Abstract
Purpose of Review
The purpose of this paper is to review recent advances in vitreoretinal surgery with a particular focus on new techniques of intraoperative visualization and new instrumentation for tissue manipulation.
Recent Findings
Advances in vitreoretinal surgical visualization include 3-D viewing systems, intraoperative OCT, and ocular endoscopy. Advances in tissue manipulation include hypersonic vitrectomy, and vitrectomy probes with improved cut rates, dual bore infusion, and shorter shafts for pediatric cases.
Summary
There are many ongoing advancements in intraoperative visualization and tissue manipulation for vitreoretinal surgeries. As these techniques continue to be developed and tested, patients will ultimately benefit from the improved intraoperative visualization, decision-making, and surgical outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Vitreoretinal microsurgery allows for the recovery of vision that would otherwise be lost to disrupted anatomy of the eye caused by degenerative changes of the vitreoretinal interface, vaso-proliferative disease, trauma, infections, and surgical complications. Reapproximating normal anatomy in these situations requires atraumatic dissection of tissue as thin as 3 microns from the 100 micron thick neurosensory retina. The special anatomy of the eye demands execution of these maneuvers viewed through a complex optical pathway involving pupillary apertures and optical aberrations. Vitreoretinal surgery can be broken down into four fundamental tasks: Visualization, dissection of tissue, reapproximation of tissue/implants, and closure of retinal breaks. The goals of a particular surgery dictate the relative importance of each task, but it is good practice to consider each task independently for even the most straightforward cases. Advances in these areas have improved outcomes, expanded indications, and reduced complications. The goal of this review is to review recent advances in retinal instrumentation in terms of how they help the surgeon with the first two of these tasks.
3-D Viewing Systems
A three dimensional digital viewing system is now available commercially as an alternative to the traditional optical viewing through the operating microscope. It is implemented as a high-resolution digital camera body that replaces the oculars, but otherwise relies on the optics of the microscope for both coaxial viewing and posterior segment viewing with contact and non-contact lens systems. The camera provides near real-time imaging with stereopsis, viewed on a large LCD monitor. Specialized glasses are required to realize the stereopsis. It has been suggested that the system may provide improved coordination of care and surgical efficiency by providing the entire surgical team with access to a high-quality view of the surgery [1]. Outcomes using this viewing system have been shown to be equivalent in a retrospective review of surgery for range of vitreoretinal diseases [2•, 3].
One might reasonably ask why additional technology is being introduced between surgeons and their surgical field. As fast as the camera is, it cannot compete with direct passage of light from the patient’s tissue, through the optics, to the surgeon’s retina. The system’s lag (90 ms) is felt to be surgically insignificant [4], but disruptions of the function of the system could introduce viewing lag that could compromise safety. Even the best digital cameras have a defined dynamic range of light detection. Vitreoretinal surgeons rely on precise manipulation of endolights to safely and accurately identify planes of dissection. These manipulations occur across a wide range of focal points and optical aberrations. Visualization in an efficient, safe manner takes advantage of a wide dynamic range of illumination, limited only by the surgeon’s own retina. A digital imaging system inherently limits this dynamic range. Practically, this is experienced as “white-out” and “black-out,” in which details of the tissue and instruments are lost during transitions to different light levels. Effective solutions have been proposed, typically involving adapting the use of the light pipe in such a way to stay within the dynamic range of the camera. Other potential downsides to the 3-D digital viewing system include the potential for decreased reliability and the cost. Several potential advantages of the 3-D digital viewing system have been put forth as justification for the concerns described above.
The ergonomics of a properly implemented 3-D viewing system may be superior to the classic operating microscope. The monitor can be positioned in a neutral position directly in front of the surgeon. This position may relieve the surgeon from some prolonged flection of the cervical spine. This is not a trivial concern. Microsurgery, and in particular vitreoretinal microsurgery, is now understood to be associated with an increased risk of musculoskeletal disease that can become disabling [5]. Proper posture and positioning at the operating scope may mitigate some of the risk, but vitreoretinal surgery still demands prolonged precise posture. Looking at a monitor allows the surgeon’s spine more freedom of movement during a case, potentially reducing musculoskeletal stress [6•].
Iatrogenic macular phototoxicity is a rare but serious risk of common vitreoretinal surgeries such as macular hole repair and epiretinal membrane peeling. Digital imaging allows for amplification and manipulation of light. If image quality can be maintained with less intense endoillumination, then the risk of macular phototoxicity is reduced [7].
Another rare cause of macular injury is toxicity from ophthalmic dyes. These dyes are typically employed to better visualize the internal limiting membrane (ILM) and assist in atraumatic removal of the membrane from the surface of the macula. The magnitude and nature of this risk is poorly understood, but is probably related to the particular dye, the effective concentration on the macular surface, the duration of the exposure to the dye, and the completeness of lavage. The 3-D digital visualization allows for manipulation of hues and contrast to improve the view of unstained ILM [8, 9]. This can allow comfortable, safe and efficient removal of ILM without dye, but it should be noted that some surgeons routinely forgo dye with traditional viewing systems with no difference in postoperative visual acuity and anatomic closure of macular hole [10]. A limited comparison of surgical outcomes between the two systems found no differences for a range of surgeries [2].
Other proposed advantages have to do with system-based aspects of medical care. The monitor allows for a high-quality view by all members of the OR team (provided they are wearing the special glasses.) Surgical assistants and the anesthesiologist may better coordinate care if they can better understand in real-time the progress of the surgery. The improved viewing with stereopsis may also improve the training of vitreoretinal surgeons [1]. With a traditional optical microscope, only one trainee shares a real-time stereo-view of the surgery. With the monitor, trainees at all levels can observe in real-time. This advantage seems most important for highly specialized, relatively rare surgeries such as pediatric retina surgery.
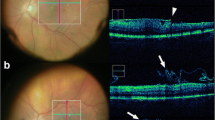
Intraoperative Optical Coherence Tomography
Intraoperative imaging of the retina by optical coherence tomography (OCT) is another advancement in the way vitreoretinal surgeons view the tissue during surgery. OCT imaging allows for micron level resolution of the vitreoretinal architecture presented as cross-sectional images. It plays a core role in the diagnosis and management of retinal vascular disease in the clinic and guides preoperative assessment of many surgical diseases. More than a decade ago, surgeons began studying the ability of OCT to guide intraoperative care. Several commercial systems are now available.
The role of intraoperative OCT has been studied retrospectively since 2009 and now with a prospective 3-year trial [11, 12]. The DISCOVER trial nicely demonstrates subclinical features of vitreoretinal disease and the impact of various surgical manipulation [13, 14]. For example, anatomic success rate for macular hole closure has been associated with intraoperative alteration in the configuration of the macular hole [11, 15]. Overall outcomes have been shown to be equivalent to conventional surgery [16•]. There is some limited evidence that intraoperative OCT imaging can guide the perioperative decision-making, such as confirming the presence of a macular hole discovered immediately following vitreous hemorrhage removal which changed the operative plan for membrane peeling and gas tamponade, or confirming placement of a repositioned IOL despite significant corneal edema [17].
Ocular Endoscopy
Potential roles for ocular endoscopy are greatly expanded with the introduction of a 23 gauge probe, which works with transconjunctival sutureless small gauge systems that are now widespread. It provides views that would otherwise be unobtainable due to media opacity. Diagnostic endoscopy can be employed at the beginning of a case to determine the visual potential of an eye in situations such as trauma, chronic retinal detachment, and infections. Therapeutic endoscopy potentially can allow a staged approach to combined corneal transplant and vitrectomy, improving long-term graft survival rates. It can help with positioning of sutured IOLs. It can allow for safer core vitrectomy in acute endophthalmitis.
Surgical endoscopy provides improved less-invasive access to surgical space at the cost of the loss of stereopsis. Ocular endoscopy provides an additional advantage: an improved view of the vitreous with coaxial illumination. This is particularly beneficial for appreciating the structure of the pediatric vitreous. The technique has been used successfully in complex retinopathy of prematurity cases that require dissection of the retrolental vitreous without compromising the crystalline lens [18]. 3-D endoscopy has also been reported and used to perform vitrectomy [19]. A summary of advances in visualization can be found in Table 1.
Dissection of Tissue
The fundamental challenge of vitrectomy is the need to efficiently and thoroughly remove vitreous without exerting excessive traction. Excess vitreoretinal traction causes most of the serious surgical complications. The earliest vitrectomy probes required large scleral incision. Infusions systems were crude. Cut rates were slow. As smaller gauge instruments, automated infusions, and higher cut rates were developed, complications rates dropped and surgical efficiency improved [20]. The flow rates during vitrectomy have been shown to be dependent on cut rate, and this can affect total operative time [21]. Increases in cute rate as high at 16,000 cuts per minute can decrease core vitrectomy time by up to 50% in vivo [22].
In addition to increasing cut rate, double-bladed probes can also increase the flow rate [23], and high flow infusion can improve flow rates in addition to decreasing pressure fluctuation in an ex vivo model [24]. Outside of changes in cut rate, the development a dual bore cannula with a laterally placed port has been proposed to allow for equilibrium of IOP during injection of dyes and liquids without causing axial fluid jet damage [25].
A hypersonic cutter disrupts the vitreous with high frequency sound waves in contrast to the typical mechanical cutting of vitreous with a high-speed guillotine [26]. In a series of 20 patients, core vitrectomy was successful, and in a prospective study with 50 patients, the anatomic success rate was 98%. It should be noted that 15 cases had technical issues that resulted in conversion to guillotine vitrectomy. Shortened probe shafts have been introduced for pediatric patients given the shorter eyes and relatively large and posterior crystalline lens [27]. Novel techniques of functionally shortening full size instruments for pediatric use have also been described [28]. Short shafts have also been used in adults for vitreous biopsy [29].
Conclusion
The field of vitreoretinal surgery is evolving as new technologies are applied to meet the challenges of viewing and manipulating delicate tissue in confined space. Surgeons in 2022 can use a variety of tools beyond traditional optical microcopy to view and manipulate the retina and vitreous. The advantages today of such technologies in isolation are incremental and highly dependent on the practice environment, but future applications are exciting. Robot-assisted surgery continues to develop in many areas of medicine, including vitreoretinal surgery. Robots have safely performed the most delicate isolated maneuvers, including epiretinal membrane peel and retinal vein cannulation [30, 31]. In the not-too-distant future, one can imagine integration of digital visualization to such systems. Once this is achieved, machine-learning and artificial intelligence can be applied to optimize the sequence of maneuvers and perhaps even limit certain maneuvers to reduce surgical trauma. At this point, in essence, the machines will be participating in surgical decision-making.
References
Recent papers of particular interest have been highlighted as: • Of importance
Chhaya N, Helmy O, Piri N, Palacio A, Schaal S. Comparison of 2D and 3D video displays for teaching vitreoretinal surgery. Retina Phila Pa. 2018;38(8):1556–61.
• KANTOR P, Matonti F, Varenne F, Sentis V, Pagot-Mathis V, Fournié P, et al. 2021 Use of the heads-up NGENUITY 3D Visualization System for vitreoretinal surgery: a retrospective evaluation of outcomes in a French tertiary center. Sci Rep. 11(1):10031. This paper establishes the feasibility of a 3-D viewing system for vitreoretinal surgery and its use in a range of vitreoretinal diseases.
Agranat JS, Miller JB, Douglas VP, Douglas KAA, Marmalidou A, Cunningham MA, et al. The scope of three-dimensional digital visualization systems in vitreoretinal surgery. Clin Ophthalmol Auckl NZ. 2019;13:2093–6.
Romano MR, Cennamo G, Comune C, Cennamo M, Ferrara M, Rombetto L, et al. Evaluation of 3D heads-up vitrectomy: outcomes of psychometric skills testing and surgeon satisfaction. Eye. 2018;32(6):1093–8.
Schechet SA, DeVience E, DeVience S, Shukla S, Kaleem M. Survey of musculoskeletal disorders among US ophthalmologists. Digit J Ophthalmol DJO. 2020;26(4):36–45.
• Park SJ, Hwang JM, Jin Park EJ, Shin JP, Park DH. 2022 Comparison of Surgeon Muscular Properties between Standard Operating Microscope and Digitally Assisted Vitreoretinal Surgery Systems. Retina Phila Pa. The study compares objective measurements of muscle fatigue in a standard operating scope compared to a 3-D viewing system, providing quantitative evidence of ergonomic benefit for the 3-D viewing system.
Eckardt C, Paulo EB. Heads-up surgery for vitreoretinal procedures: an experimental and clinical study. Retina Phila Pa. 2016;36(1):137–47.
Akiyama K, Watanabe K, Fukui M, Higuchi H, Noda T. Quantitative evaluation of digital-image enhancement during heads-up surgery. Sci Rep. 2019;9(1):15931.
Melo AGR, Conti TF, Hom GL, Greenlee TE, Cella WP, Talcott KE, et al. Optimizing visualization of membranes in macular surgery with heads-up display. Ophthalmic Surg Lasers Imaging Retina. 2020;51(10):584–7.
Mackenzie SE, Gandorfer A, Rohleder M, Schumann R, Schlottmann PG, Bunce C, et al. Ultrastructure and retinal imaging of internal limiting membrane: a clinicopathologic correlation of trypan blue stain in macular hole surgery. Retina Phila Pa. 2010;30(4):655–61.
Ehlers JP, Uchida A, Srivastava SK. The integrative surgical theater: combining intraoperative optical coherence tomography and 3D digital visualization for vitreoretinal surgery in the discover study. Retina Phila Pa. 2018;38(Suppl 1):S88-96.
Dayani PN, Maldonado R, Farsiu S, Toth CA. Intraoperative use of handheld spectral domain optical coherence tomography imaging in macular surgery. Retina Phila Pa. 2009;29(10):1457–68.
Kumar JB, Ehlers JP, Sharma S, Srivastava SK. Intraoperative oct for uveitis-related vitreoretinal surgery in the discover study. Ophthalmol Retina. 2018;2(10):1041–9.
Abraham JR, Srivastava SK, Le TK, Sharma S, Rachitskaya A, Reese JL, et al. Intraoperative oct-assisted retinal detachment repair in the discover study: impact and outcomes. Ophthalmol Retina. 2020;4(4):378–83.
Huang HJ, Sevgi DD, Srivastava SK, Reese J, Ehlers JP. Vitreomacular traction surgery from the discover study: intraoperative oct utility, ellipsoid zone dynamics, and outcomes. Ophthalmic Surg Lasers Imaging Retina. 2021;52(10):544–50.
• Tuifua TS, Sood AB, Abraham JR, Srivastava SK, Kaiser PK, Sharma S, et al. 2021 Epiretinal membrane surgery using intraoperative OCT-guided membrane removal in the discover study versus conventional membrane removal. Ophthalmol Retina. 5(12):1254–62. This manuscript shows comparable results from conventional ILM peeling compared to the intraoperative OCT-guided ERM removal, and is important to establish evidence for the use of intraoperative OCT.
Runkle A, Srivastava SK, Ehlers JP. Microscope-integrated OCT feasibility and utility with the enfocus system in the discover study. Ophthalmic Surg Lasers Imaging Retina. 2017;48(3):216–22.
Wong SC, Lee TC, Heier JS, Ho AC. Endoscopic vitrectomy. Curr Opin Ophthalmol. 2014;25(3):195–206.
Kita M, Kusaka M, Yamada H, Hama S. Three-dimensional ocular endoscope system for vitrectomy. Clin Ophthalmol Auckl NZ. 2019;27(13):1641–3.
Machemer R. The importance of fluid absorption, traction, intraocular currents, and chorioretinal scars in the therapy of rhegmatogenous retinal detachments XLI Edward Jackson memorial lecture. Am J Ophthalmol. 1984;98(6):681–93.
Abulon DJK, Buboltz DC. Performance comparison of high-speed dual-pneumatic vitrectomy cutters during simulated vitrectomy with balanced salt solution. Transl Vis Sci Technol. 2015;4(1):6.
Pavlidis M. Two-dimensional cutting (TDC) vitrectome: flow assessment and prospective clinical study evaluating core vitrectomy efficiency versus standard vitrectome. J Ophthalmol. 2016;2016: e3849316.
Oravecz R, Uthoff D, Schrage N, Dutescu RM. Comparison of modern high-speed vitrectomy systems and the advantages of using dual-bladed probes. Int J Retina Vitr. 2021;7(1):8.
Nepita I, Stocchino A, Dodero A, Castellano M, Ferrara M, Romano MR, et al. Dynamic pressure measurements during vitrectomy in a model of the eye. Transl Vis Sci Technol. 2022;11(5):21.
Toygar O, Berrocal MH, Charles M, Riemann CD. Next-generation dual-bore cannula for injection of vital dyes and heavy liquids during pars plana vitrectomy. Retina Phila Pa. 2016;36(3):582–7.
Blinder KJ, Awh CC, Tewari A, Garg SJ, Srivastava SK, Kolesnitchenko V. Introduction to hypersonic vitrectomy. Curr Opin Ophthalmol. 2019;30(3):133–7.
http://fyra.io. New Instrumentation for Pediatric Retina Cases [Internet]. Retina Today. Bryn Mawr Communications; [cited 2022 Jun 20]. Available from: https://retinatoday.com/articles/2014-mar/new-instrumentation-for-pediatric-retina-cases
Babu N, Shah PK, Narendran V, Kalpana N, Kim R. An easy method to raise the 25-gauge trocar and cannula system for retinopathy of prematurity-related lens-sparing vitrectomy. Retina Phila Pa. 2014;34(5):1014–5.
Oshima Y, Wakabayashi T, Ohguro N, Nishida K. A 27-gauge sharp-tip short-shaft pneumatic vitreous cutter for transconjunctival sutureless vitreous biopsy. Retina. 2011;31(2):419–21.
Roizenblatt M, Edwards TL, Gehlbach PL. Robot-assisted vitreoretinal surgery: current perspectives. Robot Surg Auckl. 2018;5:1–11.
Willekens K, Gijbels A, Smits J, Schoevaerdts L, Blanckaert J, Feyen JHM, et al. Phase I trial on robot assisted retinal vein cannulation with ocriplasmin infusion for central retinal vein occlusion. Acta Ophthalmol (Copenh). 2021;99(1):90–6.
Funding
No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors do not have existing conflict of interest. This literature review did not involve human or animal participants and no ethical approval was required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical collection on Ophthalmologic Surgery.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mohammed, T., Barañano, D. A Review of Recent Advances in Vitreoretinal Surgical Visualization and Tissue Manipulation. Curr Surg Rep 10, 181–185 (2022). https://doi.org/10.1007/s40137-022-00327-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40137-022-00327-8