Abstract
Pain is a common complaint in the emergency and acute care settings. Adequate control of a child’s pain is important for improved patient assessments and can have long-term benefits affecting future medical care. Pain in children may be difficult to distinguish from anxiety, but there are validated tools to assist in objectively quantifying the severity pain in children of all ages. Pharmacologic as well as non-pharmacologic pain therapies can be effective. Providers who practice in the prehospital, emergency department, and other acute care settings should consider standardized protocols or guidelines for ensuring that pain is assessed and treated in a timely and safe manner.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Control of pain and stress for children is a vital component of emergency medical care. Many patients present to the emergency department (ED) with pain related to injury or other medical or surgical conditions that are not always related to trauma. Pain is known to negatively affect the social, physical, and emotional well-being of a child. Timely administration of analgesia affects the entire emergency medical experience and can have a lasting effect on a child’s and family’s reaction to current and future medical care [1]. Thus, the emergency care staff, including prehospital providers, should be capable of assessing and safely managing pediatric pain.
Pain assessment and management have been identified as a priority by a number of organizations and accreditation bodies, including the Joint Commission, the American Academy of Pediatrics (AAP), the American College of Emergency Physicians, and the National Association of EMS Physicians (NAEMSP) [2]. The NAEMSP Position Statement “Prehospital Pain Management” states that pain relief should be a priority for every emergency medical services (EMS) system and goes further to identify the components that should be included in prehospital protocols:
-
Mandatory assessment
-
Reliable assessment tools
-
Pharmacologic and non-pharmacologic treatments
-
Mandatory patient monitoring
-
Indications and contraindications
-
Transfer of information
An evidence-based guideline for prehospital analgesia in trauma has been published [3•], and a model EMS clinical guideline for pain management was published online by the National Association of State EMS Officials [4].
Prevalence of Pain in Emergency Services
Sixty percent of patients transported by EMS suffer from conditions in which they could benefit from prehospital pain interventions [5]. An estimated ten percent of patients treated in EDs who arrive by emergency medical services (EMS) are under the age of eighteen [6]. An analysis of the National Ambulatory Medical Care Survey showed that at least 20 % of children who arrive in the ED via EMS have pain severe enough to warrant treatment (Fig. 1). Unfortunately, this study also noted that more than half of children did not have documentation of their pain assessment, if it was performed [6].
There is evidence that the majority of prehospital providers do not perform pain assessments and are uncomfortable administering pain medication in adolescents and children [7]. EMS personnel self-report that children’s pain is less thoroughly measured and treated than adults’ pain [8]. A survey of EMS providers [7] identified barriers to both pediatric pain assessment and treatment. A factor that likely contributes to the discomfort and limited self-efficacy of EMS providers is the fact that children under the age of 18 account for only 7 % of EMS responses [9].
Children who present directly from home are often in need of pain control, also. There seems to be undertreatment of pain prior to presenting to emergency services and children often do not receive pain treatment at home prior to arrival [10, 11].
Pain Concepts
Pain is subjective in nature. Every mechanism and severity of injury or pathologic process leading to inflammation will affect individuals differently. Pain also is multi-dimensional, involving not just the nervous system, but also emotions, cognition, and beliefs. There are three approaches to measuring pain that have been identified in the literature:
-
Self-report
-
Observational or behavioral
-
Physiological
Estimates of pain intensity based on each of these approaches are usually correlated only weakly to moderately with estimates based on the other approaches. The best true estimate may be some combination of these approaches, but in certain populations, not all approaches are feasible. For instance, a patient must have some understanding of the construct of pain assessment in order to be able to generate a response to a self-report scale that indicates intensity of pain, and patients with neuromuscular disorders may not have typical responses to pain that could be observed with behavioral scales.
There is great value in administering pain control for the pediatric patient as early as possible. The immediate benefits will be for the improvement of patient comfort. No one likes to be in pain and increasing patient comfort is better for the patient. Pain relief will also help to improve the patient’s vital signs by decreasing the stress on the body caused by pain. Patient assessment will be easier to perform when the patient is not in as much pain. The patient will be able to respond and interact more comfortably and a more thorough assessment may be performed. Lastly, by decreasing the patient’s pain, their physiologic state will improve. For example, in conditions such as chest wall injuries, control of pain improves respiratory effort.
The value of pain control for pediatric patients also has long-term benefits. According to research conducted by the military, pain management decreases the incidence of post-traumatic stress. There is a noted decrease in the long-term sequelae in children as a result of treating pain early in the prehospital setting. Proactive and early pain treatment may prevent the development of hypersensitized pain pathways in patients who have repeated pain stimuli.
Pain Assessment
Because pain is subjective in nature, self-report should be the primary source of information [12]. Self-report is not always feasible, especially in the case of pre-verbal and developmentally immature children. And while pain is a subjective experience, and self-report is considered the most reliable indicator when available, defining self-report as a “gold standard” is overstated, as even self-report can be affected by the other dimensions associated with pain. Consider the concomitant anxiety that is present in children with painful conditions faced with interacting with healthcare providers, and how this may affect the amount of pain that they report.
Many children as young as 3 years old can provide self-report of pain if age-appropriate tools are used [13]. Assessment of pain for pre-verbal children must be based upon observation of behavior and/or physiologic signs. There are very few scales that have been validated in the prehospital setting; none specifically for children have been validated in the prehospital setting. Brief, reliable, and age-appropriate pain assessment tools have been developed and validated and are widely used in the hospital, post-operative, and emergency settings. While not included as a criterion in these pain assessment tools, studies have shown that parental assessment of their child’s pain is superior to that of healthcare professionals [14, 15].
Two commonly used self-report measures of pain in children for the acute care and inpatient settings are the Faces Pain Scale–Revised (FPS-R) (See www.iasp-pain.org/FPSR) and the Color Analog Scale (CAS). These two have shown to be valid, reliable methods of assessing pain [16]. The Wong-Baker FACES Pain Rating Scale (Fig. 2; see http://www.WongBakerFACES.org) correlated with the visual analog scale in children ages 8–17 years presenting to the ED [17••] and with the color analog scale in children ages 5–16 [18••]. For those who are unable to use self-report scales, behavioral scales can be combined with an evaluation of the patient combined with physical findings to assess the level of pain. Pain in a neonate can be evaluated using the Neonatal Infant Pain Scale (See www.cebp.nl/vault_public/filesystem/?ID=1426 ), and pain in infants, young children, and those with cognitive impairment can be assessed using the FLACC (face, legs, activity, crying and consolability) scale (See http://wps.prenhall.com/wps/media/objects/3103/3178396/tools/flacc.pdf), or Children’s Hospital of Eastern Ontario Pain Scale (See http://www.modernmedicine.com/sites/default/files/images/Resource-Centers/Children’s%20Hospital%20of%20Eastern%20Ontario%20Pain%20Scale%20(CHEOPS).pdf) [1].
Patients with developmental delays or cognitive impairment are frequently encountered in the healthcare setting. These patients are unable to effectively express their level of pain or discomfort, due to limited communication skills, complex pain issues, or maladaptive behaviors. This makes it difficult for prehospital providers as well as emergency providers to accurately assess and treat pain. Efforts have been made to provide behavioral tools to measure pain in these situations, including the Non-Communicating Children’s Pain Checklist (NCCPC) (See http://www.community-networks.ca/wp-content/uploads/2015/07/PainChklst_BreauNCCPC-R2004.pdf), Echelle Douleur Enfant San Salvadour (DESS) (See http://www.pediadol.org/IMG/pdf/San_Sal.pdf), Pediatric Pain Profile (See http://www.ppprofile.org.uk/), revised FLACC (See http://hpcconnection.ca/wp-content/uploads/2014/07/FLACC_R.pdf), and the Pain Indicator for Communicatively Impaired Children. One study compared the NCCPC, DESS, and the Children’s Hospital of Eastern Ontario Pain Scale and found that the NCCPC was the easiest to use for pain assessment in cognitively impaired children [19].
Feasibility studies have shown that including a section on the prehospital patient care record, along with a brief educational intervention, increases the performance of pain assessments by EMS providers [20]. Including a section for recording the pain score and type of pain scale used should be a consideration as EMS agencies move toward electronic patient care records (ePCR). Electronic aids in the ePCR, such as one or more pictorial self-report scales or a table that calculates the score from an observational-behavioral scale, are suggestions. It is also worth noting that the current National EMS Information System (NEMSIS) data dictionary includes a field for pain score, but does not include a field for type of pain scale used. As EMS medical records trend toward following the NEMSIS data dictionary, pediatric providers, medical directors, and EMS coordinators may consider advocating for inclusion of the type of pain scale used to be included in the data collected.
The lack of validated, appropriate pain assessment tools for different age groups in the prehospital setting may be a main reason for lack of assessment and undertreatment of pain in pediatric patients. Without a valid tool, it may be difficult for paramedics to comfortably assess pain in pediatric patients, especially pre-verbal patients. The lack of a validated scale also makes it difficult to study the comparative effectiveness of the treatments performed, because there is no standardized method to measure how much pain is improved with interventions.
It will be helpful for hospitals to work with their EMS agencies to ensure that all involved in the continuum of emergency care recognizes that there are age-appropriate pain scales that can be used to document an objective pain assessment. This will also facilitate the transfer of information that occurs between the prehospital and ED providers. Additional training regarding simple pain measurement tools and the proper use of age-appropriate pain scales for injured children treated in the prehospital setting may help to address potential barriers with assessing and treating pediatric pain.
In the ED, assessment of pain is an important aspect of triage of pediatric patients. It has been shown that pediatric patients with fever are treated more promptly in the ED than patients with pain [21]. Because of the documented undertreatment of pain prior to ED arrival and the noted delay in receiving analgesia, pain should be assessed upon ED arrival and can begin to be addressed in triage. A triage protocol for pain management that includes early application of ice, splinting, enteral or parenteral medications, or topical anesthetics should be in place to be proactive [1]. In a cross-sectional analysis of the National Hospital Ambulatory Medical Care Survey (1997–2000), patients who had pain scores documented were more likely to have their pain treated than patients in whom no score was documented [22]. Simply incorporating a pain assessment tool into the electronic medical record can significantly increase pain assessment in children [23]. Structured pain assessment tools and nurse-initiated oral analgesia protocols reduce time to administration of analgesia and a higher percentage of patients receive analgesia [24]. Caution should be used if using multiple scales, because it has been found that there is little agreement between the different pain scales when used on the same patient [25].
Pain Treatment
Little research has been done to assess the pain relief given at home by parents or caregivers but it appears that children presenting to the ED for pain-related complaints often do not receive pain treatment at home prior to arrival [11]. The administration of pain medications by parents is limited due to parental concerns of hurting their child, not having analgesics readily available at home, and masking their child’s pain severity [26]. In a study including parental pain management of children with limb injuries, younger children were noted to receive analgesics less frequently than older children, which may represent that parents are less concerned about the adverse effects of drugs on older children, and that older children may better express their level of pain and ask for pain medications more often [26]. Parental management of pediatric pain mainly consists of non-pharmacologic techniques, such as ice packs or immobilization of fractures. Community seminars focused on parental education may improve the pre-arrival management of pain in children.
Evidence has shown that patients who arrive to the ED via EMS and do not receive analgesia in the prehospital setting suffer a 60–90 min delay in receiving pain medications [27, 28•]. Because of the impact that EMS can have in decreasing the interval to receipt of analgesia, the evidence-based guideline for prehospital analgesia in trauma [3•] recommends that every patient should be considered a candidate for pain management, regardless of anticipated transport time. Intravenous morphine and intranasal or intravenous fentanyl are the only pharmacologic treatment recommendations in the evidence-based guideline.
As previously stated, many pediatric patients do not have their pain assessment documented, and even fewer receive analgesia during transport [27, 29, 30]. Survey data from EMS providers identified the following barriers to treating pain in children [7]:
-
Inability to assess pain,
-
Difficult vascular access,
-
Fear of complications, and
-
Possibility of drug-seeking behavior (noted for pediatric patients specifically by 65 % of medics surveyed).
EMS scopes of practice are usually focused on assessment and life-threatening situations in children, rather than the actual management of pain. Certification courses, such as Pediatric Advanced Life Support (PALS) and Pediatric Education for Prehospital Professionals (PEPP), offer limited education regarding pediatric pain management [27].
Only a few studies have examined the efficacy of pediatric prehospital analgesia [31]. Evidence for pharmacologic treatment of pain in the prehospital setting is limited to acetaminophen, ibuprofen, and short-acting opiates (i.e., fentanyl, morphine); however, not every EMS agency may carry all of these medications.
Although the lack of medications that are easy to administer (i.e., without needles) was noted as a barrier, with the advent of the mucosal atomizer device and fentanyl, there is a needleless route for pain medication. Intranasal drug delivery has become an alternative method of quickly administering analgesics to children in the emergency setting, though no studies have assessed the efficacy of intranasal versus intravenous drug administration.
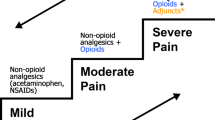
Strategies for treatment of pain in the pediatric ED are largely based on pain scores that are assessed both in triage and by the treating provider. Typically, mild-to-moderate pain can be managed by non-opioid oral analgesics, such as ibuprofen or acetaminophen. Ibuprofen has been shown to be at least as effective [32] or possibly more effective [33] than codeine. Codeine is not only a weak opioid, but also has an increased incidence of side effects compared to other opioids. Because of a genetic tract that interferes with codeine metabolism, about one-third of patients are not able to respond to codeine (“codeine nonresponders”). Moderate-to-severe pain can still be effectively treated with oral medications, and opioid medications such as hydrocodone and oxycodone are frequently used. Intranasal fentanyl is another safe and efficacious delivery method of opioid medication [34], and can be given in a more timely manner than intravenous narcotic medication [35••]. Severe pain is best treated with intravenous opioids, such as morphine, fentanyl, or hydromorphone. Onset of action for intravenous opioids is generally within minutes, with half-lives ranging from 2.3 h (hydromorphone) to 1.5–4.5 h (morphine) to 3.5 h (fentanyl). Sucrose should be available as it has been found to decrease the response to noxious stimuli, such as heel sticks and injections, in neonates [36]. See Table 1 for a list of commonly used pain medications, with typical pediatric and adult (maximum) doses.
Topical anesthetics are a useful adjunct for managing pain associated with procedures. Examples include a topical liposomal 4 % lidocaine cream, which provides anesthesia in approximately 30 min, and topical anesthetic/vasoconstrictor combinations, such as lidocaine, epinephrine, and tetracaine, which can provide excellent wound anesthesia in 20–30 min for laceration repair [37–39]. When vascular access procedures cannot be delayed or need to take place in the prehospital setting, other techniques can be used; intradermal lidocaine injection decreases the pain of venous cannulation without affecting procedural success rate. For those with a true lidocaine allergy, which is very rare, benzoyl alcohol can be used as a local anesthetic. Diphenhydramine has also been used but is not preferred as a local anesthetic since local skin necrosis and sloughing has been reported with its use. Needle-free injection systems using either powder or liquid jet injection, or use of a vapocoolant, reduce the onset time even more [1, 40].
In addition to controlling pain associated with placement of IV catheters and other minor procedures, topical anesthetics also have been reported to improve procedural success rates, likely because of decreased movement leading to better accuracy [41]. The use of vapocoolants can also decrease the pain of needlestick procedures and has been shown to significantly increase the first-attempt success rate for intravenous line placement in children [40]. Available evidence also supports the use of local and topical anesthetic for lumbar puncture in neonates [42].
Lidocaine can be used alone in urgent situations or after topical anesthetics have been applied. Lidocaine can be injected in an almost painless manner by buffering the anesthetic with bicarbonate, warming the lidocaine before injection, and injecting slowly with a small gauge needle [43–46].
Practitioners should remember basic measures for management of pain, including cold compresses, splinting, and elevation, as well as other comfort measures. Part of non-pharmacologic treatment of pain includes considering the environment. In the hospital and ED settings, reducing fear and anxiety can help reduce stress related to a painful procedure. Stress management and emotional support are essential to providing a comfortable environment for the child and have been shown to reduce anxiety in older children as well as parental perception of pain in younger children [47•]. This can be accomplished with a dedicated pediatric room or area where there are bright colors, toys, and games or other types of distractions. A child life specialist based in the ED has the ability to decrease anxiety and pain perception using developmentally appropriate education and preparation to patients and families [48]. Allowing family presence during painful procedures also may be of benefit. Although there is no evidence that family presence decreases pain, their presence for procedures can decrease child distress [49]. Skin-to-skin contact of an infant with his or her mother and breastfeeding during a procedure decrease pain behaviors associated with painful stimuli [50, 51].
Conclusions
Control of pain in children is an important concept for emergency providers not only to be familiar with, but also to advocate for. Benefits for the patient are immediate and long term. While barriers have been identified, so have strategies for overcoming these barriers. Training providers in the use of pediatric-specific pain assessment tools so that they are able to assess and measure pain objectively is the first step. Creation of guidelines or protocols allows EMS providers and triage nurses to institute pain management treatments earlier in the course of evaluation. Needle-free drug delivery systems have created the opportunity for faster and less traumatic administration of medications. The use of vapocoolants allows for rapid, needleless topical anesthesia without tissue distortion. Non-pharmacologic interventions are also effective and may be practiced in any setting.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Fein JA, Zempsky WT, Cravero JP, The Committee on Pediatric Emergency Medicine and Section on Anesthesiology and Pain Medicine, American Academy of Pediatrics. Relief of pain and anxiety in pediatric patients in emergency medical systems. Pediatrics. 2012;130:e1391–405.
Zempsky WT, Cravero JP, The Committee on Pediatric Emergency Medicine and Section on Anesthesiology and Pain Medicine. Relief of pain and anxiety in pediatric patients in emergency medical systems. Pediatrics. 2004;114:1348–56.
• Gausche-Hill M, Brown KM, Oliver ZJ, et al. An evidence-based guideline for prehospital analgesia in trauma. Prehosp Emerg Care. 2014;18(Suppl 1):25–34. Using GRADE methodology, an evidence-based guideline for prehospital analgesia was developed. Four strong recommendations were issued regarding patient assessment and narcotic medication dosing.
Model EMS clinical guidelines. https://www.nasemso.org/Projects/ModelEMSClinicalGuidelines/documents/National-Model-EMS-Clinical-Guidelines-23Oct2014.pdf. Accessed on 20 Jan 2016.
McLean SA, Maio RF, Domeier RM. The epidemiology of pain in the prehospital setting. Prehosp Emerg Care. 2002;6:402–5.
Maio RF, Garrison HG, Spaite DW, et al. Emergency medical services outcomes project I (EMSOP I): prioritizing conditions for outcomes research. Ann Emerg Med. 1999;33:423–32.
Hennes H, Kim MK, Pirrallo RG. Prehospital pain management: a comparison of providers’ perceptions and practices. Prehosp Emerg Care. 2005;9:32–9.
Rahman A, Curtis SB, DeBruyne SS, et al. Emergency medical services provider comfort with prehospital analgesia administration to children. Prehosp Disaster Med. 2015;30:66–71.
Carlson JN, Gannon E, Mann CN, et al. Pediatric out-of-hospital critical procedures in the United States. Pediatr Crit Care Med. 2015;16:e260–7.
Nicol MF, Ashton-Cleary D. “Why haven’t you taken any pain killers?” A patient focused study of the walking wounded in an urban emergency department. Emerg Med J. 2003;20:228–9.
Spedding RL, Harley D, Dunn FJ, McKinney LA. Who gives pain relief to children? J Accid Emerg Med. 1999;16:261–4.
Tomlinson D, von Baeyer CL, Stinson JL, Sung L. A systematic review of faces scales for the self-report of pain intensity in children. Pediatrics. 2010;126:e1168–98.
von Baeyer CL. Children’s self-reports of pain intensity: scale selection, limitations, and interpretation. Pain Res Manag. 2006;11:157–62.
Singer AJ, Gulla J, Thode HC Jr. Parents and practitioners are poor judges of young children’s pain severity. Acad Emerg Med. 2002;9:609–12.
Maciocia PM, Strachan EM, Akram ER, et al. Pain assessment in the pediatric emergency department: whose view counts? Eur J Emerg Med. 2003;10:264–7.
Tsze DS, von Baeyer CL, Bulloch B, Dayan PS. Validation of self-report pain scales in children. Pediatrics. 2013;132:e971–9.
•• Garra G, Singer AJ, Taira BR, et al. Validation of the Wong-Baker FACES Pain Rating scale in pediatric emergency department patients. Acad Emerg Med. 2010;17:50–4. A prospective observational study of children ages 8–17 years demonstrated excellent correlation between the Wong-Baker FACES Pain Rating Scale and the visual analog scale for patients presenting with painful conditions.
•• Bulloch B, Tenenbein M. Validation of 2 pain scales for use in the pediatric emergency department. Pediatrics 2002;110:e33. http://www.pediatrics.org/cgi/content/full/110/3/e33. A prospective study of children ages 5–16 years presenting to an emergency department demonstrated validity of the Color Analog Scale and the Faces Pain Scale.
Massaro M, Ronfani L, Ferrera G, et al. A comparison of three scales for measuring pain in children with cognitive impairment. Acta Paediatr. 2014;103:e495–500.
McLean SA, Domeier RM, DeVore HK, et al. The feasibility of pain assessment in the prehospital setting. Prehosp Emerg Care. 2004;8:155–61.
Dvorkin R, Bair J, Patel H, et al. Is fever treated more promptly than pain in the pediatric emergency department? J Emerg Med. 2014;46:327–34.
Drendel AL, Brousseau DC, Gorelick MH. Pain assessment for pediatric patients in the emergency department. Pediatrics. 2006;117:1511–8.
Kaplan CP, Sison C, Platt SL. Does a pain scale improve pain assessment in the pediatric emergency department? Pediatr Emerg Care. 2008;24:605–8.
Boyd RJ, Stuart P. The efficacy of structured assessment and analgesia provision in the paediatric emergency department. Emerg Med J. 2005;22:30–2.
Bailey B, Bergeron S, Gravel J, Daoust R. Comparison of four pain scales in children with acute abdominal pain in a pediatric emergency department. Ann Emerg Med. 2007;50:379–83.
Maimon MS, Marques L, Goldman RD. Parental administration of analgesic medication in children after a limb injury. Pediatr Emerg Care. 2007;23:223–6.
Swor R, McEachin CM, Seguin D, Grall KH. Prehospital pain management in children suffering traumatic injury. Prehosp Emerg Care. 2005;9:40–3.
• Abbuhl FB, Reed DB. Time to analgesia for patients with painful extremity injuries transported to the emergency department by ambulance. Prehosp Emerg Care. 2003;7:445–7. A retrospective chart review demonstrated that patients transported by EMS and seen in an emergency department for extremity injuries received analgesics on average 90 min later if the medication was not administered by EMS during prehospital treatment.
Johnson TJ, Schultz BR, Guyette FX. Characterizing analgesic use during air medical transport of injured children. Prehosp Emerg Care. 2014;18:531–8.
Rutkowska A, Skotnicka-Klonowicz G. Prehospital pain management in children with traumatic injuries. Pediatr Emerg Care. 2015;31:317–20.
Samuel N, Steiner IP, Shavit I. Prehospital pain management of injured children: a systematic review of current evidence. Am J Emerg Med. 2015;33:451–4.
Friday JH, Kanegaye JT, McCaslin I, et al. Ibuprofen provides analgesia equivalent to acetaminophen-codeine in the treatment of acute pain in children with extremity injuries: a randomized clinical trial. Acad Emerg Med. 2009;16:711–6.
Clark E, Plint AC, Correll R, et al. A randomized controlled trial of acetaminophen, ibuprofen, and codeine for acute pain relief in children with musculoskeletal trauma. Pediatrics. 2007;119:460–7.
Borland M, Jacobs I, King B, O’Brien D. A randomized controlled trial comparing intranasal fentanyl to intravenous morphine for managing acute pain in children in the emergency department. Ann Emerg Med. 2007;49:335–40.
•• Holdgate A, Cao A, Lo KM. The implementation of intranasal fentanyl for children in a mixed adult and pediatric emergency department reduces time to analgesia administration. Acad Emerg Med. 2010;17:214–7. A retrospective review of time to analgesic administration after introduction of a protocol allowing for administration of intranasal fentanyl or intravenous morphine to children presenting with acute pain demonstrated a 30 min reduction in time to analgesic for patients receiving intranasal fentanyl.
Stevens B, Yamada J, Ohlsson A. Sucrose for analgesia in newborn infants undergoing painful procedures. Cochrane Database Syst Rev. 2010. doi:10.1002/14651858.CD001069.pub3.
Kleiber C, Sorenson M, Whiteside K. Topical anesthetics for intravenous insertion in children: a randomized equivalency study. Pediatrics. 2002;110:758–61.
Eichenfield LF, Funk A, Fallon-Friedlander S, Cunningham BB. A clinical study to evaluate the efficacy of ELA-Max (4 % liposomal lidocaine) as compared with eutectic mixture of local anesthetics cream for pain reduction of venipuncture in children. Pediatrics. 2002;109:1093–9.
Schilling CG, Bank DE, Borchert BA, et al. Tetracaine, epinephrine (adrenalin), and cocaine (TAC) versus lidocaine, epinephrine, and tetracaine (LET) for anesthesia of lacerations in children. Ann Emerg Med. 1995;25:203–8.
Farion KJ, Splinter KL, Newhook K, et al. The effect of vapocoolant spray on pain due to intravenous cannulation in children: a randomized controlled trial. CMAJ. 2008;179:31–6.
Pinheiro JM, Furdon S, Ochoa LF. Role of local anesthesia during lumbar puncture in neonates. Pediatrics. 1993;91:379–82.
Kaur G, Gupta P, Kumar A. A randomized trial of eutectic mixture of local anesthetics during lumbar puncture in newborns. Arch Pediatr Adolesc Med. 2003;157:1065–70.
Bartfield JM, Gennis P, Barbera J, et al. Buffered versus plain lidocaine as a local anesthetic for simple laceration repair. Ann Emerg Med. 1990;19:1387–9.
Davidson JA, Boom SJ. Warming lignocaine to reduce pain associated with injection. BMJ. 1992;305:617–8.
Krause RS, Moscati R, Filice M. The effect of injection speed on the pain of lidocaine infiltration. Acad Emerg Med. 1997;4:1032–5.
Scarfone RJ, Jasani M, Gracely EJ. Pain of local anesthetics: rate of administration and buffering. Ann Emerg Med. 1998;31:36–40.
• Sinha M, Christopher NC, Fenn R, Reeves L. Evaluation of nonpharmacologic methods of pain and anxiety management for laceration repair in the pediatric emergency department. Pediatrics. 2006;117:1162–8. A randomized trial of distraction techniques in addition to usual topical anestheic for children undergoing laceration repair in the emergency department demonstrated a reduction in situational anxiety.
Krebel MS, Clayton C, Graham C. Child life programs in the pediatric emergency department. Pediatr Emerg Care. 1996;1:13–5.
Boudreaux ED, Francis JL, Loyacano T. Family presence during invasive procedures and resuscitations in the emergency department: a critical review and suggestions for future research. Ann Emerg Med. 2002;40:193–205.
Gray L, Watt L, Blass EM. Skin-to-skin contact is analgesic in healthy newborns. Pediatrics. 2000;105:e14.
Gray L, Miller LW, Philipp BL, Blass EM. Breastfeeding is analgesic in healthy newborns. Pediatrics. 2002;109(4):590–3.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Drs Gross, Gaglani, VanderWyst, and Conrad have nothing to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the author.
Additional information
This article is part of the Topical Collection on Pain Management in Pediatrics.
Rights and permissions
About this article
Cite this article
Gross, T., Gaglani, A., VanderWyst, C. et al. Acute Traumatic Pain in the Prehospital and Emergency Department Setting. Curr Emerg Hosp Med Rep 4, 81–87 (2016). https://doi.org/10.1007/s40138-016-0093-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40138-016-0093-2