Abstract
Purpose of Review
Out-of-Hospital cardiac arrest affects over 300,000 individuals in the US per year and is the third leading cause of death for Americans. Given the extent of this public health problem, investigations are ongoing to improve upon outcomes for patients who suffer cardiac arrest. This review will address the literature that informed the 2015 American Heart Association update to the Cardiopulmonary and Emergency Cardiovascular Care Guidelines (Callaway et al. in Circulation 132:S465–82, 2015).
Recent Findings
In this manuscript, we reviewed the literature that informed the major changes to the guidelines and present a concise review of the current literature that informs how patients who suffer a cardiac arrest are cared for in the pre-hospital, emergency department and in-hospital environment. Additionally, the new AHA guideline on Maternal Resuscitation will be described.
Summary
Significant updates have been made to the 2015 AHA guidelines informed by the literature to improve outcomes from cardiac arrest. This literature is summarized in this review.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Epidemiology of Out of Hospital Cardiac Arrest
Approximately 326,000 out-of-hospital cardiac arrests (OHCAs) occur annually in the United States, making sudden cardiac arrest (SCA) a leading cause of death [1••]. SCA is responsible for one in every five deaths in the US and accounts for approximately 50 % of deaths attributable to heart disease [2, 3]. Most OHCAs occur in private homes and over 50 % are unwitnessed [4].
The incidence of OHCA increases with age and is more common in men [5]. The ongoing Oregon Sudden Unexpected Death Study (SUDS), which documents demographics and arrest circumstances for individuals who experience SCA in the Portland, OR, metropolitan area, shows that age-adjusted rates for SCA are two-fold higher among black men and women, compared with white men and women. Moreover, blacks are over 6 years younger at the time of SCA when compared with whites [6].
Data has shown that the provision of quality cardiopulmonary resuscitation (CPR) and early defibrillation result in improved outcomes. However, rates of bystander CPR vary considerably over geographic regions. The advent of public access automated external defibrillators have allowed for early defibrillation when applied. Despite the aforementioned improvements in OHCA resuscitation worldwide, the majority of individuals who experience SCA will not survive.
Unfortunately, patient outcomes from OHCA are still poor and the morbidity and mortality in patients who reach return of spontaneous circulation (ROSC) after OHCA are due to the neurologic and cardiac dysfunction that result from prolonged hypoperfusion [7]. In a recent meta-analysis of over 140,000 patients with OHCA, survival to hospital admission was only 23.8 % and survival to hospital discharge only 7.6 % [8].
Pathophysiology of Cardiac Arrest
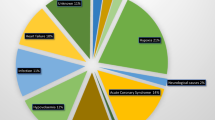
Though OHCAs can occur from noncardiac causes (i.e., trauma, drowning, overdose, asphyxia, electrocution, primary respiratory arrests, and other noncardiac etiologies), the majority (70–80 %) are cardiac in nature [9]. Coronary heart disease is known to be the most common cause of SCA and it is responsible for one in eight deaths worldwide. Many of these deaths are attributed to the development of ventricular tachyarrhythmias that occur during myocardial ischemia; this creates an unstable electrical substrate capable of arrhythmogenesis. Other cardiac causes of SCA include cardiomyopathy, inherited arrhythmia syndromes, and valvular heart disease [10].
Though SCA most often develops in older adults, it can occur in younger patients, where it is most commonly associated with inherited disease [10].
The presenting rhythms in SCA are categorized into two broad categories: tachyarrhythmic and nontachyarrhythmic (PEA, asystole, extreme bradycardia) [11, 12]. This distinction between causative cardiac rhythms in SCA is important given the significantly different survival rates and therapeutic role of defibrillation. The importance of early defibrillation in the management of ventricular defibrillation was demonstrated in a study of patients who experienced in-hospital cardiac arrest; patients who received prompt defibrillation had a survival to discharge rate of 39.3 % whereas patients in whom defibrillation was delayed by 2 min or more from the onset of VF had a survival to discharge rate of 22.2 % [13].
Multiple studies of OHCA have shown that the incidence of tachyarrhythmic rhythms, which include ventricular fibrillation (VF) and pulseless ventricular tachycardia (VT), has been decreasing. It is thought that improved medical and surgical treatment for ischemic heart disease along with the widespread use of implantable cardiac defibrillators (ICDs) have likely contributed to the declining incidence of VF arrest and may result in conversion of an otherwise VF event into a PEA arrest [3].
Pathophysiology of Post Cardiac Arrest Syndrome
Although the majority of cardiac arrest patients die during the acute event, a substantial proportion of cardiac arrest deaths occur in patients following successful resuscitation and can be attributed to the development of post-cardiac arrest syndrome [14]. This describes a complex set of pathophysiological processes consisting of brain injury, myocardial depression, and systemic ischemia/reperfusion injury, as well as ongoing injury caused by the precipitating cause of the arrest [15, 16]. The severity of each of the above is not uniform and varies across individuals.
The mechanisms of brain injury triggered by cardiac arrest are complex and include excitotoxicity, disrupted calcium homeostasis, free radical formation, pathological protease cascades, and activation of cell death signaling pathways [15]. And, as a result, cardiac arrest results in varying degrees of cognitive injury. The prevalence of seizures, nonconvulsize status epilepticus, and other epileptiform activity among patients who are comatose after cardiac arrest is estimated to be 12–22 % [17, 18].
Immediately after ROSC, there is a period of cerebral hyperemia. The intensity of neuropathologic alterations that occur during this time are varied and proportional to the duration of cardiac arrest [15]. Within seconds after the onset of cardiac arrest, intracellular acidosis develops, mitochondrial oxidative phosphorylation stops, adenosine triphosphate (ATP) is depleted, and lactate accumulates [19].
Post-cardiac arrest myocardial dysfunction also contributes to the low survival rate after cardiac arrest. Post-cardiac arrest myocardial dysfunction can be detected within min of ROSC. In one group of 148 patients who underwent coronary angiography after cardiac arrest, 49 % of patients had myocardial dysfunction manifested by tachycardia and elevated left ventricular end-diastolic pressure, followed approximately 6 h later by hypotension (MAP <75 mmHg) and low cardiac output [20]. The whole-body ischemia/reperfusion of cardiac arrest, along with associated oxygen debt causes generalized activation of immunological and coagulation pathways, increasing the risk of multiple organ failure and infection [21, 22]. This condition has many features in common with sepsis [23, 24].
Cardiac Arrest Resuscitation Management
In 2015 the American Heart Association (AHA) issued an updated to the 2010 guidelines. This update addressed areas within the previous guidelines where significant advances had been made in the science, or where there was considerable controversy. The update was released in October of 2015 and addresses out of hospital cardiac arrest, in hospital cardiac arrest, post-resuscitation care as well as exploring regionalized care for cardiac arrest. Major science that contributed to the 2015 Guideline Update will be discussed in the proceeding sections.
Bystander CPR
Bystander-initiated cardiopulmonary resuscitation (CPR) is essential to increase the chance of survival and neurological recovery [25]. In fact, bystander CPR can improve survival from OHCA by two–three fold [8]. Bystander CPR may prevent ventricular fibrillation from deteriorating to asystole and in addition, it increases the chance of defibrillation success, helps to preserve heart and neurologic function and improves overall survival [8, 26]. Based on a 2015 update to the AHA guidelines, untrained lay rescuers should provide compression-only CPR, with or without dispatcher assistance and this should continue until the arrival of an AED or rescuers with advanced training. If the rescuer is able to perform rescue breaths, these should be performed in a ration of 30 compressions to 2 breaths [26].
In a blinded, randomized, controlled trial conducted in Stockholm from April 2012 to December 2013, a mobile-phone positioning system that was activated when ambulance, fire, and police services were dispatched was used to locate trained volunteers within 50 m of patients with OHCA. These volunteers were dispatched to patients (intervention group) or not dispatched to them (control group). In the 667 OHCA that these volunteers were dispatched to, the rate of bystander-initiated CPR was 62 % in the intervention group and 48 % in the control group [27]. These data led that AHA to suggest that communities incorporate social media technology into their dispatch systems to summon volunteers trained in CPR to the scene of persons with OHCA [16].
The primary goal of CPR is to restore blood flow to the heart so that it can resume mechanical work and to maintain the energy state of the brain in order to minimize ischemic injury. The major limiting factor to oxygen delivery during CPR is blood flow; it is therefore important to maximize the oxygen content of arterial blood by maximizing inspired oxygen concentration.
The quality of CPR and chest compressions is known to be a major determinant in the rate of survival from cardiac arrest. [28] A recent study by the Resuscitation Outcomes Consortium, a large pre-hospital clinical research collaboration, demonstrated the association between chest compression rate and ROSC [29, 30]. It has been well-documented that faulty resuscitation efforts are often due to inadequate compression rate and depth; both of which may reduce survival.
The 2015 AHA Guidelines established an upper limit for the recommended compression rate. This update was based on data that suggests that an excessive rate may be associated with a lower rate of return of spontaneous circulation (ROSC). An upper limit on compression depth was also introduced. In adult cardiac arrest patients, rescuers should perform chest compressions at a rate of 100–120/min (updated from at least 100/min). Chest compressions should be performed at a depth of at least 2 inches (5 cm) for adult patients of average size, avoiding excessive compression depths (greater than 2.4 inches or 6 cm) [16, 26].
Because manual chest compressions can be difficult to do and can cause significant operator fatigue, mechanical devices are being studied that produce more consistent chest compressions. Current mechanical devices include the LUCAS system [31] and the Load Distributing Band (Autopulse) system [32]. Both devices are associated with outcomes that are similar to those obtained with manual chest compressions [31–33]
Public Access Automated External Defibrillators
The development of automated external defibrillators (AEDs) revolutionized the resuscitation of patients with OHCA. AEDs monitor a patient’s ECG via self-adhesive electrodes that are applied to the patient’s chest. Equipped with AEDs, EMS personnel achieve higher resuscitation and survival rates than those with only manual defibrillators or without defibrillators at all [11]. This is thought to be due to the reduction of time to first-shock delivery with AEDs [11].
Widespread AED availability in the community has improved survival from prehospital cardiac arrest. One large public-access defibrillation study demonstrated a significant increase in the survival of OHCA victims to hospital discharge when lay volunteers are trained in both AED use and CPR (30 survivors among 128 arrests; 23 %) compared to CPR only (15 among 107; 14 %; p = 0.03) [11, 34]. AED use by law enforcement and in schools has shown similar benefit [35, 36].
A 2-year study that looked at outcomes from sudden cardiac arrest in 2149 US high schools demonstrated that an AED was applied in 85 % (n = 59) of cases and shock delivered onsite in 66 %. Seventy-one percent of SCA victims survived to hospital discharge, including 85 % of students and 61 % of adults [35].
Organized community programs that prepare the lay public to provide bystander CPR and early defibrillation provide the best opportunity for improving outcomes for patients with OHCA. Patients who develop sudden OHCA depend on community response for support. Lay rescuers must recognize the arrest, call for help, and initiate CPR and early defibrillation (public-access defibrillation [PAD]) prior to the arrival of a team of EMS professionals who then transport the patient to an Emergency Department (ED). The 2015 AHA guidelines point out that a cardiac arrest can present anywhere, at home, in a public arena, or in an inpatient hospital bed. The system of care must be able to manage cardiac emergencies wherever they may occur.
In preparation for the AHA 2015 guidelines, evidence from several studies on the use of public access defibrillation was reviewed. The use of automated external defibrillators (AEDs) by laypersons continues to improve survival from OHCA [16]. Efforts to improve implementation of public access defibrillation programs for the treatment of patients with OHCA in communities who have persons at risk for cardiac arrest.
Hemodynamic-Guided Resuscitation
Though CPR efforts are primarily concerned with maintenance of adequate myocardial blood flow, much of the morbidity associated with SCA is attributed to global brain hypoxic ischemic injury [37].
Conventional methods for optimal resuscitation are “rescuer focused” in that the rescuer provides an optimal rate and depth of compression. Current resuscitation algorithms are driven by this approach and all victims essentially receive the same treatment. Recent studies have begun to explore more individualized “patient centered” resuscitation methods, which monitor and seek to optimize hemodynamic response during ongoing resuscitation [38, 39].
Though the American Heart Association recommends that resuscitation efforts be monitored using arterial blood pressure, no study has demonstrated that targeting these goals during resuscitation improves survival [39, 40]. ROSC after SCA depends on adequate myocardial blood flow during CPR [41, 42]. The principle determinant of myocardial blood flow is coronary perfusion pressure (CPP), which is the mathematical difference between arterial and right atrial diastolic pressures [43]. Though it is unrealistic to measure myocardial blood flow during resuscitation efforts, both CPP and arterial diastolic pressure are readily available in many ICUs.
A 2013 study that used a porcine model of asphyxia-associated VF cardiac arrest found that blood pressure targeted, “patient-centered” resuscitation efforts improved 24-h survival compared with optimal provider-centered” efforts per current resuscitation algorithms outlined by AHA-guideline care [39]. Findings from this study highlight a promising new trend for the use of hemodynamic monitoring to guide resuscitation efforts and to ultimately improve survival after cardiac arrest.
Airway
The 2010 AHA Guidelines emphasized the prioritization of circulation over ventilation, reflecting both the importance of blood flow in successful resuscitation and the practical delays that are often inherent in the initiation of rescue breaths [28]. Options to support ventilation and oxygenation include standard bag-mask ventilation versus the placement of an advanced airway (i.e. endotracheal tube (ETT), supraglottic airway device (SGA). Recent studies along with the 2015 AHA summary did not demonstrate any difference in either survival or neurologic outcome with bag-mask ventilation compared with endotracheal intubation or other advanced airway device [44–49].
Use of respiratory mechanics monitors have been reported to prevent excessive pressures and tidal volumes and exhaled CO2 monitors may help assess that actual gas exchange is occurring during face-maks PPV attempts. Although use of such devices is feasible, thus far their effectiveness, particularly in changing important outcomes, has not been established. A laryngeal mask may be considered as an alternative to tracheal intubation if face-mask ventilation is unsuccessful in achieving effective ventilation.
Pharmacologic Management
A recent prospective randomized controlled trial studied 336 victims of OHCA, randomly assigning them to receive a maximum of 4 injections of either 40 IU of vasopressin (vasopressin group) or 1 mg of epinephrine (epinephrine group) immediately upon admission to the Emergency Department (ED). Patients were excluded if they received vasopressors prior to ED admission or if they suffered from non-cardiogenic arrest. No difference was found between the two groups in the rates of ROSC (28.7 vs. 26.6 %), 24 h survival (16.9 vs 20.3 %), or survival to hospital discharge (5.6 vs. 3.8 %) [50].
AHA 2015 guidelines reinforced the use of standard dose epinephrine (1 mg every 3–5 min) based on a new prospective randomized clinical trial that demonstrated both improved ROSC and survival to hospital admission [16]. The pharmacologic approach to cardiac arrest was streamlined by the removal of vasopressin from the ACLS Cardiac Arrest Algorithm; this was based on evidence demonstrating the equivalence of effect between the two medications [16]. The recommendations for timing of epinephrine administration were updated and are now based on the initial presenting rhythm. For a nonshockable rhythm, it may be reasonable to administer epinephrine as soon as feasible. For patients with a shockable rhythm, resuscitation efforts should be focused on defibrillation as there is insufficient evidence and those no specific recommendation regarding the optimal timing of epinephrine administration [16].
Management of Post Cardiac Arrest Syndrome
Care of the post-cardiac arrest patient is time-sensitive and requires a multi-disciplinary team approach including therapies, intervention and intensive care monitoring. Early hemodynamic optimization or early goal-directed therapy is an algorithmic approach to restoring and maintaining the balance between systemic oxygen delivery and demands. This approach focuses on optimization of preload, arterial oxygen content, afterload, contractility, and systemic oxygen utilization [15]. Hemodynamic instability is common after cardiac arrest and manifests as dysrythmias, hypotension, and low cardiac index [20]. Maintaining adequate tissue perfusion while limiting oxidative injury is paramount. Additional therapies have been deployed to impart neuro-protection to the PCAS patient, including Targeted Temperature Management (TTM).
Targeted Temperature Management
After ROSC, unconscious patients are at high risk for death and neurologic deficits are common in those who survive [51]. Targeted temperature management is one of the few therapies that contributed to improved survival with good neurological outcomes in comatose patients admitted to the hospital after OHCA. Early studies demonstrated that, among patients in whom spontaneous circulation has been restored after cardiac arrest due to ventricular fibrillation, systemic cooling to a bladder temperature between 32 and 34 °C for 24 h increased the chance of survival and of a favorable neurologic outcome [52, 53]. Though significant controversy remains regarding the optimal target temperature in targeted temperature management, several randomized controlled trials have demonstrated that targeted temperature management can reduce post-arrest anoxic-ischemic brain injury and improve functional outcomes [15, 54–56]
Prehospital Use of Cold Saline
Sudden cardiac arrest results in the immediate interruption of perfusion with consequent global ischemia. In 1987, Bulkley first proposed the bimodal model of injury due to prolonged ischemia followed by reperfusion [57]. The first phase is mainly due to ischemia and the extent of damage depends on the duration of ischemia. When oxygen is reintroduced and perfusion restored, the infiltration of reactive oxygen species and pro-inflammatory processes lead to further biochemical changes. After cardiac arrest with no perfusion for more than 5 min, the generation of free radicals, together with other inflammatory mediators during reperfusion leads to chemical cascades that result in cerebral injury [58].
Despite advances in CPR, reperfusion injury often leads to devastating neurologic damage resulting in anoxic brain injury and other unfavorable neurologic outcomes. Two clinical trials that were published in 2002 demonstrated that the induction of mild hypothermia could improve survival and functional neurologic outcome in comatose survivors of OHCA [52, 53].
Evidence has demonstrated that mild therapeutic hypothermia after cardiac arrest increases the rate of favorable neurologic outcome and decreases mortality. There are multiple mechanisms through which mild hypothermia may improve neurological outcome following ischemia–reperfusion injury; cooling reduces apoptosis, inhibits the neuroexcitatory cascade, decreases cerebral metabolism, suppresses the production of proinflammatory cytokines, and reduces free-radical production and vascular permeability [59].
Recent reports have brought into question the efficacy and safety of prehospital therapeutic hypothermia. Several randomized controlled trials have tested prehospital administration of cold intravenous fluids to initiate hypothermia after OHCA. The absence of any benefit and the presence of some complications during these trials led to a recommendation against the routine prehospital cooling of patients after ROSC using rapid infusion of cold saline [60]. However, this recommendation does not preclude the use of cold intravenous fluids in more controlled or more selected settings and did not address other methods of inducing hypothermia [16, 61].
Maternal Resuscitation
Fortunately, cardiac arrest in pregnancy is relatively rare, particularly in the Western world. The American Heart Association estimates that in the United States, maternal cardiac arrest occurs at a rate of 8.5 arrests per 100,000 hospitalizations for delivery or 1:12000. Females who are most likely to suffer cardiac arrest during pregnancy are black women (non-Hispanic by U.S. Centers for Disease Control and Prevention race/ethnicity coding), aged 35 and older.
Though survival to hospital discharge is largely dependent upon the arrest etiology, the best outcomes for both mother and fetus are likely to be achieved through successful maternal resuscitation. Though hemorrhage is the most common cause of maternal arrest, other medical conditions that are strongly associated with cardiopulmonary arrest include cardiovascular disease (ischemic heart disease, aortic dissection, myocarditis, congenital heart disease, valvular disease, and pre-existing hypertension), liver disease, systemic lupus erythematosus (SLE), amniotic fluid embolism, sepsis, aspiration pneumonitis, pulmonary embolism, and eclampsia.
Management of the unstable pregnant patient requires optimization of maternal hemodynamics. The patient should be placed in a full left lateral decubitus position in order relieve aortocaval compression. She should be given 100 % oxygen by facemask and intravenous access should be established above the diaphragm in order to ensure that intravenous therapy is not obstructed by the gravid uterus.
Patient positioning during CPR affects the overall quality of CPR and resultant compression force and cardiac output. For high-quality chest compressions, the patient should be laying supine, on a solid flat surface. Recommendations for chest compressions for pregnant patients are equivalent to those for all adult patients. The rescuer’s hands must be placed correctly and the correct rate and depth of compressions must be performed at a steady rate, with interruptions minimized and limited to 10 s outside of specific interventions such as placement of an advanced airway or use of a defibrillator [62•]. One large randomized trial that studied adults with OHCA, found that compared with continuous manual chest compressions with positive-pressure ventilation, manual chest compressions with interruptions for ventilation performed by EMS providers was not associated with a significantly higher rate of survival to discharge or a favorable neurologic function [63].
When performed in the right circumstances, a perimortem caesarean section (PMCS) has the potential to save both the pregnant woman and her baby. Starting from the gestational age of 20 weeks, the gravid uterus causes aortocaval compression, thereby impending venous return and cardiac output [64, 65]. Delivery of the fetus and placenta improves venous return and cardiac output, facilitating closed chest compressions, reducing oxygen consumption, and making it easier to ventilate [66]. The greater the gestational age, the greater the potential benefit of performing a PMCS. Revised recommendations by the AHA state that PMCS should be performed from 20 weeks gestation to women with an obviously gravid uterus that is deemed sufficiently large such that it causes aortocaval compression [67].
Because pregnant women become hypoxic more quickly than non-pregnant women, irreversible brain damage can occur within 4–6 min of cessation of cerebral blood flow [65]. For PMCS to be indicated, all three of the following must apply: unsuccessful attempts at resuscitation at 4 min post maternal cardiac arrest, gestation 20–24 weeks or greater (i.e. uterine fundus palpable at or above umbilicus), and ‘short’ time interval from onset of maternal cardiac arrest (PMCS should ideally be initiated at 4 min and completed by 5 min post arrest, but it should still be considered at 15 min post arrest) [66].
Conclusion
Outcomes from cardiac arrest have improved over time, with a focus on pre-hospital CPR quality, public access to defibrillation and adherence to guideline concordant bundles of post-arrest care. However, given the continued high rates of morbidity and mortality, further investigation continues to be necessary to reduce the public health burden of cardiac arrest. In 2015, the American Heart Association issued a guideline update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care and created the first Maternal Resuscitation Algorithm. In order to observe widespread improvements in outcomes from cardiac arrest, it is critical that patients receive guideline concordant care in order to optimize their chances for recovery.
References
Papers of particular interest, published recently, are highlighted as: • Of importance •• Of major importance
•• Callaway CW, Donnino MW, Fink EL, Geocadin RG, Golan E, Kern KB, et al. Part 8: Post–Cardiac Arrest Care 2015 American Heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18 suppl 2):S465–82. This manuscript details the 2015 AHA Guideline update for post-arrest care. The authors gave a stronger recommendation for the use of targeted temperature management for all initial arrest rhythms and for both in and out of hospital cardiac arrest patients.
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics–2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–322.
Keller SP, Halperin HR. Cardiac Arrest: the changing incidence of ventricular fibrillation. Curr Treat Options Cardiovasc Med. 2015;17(7):392.
Weisfeldt ML, Everson-Stewart S, Sitlani C, Rea T, Aufderheide TP, Atkins DL, et al. Ventricular tachyarrhythmias after cardiac arrest in public versus at home. N Engl J Med. 2011;364(4):313–21.
Engdahl J, Holmberg M, Karlson BW, Luepker R, Herlitz J. The epidemiology of out-of-hospital “sudden” cardiac arrest. Resuscitation. 2002;52(3):235–45.
Reinier K, Nichols GA, Huertas-Vazquez A, Uy-Evanado A, Teodorescu C, Stecker EC, et al. Distinctive clinical profile of blacks versus whites presenting with sudden cardiac arrest. Circulation. 2015;132(5):380–7.
Uchino H, Ogihara Y, Fukui H, Chijiiwa M, Sekine S, Hara N, et al. Brain injury following cardiac arrest: pathophysiology for neurocritical care. J Intensive Care [Internet]. 2016 Apr 27 [cited 2016 May 27];4. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4847238/.
Sasson C, Rogers MAM, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3(1):63–81.
Out-of-Hospital Cardiac Arrest Surveillance—Cardiac Arrest Registry to Enhance Survival (CARES), United States, October 1, 2005–December 31, 2010 [Internet]. [cited 2015 Nov 23]. Available from: http://www.cdc.gov/mmwr/preview/mmwrhtml/ss6008a1.htm.
Hayashi M, Shimizu W, Albert CM. The spectrum of epidemiology underlying sudden cardiac death. Circ Res. 2015;116(12):1887–906.
Patil KD, Halperin HR, Becker LB. Cardiac arrest: resuscitation and reperfusion. Circ Res. 2015;116(12):2041–9.
Goldberger JJ, Basu A, Boineau R, Buxton AE, Cain ME, Canty JM, et al. Risk stratification for sudden cardiac death: a plan for the future. Circulation. 2014;129(4):516–26.
Chan PS, Krumholz HM, Nichol G, Nallamothu BK. American Heart Association National Registry of Cardiopulmonary resuscitation investigators. delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med. 2008;358(1):9–17.
Girotra S, Chan PS, Bradley SM. Post-resuscitation care following out-of-hospital and in-hospital cardiac arrest. Heart Br Card Soc. 2015;101(24):1943–9.
Nolan JP, Neumar RW, Adrie C, Aibiki M, Berg RA, Bbttiger BW, et al. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication: a scientific statement from the International Liaison Committee on Resuscitation; the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; the Council on Stroke (Part II). Int Emerg Nurs. 2010;18(1):8–28.
Neumar RW, Shuster M, Callaway CW, Gent LM, Atkins DL, Bhanji F, et al. Part 1: executive Summary 2015 American Heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18 suppl 2):S315–67.
Longstreth WT, Fahrenbruch CE, Olsufka M, Walsh TR, Copass MK, Cobb LA. Randomized clinical trial of magnesium, diazepam, or both after out-of-hospital cardiac arrest. Neurology. 2002;59(4):506–14.
Rittenberger JC, Popescu A, Brenner RP, Guyette FX, Callaway CW. Frequency and timing of nonconvulsive status epilepticus in comatose post-cardiac arrest subjects treated with hypothermia. Neurocrit Care. 2012;16(1):114–22.
Chalkias A, Xanthos T. Post-cardiac arrest brain injury: pathophysiology and treatment. J Neurol Sci. 2012;315(1):1–8.
Laurent I, Monchi M, Chiche J-D, Joly L-M, Spaulding C, Bourgeois B, et al. Reversible myocardial dysfunction in survivors of out-of-hospital cardiac arrest. J Am Coll Cardiol. 2002;40(12):2110–6.
Cerchiari EL, Safar P, Klein E, Diven W. Visceral, hematologic and bacteriologic changes and neurologic outcome after cardiac arrest in dogs, the visceral post-resuscitation syndrome. Resuscitation. 1993;25(2):119–36.
Adams JA. Endothelium and cardiopulmonary resuscitation. Crit Care Med. 2006;34(12 Suppl):S458–65.
Adrie C, Laurent I, Monchi M, Cariou A, Dhainaou J-F, Spaulding C. Postresuscitation disease after cardiac arrest: a sepsis-like syndrome? Curr Opin Crit Care. 2004;10(3):208–12.
Adrie C, Adib-Conquy M, Laurent I, Monchi M, Vinsonneau C, Fitting C, et al. Successful cardiopulmonary resuscitation after cardiac arrest as a “sepsis-like” syndrome. Circulation. 2002;106(5):562–8.
Stiell I, Nichol G, Wells G, De Maio V, Nesbitt L, Blackburn J, et al. Health-related quality of life is better for cardiac arrest survivors who received citizen cardiopulmonary resuscitation. Circulation. 2003;108(16):1939–44.
Kleinman ME, Brennan EE, Goldberger ZD, Swor RA, Terry M, Bobrow BJ, et al. Part 5: adult basic life support and cardiopulmonary resuscitation quality: 2015 american heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18 Suppl 2):S414–35.
Ringh M, Rosenqvist M, Hollenberg J, Jonsson M, Fredman D, Nordberg P, et al. Mobile-phone dispatch of laypersons for CPR in out-of-hospital cardiac arrest. N Engl J Med. 2015;372(24):2316–25.
Berg RA, Hemphill R, Abella BS, Aufderheide TP, Cave DM, Hazinski MF, et al. Part 5: adult basic life support: 2010 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122(18 Suppl 3):S685–705.
Idris AH, Guffey D, Aufderheide TP, Brown S, Morrison LJ, Nichols P, et al. The relationship between chest compression rates and outcomes from cardiac arrest. Circulation. 2012;125(24):3004–12.
Abella BS. The importance of cardiopulmonary resuscitation quality. Curr Opin Crit Care. 2013;19(3):175–80.
Rubertsson S, Lindgren E, Smekal D, Östlund O, Silfverstolpe J, Lichtveld RA, et al. Mechanical chest compressions and simultaneous defibrillation vs conventional cardiopulmonary resuscitation in out-of-hospital cardiac arrest: the LINC randomized trial. JAMA. 2014;311(1):53–61.
Wik L, Olsen J-A, Persse D, Sterz F, Lozano M, Brouwer MA, et al. Manual vs. integrated automatic load-distributing band CPR with equal survival after out of hospital cardiac arrest. the randomized CIRC trial. Resuscitation. 2014;85(6):741–8.
Perkins GD, Lall R, Quinn T, Deakin CD, Cooke MW, Horton J, et al. Mechanical versus manual chest compression for out-of-hospital cardiac arrest (PARAMEDIC): a pragmatic, cluster randomised controlled trial. Lancet Lond Engl. 2015;385(9972):947–55.
Hallstrom AP, Ornato JP, Weisfeldt M, Travers A, Christenson J, McBurnie MA, et al. Public-access defibrillation and survival after out-of-hospital cardiac arrest. N Engl J Med. 2004;351(7):637–46.
Drezner JA, Toresdahl BG, Rao AL, Huszti E, Harmon KG. Outcomes from sudden cardiac arrest in US high schools: a 2-year prospective study from the National Registry for AED Use in Sports. Br J Sports Med. 2013;47(18):1179–83.
Husain S, Eisenberg M. Police AED programs: a systematic review and meta-analysis. Resuscitation. 2013;84(9):1184–91.
Friess SH, Sutton RM, French B, Bhalala U, Maltese MR, Naim MY, et al. Hemodynamic directed CPR improves cerebral perfusion pressure and brain tissue oxygenation. Resuscitation. 2014;85(9):1298–303.
Neumar RW, Otto CW, Link MS, Kronick SL, Shuster M, Callaway CW, et al. Part 8: adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122(18 Suppl 3):S729–67.
Sutton RM, Friess SH, Naim MY, Lampe JW, Bratinov G, Weiland TR, et al. Patient-centric Blood Pressure–targeted Cardiopulmonary Resuscitation Improves Survival from Cardiac Arrest. Am J Respir Crit Care Med. 2014;190(11):1255–62.
Meaney PA, Bobrow BJ, Mancini ME, Christenson J, de Caen AR, Bhanji F, et al. Cardiopulmonary resuscitation quality: [corrected] improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association. Circulation. 2013;128(4):417–35.
Kern KB, Ewy GA, Voorhees WD, Babbs CF, Tacker WA. Myocardial perfusion pressure: a predictor of 24-hour survival during prolonged cardiac arrest in dogs. Resuscitation. 1988;16(4):241–50.
Ralston SH, Voorhees WD, Babbs CF. Intrapulmonary epinephrine during prolonged cardiopulmonary resuscitation: improved regional blood flow and resuscitation in dogs. Ann Emerg Med. 1984;13(2):79–86.
Sanders AB, Ewy GA, Taft TV. Prognostic and therapeutic importance of the aortic diastolic pressure in resuscitation from cardiac arrest. Crit Care Med. 1984;12(10):871–3.
McMullan J, Gerecht R, Bonomo J, Robb R, McNally B, Donnelly J, et al. Airway management and out-of-hospital cardiac arrest outcome in the CARES registry. Resuscitation. 2014;85(5):617–22.
Shin SD, Ahn KO, Song KJ, Park CB, Lee EJ. Out-of-hospital airway management and cardiac arrest outcomes: a propensity score matched analysis. Resuscitation. 2012;83(3):313–9.
Hanif MA, Kaji AH, Niemann JT. Advanced airway management does not improve outcome of out-of-hospital cardiac arrest. Acad Emerg Med Off J Soc Acad Emerg Med. 2010;17(9):926–31.
Studnek JR, Thestrup L, Vandeventer S, Ward SR, Staley K, Garvey L, et al. The association between prehospital endotracheal intubation attempts and survival to hospital discharge among out-of-hospital cardiac arrest patients. Acad Emerg Med Off J Soc Acad Emerg Med. 2010;17(9):918–25.
Takei Y, Enami M, Yachida T, Ohta K, Inaba H. Tracheal intubation by paramedics under limited indication criteria may improve the short-term outcome of out-of-hospital cardiac arrests with noncardiac origin. J Anesth. 2010;24(5):716–25.
Link MS, Berkow LC, Kudenchuk PJ, Halperin HR, Hess EP, Moitra VK, et al. Part 7: adult advanced cardiovascular life support: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18 Suppl 2):S444–64.
Mukoyama T, Kinoshita K, Nagao K, Tanjoh K. Reduced effectiveness of vasopressin in repeated doses for patients undergoing prolonged cardiopulmonary resuscitation. Resuscitation. 2009;80(7):755–61.
Moulaert VRMP, Verbunt JA, van Heugten CM, Wade DT. Cognitive impairments in survivors of out-of-hospital cardiac arrest: a systematic review. Resuscitation. 2009;80(3):297–305.
Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346(8):549–56.
Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346(8):557–63.
Donnino MW, Andersen LW, Berg KM, Reynolds JC, Nolan JP, Morley PT, et al. Temperature Management after cardiac arrest: an advisory statement by the advanced life support task force of the international liaison committee on resuscitation and the american heart association emergency cardiovascular care committee and the council on cardiopulmonary, critical care, perioperative and resuscitation. Resuscitation. 2016;98:97–104.
Dale CM, Sinuff T, Morrison LJ, Golan E, Scales DC. Understanding early decisions to withdraw life-sustaining therapy in cardiac arrest survivors: a qualitative investigation. Ann Am Thorac Soc. 2016;13(7):1115–22.
Nielsen N, Wetterslev J, Cronberg T, Erlinge D, Gasche Y, Hassager C, et al. Targeted temperature management at 33°C versus 36°C after cardiac arrest. N Engl J Med. 2013;369(23):2197–206.
Bulkley GB. Free radical-mediated reperfusion injury: a selective review. Br J Cancer Suppl. 1987;8:66–73.
Negovsky VA. Postresuscitation disease. Crit Care Med. 1988;16(10):942–6.
Nolan JP, Soar J, Zideman DA, Biarent D, Bossaert LL, Deakin C, et al. European Resuscitation council guidelines for resuscitation 2010 section 1. executive summary. Resuscitation. 2010;81(10):1219–76.
Kim F, Nichol G, Maynard C, Hallstrom A, Kudenchuk PJ, Rea T, et al. Effect of prehospital induction of mild hypothermia on survival and neurological status among adults with cardiac arrest: a randomized clinical trial. JAMA. 2014;311(1):45–52.
Cortez E, Panchal AR, Davis J, Zeeb P, Keseg DP. Clinical Outcomes in cardiac arrest patients following prehospital treatment with therapeutic hypothermia. Prehospital Disaster Med. 2015;30(5):452–6.
• Jeejeebhoy FM, Zelop CM, Lipman S, Carvalho B, Joglar J, Mhyre JM, et al. Cardiac arrest in pregnancy: A scientific statement from the American Heart Association. Circulation. 2015;132(18):1747–73. This represents the first maternal resuscitation algorithm. Although a rare event, resuscitating a pregnant woman from cardiac arrest may yield different challenges than the general patient population and having this guideline to support decision-making may improve outcomes.
Nichol G, Leroux B, Wang H, Callaway CW, Sopko G, Weisfeldt M, et al. Trial of continuous or interrupted chest compressions during cpR. N Engl J Med. 2015;373(23):2203–14.
Kerr MG. THE mechanical effects of the gravid uterus in late pregnancY. J Obstet Gynaecol Br Commonw. 1965;72:513–29.
Katz V, Balderston K, DeFreest M. Perimortem cesarean delivery: were our assumptions correct? Am J Obstet Gynecol. 2005;192(6):1916–20.
Parry R, Asmussen T, Smith JE. Perimortem caesarean section. Emerg Med J EMJ. 2016;33(3):224–9.
Hui D, Morrison LJ, Windrim R, Lausman AY, Hawryluck L, Dorian P, et al. The American Heart Association 2010 guidelines for the management of cardiac arrest in pregnancy: consensus recommendations on implementation strategies. J Obstet Gynaecol Can JOGC J Obstétrique Gynécologie Can JOGC. 2011;33(8):858–63.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interests
Drs Milan and Perman declare no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain studies with human or animal subjects performed by the author.
Additional information
This article is part of the Topical collection on Acute Coronary Syndrome.
Rights and permissions
About this article
Cite this article
Milan, M., Perman, S.M. Out of Hospital Cardiac Arrest: A Current Review of the Literature that Informed the 2015 American Heart Association Guidelines Update. Curr Emerg Hosp Med Rep 4, 164–171 (2016). https://doi.org/10.1007/s40138-016-0118-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40138-016-0118-x