistent information to the perioperative literature outlining chronic kidney disease as an important source of postoperative morbidity [10]. In a cost-effectiveness analysis, Komenda et al. [11] showed that screening for CKD is suggested to be cost-effective in patients with diabetes and hypertension and may be cost-effective as well in populations with higher incidences of CKD, rapid rates of progression, and more effective drug therapy. Accurate risk prediction of end-stage renal disease may improve clinical planning, outcomes, and resource allocation [12•, 13]. These considerations offer new pathways for integrating perioperative medicine and health-economic approaches [14•].
We reviewed the works published in the field of health-economy and perioperative medicine. We present the main types of study design. We address the critical appraisal of health-economic papers and systematic reviews for economic studies. Then we define cost and costing and the main steps to follow. Finally, we introduce the different types of costing approaches.
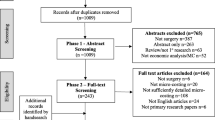
Few Published Works
Economic evaluation is the comparative analysis of alternative courses of action in terms of both their costs and their consequences. It requires collecting items such as resource use, costs, preference-related information, or cost-effectiveness results. Since healthcare costs have continued to rise, health-economic approaches tend to create potential benefits. However, surveys of perioperative literature reveal very few published economic analyses [15–17•]. Since evidence-based best practice and pay for performance are focused toward patient-centered care and cost-effective management, including the tools and methodologies of health-economics appears determinant for orienting public health decision-making [18].
An Evidence-Based Bibliographic Approach
An evidence-based approach through a bibliographic search on the specific subject of perioperative medicine and health-economy shows that today the development of these two conjugated themes gives restricted results [17•]. For instance, the terms gross costing or microcosting are not even listed in the Medical Subject Headings (MeSH). However, the main types of economic analyses are represented.
Health-Economic Analysis
Medico-economic analysis is schematically based on four types of analysis: (i) cost minimization, (ii) cost-benefit, (iii) cost-effectiveness, and (iv) cost-utility [17•, 19].
-
(i)
Cost minimization analysis is used to measure and compare the costs of different medical interventions. A limitation of the method is that the consequences of compared interventions are required to be equivalent, and only relative costs are compared. It is used for instance in pharmaco-economics studies to compare the cost per course of treatment when alternative therapies have demonstrably equivalent clinical effectiveness. Thus, it calculates costs to project the least costly drug or therapeutic modality. We did not find any study of this type in perioperative medicine published within the past year.
-
(ii)
Cost-benefit analysis is used to value both incremental costs and outcomes in monetary terms. It thus requires the effects of interventions to be transformed into monetary unit equivalents. However, converting benefits into monetary unit equivalents may be debatable. It allows a direct calculation of the net monetary cost of achieving a health outcome. For instance, a survival gain in life years may be considered as the cost of the productive value to society of that life year using, for example, the average wage. Methods are thus necessary for valuing gains in quality of life. It may be for instance the willingness-to-pay. It evaluates the amount that individuals would be willing to pay for a given quality-of-life benefit.
-
(iii)
Cost-effectiveness analysis is a method for assessing the gains in health relative to the costs of different health interventions [20, 21]. It enables weighing different costs and health outcomes and thus is an aid to policy makers. It is the “price” of achieving health improvements through different kinds of interventions and thereby helps policy makers make decisions that get the most out of their financial resources. It is the analysis most frequently performed.
The incremental cost-effectiveness ratio (ICER) summarizes the cost-effectiveness of a health care intervention. It is defined as the difference in cost between a new technology and the standard of care, divided by the difference in their effect, i.e., the outcomes between the new technology studied vs the standard of care (whether identifiable). It represents the average incremental cost associated with one additional unit of the measure of effect. The ICER is used for instance in cost-utility analysis, where it corresponds to the cost per quality-adjusted life year (QALY) gained. The incremental cost per incremental outcome between competing alternatives is considered. The value of the outcomes is incorporated into the analysis.
For clinicians, an ICER is not a concept difficult to grasp [22]. However, this ratio has three limitations. One cannot include more than one clinical outcome in the ICER at a time. Moreover, in clinical studies, there are often several benefits and risks of relevance when choosing between alternatives. Lastly, it is not possible to compare ICERs across interventions with different benefits. Practically, it means that if different economic analyses report different metrics, (e.g., cost per acute renal failure avoided versus cost per life year gained), there is no common metric to share. It thus does not allow selecting the best alternative use of resources.
Sadique et al. conducted a study in order to evaluate the cost-effectiveness of perioperative cardiac output-guided hemodynamic therapy versus usual care in high-risk patients undergoing major gastrointestinal surgery. The authors undertook a cost-effectiveness analysis from a multicenter randomized trial performed in the United Kingdom. They reported quality-adjusted life years (QALYs); each QALY was valued using the National Institute for Health and Care Excellence recommended threshold of willingness to pay (£20,000 per QALY) in conjunction with the costs of each group to report the incremental net monetary benefits of the treatment algorithm versus usual care.
From January 2007 through December 2011, Kim et al. performed a cost-effectiveness analysis of robotic surgery (RS) compared with laparoscopic surgery (LS) for rectal cancer [23], 311 and 560 patients underwent totally RS and conventional LS, respectively. A propensity score-matching analysis was performed with a ratio of 1:1 to reduce the possibility of selection bias. Costs and perioperative short-term outcomes were compared. Additional costs due to readmission were also analyzed. Robotic surgery showed the similar short-term outcomes with higher costs than laparoscopic surgery. Cost-effectiveness focusing on short-term perioperative outcomes of robotic surgery was thus not demonstrated in this study.
Makhni and colleagues [24•] outlined the heterogeneity of methodological reporting of cost-effectiveness studies in orthopedic surgery. The results of cost-effectiveness studies are either unreliable or heavily dependent on sensitivity analyses of the findings from the source studies. Interpreting the conclusions of cost-effectiveness studies needs high-quality primary-source data and appropriate methodology. Of the 79 articles included in the study, 63 % provided strong recommendations, whereas 37 % provided weak recommendations. Methodological reporting varied greatly. Clearly defined intervention, adequate description of a comparator, definition of the study perspective, reported discount rate for future costs, quality-adjusted life years or sensitivity analysis were often inhomogeneous or inappropriate.
Prior to making decision from the results of cost-effectiveness analysis one has to assess whether the calculated ratios would differ substantially in his/her country because prices, demographics, epidemiology, or service coverage may differ significantly from the country where the study has been conducted.
-
(iv)
Cost-utility analysis is used to determine the cost in terms of utilities, especially quantity and quality of life. Multiple outcomes (benefits and risks) may be incorporated into one-single metric, most commonly the quality-adjusted life years (QALY). However, it may be difficult to put a value on a health status or an improvement in health status as perceived by different individuals or societies. It can be used for instance to compare two different drugs or procedures whose benefits may be different
Thus, Manchikanti and colleagues [25] assessed the cost-utility of percutaneous adhesiolysis procedures in managing chronic low back and lower extremity pain secondary to postlumbar surgery syndrome and lumbar central spinal stenosis. Two controlled studies were conducted assessing the clinical effectiveness of percutaneous adhesiolysis for postlumbar surgery syndrome and lumbar central spinal stenosis in an interventional pain management. The cost-utility analysis was performed with direct payment data over a 2-year period. Outcome measures were defined as at least 50 % improvement with reduction in pain and disability status.
Critical Appraisal of Health-Economic Papers and Systematic Reviews
The Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement proposes an update of previous health-economic evaluation guidelines to optimize reporting of health-economic evaluations. [26••] The recommendations are summarized in a 24-item checklist. Recommendations of the minimum set of reporting items were developed through a modified Delphi panel process. This statement provides a helpful checklist to guide reading articles in the field of health-economic.
Conducting a systematic review of economic evaluations still needs defining guidelines. A working group proposed a review of the literature on the utility/futility of systematic reviews of economic evaluations, as well as an assessment of the critical appraisal tool in the existing Joanna Briggs Institute guidance for health intervention cost-effectiveness against criteria that promotes validity in economic evaluation research [27••]. Nevertheless, some aspects need further improvement such as separating out questions addressing intervention cost and effectiveness measurement, and assessing generalizability of findings.
Xu et al. [28••] conducted a review of the current literature on microcosting studies of health and medical interventions, strategies, and programs. They assessed the variation in microcosting methodology and the quality of existing studies. Their objectives were to help standardizing methods and techniques for conducting and reporting microcosting studies. It was, conceived as an aid to improve the quality and transparency of studies and enhance comparability and interpretation of findings.
All these studies are oriented toward fostering clinical and health policy decision-making about resource allocation. The comprehension of the way the costs are estimated is an important step in better understanding health-economic approaches.
Cost and Costing
The cost of goods is not an intrinsic characteristic of an object or a product itself, but it derives from calculation based on a theory and conventions. A cost can only be set if one makes a choice on the specific point of view retained, the extent of the scope to explore, the purpose of the study, and the time horizon to adopt. [29] Costing is approached according to the point of view adopted. Several points of view may differ along with the perspective of the retained analysis: the payer (a tariff, for instance, Diagnosis-Related Groups are the basis of the national tariff defined by the National Insurance Service for acute hospital care in France), the patient (out of the pocket), the care provider (mobilized expenditures for the realization of an act), the family (sick leave, financial aid, and illness contracted by a loved one), or the society. The cost differs according to each point of view.
Measuring the costs may have several purposes. When introducing an innovative technology, it is for instance, estimating a new pricing for an act or a procedure. It may be an incentive lever of medical practices in order to homogenize the practices and optimize medical care. It enables evaluating the cost of production of an act in the international context, thus avoiding the pitfall of the specificity of the reimbursement system.
Costing Principles and Costing Process
Six costing principles have been proposed by the NHS and described as follows [30••]: (i) the stakeholder engagement; effective costing requires input from a wide range of stakeholders, including frontline clinical staff and departments providing clinical support services such as pathology. (ii) Consistency; a consistent approach to costing is required across and within organizations. (iii) Data accuracy; accurate costing relies on the quality and coverage of the underlying data input. (iv) Materiality; costing effort should focus on material costs and activities. (v) Causality and objectivity: costing should be based on an understanding of how resources are used during the patient care pathway, to minimize subjectivity. (vi) Transparency: costing processes and outputs should be transparent and auditable.
The costing process includes several steps. For instance, the NHS has proposed six steps [31••]: (i) Defining the patient care to be costed, (ii) Identifying the activities, (iii) Identifying the relevant costs, (iv) Classifying the costs, (v) Assigning the costs, and (vi) Validating the outputs. All these steps are essential and detailed in the NHS guidance. [31••] In any case, one must be aware that the choices retained may hamper the generalizability/comparability of the results.
Identification, measurement, and valuation are three important steps in costing. What to include in costing depends on the objective of the study. It may be costing quality-adjusted life years (QALYs) with standardized approaches for “reference cases.” Measuring the resource changes may target the amounts of labor input or output, patients’ or carers’ time. Valuation of the resource effects is proposed if prices are available and reflect the costs. However, in some situation either prices do not exist for the relevant changes, or available prices do not reflect the societal value of resources. Several methods are proposed for adjusting prices in order to better cope with the resource used from a societal standpoint [32].
Gross Costing and Microcosting
Two types of costing are generally described. Gross costing, also referred as top-down costing, allocates a total budget to specific services such as hospital stays or doctors’ visits according to predefined rules. It uses apportionment to distribute costs to activity, and it gives average unit costs thus simplifying the costing. However, gross costing may mask variation in clinical practice or resource use. Classically, for the gross costing approach, the cost factors are defined at a supra-individual level. The gross-costing approach calculates an average cost from the total amount of charges on the basis of accounting aggregates [33]. Over a long period, the gross costing approach divides the total cost by the total units of care provided.
The microcosting approach is defined as a method for determining the cost of each resource mobilized for making a benefit or providing a service. It refers to calculating unit costs on the basis of the resources spent by patients. The cost factors are defined at the patient level. The microcosting approach determines each input, find its price, and then sum (quantity by price) across all inputs. Estimating the cost of new technologies or community-based interventions, producing estimates in studies including nonmarket goods, or studying within-procedure cost variation can be approached through microcosting studies [34].
Microcosting is a basis of a broader method named activity-based costing (ABC). It has been defined by the Chartered Institute of Management Accountant (CIMA) as ‘an approach to the costing and monitoring of activities which involves tracing resource consumption and costing final outputs. Resources are assigned to activities, and activities to cost objects based on consumption estimates. The latter utilizes cost drivers to attach activity costs to outputs’. (CIMA Official Terminology, 2005). [35] An activity is defined as a measurable amount of work performed by resources to deliver elements of patient care. This method assigns more indirect costs (overheads) into direct costs compared to conventional methods. Splitting costs help identifying factors (cost drivers) that create or drive the cost of the activity. The ABC method helps allocating more resources on profitable products or activities. It affords a better management, helps calculating costs more accurately or evaluating and justifying investments in new technologies.
Between the top-down and bottom-up approaches, several methods of measuring the costs have been proposed considering the level of accuracy of the cost measurement [36, 37]. These two methods are not irreconcilable [38•]. Thus, it is possible to incorporate an approach combining the two, referred to as the “outside –In” approach. The methods available to calculate the cost of an act, either consider the accuracy in identifying the resources or the accuracy of valorizing the resources [39••].
Conclusion
The demand of care is increasing. However, healthcare resources are not unlimited. Innovative technologies, new procedures, new treatment approaches improve prevention, diagnosis, treatment, and prognosis. Health-economic analysis provides tools to orient decision-making in order to better use the available resources. Anesthesiologists should seize the health-economic concepts and methods to better guide their medical decision and orient their policymaking in the domain of perioperative medicine.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Rock P. The future of anesthesiology is perioperative medicine. Anesthesiol Clin North America. 2000;18(3):495–513 v.
• Kain ZN, Fitch JC, Kirsch JR, Mets B, Pearl RG. Future of anesthesiology is perioperative medicine: a call for action. Anesthesiology. 2015;22(6): 1192–5. As stated: a call for action.
Dutta S, Cohn SL, Pfeifer KJ, Slawski BA, Smetana GW, Jaffer AK. Updates in perioperative medicine. J Hosp Med. 2016;11(3):231–6.
Le Manach Y, Collins G, Rodseth R, Le Bihan-Benjamin C, Biccard B, Riou B, Devereaux PJ, Landais P. Preoperative score to predict postoperative mortality (POSPOM): derivation and Validation. Anesthesiology. 2016;124(3):570–9.
•• Jammer I, Wickboldt N, Sander M, Smith A, Schultz MJ, Pelosi P, Leva B, Rhodes A, Hoeft A, Walder B, Chew MS, Pearse RM; European Society of Anaesthesiology (ESA) and the European Society of Intensive Care Medicine (ESICM); European Society of Anaesthesiology; European Society of Intensive Care Medicine. Standards for definitions and use of outcome measures for clinical effectiveness research in perioperative medicine: European Perioperative Clinical Outcome (EPCO) definitions: a statement from the ESA-ESICM joint taskforce on perioperative outcome measures. Eur J Anaesthesiol. 2015;32(2):88–105. Definition of standards for clinical effectiveness research in perioperative medicine.
• Neuman MD, Fleisher LA. Evaluating outcomes and costs in perioperative care. JAMA Surg. 2013;148(10):905–6. Cost-effectiveness of health care in the United States vs Europe.
•• Raphael DR, Cannesson M, Rinehart J, Kain ZN. Health Care Costs and the Perioperative Surgical Home: A Survey Study. Anesth Analg. 2015;121(5):1344–9. Assessing anesthesiologists’ views of their own importance in cost-reduction strategies. A cross-sectional survey in the US.
•• Szokol JW1, Stead S. The changing anesthesia economic landscape: emergence of large multispecialty practices and Accountable Care Organizations. Curr Opin Anaesthesiol. 2014;27(2):183–9. Analyzing the impact of the Accountable Care Organizations and the reimbursement of the anesthesiologists along with the consequences in their involvement in perioperative patient care and outcomes.
Ackland GL, Laing CM. Chronic kidney disease: a gateway for perioperative medicine. Br J Anaesth. 2014;113(6):902–5.
Mases A, Sabate S, Guilera N, et al. Preoperative estimated glomerular filtration rate and the risk of major adverse cardiovascular and cerebrovascular events in non-cardiac surgery. Br J Anaesth. 2014;113:644–51.
Komenda P, Ferguson TW, Macdonald K, Rigatto C, Koolage C, Sood MM, Tangri N. Cost-effectiveness of primary screening for CKD: a systematic review. Am J Kidney Dis. 2014;63(5):789–97.
• Ferguson TW, Tangri N, Rigatto C, Komenda P. Expert Rev Pharmacoecon. Cost-effective treatment modalities for reducing morbidity associated with chronic kidney disease. Outcomes Res. 2015;15(2):243–52. A working example: cost-effective treatments and reduction of CKD morbidity.
Roggeri DP, Mazzaferro S, Brancaccio D, Cannella G, Messa P, Di Luca M, Morosetti M, Costanzo AM, di Luzio Paparatti U, Cornago D, Cozzolino M, FARO Study Group. Pharmacological control of secondary hyperparathyroidism in hemodialysis subjects: a cost consequences analysis of data from the FARO study. J Med Econ. 2012;15(6):1110–7.
• Grocott MP, Mythen MG. Perioperative medicine: The value proposition for anesthesia?: a uk perspective on delivering value from anesthesiology. Anesthesiol Clin. 2015;33(4):617–28. Key opportunities for adding value in the perioperative journey are suggested: collaborative decision-making, lifestyle modification before surgery, standardization of in-hospital perioperative care, achieving full recovery after surgery, and the use of data for quality improvement.
Meltzer D. Economic analysis in patient safety: a neglected necessity. BMJ Qual Saf. 2012;21:443–5.
Etchells E, Koo M, Daneman N. Comparative economic analyses of patient safety improvement strategies in acute care: a systematic review. BMJ Qual Saf. 2012;21:448–56.
• Martin J, Cheng D. Role of the anesthesiologist in the wider governance of healthcare and health economics. Can J Anaesth. 2013;60(9):918–28. How to allocate limited resources across unlimited demands in order to maximize health gains per resource expended.
Lindenauer P. Public reporting and pay-for-performance programs in perioperative medicine: are they meeting their goals? Cleve Clin J Med. 2009;76(Suppl 4):S3–8.
Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the economic evaluation of health care programmes. 3rd ed. United Kingdom: Oxford University Press; 2005.
Gold MR, Siegel JE, Russell LB, Weinstein MC, editors. Cost-effectiveness in health and medicine. New York: Oxford University Press; 1996.
Cost-Effectiveness Analysis. Chapter 3. In: Jamison DT, Breman JG, Measham AR, et al., editors. Priorities in health. Washington (DC): World Bank; 2006.
Hoch JS, Dewa CS. A clinician’s guide to correct cost effectiveness analysis: think incremental not average. Can J Psychiatry. 2008;53:267–74.
Kim CW, Baik SH, Roh YH, Kang J, Hur H, Min BS, Lee KY, Kim NK. Cost-effectiveness of robotic surgery for rectal cancer focusing on short-term outcomes: a propensity score-matching analysis. Medicine (Baltimore). 2015;94(22):e823.
• Makhni EC, Steinhaus ME, Swart E, Bozic KJ. What Are the Strength of Recommendations and Methodologic Reporting in Health Economic Studies in Orthopaedic Surgery? Clin Orthop Relat Res. 2015;473(10):3289–96. Orthopaedic and Recommendations as well as Methodologic Reporting in Health Economic Studies.
Manchikanti L, Helm S 2nd, Pampati V, Racz GB. Cost utility analysis of percutaneous adhesiolysis in managing pain of post-lumbar surgery syndrome and lumbar central spinal stenosis. Pain Pract. 2015;15(5):414–22.
•• Consolidated Health Economic Evaluation Reporting Standards (CHEERS)–explanation and elaboration: a report of the ISPOR Health Economic Evaluation Publication Guidelines Good Reporting Practices Task Force. Value Health. 2013;16(2):231–50. Health Economic Evaluation Reporting Standards: essential.
•• Gomersall JS, Jadotte YT, Xue Y, Lockwood S, Riddle D, Preda A. Conducting systematic reviews of economic evaluations. Int J Evid Based Healthc. 2015;13(3):170–8. A guidance for systematic reviews of economic evaluation.
•• Xu X, Nardini HKG, Ruger JP. Micro-costing studies in the health and medical literature: protocol for a systematic review. Syst Rev 2014;3:47.Specific article for discerning reader.
Launois R, Vergnenègre A, Garrigues B. Costs, costs and more costs: which one should we use? Bull Cancer. 2003;90(11):946–54.
•• https://www.google.fr/search?q=nhs+costing+manual+2015&ie=utf-8&oe=utf-8&client=firefox-b&gfe_rd=cr&ei=eDwyV5-uHofF8Afn44GADA. Accessed 10 May 2016. The basic concepts of costing.
•• https://www.hfma.org.uk/our-work/costing/clinical-costing-standards. Accessed 10 May 2016. The HFMA clinical costing standards and guidance papers form part of Monitor’s Approved costing guidance which sets out the costing approach that Monitor recommends providers of NHS services adopt.
Raftery J. Costing in economic evaluation. BMJ. 2000;320(7249):1597.
Clement Nee Shrive FM, Ghali WA, Donaldson C, Manns BJ. The impact of using different costing methods on the results of an economic evaluation of cardiac care: microcosting vs gross-costing approaches. Health Econ. 2009;18:377–88.
Frick KD. Micro-Costing Quantity Data Collection Methods Med Care. 2009;47(7 Suppl 1):S76–81.
http://www.cimaglobal.com/Documents/…/MigratedDocsMarch2010/Resouces%20(pdfs)/Topic%20gateways/Activity%20based%20costing.pdf. Accessed 10 May 2016.
Smith MW, Barnett PG. Direct measurement of health care costs. Med Care Res Rev. 2003;60(3 Suppl):74S–91S.
www.herc.research.va.gov/files/book_458.pdf. Accessed 10 May 2016
• Wilson EC, Mugford M, Barton G, Shepstone L. Efficient research design: using value-of-information analysis to estimate the optimal mix of top-down and bottom-up costing approaches in an economic evaluation alongside a clinical trial. Med Decis Making. 2016;36(3):335–48. Value-of-information analysis and combination of bottom-up and top-down approaches.
•• Tan SS, Rutten FF, van Ineveld BM, Redekop WK, Hakkaart-van Roijen L. Comparing methodologies for the cost estimation of hospital services. Eur J Health Econ 2009;10: 39–45. A methodological point of view: an essential reading.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Paul Landais, Sihame Chkair, Thierry Chevallier, Mariella Lomma, Yannick Le Manach, and Jean-Pierre Daurès declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Research Methods and Statistical Analyses.
Rights and permissions
About this article
Cite this article
Landais, P., Chkair, S., Chevallier, T. et al. Health-Economic Researches in Perioperative Medicine. Curr Anesthesiol Rep 6, 299–304 (2016). https://doi.org/10.1007/s40140-016-0173-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-016-0173-6