Abstract
Purpose of Review
Our review aims to describe the use of simulation-based training throughout the continuum of surgical education.
Recent Findings
In addition to well-known procedural-based surgical simulation modalities like the Fundamentals of Laparoscopic Surgery and Fundamentals of Endoscopic Surgery, there are several novel uses of simulation including its use for preparing medical students for surgical residency, resident interviews and onboarding, residency training, mental skills training, and continuing education for practicing surgeons.
Summary
Simulation is a cost effective and useful method to improve trainee exposure and confidence to execute technical and nontechnical skills throughout the surgical career. There is clearly a role for simulation-based training with medical students, residents, and practicing surgeons to optimize performance through deliberate practice of skills in a safe environment. Due to the evolution of surgical techniques and an increased emphasis for proficiency-based training and certification of skills, simulation will play an increasingly integral role in surgical education.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The environment of surgical education has changed dramatically over the past few decades as duty hour limitations and changes in surgical practice patterns have led to significantly diminished autonomy, and thus, reduced experience in the operating room [1, 2]. As a result of this, modern residents have fewer opportunities to hone their surgical skills, resulting in residents feeling unprepared for independent practice upon graduation [3]. One proposed method for addressing these limitations in resident exposure and training is through the use of simulation. Simulation has been shown to be successful in improving practice and creating measurable technical and nontechnical performance standards for surgical trainees [4, 5], and is increasingly being used throughout the career of the physician to prevent arrested skill development, as well as perfect new techniques and improve teaching abilities and other important competencies.
Surgical simulation training, which includes benchtop trainers, animal models, fully-simulated operating rooms, and virtual reality simulators, has been identified as an effective method of enhancing surgeons’ surgical skills, as it affords learners an opportunity to learn and refine nontechnical and technical skills by practicing advanced patient care scenarios prior to confronting comparable situations in the clinical environment [6,7,8]. Expertise in any domain cannot be distilled as the product of innate ability or experience alone, rather, is the result of deliberate efforts to practice skills and improve [9]. For surgeons, expert performance is defined, in part, as being highly sensitive to and anticipatory of technical and cognitive errors, flexible to correct any identified errors, having the ability to recognize patterns (e.g., anatomical, diagnostic, etc.) quickly with limited information, and having highly developed fine motor skills, among other factors [10]. These hallmarks of surgical expertise are developed through the same process of extensive experience, deliberate practice, and study. Through the deliberate practice afforded through simulation, learners can hone their technical and nontechnical surgical skills without endangering patients. Furthermore, surgical simulation also can provide exposure to rare but critical clinical conditions, and allows faculty to assess learners’ surgical skill competency prior to performing these skills on patients [11]. Thus, simulation is clearly a modality that should be widely adopted and implemented throughout all levels of surgical education. The goal of this review is to provide an overview of how simulation training has been implemented throughout the continuum of surgical education from preparing medical students for surgical training to maintenance of proficiency as a practicing surgeon.
Selection and Onboarding into Residency
Simulation to Prepare Medical Students for Surgical Training
Particularly for medical students, high-fidelity simulation is a teaching modality that can allow students to engage in the practice of medicine without endangering patients, which can help them learn how to manage and care for ill patients before they encounter these situations as residents [6]. Accordingly, the American College of Surgeons (ACS) and the Association for Surgical Education (ASE) acknowledged the importance of developing a simulation-based surgical skills modular curriculum for medical students (i.e., 1–3 years) to enable them to develop basic surgical examination and procedural skills [12∙]. Using feedback from Clerkship Directors and fourth-year medical students, the ACS/ASE task force developed a free and publicly available 25 model curriculum spreading over 3 years focusing on skills training in communication, basic examinations, and more advanced skills such as chest tube placement and laparoscopy [13∙, 14].
Selection into Surgical Residency
There has also been an increasing amount of attention on using simulation as a potential screening tool for medical students planning on entering surgical training [15, 16∙]. Not only can simulation offer a unique opportunity for residency program decision makers to gain insight into applicant competencies and skills by placing them in scenarios or task environments that mimic those in residency, but participating in these simulations may also provide applicants with a realistic preview of what is expected of the specialty and/or program. Work conducted by national organizations [17∙] has shown that Program Directors see value in the use of simulation for selection as it allows an opportunity to assess critical nontechnical competencies, such as receptivity to feedback, communication, leadership, and decision making. In this study, students similarly expressed value in simulation as a screening methodology, indicating that it could provide them with insight into a program’s values and attitudes towards teaching, but also provides them with an opportunity to demonstrate their skills. With agreement on its value from stakeholders on both sides of the screening process, simulation is likely to play an increasing role in selection decisions in years to come.
Intern Boot Camps
For those who do enter surgical training, simulation may also be able to reduce the learning curve from medical school to surgical residency. Okusanya et al. developed a pre-surgical internship “boot camp” that featured simulation-based technical skills training that emphasized the significance of patient safety and the consideration of treatment benefits, risks, and care alternatives, as well as team-based clinical scenario simulations increasing in difficulty over the course of 5 days [18]. Upon completion, medical students were significantly more confident in their medical management and technical skills, particularly for high-risk, rarely performed cases. Similarly, residents who participated in the course displayed sustained confidence in their technical skills over time. The Fundamentals of Surgery curriculum is a similar pre-internship simulation-based training program developed through a collaborative effort by the ACS, ASE, and Association of Program Directors in Surgery (APDS) [19∙∙]. This robust, simulation-based curriculum focuses on teaching students about surgical patient care, technical skills (e.g., basic laparoscopy, bedside procedures, open surgery, etc.), interpersonal skills and communication, professionalism, and system-based practice (e.g., utilizing the medical record) [20]. In a 2013 study, Krajewski and colleagues implemented a 2-month simulation-based boot camp with general surgery interns that combined the Fundamentals of Surgery curriculum with simulation focused on teaching and assessing interns’ preoperative evaluation, postoperative management of clinical issues, procedural skills, and management of simulated patients on high-fidelity simulators [21]. Compared to historical controls who had not undergone a simulation-based skills boot camp, interns who had participated in the boot camp were rated higher at several elements of patient care by nursing staff and faculty and had significantly higher American Board of Surgery In-Training Examination (ABSITE) scores.
Boot camps may not only bridge the learning gap between medical school and residency, but may also be useful in identifying the areas for skill remediation. Fernandez et al. developed an intensive intern preparatory course and implemented it with 30 general surgery interns over a 4-year period [22]. Utilizing procedural skills lab sessions, simulated patient encounters, or a combination of the two modalities, this course taught and tested interns’ surgical skills in eight areas such as instrument identification and use, suturing and knot tying, laparoscopic skills, and cardiopulmonary resuscitation skills. Poor boot camp performance scores were correlated with clinical performance evaluations, suggesting that intern boot camps can be utilized to identify areas for skill remediation and further simulated practice prior to allowing interns to perform these skills in the clinical arena.
Simulation in Training and Assessing Residents
Simulation for Surgical Skill Mastery
In regard to surgical resident education, simulation plays a significant role in skill mastery. Simulation is proving to be a safe and effective method to address some of the issues of inadequate operative exposure in current resident training; allowing residents to practice skills deliberately and safely [1, 2]. In an effort to address some of the issues with resident operative training and standardize simulation training for residents on the national level, the ACS and APDS assembled a group of surgical education experts to develop a peer-reviewed comprehensive, simulation-based training curriculum [4]. The resulting surgery resident skills curriculum consists of three phases of modular education, which focuses on teaching surgical residents basic/core surgical skills, advanced surgical skills, and team-based skills (Table 1) [5]. We will review the use of simulation in each of these phases.
General Characteristics of Simulation-Based Skills Training
Aside from the ACS/APDS national simulation curriculum, the efforts to develop simulation-based training curricula have been largely uncoordinated, with no consistent methodology to developing simulation-based training curricula, despite the fact that over the past 2 decades, simulation-based training has developed into an integral element of surgical education [23∙∙]. Although there are many different simulation curricula available, in general, simulation curricula should involve knowledge-based learning as well as deconstruction of the procedure into its various components accompanied by skills training [24,25,26]. In their systematic review of simulation-based surgical skills training curricula, Stefanidis and colleagues identified critical elements of curricular design for simulation-based training, which include proficiency-based learning (i.e., training to expert-level benchmarks), distributed training (i.e., multiple training sessions over time), training to automaticity (i.e., learning which results in reduced attentional demands during performance), and deliberate practice [23∙∙]. The effectiveness of simulation-based training should therefore be evaluated based on whether it incorporates these elements. Our review of these methods is by no means exhaustive but is meant to highlight some of the curricula that have been validated and more widely utilized.
Phases I and II: Core and Advanced Technical Skills
Suturing and Knot Tying
One of the earliest uses of simulation in surgical training was knot tying; what was once simply a board and suture has evolved to be even more effective when integrated into a curriculum. In 2007, the University of Texas Southwestern (UTSW) created a proficiency-based curriculum focused on 12 core open surgical skills including instrument handling, 1- and 2-handed knots, and basic suturing techniques [27]. They utilized inexpensive and readily available materials to create a cost effective curriculum, which has been shown to have construct validity, with residents reporting greater confidence and improved performance after completion [28]. Furthermore, an intermediate knot tying and suturing curriculum was developed that used six more advanced procedures such as tying and suturing at depth, stick tie, and atraumatic tie [29]. Successfully implemented at outside institutions, this curriculum resulted in performance levels by first-year residents equal to, and, at times, superior to, senior-level residents on these intermediate skills [30∙].
Central Line Placement
Simulation has also been commonly used to train residents how to place central lines. Studies have shown that simulation training reduces central line-associated bloodstream infections [31, 32] and results in fewer needle passes and higher reported confidence by operators [31]. These initial findings are supported by a more recent systematic review showing that residents trained in central line placement using simulation have fewer needle passes and subsequently fewer pneumothoraces, as well as better knowledge of the procedure and greater confidence in their ability to perform it [33].
Laparoscopic Skills
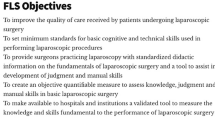
One of the benefits of simulation is the ability to educate residents safely in an environment where they can learn from their mistakes without negatively impacting patient safety. With an ever-increasing breadth of surgeries being performed laparoscopically, the use of simulation is becoming ever more important. In order to ensure a minimum standard of care for all surgeons performing laparoscopic surgery, starting in 2009, the ABS required that all residents pass the Fundamentals of Laparoscopic Surgery (FLS) exam prior to sitting for the ABS exam. FLS certification requires that residents pass both a written multiple choice exam that tests key knowledge points, as well as a proctored manual skills exam. This exam evaluates residents’ performance on five basic laparoscopic skills in a laparoscopic box trainer. These skills assessments were developed by Fried and colleagues [34] and are shown to correlate with intraoperative technical skills ratings during actual laparoscopic procedures [34,35,36].
The Society of American Gastrointestinal Endoscopic Surgery (SAGES) subsequently created a committee to develop educational materials and curricula to teach these fundamental laparoscopic skills. The FLS curriculum, launched in 2004, is a reliable program with construct and predictive validity, that results in improved performance as well as retention of learned laparoscopic skills [34,35,36,37]. Residents trained with simulation show greater improvement in operative performance compared to those who did not receive simulation training [36], and systematic reviews have shown better performance in both laparoscopic and endoscopic skills in simulation-trained residents compared to their counterparts [38∙, 39]. Furthermore, the proficiency-based curriculum for the five FLS exercises showed that residents who trained to proficiency had a 100% pass rate on the technical skills portion of the FLS exam, with skill retention at 1-year follow-up [40,41,42].
Although there remains some debate over whether basic box trainers or virtual reality trainers are superior, a 2013 Cochrane review concluded that, although there is limited evidence, VR trainers may be superior to box trainers; however, any form of simulation is superior to none [43]. The ability to pass FLS has been shown to be closely linked with operative performance, to the point that FLS is considered a benchmark for patient safety by malpractice insurers [44].
Endoscopic Skills
Colonoscopies can comprise up to 40% of the procedures performed by rural surgeons [45], and were recently identified as the most common procedure performed by general surgeons [46]. In response to the concern for inadequate exposure in endoscopic procedures, the Residency Review Committee (RRC) increased the number of upper and lower endoscopies required for resident graduation [47]. To ensure that residents receive the same training despite differences in exposure, the ABS, in conjunction with SAGES, the American Society of Colon and Rectal Surgeons (ASCRS), the American Society for Metabolic and Bariatric Surgery (ASMBS), and the Society for Surgery of the Alimentary Tract (SSAT), developed the Flexible Endoscopy Curriculum (FEC). The FEC consists of two parts: the first part involves 12 web-based didactic sessions as well as hands-on simulation practice, and second part involves completion of the Fundamentals of Endoscopic Surgery (FES) certification exam. Starting with the 2017–2018 academic year, all residents are required to pass the FES exam in order to be eligible to sit for board certification [48]. FES is the culmination of FEC, it was designed similarly to FLS and has undergone a similar validation process [49∙, 50, 51]. The FES examination involves both cognitive and skills assessment, with an 80-question web-based exam and a technical skills exam consisting of five simulation exercises on the GI mentor (Simbionix USA, Cleveland, OH, USA) endoscopy simulator. These five simulation exercises deconstruct the skills required to perform flexible endoscopy (Table 2) [50] and the ability to complete them safely has been associated with improved performance [51,52,53].
Various curricula have been created to ensure competency as measured by the FES examination. For example, Surgical Training for Endoscopic Proficiency (STEP) has been created by SAGES in partnership with Olympus America. STEP provides residency programs with a combination of didactic and hands-on training resources, in addition to assessment forms. Similar to FES, STEP deconstructs the basic skills of endoscopy and provides trainees with an opportunity to gain proficiency on these skills, which is crucial since trainees cannot have exposure to the actual scenarios until the exam [49∙, 50, 52]. More recent curricula have been developed as well, such as the mastery learning curriculum developed by Ritter et al. [54∙] using the Endoscopy Training System (ETS). Preliminary work done by this research group has demonstrated a 100% pass rate among trainees who have completed the curriculum. The skills gained through simulation for laparoscopic and endoscopic performance have been shown to be as effective as patient-based training [55] and have been found to result in skills transfer to the operating room setting [38∙].
Use of Simulation in Robotics
With increasing demand for robotic surgery, there has been a similar drive to answer the question “how do we adequately train people to perform robotic surgery?” There have been multiple proficiency-based robotic surgery curricula developed over the past few years; however, no one program has yet been endorsed for robotics as programs have been for FLS and FES. Dulan and colleagues deconstructed robotic skills and developed a curriculum that combines online sessions with nine inanimate exercises (5 tasks derived from FLS and 4 novel robotic tasks) with objective metrics; [56] this curriculum has been found to be educationally beneficial as well as reliable, valid, and feasible for proficiency training [57, 58]. Currently, SAGES is in the process of developing a Fundamentals of Robotic Surgery (FRS) curriculum, which is expected to be released in the next several months.
Simulation in Training for Open Surgery
With increasing breadth of operations available and advancements in laparoscopy and endoscopy, true open surgery is becoming increasingly rare. In 2010, one study estimated that between 1993 and 2007, there was a dramatic increase in percutaneous and endovascular procedures and an associated 30–70% decline in the number of open gastrointestinal and vascular cases [59]. Despite the detrimental effect that this lack of experience may have on patient care and resident development, there has been little focus on developing open simulation models for training outside of trauma. A 2010 systematic review of randomized controlled trials assessing simulation training, found that only 1 of 30 included studies was focused on open surgical simulation [6]. Similarly, a 2013 systematic review of open surgical simulation in residency training by Fonseca and colleagues revealed few studies focused on open simulation, the majority of which were focused on a specific, basic process and did not involve more complex open procedures [60].
The use of simulation in trauma is not new however, as the Advanced Surgical Skills for Exposure in Trauma (ASSET) curriculum has been around since 2005. This course uses human cadavers to teach senior residents how to best gain exposure in trauma. Trainees generally report high satisfaction and confidence following these courses [61, 62]. Similarly, the Advanced Trauma Operative Management (ATOM) course was designed to teach senior residents how to deal with penetrating trauma injuries using a porcine model. Again, trainees reported greater confidence following training [63, 64]. The success of trauma models for open training suggests that there may be benefit to developing high-fidelity models for complex open surgical training.
Phase 3: Team-based Skills
Team-based skills training, such as interpersonal communication and leadership skills, have received increased attention in surgical education and have been shown to be an integral element of simulation-based surgical skills training. The ACS/APDS surgery resident skills curriculum has integrated team-based skills as a distinct phase within the curriculum, focusing on teaching residents how to execute team-based skills such as handoffs, preoperative briefing/checklists, and interpersonal communication, effectively [4, 5]. Despite being more difficult to measure, these aspects of team-based skills all have a role within the ACS/APDS surgical skills curriculum and all are enhanced with simulation-based training [65,66,67]. Arriaga et al. found that surgical teams who were trained to manage trauma patients by utilizing a preoperative checklist during simulated crisis scenarios performed significantly better than they had when checklists were not available [65]. Telem et al. found that patient care order entry and communication could be improved through the use of a novel handoff training curriculum using simulation [66]. Following simulated scenarios, there was a decrease in order entry errors, and participating residents felt this training addressed important clinical deficiencies. Teamwork training through simulation has also proven to have positive effect on the performance of surgical teams. In an effort to help surgical trainees, faculty, and nurses develop effective teamwork during trauma patient management, Capella et al. implemented the team strategies and tools to enhance performance and patient safety (TeamSTEPPS) curriculum (https://www.ahrq.gov/teamstepps/index.html), supplemented with simulated trauma scenarios with surgical teams [67]. The TeamSTEPPS curriculum aims to enhance patient safety by optimizing surgical team communication during crisis scenarios. The researchers found that TeamSTEPPS was effective at enhancing participants’ leadership, communication, situation monitoring, mutual support, and improved efficiency in the trauma bay. It is clear that simulation training is a useful training tool to help surgical trainees optimize their team-based nontechnical skills. Furthermore, simulation training may be effective at helping trainees integrate nontechnical strategies to optimize their individual performance as well.
Individual Skills
Through simulation training, surgical educators have recently begun implementing individual-based nontechnical skills to supplement trainees’ simulation training and optimize their surgical performance. Mental imagery, the process of mentally rehearsing a task in the absence of explicit physical movement, can be used to cognitively practice an action before an actual performance [68]. Arora et al. developed a guided mental imagery protocol to implement with experienced and novice surgeons, and found that it was effective at enhancing participants’ knowledge and confidence to perform a laparoscopic cholecystectomy. In a follow-up randomized-controlled study, the authors implemented mental imagery with novice surgeons prior to virtual reality laparoscopic cholecystectomy simulation training and found that imagery-trained participants significantly outperformed controls (i.e., who received only simulation training) on objective measures of surgical performance [69]. The authors concluded that mental imagery may be a cost- and time-effective strategy to supplement surgical simulation training. Aside from mental imagery, though, there may be other mental skills that can be implemented during surgical simulation training to optimize trainee performance.
Recently, there have been attempts to implement a more comprehensive mental skills curriculum (MSC) with surgical novices to reduce the variability in their surgical performance and help them perform at a consistently higher level [70∙, 71∙]. Since stress has been identified as a significant barrier to surgical performance, particularly for inexperienced surgeons, this comprehensive curriculum was designed to help novices manage stress effectively [72]. This comprehensive MSC, which taught novices several mental skills including mental imagery, energy and attention management strategies, goal setting, performance routines, and refocusing strategies, was implemented during participants’ FLS training to help learners crystalize these skills as habits for surgical performance [70∙, 71∙]. Upon completion of the MSC, participants displayed significantly enhanced laparoscopic performance and increased use of mental skills. Also, despite experiencing significantly heightened physiological arousal during a transfer test of performance to the simulated clinical environment, participants reported no appreciable increase in perceived stress, indicating that they felt a sense of control over their stress during the transfer test [70∙]. In a follow-up randomized-controlled trial, this MSC was again implemented with surgical novices and the MSC-trained group displayed significantly improved mental skills use from baseline to posttest and demonstrated higher laparoscopic skill improvement than controls during a laparoscopic suturing retention test despite having similar skills at baseline [71∙]. Based on these results, it is clear that individual-based nontechnical skills, like mental imagery and other mental skills, can enhance trainees’ surgical performance when implemented during simulation training.
Ongoing Professional Development
In addition to educating medical students and surgical residents, simulation training can also offer benefits to experienced surgeons’ continuing professional development. As previously discussed, surgical simulation modalities afford learners the opportunity to engage in deliberate practice [8] which can allow experienced surgeons to continue to develop and improve as a function of continued skill and advanced cognitive process (e.g., problem solving and decision making) refinement, as well as prevent arrested skill development or skill decay [73]. Feedback is an integral method of performance optimization, even for experienced performers, and can highlight positive areas of performance that should be replicated or identify deficient mechanics of skills that require improvement.
Coaching Curricula
Augmented feedback, which consists of information provided by an external source that supplements intrinsic feedback, can serve to motivate a performer to sustain effort in practice, identify errors, and provide methods to correct undesirable performance [74]. One example of this is coaching, which consists of a collaborative relationship between mentors and learners where the mentors provide augmented feedback to the learners to empower them to achieve improved performance through self-directed learning and growth [75]. Simulation training gives surgical educators methods of coaching and enhancing the performance of surgeons of all experience levels, and offers experienced surgeons an opportunity to engage in continuing education to prevent arrested skill development.
Traditionally, surgical skills coaching curricula have been implemented with practicing surgeons in the clinical environment in a peer mentorship model [76∙]. This model, however, does not allow surgeons to engage in deliberate practice to implement the augmented feedback they receive to safely develop these deficient skills into habits for surgical performance. Implementing surgical coaching during surgical simulation training may address this issue. Stefanidis et al. developed a coaching curriculum to enhance the performance of practicing general surgeons and gynecologists, consisting of video review, peer mentoring, and simulated technical and nontechnical skills training with coaching [77∙]. The simulated technical (i.e., FLS) and nontechnical skills training (i.e., managing intraoperative disruptions) gave the coaches an effective method of assessing and providing feedback to participating surgeons on how to improve their skills. Participants rated the coaching curriculum as highly valuable. Thus, coaching through simulation may be an effective strategy to provide continuing education for practicing surgeons.
Faculty Development
Surgical training is an integral element of surgical faculty’s responsibility, yet the development of optimal methods to educate trainees has been slow in comparison to other areas of surgical education [78]. Recently, there have been attempts to “train the trainer” to standardize the instruction provided to surgical trainees during procedural-based simulation training, to ensure that trainees are consistently exposed to the most effective instructional methods possible [79∙]. Mackenzie et al. studied the effectiveness of a 2-day training course for expert colorectal laparoscopic surgeons teaching laparoscopic skills to learners through simulation training, and found that this course improved expert teaching strategies by providing a structured training framework that the trainers took back to their native institutions, which ultimately reduced the learning curve of laparoscopic skills for the learners at their institution. This work supports the concept that “how” to teach can be learned and that trainees may benefit from improved faculty training as well [80∙∙].
Multidisciplinary Training and Team-based Skills
Finally, simulation can also be extremely effective in teaching surgeons and staff how to work together. Research has shown that poor intraoperative teamwork is among the leading causes of intraoperative errors, which can result in poor patient outcomes [81]. Since surgeons are the leaders of the surgical team, it is necessary to ensure that surgeons’ teamwork and communication is at the highest possible standard to avoid communication and associated performance errors [82∙]. Scenario-based simulation training may be an effective tool to enhance practicing surgeons’ communication and teamwork skills, better preparing them to manage the demands of crisis scenarios. Steinemann et al. developed an in situ team-training curriculum that featured a 1-h pre-simulation online presentation, and a 3-h simulation session on a patient simulator with didactic education that focused on teaching participants communication skills during a simulated trauma scenario [83]. The results demonstrated that this multidisciplinary teamwork training curriculum was effective at significantly enhancing trauma team teamwork and communication, and clinical task efficiency and performance. Arriaga et al. developed a standardized operating room teamwork curriculum that focused on teaching principles related to using the World Health Organization Surgical Safety Checklist, communication, and assertiveness. They implemented it with surgical teams at four participating simulation programs [84∙]. The teams then participated in simulated intraoperative emergency scenarios. The researchers found that the majority of participants indicated that the scenarios were challenging, realistic, salient to their practice, and would help them provide more effective patient care. Teamwork and communication skills training may be feasible to execute through simulated emergency scenarios, which can be valuable to practicing surgeons.
Conclusions
Simulation, which began in surgery as an innovative method for teaching skills needed for new technologies, has become a crucial (and even required) [85] methodology for developing and polishing skills and competencies of surgeons at all stages of their career. Medical students are exposed to surgical simulation curricula as early as their second year; this exposure only increases as students require more hands-on skills for the clinical portion of their training. Simulation may be used for selection and onboarding into residency programs, and then may become a frequent methodology for training, diagnosing, and assessing a wide array of competencies during training. Once nearing the end of formal training, simulation offers a venue for required high-stakes assessments, such as FLS and FES. Surgeons in practice have multiple opportunities to hone and polish skills through simulation as well, through ongoing skill development with peer coaches, faculty development initiatives around teaching, team-training opportunities, and beyond. Thus, simulation plays a critical role throughout the life of a surgeon. In light of the ever-changing training environment, where technologies and techniques continue to expand and the focus on competency-based training and certification continues to grow, it appears that the use of simulation to increase exposure and proficiency will only continue and that simulation is likely to play an even larger role throughout a surgeon’s career.
References
Papers of particular interest, published recently, have been highlighted as: ∙ Of importance ∙∙ Of major importance
Nasca T, Day S, Amis E Jr, ACGME Duty Hour Task Force. The new recommendations on duty hours from the ACGME Task Force. N Engl J Med. 2010;3(1):1–6. doi:10.1056/NEJMsb1005800.
Williams RG, Dunnington GL. Accreditation Council for Graduate Medical Education core competencies initiative: the road to implementation in the surgical specialties. Surg Clin North Am. 2004;84(6):1621–46. doi:10.1016/j.suc.2004.06.018.
Mattar SG, Alseidi AA, Jones DB, Jeyarajah DR, Swanstrom LL, Aye RW, et al. General surgery residency inadequately prepares trainees for fellowship: results of a survey of fellowship program directors. Ann Surg. 2013;258(3):440–9. doi:10.1097/SLA.0b013e3182a191ca.
Scott DJ, Dunnington GL. The new ACS/APDS skills curriculum: moving the learning curve out of the operating room. J Gastrointest Surg. 2008;12(2):213–21. doi:10.1007/s11605-007-0357-y.
American College of Surgeons. ACS/APDS surgery resident skills curriculum. 2017. https://www.facs.org/education/program/resident-skills. Accessed 28 Apr 2017.
Sutherland LM, Middleton PF, Anthony A, Hamdorf J, Cregan P, Scott D, et al. Surgical simulation. Ann Surg. 2006;243(3):291–300. doi:10.1097/01.sla.0000200839.93965.26.
Dunkin B, Adrales GL, Apelgren K, Mellinger JD. Surgical simulation: a current review. Surg Endosc Other Interv Tech. 2007;21(3):357–66. doi:10.1007/s00464-006-9072-0.
Gordon JA. The human patient simulator: acceptance and efficacy as a teaching tool for students. Acad Med. 2000;75(5):522.
Ericsson KA, Krampe RT, Tesch-Römer C. The role of deliberate practice in the acquisition of expert performance. Psychol Rev. 1993;100(3):363–406. doi:10.1037/0033-295X.100.3.363.
Abernethy B, Poolton JM, Masters RSW, Patil NG. Implications of an expertise model for surgical skills training. ANZ J Surg. 2008;78(12):1092–5. doi:10.1111/j.1445-2197.2008.04756.x.
Sanfey H, Ketchum J, Bartlett J, Markwell S, Meier AH, Williams R, et al. Verification of proficiency in basic skills for postgraduate year 1 residents. Surgery. 2010;148(4):759–67. doi:10.1016/j.surg.2010.07.018.
∙ Glass CC, Acton RD, Blair PG, Campbell AR, Deutsch ES, Jones DB, et al. American College of Surgeons/Association for Surgical Education medical student simulation-based surgical skills curriculum needs assessment. Am J Surg. 2014;207(2):165–9. doi:10.1016/j.amjsurg.2013.07.032. Needs assessment of Clerkship Directors and medical students to identify educational content for a simulation-based curriculum for medical students.
∙ Acton RD, Jones DB LKR. American College of Surgeons and Association for Surgical Education medical student simulation based surgical skills curriculum. Bull Am Coll Surg. 2015;100(4):35–9. Overview of ACS/ASE simulation-based curriculum for medical students, including methods of curriculum development and modules within the curriculum.
American College of Surgeons. ACS/ASE medical student simulation-based surgical skills curriculum. 2013. https://www.facs.org/education/program/simulation-based. Accessed 20 Apr 2017.
Louridas M, Szasz P, Fecso AB, Zywiel MG, Lak P, Bener AB, et al. Practice does not always make perfect: need for selection curricula in modern surgical training. Surg Endosc. 2017;70(2):193–9. doi:10.1007/s00464-017-5572-3.
∙ Gardner AK, Ritter EM, Paige JT, Ahmed RA, Fernandez G, Dunkin BJ. Simulation-based selection of surgical trainees: considerations, challenges, and opportunities. J Am Coll Surg. 2016;223(3):530–6. doi:10.1016/j.jamcollsurg.2016.05.021. Aimee can you give a brief summary of why this is important please?
∙ Gardner AK, Steffes CP, Nepomnayshy D, Nicholas C, Widmann WD, Fitzgibbons SC, et al. Selection bias: examining the feasibility, utility, and participant receptivity to incorporating simulation into the general surgery residency selection process. Am J Surg. 2016;1171–7. doi:10.1016/j.amjsurg.2016.09.029. Aimee can you give a brief summary of why this is important please?
Okusanya OT, Kornfield ZN, Reinke CE, Morris JB, Sarani B, Williams NN, et al. The effect and durability of a pregraduation boot camp on the confidence of senior medical student entering surgical residencies. J Surg Educ. 2012;69(4):536–43. doi:10.1016/j.jsurg.2012.04.001.
∙∙ Minter RM, Amos KD, Bentz ML, Blair PG, Brandt C, D’Cunha J, et al. Transition to surgical residency. Acad Med. 2015;90(8):1116–24. doi:10.1097/ACM.0000000000000680. Mixed-methods, multi-institutional evaluation of surgery interns’ preparedness for surgical residency. This study compares responses from interns who participated in a residency preparatory course in their fourth year of medical school compared to those that had not participated in a preparatory course.
ACS/ASE/APDS Resident Prep Curriculum. 2014. https://www.facs.org/education/program/resident-prep. Accessed 16 Apr 2017.
Krajewski A, Filippa D, Staff I, Singh R, Kirton OC. Implementation of an intern boot camp curriculum to address clinical competencies under the new accreditation council for graduate medical education supervision requirements and duty hour restrictions. JAMA Surg. 2013;148(8):727. doi:10.1001/jamasurg.2013.2350.
Fernandez GL, Page DW, Coe NP, Lee PC, Patterson LA, Skylizard L, et al. Boot camp: educational outcomes after 4 successive years of preparatory simulation-based training at onset of internship. J Surg Educ. 2012;69(2):242–8. doi:10.1016/j.jsurg.2011.08.007.
∙∙ Stefanidis D, Sevdalis N, Paige J, Zevin B, Aggarwal R, Grantcharov T, et al. Simulation in surgery: what’s needed next? Ann Surg. 2015;261(5):846–53. doi:10.1097/SLA.0000000000000826. A very important review of the current state of surgical simulation that identifies challenges to implementation in training programs, and directions for future research.
Aggarwal R, Grantcharov TP, Darzi A. Framework for systematic training and assessment of technical skills. J Am Coll Surg. 2007;204(4):697–705. doi:10.1016/j.jamcollsurg.2007.01.016.
Zevin B, Levy JS, Satava RM, Grantcharov TP. A consensus-based framework for design, validation, and implementation of simulation-based training curricula in surgery. J Am Coll Surg. 2012;215(4):580–6. doi:10.1016/j.jamcollsurg.2012.05.035.
Stefanidis D. The formula for a successful laparoscopic skills curriculum. Arch Surg. 2009;144(1):77. doi:10.1001/archsurg.2008.528.
Scott DJ, Goova MT, Tesfay ST. A cost-effective proficiency-based knot-tying and suturing curriculum for residency programs. J Surg Res. 2007;141(1):7–15. doi:10.1016/j.jss.2007.02.043.
Goova MT, Hollett LA, Tesfay ST, Gala RB, Puzziferri N, Kehdy FJ, et al. Implementation, construct validity, and benefit of a proficiency-based knot-tying and suturing curriculum. J Surg Educ. 2008;65(4):309–15. doi:10.1016/j.jsurg.2008.04.004.
Mashaud LB, Arain NA, Hogg DC, Scott DJ. Development, validation, and implementation of a cost-effective intermediate-level proficiency-based knot-tying and suturing curriculum for surgery residents. J Surg Educ. 2013;70(2):193–9. doi:10.1016/j.jsurg.2012.09.008.
∙ Gomez PP, Willis RE, Schiffer BL, Gardner AK, Scott DJ. External validation and evaluation of an intermediate proficiency-based knot-tying and suturing curriculum. J Surg Educ. 2014;71(6):839–45. doi:10.1016/j.jsurg.2014.04.013. Evaluated the use of UT southwest intermediate proficiency knot-tying and suturing curriculum at external programs- showed external validity and construct validity of the curriculum. Also showed that interns could be trained to proficiency on intermediate tasks using simulation.
Barsuk JH, Cohen ER, Feinglass J, McGaghie WC, Wayne DB. Use of simulation-based education to reduce catheter-related bloodstream infections. Arch Intern Med. 2009;169(15):1420–3. doi:10.1001/archinternmed.2009.215.
Cohen ER, Feinglass J, Barsuk JH, Barnard C, O’Donnell A, McGaghie WC, et al. Cost savings from reduced catheter-related bloodstream infection after simulation-based education for residents in a medical intensive care unit. Simul Healthc. 2010;5(2):98–102. doi:10.1097/SIH.0b013e3181bc8304.
Ma IWY, Brindle ME, Ronksley PE, Lorenzetti DL, Sauve RS, Ghali WA. Use of simulation-based education to improve outcomes of central venous catheterization: a systematic review and meta-analysis. Acad Med. 2011;86(9):1137. doi:10.1097/ACM.0b013e318226a204.
Fried GM, Feldman LS, Vassiliou MC, Fraser SA, Stanbridge D, Ghitulescu G, et al. Proving the value of simulation in laparoscopic surgery. Ann Surg. 2004;240(3):518–528. doi:10.1097/01.sla.0000136941.46529.56.
McCluney AL, Vassiliou MC, Kaneva PA, Cao J, Stanbridge DD, Feldman LS, et al. FLS simulator performance predicts intraoperative laparoscopic skill. In: Surgical endoscopy and other interventional techniques. 2007. p. 1991–5. doi:10.1007/s00464-007-9451-1.
Sroka G, Feldman LS, Vassiliou MC, Kaneva PA, Fayez R, Fried GM. Fundamentals of laparoscopic surgery simulator training to proficiency improves laparoscopic performance in the operating room-a randomized controlled trial. Am J Surg. 2010;199(1):115–20. doi:10.1016/j.amjsurg.2009.07.035.
Derossis AM, Bothwell J, Sigman HH, Fried GM. The effect of practice on performance in laparoscopic simulator. Surg Endosc. 1998;12:1117–20. doi:10.1007/s004649900796.
∙ Dawe SR, Pena GN, Windsor JA, Broeders JAJL, Cregan PC, Hewett PJ, et al. Systematic review of skills transfer after surgical simulation-based training. Br J Surg. 2014;101(9):1063–76. doi:10.1002/bjs.9482. Showed that proficiency in simulation-based training relates to clinical performance (skills transfer), with simulation trained participants having improved performance in patient-based setting compared to those without simulation training.
Zendejas B, Brydges R, Hamstra SJ, Cook DA. State of the evidence on simulation-based training for laparoscopic surgery: a systematic review. Ann Surg [Internet]. 2013;257(4):586–93. doi:10.1097/SLA.0b013e318288c40b.
Scott DJ, Ritter EM, Tesfay ST, Pimentel EA, Nagji A, Fried GM. Certification pass rate of 100% for fundamentals of laparoscopic surgery skills after proficiency-based training. Surg Endosc Other Interv Tech. 2008;22(8):1887–93. doi:10.1007/s00464-008-9745-y.
Ritter EM, Scott DJ. Design of a proficiency-based skills training curriculum for the fundamentals of laparoscopic surgery. Surg Innov. 2007;14:107–12. doi:10.1177/1553350607302329.
Castellvi AO, Hollett LA, Minhajuddin A, Hogg DC, Tesfay ST, Scott DJ. Maintaining proficiency after fundamentals of laparoscopic surgery training: a 1-year analysis of skill retention for surgery residents. Surgery. 2009;146(2):387–93. doi:10.1016/j.surg.2009.05.009.
Nagendran M, Ks G, Aggarwal R, Loizidou M, Br D. Virtual reality training for surgical trainees in laparoscopic surgery. Cochrane Database Syst Rev. 2013;8:1–45. doi:10.1002/14651858.CD006575.pub3.
Derevianko AY, Schwaitzberg SD, Tsuda S, Barrios L, Brooks DC, Callery MP, et al. Malpractice carrier underwrites fundamentals of laparoscopic surgery training and testing: a benchmark for patient safety. Surg Endosc Other Interv Tech. 2010;24(3):616–23. doi:10.1007/s00464-009-0617-x.
Harris JD, Hosford CC, Sticca RP. A comprehensive analysis of surgical procedures in rural surgery practices. Am J Surg. 2010;200(6):820–6. doi:10.1016/j.amjsurg.2010.07.029.
Decker MR, Dodgion CM, Kwok AC, Hu YY, Havlena JA, Jiang W, et al. Specialization and the current practices of general surgeons. J Am Coll Surg. 2014;218(1):8–15. doi:10.1016/j.jamcollsurg.2013.08.016.
Accreditation Council for Graduate Medical Education. Surgery and pediatric surgery program requirements. RRC News for Surgery 2008.
SAGES. SAGES fundamentals of endoscopic surgery (FES) required by american board of surgery, fes elevates the standards and training for minimally invasive surgery. PR Web [Internet]. 2014
∙ Dietl CA, Russell JC. Effects of technological advances in surgical education on quantitative outcomes from residency programs. J Surg Educ. 2016;73(5):819–30. doi:10.1016/j.jsurg.2016.03.016. Systematic review of current technology and simulation in surgical education and their impact on performance on training metrics.
Wilcox V, Trus T, Salas N, Martinez J, Dunkin BJ. A proficiency-based skills training curriculum for the sages surgical training for endoscopic proficiency (STEP) program. J Surg Educ [Internet]. 2014;71(3):282–8. doi:10.1016/j.jsurg.2013.10.004.
SAGES. Program description: fundamentals of endoscopic surgery. 2017. http://www.fesprogram.org/about/program-description-2/. Accessed 2 May 2017.
Hazey JW, Marks JM, Mellinger JD, Trus TL, Chand B, Delaney CP, et al. Why fundamentals of endoscopic surgery (FES)? Surg Endosc Other Interv Tech. 2014;28(3):701–3. doi:10.1007/s00464-013-3299-3.
Vassiliou MC, Dunkin BJ, Fried GM, Mellinger JD, Trus T, Kaneva P, et al. Fundamentals of endoscopic surgery: creation and validation of the hands-on test. Surg Endosc Other Interv Tech. 2014;28(3):704–11. doi:10.1007/s00464-013-3298-4.
∙ Ritter E, Taylor Z, Wolf K, Franklin B, Placek S, Korndorffer J, et al. Simulation based mastery learning for endoscopy using the endoscopy training system: a strategy to improve endoscopic skills and prepare for the Fundamentals of Endoscopic Surgery (FES) manual skills exam. Surg Endosc. 2017 (in press). Aimee can you give a brief summary of why this is important please- since I can’t actually find a copy anywhere.
Dawe SR, Windsor JA, Broeders JA, Cregan PC, Hewett PJ, Maddern GJ. A systematic review of surgical skills transfer after simulation-based training: laparoscopic cholecystectomy and endoscopy. Ann Surg. 2014;259(2):236–48. doi:10.1097/SLA.0000000000000245.
Dulan G, Rege RV, Hogg DC, Gilberg-Fisher KM, Arain NA, Tesfay ST, et al. Developing a comprehensive, proficiency-based training program for robotic surgery. Surg (United States). 2012;152(3):477–88. doi:10.1016/j.surg.2012.07.028.
Dulan G, Rege RV, Hogg DC, Gilberg-Fisher KM, Arain NA, Tesfay ST, et al. Proficiency-based training for robotic surgery: construct validity, workload, and expert levels for nine inanimate exercises. Surg Endosc Other Interv Tech. 2012;26(6):1516–21. doi:10.1007/s00464-011-2102-6.
Arain NA, Dulan G, Hogg DC, Rege RV, Powers CE, Tesfay ST, et al. Comprehensive proficiency-based inanimate training for robotic surgery: reliability, feasibility, and educational benefit. Surg Endosc Other Interv Tech. 2012;26(10):2740–5. doi:10.1007/s00464-012-2264-x.
Eckert M, Cuadrado D, Steele S, Brown T, Beekley A, Martin M. The changing face of the general surgeon: national and local trends in resident operative experience. Am J Surg. 2010;199(5):652–6. doi:10.1016/j.amjsurg.2010.01.012.
Fonseca AL, Evans LV, Gusberg RJ. Open surgical simulation in residency training: a review of its status and a case for its incorporation. J Surg Educ. 2013;70:129–37. doi:10.1016/j.jsurg.2012.08.007.
Kuhls DA, Risucci DA, Bowyer MW, Luchette FA. Advanced surgical skills for exposure in trauma: a new surgical skills cadaver course for surgery residents and fellows. J Trauma Acute Care Surg [Internet]. 2013;74(2):664–70. doi:10.1097/TA.0b013e31827d5e20.
Bowyer MW, Kuhls DA, Haskin D, Sallee RA, Henry SM, Garcia GD, et al. Advanced surgical skills for exposure in trauma (ASSET): the first 25 courses. J Surg Res. 2013;183(2):553–8. doi:10.1016/j.jss.2013.02.005.
Jacobs LM, Burns KJ, Kaban JM, Gross RI, Cortes V, Brautigam RT, et al. Development and evaluation of the advanced trauma operative management course. J Trauma. 2003;55(3):471–9. doi:10.1097/01.TA.0000059445.84105.26.
Jacobs LM, Burns KJ, Luk SS, Marshall WT 3rd. Follow-up survey of participants attending the advanced trauma operative management (ATOM) course. J Trauma [Internet]. 2005;58(6):1140–3. doi:10.1097/01.TA.0000171549.40895.2D.
Arriaga AF, Bader AM, Wong JM, Lipsitz SR, Berry WR, Ziewacz JE, et al. Simulation-based trial of surgical-crisis checklists. N Engl J Med. 2013;368(3):246–53. doi:10.1056/NEJMsa1204720.
Telem DA, Buch KE, Ellis S, Coakley B. Integration of a formalized handoff system into the surgical curriculum. Arch Surg. 2011;146(1):89. doi:10.1001/archsurg.2010.294.
Capella J, Smith S, Philp A, Putnam T, Gilbert C, Fry W, et al. Teamwork training improves the clinical care of trauma patients. J Surg Educ. 2010;67(6):439–43. doi:10.1016/j.jsurg.2010.06.006.
Arora S, Aggarwal R, Sevdalis N, Moran A, Sirimanna P, Kneebone R, et al. Development and validation of mental practice as a training strategy for laparoscopic surgery. Surg Endosc Other Interv Tech. 2010;24(1):179–87. doi:10.1007/s00464-009-0624-y.
Arora S, Aggarwal R, Sirimanna P, Moran A, Grantcharov T, Kneebone R, et al. Mental practice enhances surgical technical skills. Ann Surg. 2011;253(2):265–70. doi:10.1097/SLA.0b013e318207a789.
∙ Stefanidis D, Anton NE, McRary G, Howley LD, Pimentel M, Davis C, et al. Implementation results of a novel comprehensive mental skills curriculum during simulator training. Am J Surg. 2017;213(2):353–61. doi:10.1016/j.amjsurg.2016.06.027. Pilot study that evaluates the effectiveness of a novel mental skills curriculum to enhance surgical performance, which supports its use in surgical simulation-based training.
∙ Stefanidis D, Anton NE, Howley LD, Bean E, Yurco A, Pimentel ME, et al. Effectiveness of a comprehensive mental skills curriculum in enhancing surgical performance: results of a randomized controlled trial. Am J Surg. 2017;213(2):318–24. doi:10.1016/j.amjsurg.2016.10.016. Randomized controlled trial that evaluated the effectiveness of a novel mental skills curriculum with surgical novices, which indicated that the curriculum was effective at enhancing surgical skill retention over time.
Arora S, Sevdalis N, Nestel D, Woloshynowych M, Darzi A, Kneebone R. The impact of stress on surgical performance: a systematic review of the literature. Surgery. 2010;147(3):318–330. doi:10.1016/j.surg.2009.10.007.
Ericsson KA. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med. 2004;79(10):870–81.
Coker CA, Fishman MG. Motor skill learning for effective coaching and performance. In: Williams JM, editor. Applied sport psychology: personal growth to peak performance. New York: McGraw Hill; 2010. p. 21–41.
Bresser F, Wilson C. What is coaching? In: Passmore J, editor. Excellence in coaching: the industry guide. London: Kogan Page Limited; 2010. p. 9–27.
∙ Min H, Morales DR, Orgill D, Smink DS, Yule S. Systematic review of coaching to enhance surgeons’ operative performance. Surg (United States). 2015;158(5):1168–91. doi:10.1016/j.surg.2015.03.007. Comprehensive review of coaching interventions with surgeons and trainees, which can help inform future coaching interventions.
∙ Stefanidis D, Anderson-Montoya B, Higgins R V, Pimentel ME, Rowland P, Scarborough MO, et al. Developing a coaching mechanism for practicing surgeons. Surg (United States). 2016;160(3):536–45. doi:10.1016/j.surg.2016.03.036. Study of a novel coaching mechanism for practicing surgeons, which identified several nontechnical and technical skills to improve through coaching.
Reznick RK. Teaching and testing technical skills. Am J Surg. 1993;165(March):4.
∙ Mackenzie H, Cuming T, Miskovic D, Wyles SM, Langsford L, Anderson J, et al. Design, delivery, and validation of a trainer curriculum for the national laparoscopic colorectal training program in England. Ann Surg. 2015;261(1):149–56. doi:10.1097/SLA.0000000000000437. Study of the effectiveness of a train the trainer course for a laparoscopic colorectal training program, which is designed to standardize trainer instruction. The researchers found that this train the trainer course effectively enhanced short- and long-term training performance.
∙∙ Timberlake MD, Mayo HG, Scott L, Weis J, Gardner AK. What do we know about intraoperative teaching?: A systematic review. Ann Surg. 2017 Jan; doi:10.1097/SLA.0000000000002131. An important review to identify important characteristics of effective intraoperative teaching to inform future interventions to enhance faculty instruction.
Rogers SO, Gawande AA, Kwaan M, Puopolo AL, Yoon C, Brennan TA, et al. Analysis of surgical errors in closed malpractice claims at 4 liability insurers. Surgery. 2006;140(1):25–33. doi:10.1016/j.surg.2006.01.008.
∙ Siu J, Maran N, Paterson-Brown S. Observation of behavioural markers of non-technical skills in the operating room and their relationship to intra-operative incidents. Surgeon. 2016;14(3):119–28. doi:10.1016/j.surge.2014.06.005. Study of OR team members’ nontechnical skills that influence surgical safety, which found that a significant number of avoidable incidents that compromise surgical safety are related to poor nontechnical skills.
Steinemann S, Berg B, Skinner A, Ditulio A, Anzelon K, Terada K, et al. In situ, multidisciplinary, simulation-based teamwork training improves early trauma care. J Surg Educ. 2011;68(6):472–7. doi:10.1016/j.jsurg.2011.05.009.
∙ Arriaga AF, Gawande AA, Raemer DB, Jones DB, Smink DS, Weinstock P, et al. Pilot testing of a model for insurer-driven, large-scale multicenter simulation training for operating room teams. Ann Surg. 2014;259(3):403–10. doi:10.1097/SLA.0000000000000342. Pilot study of a teamwork training program for OR teams implemented during simulation training, which was widely acknowledged to be realistic and relevant to participants’ clinical practice.
ACGME Program Requirements. 2016. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/440_general_surgery_2016.pdf. Accessed 5 May 2017.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Steinemann is President Elect for Association for Surgical Education and Vice Chair of American College of Surgeons Committee on Medical Student Education. Drs. Gardner and Perone and Mr. Anton declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical collection on Surgical Education.
Rights and permissions
About this article
Cite this article
Perone, J.A., Anton, N.E., Gardner, A.K. et al. Simulation Training in Surgical Education. Curr Surg Rep 5, 20 (2017). https://doi.org/10.1007/s40137-017-0182-5
Published:
DOI: https://doi.org/10.1007/s40137-017-0182-5