Abstract
Purpose of Review
The significance of stroke in the noncardiac, nonneurologic, and nonvascular perioperative setting has been routinely underestimated. A complex interplay of multiple perioperative, patient, and surgical factors is involved in the pathogenesis of perioperative stroke. Multiple risk reduction strategies are required to decrease the incidence of this devastating complication.
Recent Findings
Recent evidence demonstrates that one in every 1000 patients undergoing low-risk surgery may develop perioperative stroke which can result in significant morbidity or mortality. The incidence of covert stroke is much higher. Further, it is now established that the majority of strokes do not occur during or immediately after surgery but at least 24 h later—thus emphasizing the need for active surveillance.
Summary
A high index of suspicion throughout the perioperative period, prompt diagnosis, and immediate management based on a multidisciplinary protocol is the key for successful outcome. In this article, we review recent evidence pertaining to this topic. We also suggest a model clinical care pathway for institutional management of perioperative stroke that could form the basis of multidisciplinary care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stroke is an acute focal injury of the central nervous system due to a vascular cause, either infarction or hemorrhage [1]. In-hospital stroke is associated with worse outcomes compared to community-onset stroke, and, in one study, surgical patients represented almost 50 % of all in-hospital strokes [2]. Although well recognized in the cardiac, neurologic, and vascular surgery settings, perioperative stroke in the context of noncardiac, nonneurological surgery has not been as thoroughly studied. Current evidence indicates that perioperative stroke in the noncardiac, nonneurologic surgical setting is a distinct clinical entity associated with higher morbidity and hospital length of stay, and up to an 8-fold increase in mortality compared to patients not suffering stroke [3]. The purpose of this article is to review the current evidence on perioperative stroke in the noncardiac, nonneurologic setting, with particular emphasis on the consensus recommendations for perioperative care of patients at risk for stroke by the Society for Neuroscience in Anesthesiology and Critical Care (SNACC) [4••].
Definition
Until recently, there was no universally accepted definition for perioperative stroke. Consequently, there was wide variation in the reported incidence, risk factors, and management of this event. The SNACC consensus statement has provided a standardized definition of perioperative stroke: “a brain infarction of ischemic or hemorrhagic etiology that occurs during surgery or within 30 days after surgery” [4••]. The American Heart Association (AHA)/American Stroke Association (ASA) definition for CNS infarction is “Brain, spinal cord or retinal cell death attributable to ischemia based on neuropathological, neuroimaging, and/or clinical evidence of permanent injury” [1].
Incidence
There is wide variation in the reported incidence of perioperative stroke because of the lack of a standardized definition, low incidence, and difficulty recognizing stroke in the perioperative setting. Furthermore, unlike perioperative myocardial infarction, there is also a lack of easily accessible biomarkers, further complicating the recognition of stroke in the postoperative patient [3, 5••]. Table 1 depicts the wide variance of stroke reported for different surgical procedures. The incidence of perioperative stroke in noncardiac, nonneurologic surgery is estimated as 0.1 % [3]. This figure excludes cases of covert stroke which is a clinically silent ischemic event detected by neuroimaging [6]. In a relatively low-risk surgical population, the incidence of covert stroke may be as high as 10 % [7]. The incidence of other subtle clinical neurologic outcomes such as cognitive dysfunction is likely to be even higher, although there is currently insufficient evidence to quantify this. It is important to understand that most postoperative strokes present at least 24 h after surgery, and that only 5–15 % occur intraoperatively or in the immediate postoperative period [5, 8••].
Pathophysiology
Stroke can be broadly classified as ischemic or hemorrhagic. The majority of perioperative strokes are ischemic [17–19]; <4 % are secondary to hemorrhage [8••, 20]. Although the Acute Stroke Treatment classification system is useful to differentiate the etiology of ischemic stroke in the nonoperative setting [21], the lack of robust studies and infrequent occurrence prevent the same level of granularity in defining the etiologies of perioperative stroke. The majority of perioperative strokes are cortical infarcts located in the MCA territory [22]. The major mechanisms implicated in the development of perioperative stroke are thrombosis, embolism, anemic tissue hypoxia, and cerebral hypoperfusion [17, 23–25]. Stroke presenting on the day of surgery is relatively infrequent (<6 %) [8••]. The majority of perioperative strokes occur after the second postoperative day [26], suggesting that postoperative events may play an important role in their pathogenesis [17, 26]. This has important clinical consequences as it highlights the importance of continued meticulous monitoring during the recovery and postoperative periods.
Thrombosis
The perioperative period induces a hypercoagulable state in surgical patients. The reasons for this are multifactorial and include a combination of activation of prothrombotic inflammatory cascades [27], endothelial dysfunction, and rebound hypercoagulation secondary to discontinuation of antiplatelet or anticoagulant therapy [28, 29].
The prothrombotic inflammatory cascade is characterized by an elevation in inflammatory markers including interleukins-1 and -6, tumor necrosis factor α [30], and C-reactive protein [31]. Inflammation is an important component in stroke pathophysiology [32, 33], and peak plasma concentration of interleukin-6 correlates significantly with infarct volume, clinical outcomes, and mortality following stroke [34, 35]. Further, the antiinflammatory effect of statins has been shown to have a protective role in the prevention of stroke in nonoperative [36] and perioperative settings in vascular and cardiac surgery patients [37, 38].
Endothelial dysfunction in the postoperative period is a recognized event, and general anesthetics, especially nitrous oxide, can further impair endothelial function [39, 40]. In combination with the pro-inflammatory state induced by surgery, vascular endothelial dysfunction may predispose to increased risk of thrombotic stroke in the perioperative period. However, as of yet these concerns remain theoretical and there is no evidence for this association in clinical practice.
Embolism
In cardiac surgery, cardioembolism is the major cause of perioperative ischemic stroke (>60 %) [20], related to manipulation of the heart and aorta, and the risks inherent to cardiopulmonary bypass [15, 41]. In contrast, in the noncardiac nonneurosurgical setting, the majority of strokes occur secondary to thrombosis (68 %) [17, 23, 42, 43]. The main etiology of embolic stroke in the noncardiac setting is preexisting or new onset atrial fibrillation [10, 44].
Anemia
Cerebral hypoxia in the setting of hemodilution and anemia has been demonstrated in animal studies [45]. In humans, an increased risk of stroke has been observed in surgical patients receiving beta-blockers, particularly metoprolol, with hemoglobin levels below 9 g/dl [24]. The underlying mechanism of this increased stroke risk may be the suppression of the protective, compensatory increase in cardiac output by metoprolol. Based on animal studies, another theory for the observed increased risk of stroke may be antagonism of β2-mediated cerebral vasodilation [46, 47]. When this antagonism was minimized, the risk for ischemia and stroke was lessened further supporting this theory [48].
Hypoperfusion
Watershed areas occur at the junction of the distal fields of two or more nonanastomosing arterial systems. Perfusing pressures may be limited in these regions making them particularly vulnerable to ischemia [49]. Watershed infarcts are responsible for approximately 10 % of strokes in cardiac surgery [50]. Relative hypotension may result in hypoperfusion to vulnerable vascular beds, particularly when combined with fixed vessel stenosis proximal to the area at risk. Interestingly, deliberate hypotension does not seem to adversely affect cerebral perfusion [51]. Even if hypotension per se is not the cause of a stroke, it might still adversely affect its severity by compromising perfusion to the ischemic penumbra [52] and by reducing the clearance of microemboli, thus increasing the ischemic insult [53].
Risk Factors
There are three major categories of risk that may contribute to the development of perioperative stroke–patient comorbidities, surgical factors, and perioperative events. These major components and related causes are illustrated in Fig. 1. As regards the patient comorbidities associated with perioperative stroke, Mashour et al. developed a model to predict the risk of perioperative stroke based on National Surgery Quality Improvement Program (NSQIP) data from more than 350,000 noncardiac, nonneurologic surgical patients [3]. This model was validated in a second cohort that included more than 150,000 patients (Table 2). It is important to note that, while the incidence of perioperative stroke in this low-risk surgical population was 0.1 % in patients with ≤2 risk factors, stroke incidence increased 20-fold for patients with ≥5 risk factors.
Risk Reduction
Preoperative Management
Timing of Elective Surgery After Recent Stroke
All patients presenting for surgery with a history of cerebrovascular compromise should be regarded as high risk for perioperative stroke [4••]. Stroke results in deranged cerebral autoregulation that persists for several months, thereby increasing the likelihood of cerebral ischemia with minimal additional stress [54–57]. A recent large study using the Danish nationwide cohort dramatically supported this concern [58•]. When elective noncardiac surgery was performed within 3 months of a known stroke, the adjusted odds of perioperative stroke was increased 67-fold compared to patients with no prior history of stroke. This elevated risk of perioperative stroke extended up to 9 months beyond the initial stroke event. Additionally, in this large cohort the risk of major adverse cardiac events (MACE include ischemic stroke, acute myocardial infarction, and cardiovascular death) was also markedly increased in patients having suffered recent stroke, and this increased risk also persisted up to 9 months following the initial stroke event [58•]. Based on these recent data it can be concluded that, when possible, elective surgery should be delayed 6–9 months following acute ischemic stroke and that patients requiring emergent surgery within 9 months of stroke are not only at risk for recurrent stroke but also for other major cardiovascular complications.
Anticoagulant and Antiplatelet Therapy
Discontinuation of antiplatelet and antithrombotic therapy in nonoperative patients is associated with a 5.2 % incidence of stroke within 60 days compared to patients who continue treatment [29]. Because of the increased risk of bleeding with continued antiplatelet therapy [59•], this becomes a complex clinical issue in the perioperative setting. The bleeding complications resulting from continued antiplatelet therapy should be balanced against the risk of thrombosis resulting in stroke or myocardial ischemia when antiplatelet agents are withheld. A practical approach is to continue antiplatelet drugs in patients scheduled for minor surgeries or those in which high blood loss is unlikely. If a procedure is associated with significant bleeding, discontinuation of antiplatelet therapy should be considered and treatment restarted as soon as the risk of surgical bleeding is considered to be low, with appropriate bridging strategies.
Several studies have confirmed that aspirin taken within 5 days prior to cardiac surgery is protective against perioperative stroke [60–62]. The evidence for this protection is less conclusive for noncardiac, noncarotid surgery, except for hip arthroplasty [63]. Thus current evidence does not support the initiation of aspirin before and after noncardiac surgery for stroke prevention [64]. Patients presenting for surgery who are taking aspirin for primary (10-year Framingham coronary risk estimate >10 %) or secondary (prevention of MI, stroke, and death secondary to vascular causes) preventative therapy, and who are undergoing nonclosed space or nonprostate procedures, should be considered for aspirin continuation throughout the perioperative period [65]. Further study is needed to clarify management of this patient group.
Perioperative Beta-Blockade
Since the PeriOperative ISchemic Evaluation (POISE) trial demonstrated a higher risk of stroke and death in patients receiving metoprolol in the immediate preoperative period [25], considerable interest surrounds the possible association between beta-blockers and stroke. It is unclear if this association represents a metoprolol-specific effect, or if the poor outcomes were related to the observed bradycardia and hypotension in patients randomized to receive metoprolol. Subsequent studies have shown no increased risk of stroke with clinically routine doses of bisoprolol [66], and that bisoprolol is associated with lower stroke risk than either metoprolol or atenolol [24].
There is evidence of a reduced risk of MACE with perioperative beta-blockade, though this may come at the expense of an increased risk of stroke in noncardiac surgery patients [67]. The 2014 American College of Cardiology/AHA guidelines recommend balancing the risks and benefits of perioperative beta-blockade on a patient-specific basis [68]. In cases where the risk of MACE may be higher than that of perioperative stroke, perioperative beta-blockade may be beneficial. In such circumstances it is suggested that beta-blockers be gradually up-titrated prior to surgery when possible [4••]. For patients on chronic beta-blocker therapy, at present the known risks of acute cessation outweigh the theoretical risks of stroke with continued therapy. Beta-blocker therapy should therefore be continued through the perioperative period in such patients.
Perioperative Statins
In the nonoperative setting, discontinuation of statins in individuals with acute ischemic stroke is associated with a high risk of early neurologic deterioration [69]. In asymptomatic surgical patients presenting for carotid endarterectomy, statins can reduce neurologic injury [70]. The protective effects of statins for noncardiac and noncarotid patients, however, are less clear. While the Vascular Events in Noncardiac Surgery Patients Cohort Evaluation study demonstrated that preoperative statin use was associated with a lower risk of a composite of adverse cardiovascular events (all-cause mortality, myocardial injury after noncardiac surgery or stroke), there was no protection against myocardial infarction or stroke per se [71]. Thus, with regard to perioperative stroke in the noncardiac and nonvascular surgical population, to date there are no data to support any beneficial effect from the initiation of statins. It seems advisable however to continue statins perioperatively for patients presenting on chronic statin therapy.
Intraoperative Management
While intraoperative events are frequently cited as a direct cause of perioperative stroke, the evidence for this is not strong. Based on NSQIP data from over 47,000 noncarotid major vascular surgery patients, Sharifpour et al. demonstrated that only 15 % of strokes occurred on postoperative day 0 or 1 [5••]. This is consistent with results from other studies [11, 42, 72], and suggests that the postoperative rather than intraoperative period may be critical for stroke development. None of the independent predictors of stroke identified by Sharifpour et al. (increasing age, cardiac history, female sex, history of cerebrovascular disease, and acute renal failure or dialysis dependence) is potentially modifiable [5••], highlighting the importance of conducting further prospective investigations to identify intraoperative and postoperative risk factors. Nevertheless, we discuss different intraoperative anesthetic techniques and strategies that have been studied to decrease postoperative stroke risk.
Anesthetic and Monitoring Techniques
Regional versus General Anesthesia
There is no conclusive evidence to suggest that either a regional or general anesthesia technique is superior with regard to perioperative stroke risk reduction [8••]. The General Anesthesia versus Local Anesthesia for carotid surgery (GALA) trial, an international multicenter study, did not show any definitive difference in stroke outcomes between regional or general anesthesia for carotid endarterectomy [73]. However, there is some evidence to suggest that central neuraxial blocks may be associated with lower risk of stroke (0.07 vs. 0.13 %) and reduced mortality in joint arthroplasty [74]. This is further supported by another single-center observational study that identified general anesthesia as an independent predictor of postoperative stroke in joint arthroplasty patients (OR 3.54, 95 % CI 1.01–12.39) [75]. The SNACC Perioperative Stroke Consensus Statement recognizes that neuraxial techniques may be associated with a lower incidence of perioperative stroke for joint arthroplasty, but emphasizes that this finding may not be applicable to other surgical populations.
Nitrous Oxide
Nitrous oxide can increase plasma homocysteine levels [39]. There is a hypothetical risk that this could result in impairment of endothelial function which may lead to adverse cardiovascular events including stroke. However, neither the Nitrous oxide and perioperative cardiac morbidity (ENIGMA-II) trial [76] nor subgroup analysis in the GALA trial [77] supports this hypothesis. Based on several studies, it is safe to deduce that there is no clinically significant association between intraoperative administration of nitrous oxide and postoperative stroke [8••, 77–79]. This view is also reflected in the SNACC consensus statement [4••].
Ventilation Strategies
Although there is no direct relationship between ventilation strategies and stroke risk, hyperventilation results in hypocapnia with consequent reduction in cerebral blood flow. In the nonoperative setting, imaging studies have demonstrated a higher incidence of cerebral ischemia and worse outcome in stroke patients who were hypocapnic when compared to normocapnic patients [80]. There is no similar evidence in the surgical cohort. In theory, hyperventilation can cause an ‘inverse steal phenomenon’ and therefore favorably redistribute blood flow to ischemic regions, but animal studies do not support this hypothesis [81–84]. Intraoperative hyperventilation has other deleterious effects such as reduced oxygenation, increased myocardial oxygen, dysrhythmias, and reduced cerebral blood flow. Thus hyperventilation should not be employed because of a theoretical potential for favorable cerebral blood flow distribution after stroke, and it seems reasonable to maintain normocapnia when possible.
Physiologic Management
Blood Pressure and Positioning
Until recently there was very little evidence to support a link between intraoperative hypotension and postoperative stroke [17]. The low incidence of watershed infarctions in noncardiac surgical patients [85], and the possibility of embolic phenomena as the cause of cortical watershed infarcts [53, 86], suggest a cause other than intraoperative hypotension. However, the hypotension associated with acute beta-blockade in the POISE trial revived interest on this subject [25]. Bijker et al. demonstrated a small association between intraoperative hypotension and postoperative stroke when mean arterial pressure (MAP) was reduced by 30 % compared with baseline (OR 1.01; 99.9 % CI 1.00–1.03) [22], although the clinical significance of this result is unclear. Mashour et al. also found an association between postoperative stroke and intraoperative hypotension defined as blood pressure 20 % below baseline for both systolic blood pressure and MAP [8••]. Thus, while it seems reasonable to assume that there is an association between intraoperative hypotension and postoperative stroke, the threshold and duration at which this association is significant is not clear. Further prospective studies are required to assess the strength of this association.
Given the evidence for the detrimental effects of intraoperative hypotension on stroke incidence, one might assume that the reverse scenario (maintaining blood pressure near preoperative baseline values) should lower the risk of postoperative stroke risk. However, evidence for this notion is lacking. Further, the timing of postoperative stroke (most common after 24 h), emphasizes the importance of hypotension in the postoperative period as an important contributing factor.
Postural hypotension, especially in the beach chair position, may also play a role in stroke incidence after noncardiac surgery [87]. Neurologic injury may result from inadvertent reduction in cerebral perfusion pressures despite acceptable recorded blood pressures because of the postural effects of the seated position on blood pressure [88]. MAP measured at the level of the brain stem can be 12–24 mmHg lower than the pressure measured by cuff on the nonoperative arm, and further divergent if measured on the lower extremity [89]. Cerebral oximetry studies reveal a high incidence of regional cerebral oxygen desaturation in the beach chair position [90–92], but the relationship between the severity and duration of these episodes of desaturation and the risk of neurologic injury is not yet known [93, 94].
Intraoperative Hemorrhage and Optimal Transfusion Therapy
There is evidence in nonoperative patients that anemia is associated with stroke even in the absence of hypotension [95, 96]. In cardiac surgery, there is evidence of an association between low hematocrit and increased risk of perioperative stroke [97–99]. The POISE trial identified ‘significant bleeding’ to be an independent predictor of postoperative stroke in the population of high-risk patients undergoing noncardiac surgery [25]. Furthermore, in noncardiac, noncarotid, and nonneurologic surgery, it has been demonstrated that patients receiving more than four units of packed red blood cells have a 2.5-fold increased risk of stroke [100]. Although there is evidence to demonstrate increased risk of stroke or myocardial infarction relating to number of units of transfusion [101], the possibility still remains that any transfusion is simply a marker for unmeasured or unmeasurable variables such as a clinical instability, more extensive surgery, or an individual clinician’s threshold to transfuse. As previously discussed, patients on beta-blockers may be at particular risk for cerebral ischemia in the setting of anemia due to inhibition of B2-mediated cerebral vasodilation [24]. The SNACC consensus statement recommends maintaining hemoglobin >9 gm/dl in surgical patients on chronic beta-blocker therapy.
Blood Glucose Homeostasis
In cardiac surgery, both hypoglycemia [102] and hyperglycemia [103] have been identified as risk factors for perioperative stroke. Hyperglycemia has also been identified as a risk factor for perioperative stroke in carotid endarterectomy [104] and open cerebral aneurysm surgery [105], but similar evidence in noncardiac, nonneurologic surgery is lacking. Most authors recommend intervention for serum glucose values exceeding 150 mg/dl, with an absolute upper limit of 180 mg/dl in patients undergoing major surgery [106, 107]. For avoidance of hypoglycemia, insulin therapy should be reduced if blood glucose concentrations decline below 100 mg/dl with an absolute lower limit of 70 mg/dl [108].
Intraoperative Beta-Blockade
The most important intraoperative pharmacologic association with postoperative stroke is the administration of beta-blockers. As discussed earlier, the POISE trial identified an association between perioperative metoprolol and postoperative stroke [25], and subsequent studies have confirmed this effect. Mashour et al. found a greater than threefold increased risk of perioperative stroke in patients who received intraoperative metoprolol [8••]. This effect was not observed with esmolol and labetalol. As a nonselective beta-blocker, metoprolol may uniquely place patients at risk for stroke in the setting of hemodilution [46, 47, 109, 110]. Accordingly, the SNACC consensus statement suggests that beta-blockers with a short duration of action and greater β1 selectivity such as esmolol should be considered for intraoperative use.
Management of Perioperative Stroke
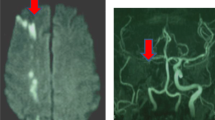
Clinical recognition of perioperative stroke is predictably difficult in the setting of emergence from general anesthesia, pain, sleep deprivation, and ongoing opiate therapy. Delayed recognition of symptoms, delayed neuroimaging, lower rates of thrombolysis, and exceptionally severe stroke have all been associated with in-hospital stroke [2]. Whenever possible, management should follow the most recent AHA guidelines for the management of patients with acute ischemic stroke [111], although postoperative patients clearly present unique clinical problems that are not relevant in the nonoperative setting. An organized protocol for emergency evaluation of surgical patients with suspected perioperative stroke facilitates the activities of a multidisciplinary team. An institutional pathway also promotes higher efficiency, more rapid therapeutic intervention, and a more reliable transfer of information pertinent to a patient’s optimal care [112]. In the management of stroke, it should be remembered that ‘Time is Brain’! See Fig. 2 for a suggested treatment algorithm.
Initial Assessment
A high index of suspicion, particularly in patients with known risk factors for stroke, is the key to early identification and management of perioperative stroke. A delay in emergence from anesthesia, altered mental status upon emergence, or any new focal neurological deficit should immediately alert the clinical team to the possibility of stroke. If suspected, a rapid assessment should be performed using a simple, quick screening tool. This could include any of a number of scales, including FAST [113], LAPSS [114], MASS [115], and ROSIER [116], although all of them were established for recognizing stroke in the nonoperative setting. Currently, there is no ideal tool for recognizing stroke in the postoperative patient.
Confirmation of Diagnosis
If the initial assessment is nonreassuring then the hospital stroke team should be activated immediately. The members of this team generally include stroke neurology, interventional neuroradiology, intensive care, and anesthesia. This team can perform a detailed evaluation, and confirm or refute the clinical diagnosis of stroke.
Simultaneously, the clinical team in the postoperative unit should assess the possibility of any physiologic, pharmacologic, or pathologic cause that may mimic or mask features of stroke. Residual action of perioperative medications (opiates, sedative hypnotics, neuromuscular blockers, or residual inhalational agent) should be considered. The primary surgical team should also perform an initial assessment to rule out any surgical cause of the patient’s clinical state. Vital signs should be monitored as part of the initial evaluation and as a baseline to assess subsequent measurements. Baseline blood investigations, including complete blood count, electrolytes, coagulation status, point of care glucose measurement, and arterial blood gases, should also be considered.
A noncontrast head CT should be immediately obtained to rule out acute hemorrhage as the cause of neurologic decline. The information obtained from CT has important therapeutic implications as the patient can not be considered for any mode of acute intervention until the absesnce of intracranial hemorrhage is confirmed. Radiologic findings should be correlated with clinical findings. If the diagnosis remains unclear, or if stroke is suspected but the timing of onset is unknown, an MRI may be indicated recognizing the delays inherent to this imaging modality.
The vast majority of perioperative stroke is ischemic in origin and therefore further discussion will focus on the management of ischemic stroke in this population. If a hemorrhagic stroke is identified, then ASA/AHA guidelines should be followed [117].
To Thrombolyse or Not?
There are three main therapeutic options available in the management of ischemic stroke: systemic thrombolysis [111], intraarterial thrombolysis [118–120], or catheter-based mechanical interventions [121]. If ischemic stroke is confirmed radiologically and clinically, then a meticulous, multidisciplinary, risk-benefit analysis should be performed regarding patient suitability for thrombolysis. This decision will depend on patient factors, the surgical intervention performed, time since surgery, and the site and severity of the stroke. If appropriate resources are available, acute mechanical endovascular treatment may alleviate the need for thrombolysis. If pharmacological thrombolysis is decided then this can be accomplished either by intravenous or intraarterial routes (if patient is at high risk of systemic hemorrhage). Recombinant tissue plasminogen activator (rtPA) is the currently available thrombolytic agent employed in the United States. Unlike treatment protocols for acute myocardial infarction, administration of aspirin or other anticoagulant is not indicated within 24 h of stroke onset and may in fact render the patient ineligible for thrombolytic therapy. There are new prospective studies in strong support of endovascular management for acute ischemic stroke, and improved techniques including the use of stent-retrievers may minimize the need for systemic thrombolytics in the postsurgical patient [122].
Further Care
Patients who suffer a perioperative stroke should be recovered in a neurocritical care unit or a dedicated stroke unit for close neurologic and physiologic monitoring. Airway control with intubation should be strongly considered if GCS is <8 in order to decrease the chance of aspiration, prevent hypercapnia, manage intracranial pressure, and treat cerebral edema. SpO2 should be maintained above 94 %, achieved through oxygen supplementation and mechanical ventilation as required. Sufficient perfusion pressure should be maintained at all times. In this regard, blood pressure lowering is not recommended unless >180/105 mmHg in thrombolysed patients, or >220/120 in nonthrombolysed patients or in the presence of significant comorbidities such as cardiac failure. Continuous EKG monitoring should be performed because stroke patients are prone to serious arrhythmias which require immediate treatment to restore sinus rhythm. Pain can initiate a stress response and should be avoided or treated with appropriate analgesia. Hypovolemia should be corrected with normal saline.
Conclusion
Perioperative stroke is a devastating consequence for patients and their families. Risk stratification and risk reduction strategies are crucial to minimize the risk of perioperative stroke. Early identification and expeditious management involving a multidisciplinary approach is the key to avoiding a poor outcome following perioperative stroke.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Sacco RL, Kasner SE, Broderick JP, et al. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:2064–89.
Saltman AP, Solver FL, Fang J, Stamplecoski M, Kapral MK. Care and outcomes of patients with in-hospital stroke. JAMA Neurol. 2015;72:749–55.
Mashour GA, Shanks AM, Kheterpal S. Perioperative stroke and associated mortality after noncardiac, nonneurologic surgery. Anesthesiology. 2011;114:1289–96.
•• Mashour GA, Moore LE, Lele AV, Robicsek SA, Gelb AW. Perioperative care of patients at high risk for stroke during or after non-cardiac, non-neurologic surgery: consensus statement from the Society for Neuroscience in Anesthesiology and Critical Care. J Neurosurg Anesthesiol. 2014;26:273–85. Evidence-based recommendations and opinions regarding the preoperative, intraoperative and postoperative care of patients at high risk of perioperative stroke.
•• Sharifpour M, Moore LE, Shanks AM, Didier TJ, Kheterpal S, Mashour GA. Incidence, predictors and outcomes of perioperative stroke in noncarotid major vascular surgery. Anesth Analg. 2013;116:424–34. Large database analysis that identified risk factors associated with perioperative stroke. Demonstrated that none were readily modifiable—advancing age, cardiac history, female sex, history of cerebrovascular disease, acute renal failure or dialysis dependence. Perioperative stroke incidence in this population was 0.6% and associated with 3-fold increase in 30 day all-cause mortality and increased length of stay. Also identifed that majority of strokes occur after postoperative day 1.
Debette S, Markus HS. The clinical importance of white matter hyperintensities on brain magnetic resonance imaging: systematic review and meta-analysis. BMJ. 2010;341:c3666.
Mrkobrada M, Hill M, Chan M, et al. Abstract tmp9: the neurovision pilot study: non-cardiac surgery carries a significant risk of acute covert stroke. Stroke. 2013;44:ATMP9.
•• Mashour GA, Sharifpour M, Freundlich RE, Tremper KK, Shanks A, Nallamothu BK, Vlisides PE, Weightman A, Matlen L, Merte J, Kheterpal S. Perioperative metoprolol and risk of stroke after noncardiac surgery. Anesthesiology. 2013;119:1340–6. Retrospective analysis that investigated the association between betablockers, especially metoprolol and perioperative stroke after noncardiac surgery. Results revealed routine use of preoperative metoprolol, but not atenolol, was associated with stroke after noncardiac surgery. Similarly, intraoperative metoprolol but not esmolol or labetalol, was associated with increased risk of perioperative stroke.
Moore LE, Gelb AW. Perioperative stroke. ASA Refresh Courses Anesthesiol. 2014;42:100–7.
Bateman BT, Schumacher HC, Wang S, Shaefi S, Berman MF. Perioperative acute ischemic stroke in noncardiac and nonvascular surgery: incidence, risk factors, and outcomes. Anesthesiology. 2009;110:231–8.
Axelrod DA, Stanley JC, Upchurch GR Jr, Khuri S, Daley J, Henderson W, Demonner S, Henke PK. Risk for stroke after elective noncarotid vascular surgery. J Vasc Surg. 2004;39:67–72.
Harthun NL, Stukenborg GJ. Atrial fibrillation is associated with increased risk of perioperative stroke and death from carotid endarterectomy. J Vasc Surg. 2010;51:330–6.
Merie C, Kober L, Olsen PS, et al. Risk of stroke after coronary artery bypass grafting: effect of age and comorbidities. Stroke. 2012;43:38–43.
Roach GW, Kanchuger M, Mangano CM, et al. Adverse cerebral outcomes after coronary bypass surgery. Multicenter study of perioperative ischemia research group and the ischemia research and education foundation investigators. N Engl J Med. 1996;335:1857–63.
Bucerius J, Gummert JF, Borger MA, et al. Stroke after cardiac surgery: a risk factor analysis of 16,184 consecutive adult patients. Ann Thorac Surg. 2003;75:472–8.
Hedberg M, Engstrom KG. Stroke after cardiac surgery–hemispheric distribution and survival. Scand Cardiovasc J. 2013;47:136–44.
Limburg M, Wijdicks EF, Li H. Ischemic stroke after surgical procedures: clinical features, neuroimaging, and risk factors. Neurology. 1998;50:895–901.
Restrepo L, Wityk RJ, Grega MA, et al. Diffusion- and perfusion-weighted magnetic resonance imaging of the brain before and after coronary artery bypass grafting surgery. Stroke. 2002;33:2909–15.
Brooker RF, Brown WR, Moody DM, et al. Cardiotomy suction: a major source of brain lipid emboli during cardiopulmonary bypass. Ann Thorac Surg. 1998;65:1651–5.
Likosky DS, Marrin CA, Caplan LR, et al. Determination of etiologic mechanisms of strokes secondary to coronary artery bypass graft surgery. Stroke. 2003;34:2830–4.
Chung JW, Park SH, Kim N, Kim WJ, Park JH, Ko Y, Yang MH, Jang MS, et al. Trial of ORG 10172 in Acute Stroke Treatment (TOAST) classification and vascular territory of ischemic stroke lesions diagnosed by diffusion-weighted imaging. J Am Heart Assoc. 2014;3:1–8.
Bijker JB, Persoon S, Peelen LM, et al. Intraoperative hypotension and perioperative ischemic stroke after general surgery: a nested case-control study. Anesthesiology. 2012;116:658–64.
Parikh S, Cohen JR. Perioperative stroke after general surgical procedures. N Y State J Med. 1993;93:162–5.
Ashes C, Judelman S, Wijeysundera DN, et al. Selective beta 1- anatagonism with bisoprolol is associated with fewer postoperative strokes than atenolol or metoprolol: a single-center cohort study of 44,092 consecutive patients. Anesthesiology. 2013;119:777–87.
Devereaux PJ, Yang H, Yusuf S, POISE Study Group, et al. Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): a randomised controlled trial. Lancet. 2008;371:1839–47.
Hart R, Hindman B. Mechanisms of perioperative cerebral infarction. Stroke. 1982;13:766–73.
Khafagy HF, Hussein NA, Madkour ME, et al. Perioperative effects of anesthesia and surgery on inflammation-coagulation interaction. Life Sci J. 2014;11:900–6.
Cundiff DK. Clinical evidence for rebound hypercoagulability after discontinuing oral anticoagulants for venous thromboembolism. Medscape J Med. 2008;10:258.
Broderick JP, Bonomo JB, Kissela BM, et al. Withdrawal of antithrombotic agents and its impact on ischemic stroke occurrence. Stroke. 2011;42:2509–14.
Bastian D, Tamburstuen MV, Lyngstadaas SP, Reikeras O. Systemic and local cytokine kinetics after total hip replacement surgery. Eur Surg Res. 2008;41:334–40.
Riche F, Dosquet C, Panis Y, Valleur P, Laisne MJ, Briard C, Wautier JL. Levels of portal and systemic blood cytokines after colectomy in patients with carcinoma or Crohn’s disease. J Am Coll Surg. 1995;180:718–24.
Elkind MS. Inflammatory mechanisms of stroke. Stroke. 2010;41:S3–8.
McColl BW, Rothwell NJ, Allan SM. Systemic inflammatory stimulus potentiates the acute phase and CXC chemokine responses to experimental stroke and exacerbates brain damage via interleukin-1 and neutrophil-dependent mechanisms. J Neurosci. 2007;27:4403–12.
Smith CJ, Emsley HC, Gavin CM, et al. Peak plasma interleukin-6 and other peripheral markers of inflammation in the first week of ischaemic stroke correlate with brain infarct volume, stroke severity and long-term outcome. BMC Neurol. 2004;4:2.
Rallidis LS, Vikelis M, et al. Inflammatory markers and in-hospital mortality in acute ischaemic stroke. Atherosclerosis. 2006;189:193–7.
Everett BM, Glynn RJ, MacFadyen JG, Ridker PM. Rosuvastatin in the prevention of stroke among men and women with elevated levels of C-reactive protein: Justification for the Use of statins in Prevention: an Intervention Trial Evaluating Rosuvastatin (JUPITER). Circulation. 2010;121:143–50.
Kuhn EW, Liakopoulos OJ, Stange S, et al. Preoperative statin therapy in cardiac surgery: a meta-analysis of 90,000 patients. Eur J Cardiothorac Surg. 2014;45:17–26.
Antoniou GA, Hajibandeh S, Hajibandeh S, Vallabhaneni SR, Brennan JA, Torella F. Meta-analysis of the effects of statins on perioperative outcomes in vascular and endovascular surgery. J Vasc Surg. 2015;61:519–32.
Myles PS, Chan MT, Leslie K, Peyton P, Paech M, Forbes A. Effect of nitrous oxide on plasma homocysteine and folate in patients undergoing major surgery. Br J Anaesth. 2008;100:780–6.
Myles PS, Chan MTV, Kaye DM, et al. Effect of nitrous oxide anesthesia on plasma homocysteine and endothelial dysfunction. Anesthesiology. 2008;109:657–63.
Likosky DS, Caplan LR, Weintraub RM, et al. Northern New England Cardiovascular Disease Study Group. Intraoperative and postoperative variables associated with strokes following cardiac surgery. Heart Surg Forum. 2004;7:E271–6.
Ng JL, Chan MT, Gelb AW. Perioperative stroke in noncardiac, nonneurosurgical surgery. Anesthesiology. 2011;115:879–90.
Popa AS, Rabinstein AA, Huddleston PM, Larson DR, Gullerud RE, Huddleston JM. Predictors of ischemic stroke after hip operation: a population-based study. J Hosp Med. 2009;4:298–303.
Kaatz S, Douketis JD, Zhou H, Gage BF, White RH. Risk of stroke after surgery in patients with and without chronic atrial fibrillation. J Thromb Haemost. 2010;8:884–90.
McLaren AT, Marsden PA, Mazer CD, et al. Increased expression of HIF-1alpha, nNOS, and VEGF in the cerebral cortex of anemic rats. Am J Physiol Regul Integr Comp Physiol. 2007;292:R403–14.
Hare GM, Worrall JM, Baker AJ, Liu E, Sikich N, Mazer CD. β2 Adrenergic antagonist inhibits cerebral cortical oxygen delivery after severe haemodilution in rats. Br J Anaesth. 2006;97:617–23.
El Beheiry MH, Heximer SP, Voigtlaender-Bolz J, et al. Metoprolol impairs resistance artery function in mice. J Appl Physiol (1985). 2011;111:1125–33.
Hu T, Beattie WS, Mazer CD, et al. Treatment with a highly selective beta 1 antagonist causes dose-dependent impairment of cerebral perfusion after hemodilution in rats. Anesth Analg. 2013;116:649–62.
Mohr JP. Distal field infarction. Neurology. 1969;19:279.
Joregensen L, Torvik A. Ischaemic cerebrovascular diseases in an autopsy series: prevalence, location, pathogenesis and clinical course of cerebral infarcts. J Neurol Sci. 1969;9:285–320.
Selim M. Perioperative stroke. N Engl J Med. 2007;7:706–13.
de Haan P, Kalkman CJ, et al. Development of spinal cord ischemia after clamping of non-critical segmental arteries in the pig. Ann Thorac Surg. 1999;68:1278–84.
Caplan LR, Hennerici M. Impaired clearance of emboli (washout) is an important link between hypoperfusion, embolism, and ischemic stroke. Arch Neurol. 1998;55:1475–82.
Dawson SL, Blake MJ, Panerai RB, et al. Dynamic but not static cerebral autoregulation is impaired in acute ischaemic stroke. Cerebrovasc Dis. 2000;10:126–32.
Rubin G, Levy EI, Scarrow AM, et al. Remote effects of acute ischemic stroke: a xenon ct cerebral blood flow study. Cerebrovasc Dis. 2000;10:221–8.
Dawson SL, Panerai RB, Potter JF. Serial changes in static and dynamic cerebral autoregulation after acute ischaemic stroke. Cerebrovasc Dis. 2003;16:69–75.
Aries MJ, Elting JW, De Keyser J, et al. Cerebral autoregulation in stroke: a review of transcranial doppler studies. Stroke. 2010;41:2697–704.
• Jorgensen ME, Torp-Pedersen C, Gislason GH, et al. Time elapsed after ischemic stroke and risk of adverse cardiovascular events and mortality following elective noncardiac surgery. JAMA. 2014;312:269–77. Danish nationwide cohort study that identified higher risk of major adverse cardiovascular events and mortality in the stroke group, especially if time between stroke and surgery was less than 9 months. Beyond 9 months, the risk was still higher in the stroke cohort but the risk leveled off .
• Deveraux PJ, Mrkobrada M, Sessler DI, POISE-2 Investigators, et al. Aspirin in patients undergoing noncardiac surgery. N Eng J Med. 2014;370:1494–503. International, randomized controlled trial in patients undergoing noncardiac surgery. Administration of aspirin before surgery and throughout the early postsurgical period had no significant effect on the rate of death or nonfatal myocardial infarction but increased the risk of major bleeding. Of note, the authors suggest there was a spurious subgroup effect that revealed a reduction in stroke incidence among patients in whom aspirin was initiated but not in those who were already on long-term therapy.
Cao L, Silvestry S, Zhao N, Diehl J, Sun J. Effects of preoperative aspirin on cardiocerebral and renal complications in non-emergent cardiac surgery patients: a sub-group and cohort study. PLoS One. 2012;7:e30094.
Cao L, Young N, Liu H, et al. Preoperative aspirin use and outcomes in cardiac surgery patients. Ann Surg. 2012;255:399–404.
Mangano DT, Multicenter Study of Perioperative Ischemia Research Group. Aspirin and mortality from coronary bypass surgery. N Engl J Med. 2002;347:1309–17.
Lalmohamed A, Vestergaard P, Cooper C, et al. Timing of stroke in patients undergoing total hip replacement and matched controls: a nationwide cohort study. Stroke. 2012;43:3225–9.
Duceppe E, Mrkobrada M, Thomas S, Devereaux PJ. Role of aspirin for prevention and treatment of perioperative cardiovascular events. J Thromb Haemost. 2015;13:S297–303.
Gerstein NG, Carey MC, Cigarroa JE, Schulman PM. Perioperative aspirin management after POISE-2: some answers, but questions remain. Anesth Analg. 2015;120(3):570–5.
van Lier F, Schouten O, Hoeks SE, et al. Impact of prophylactic beta-blocker therapy to prevent stroke after noncardiac surgery. Am J Cardiol. 2010;105:43–7.
Blessberger H, Kammler J, Domanovits H, et al. Perioperative beta-blockers for preventing surgery-related mortality and morbidity. Cochrane Database Syst Rev. 2014;9:CD004476.
Fleisher LA, Fleischmannn KE, Auerbach AD, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2014;64:e77–137.
Blanco M, Nombela F, Castellanos M, et al. Statin treatment withdrawal in ischemic stroke: a controlled randomized study. Neurology. 2007;69:904–10.
Heyer EJ, Mergeche JL, Bruce SS, et al. Statins reduce neurologic injury in asymptomatic carotid endarterectomy patients. Stroke. 2013;44:1150–2.
Berwanger O, Le Manach Y, Suzumura EA, Biccard B, Srinathan SK, Szczeklik W, Santo JAE, Santucci E, Cavalcanti AB, Archbold RG, Devereaux PJ. Association between pre-operative statin use and major cardiovascular complications among patients undergoing non-cardiac surgery: the VISION study. Eur Heart J. 2015;. doi:https://doi.org/10.1093/eurheartj/ehv456.
Kim J, Gelb AW. Predicting perioperative stroke. J Neurosurg Anesthesiol. 1995;7:211–5.
Lewis SC, Warlow CP, Bodenham AR, GALA Trial Collaborative Group GTC, et al. General anaesthesia versus local anaesthesia for carotid surgery (GALA): a multicentre, randomised controlled trial. Lancet. 2008;372:2132–42.
Memtsoudis SG, Sun X, Chiu YL, et al. Perioperative comparative effectiveness of anesthetic technique in orthopedic patients. Anesthesiology. 2013;118:1046–58.
Mortazavi SM, Kakli H, Bican O, Moussouttas M, Parvizi J, Rothman RH. Perioperative stroke after total joint arthroplasty: prevalence, predictors, and outcome. J Bone Joint Surg Am. 2010;92:2095–101.
Myles PS, Leslie K, Chan MT, Investigators, ANZCA Trials Group for the ENIGMA-II, et al. The safety of addition of nitrous oxide to general anaesthesia in at-risk patients having major non-cardiac surgery (ENIGMA-II): a randomised, single-blind trial. Lancet. 2014;384:1446–54.
Sanders RD, Graham C, Lewis SC, et al. Nitrous oxide exposure does not seem to be associated with increased mortality, stroke, and myocardial infarction: a non-randomized subgroup analysis of the general anaesthesia compared with local anaesthesia for carotid surgery (GALA) trial. Br J Anaesth. 2012;109:361–7.
Leslie K, Myles PS, Chan MT, et al. Nitrous oxide and long-term morbidity and mortality in the enigma trial. Anesth Analg. 2011;112:387–93.
Leslie K, Myles P, Devereaux PJ, et al. Nitrous oxide and serious morbidity and mortality in the POISE trial. Anesth Analg. 2013;116:1034–40.
Stringer WA, Hasso AN, Thompson JR, et al. Hyperventilation-induced cerebral ischemia in patients with acute brain lesions: demonstration by xenon-enhanced CT. Am J Neuroradiol. 1993;14:475–84.
Ruta TS, Drummond JC, Cole DJ. The effect of acute hypocapnia on local cerebral blood flow during middle cerebral artery occlusion in isoflurane anesthetized rats. Anesthesiology. 1993;78:134–40.
Fourcade HE, Larson CP Jr, Ehrenfeld WK, et al. The effects of CO2 and systemic hypertension on cerebral perfusion pressure during carotid endarterectomy. Anesthesiology. 1970;33:383–90.
Boysen G, Ladegaard-Pedersen HJ, Henriksen H, et al. The effect of PaCO2 on regional cerebral blood flow and internal carotid arterial pressure during carotid clamping. Anesthesiology. 1971;35:286–300.
Michenfelder JD, Milde JH. Failure of prolonged hypocapnia, hypothermia, or hypertension to favorably alter acute stroke in primates. Stroke. 1977;8:87–91.
Bijker JB, Geld AW. Review article: the role of hypotension in perioperative stroke. Can J Anesth. 2013;60:159–67.
Momjian-Mayor I, Baron JC. The pathophysiology of watershed infarction in internal carotid artery disease: review of cerebral perfusion studies. Stroke. 2005;36:567–77.
Pohl A, Cullen DJ. Cerebral ischemia during shoulder surgery in the upright position: a case series. J Clin Anesth. 2005;17:463–9.
Cullen DJ, Kirby RR. Beach chair postion may decrease cerebral perfusion. APSF Newsl. 2007;22:25–7.
Malhotra A, Cohen D, Syms C, et al. Blood pressure changes in the leg on standing. J Clin Hypertens. 2002;4:350–4.
Murphy GS, Szokol JW, Marymont HJ, et al. Cerebral oxygen desaturation events assessed by near-infrared spectroscopy during shoulder arthroscopy in the beach chair and lateral decubitus positions. Anesth Analg. 2010;111:496–505.
Salazar D, Sears BW, Andre J, et al. Cerebral desaturation during shoulder arthroscopy: a prospective observational study. Clin Orthop Relat Res. 2013;47:4027–34.
Salazar D, Sears BW, Aghdasi B, et al. Cerebral desaturation events during shoulder arthroscopy in the beach chair position: patient risk factors and neurocognitive effects. J Shoulder Elbow Surg. 2013;22:1228–35.
Mortiz S, Kasprzak P, Arlt M, et al. Accuracy of cerebral monitoring in detecting cerebral ischemia during carotid endarterectomy: a comparison of transcranial doppler sonography, near-infrared spectroscopy, stump pressure, and somatosensory evoked potentials. Anesthesiology. 2007;107:563–9.
Samra SK, Dy EA, Wlch K, et al. Evaluation of a cerebral oximeter as a monitor of cerebral ischemia during carotid endarterectomy. Anesthesiology. 2000;93:964–70.
Tsai CF, Yip PK, Chen CC, et al. Cerebral infarction in acute anemia. J Neurol. 2010;257:2044–51.
Kimberly WT, Wu O, Arsava EM, et al. Lower hemoglobin correlates with larger stroke volumes in acute ischemic stroke. Cerbrovasc Dis Extra. 2011;1:44–53.
Fowler AJ, Ahmad T, Phull MK, Allard S, Gillies MA, Pearse RM. Meta-analysis of the association between preoperative anaemia and mortality after surgery. Br J Surg. 2015;102(11):1314–24.
Karkouti K, Djaiani G, Borger MA, et al. Low hematocrit during cardiopulmonary bypass is associated with increased risk of perioperative stroke in cardiac surgery. Ann Thorac Surg. 2005;80:1381–7.
Bahrainwala ZS, Grega MA, Hogue CW, et al. Intraoperative hemoglobin levels and transfusion independently predict stroke after cardiac operations. Ann Thorac Surg. 2011;91:1113–8.
Kamel H, Johnston SC, Kirkham JC, et al. Association between major perioperative hemorrhage and stroke or q-wave myocardial infarction. Circulation. 2012;126:207–12.
Whitlock EL, Kim H, Auerbach AD. Harms associated with single unit perioperative transfusion:retrospective population based analysis. BMJ. 2015;350:h3037.
Ghandi GY, Nuttall GA, Abel MD, et al. Intensive intraoperative insulin therapy versus conventional glucose management during cardiac surgery: a randomized trial. Ann Intern Med. 2007;146:233–43.
Doenst T, Wijeysundera D, Karkouti K, et al. Hyperglycemia during cardiopulmonary bypass is an independent risk factor for mortality in patients undergoing cardiac surgery. J Thorac Cardiovasc Surg. 2005;130:1144.
McGirt MJ, Woodworth GF, Brooke BS, et al. Hyperglycemia independently increases the risk of perioperative stroke, myocardial infarction and death after carotid endarterectomy. Neurosurgery. 2006;58:1066–73.
Pasternak JJ, McGregor DG, Schroeder DR, et al. Hyperglycemia in patients undergoing cerebral aneurysm surgery: its association with long-term gross neurologic and neuropsychological function. Mayo Clin Proc. 2008;83:406–17.
Engelhard K. Anaesthetic techniques to prevent perioperative stroke. Curr Opin Anaesthesiol. 2013;26:368–74.
Jacobi J, Bircher N, Krinsley J, et al. Guidelines for the use of an insulin infusion for the management of hyperglycemia in critically ill patients. Crit Care Med. 2012;40:3251–76.
Engelhard K. Anaesthetic techniques to prevent perioperative stroke. Curr Opin Anesthesiol. 2013;26(3):368–74.
Ragoonanan TE, Beattie WS, Mazer CD, et al. Metoprolol reduces cerebral tissue oxygen tension after acute hemodilution in rats. Anesthesiology. 2009;111:988–1000.
Baker JG. The selectivity of beta-adrenoceptor antagonists at the human beta1, beta2 and beta3 adrenoceptors. Br J Pharmacol. 2005;144:317–32.
Jauch EC, Saver JL, Adams HP Jr, American Heart Association Stroke Council, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:870–947.
Reason J. Human error: models and management. BMJ. 2000;320:768–70.
Nor AM, Davis J, Sen B, et al. Agreement between ambulance paramedic- and physician-recorded neurological signs with face arm speech test (FAST) in acute stroke patients. Stroke. 2004;35:1355–9.
Kidwell CS, Starkman S, Eckstein M, et al. Identifying stroke in the field. Prospective validation of the Los Angeles prehospital stroke screen (LAPSS). Stroke. 2000;31:71–6.
Bray JE, Martin J, Cooper G, et al. Paramedic identification of stroke: community validation of the Melbourne ambulance stroke screen. Cerebrovasc Dis. 2005;20:28–33.
Nor AM, Davis J, Sen B, et al. The recognition of stroke in the emergency room (ROSIER) scale: development and validation of a stroke recognition instrument. Lancet Neurol. 2005;4:727–34.
Hemphil JC 3rd, Greenberg SM, Anderson CS, Becker K, et al. Guidelines for the management of spontaneous intracranial hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015;46:2032–60.
Chalea JA, Katzan I, Liebeskind DS, et al. Safety of intra-arterial thrombolysis in the postoperative period. Stroke. 2001;32:1365–9.
Moazami N, Smedira NG, McCarthy PM, et al. Safety and efficacy of intraarterial thrombolysis for perioperative stroke after cardiac operation. Ann Thorac Surg. 2001;72:1933–7.
Katzan IL, Masaryk TJ, Furlan AJ, et al. Intra-arterial thrombolysis for perioperative stroke after open heart surgery. Neurology. 1999;52:1081–4.
Goyal M, Demchuk AM, Menon BK, Investigators, ESCAPE trial, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372:1019–30.
Grotta JC, Hacke W. Stroke Neurologist’s perspective on the new endovascular trials. Stroke. 2015;46(6):1447–52.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Raja V. Lakshmanan, Baskar Rajala, and Laurel E. Moore declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Neuroanesthesia.
Rights and permissions
About this article
Cite this article
Lakshmanan, R.V., Rajala, B. & Moore, L.E. Perioperative Stroke. Curr Anesthesiol Rep 6, 202–213 (2016). https://doi.org/10.1007/s40140-016-0167-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-016-0167-4