Abstract
Purpose of Review
Dementia is a highly prevalent and potentially devastating disease that has garnered considerable attention from public health researchers as a target for public policy. Given the multifactorial nature of its development and the lack of effective medical therapies, a common public health strategy for addressing this disease is to focus on its modifiable risk factors. Hearing loss is one such risk factor. The purpose of this review is to examine the role of hearing rehabilitation in modifying the association between hearing loss and cognitive impairment.
Recent Findings
Various studies have been conducted to analyze how hearing aid use may impact the relationship between hearing loss and cognitive impairment/dementia, including cross-sectional and retrospective cohort studies, prospective cohort studies, and randomized controlled trials (RCTs).
Summary
This review discusses the role of hearing loss as a modifiable risk factor for cognitive impairment/dementia, proposed causal mechanisms between hearing loss and cognitive impairment, and studies at multiple levels of evidence examining the role of hearing rehabilitation in mitigating the association between hearing loss and cognitive impairment. Although more randomized controlled trials of hearing aid use are required to clarify whether hearing aid use attenuates cognitive impairment, the authors recommend consideration of hearing aid use as one measure to potentially lower the risk of cognitive impairment/dementia development or progression in at-risk populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dementia is a highly prevalent and potentially devastating disease that has garnered considerable attention from researchers as a target for public policy. Over 57 million people globally are estimated to have dementia, and recent forecasts suggest that number could approximately triple by 2050, with much of that growth being due to a mixture of population growth and aging [1]. Although estimates of the economic impact of dementia vary, studies suggest societal costs of dementia have swelled as the prevalence of dementia has increased, even as some environments experience a reduction in dementia incidence [2•]. In 2010, for example, the total estimated worldwide costs of dementia were $604 million [3]. In contrast, the global annual costs of dementia were estimated to be over $1 trillion in 2018 and to increase to $2 trillion by 2030 [4, 5]. Dementia, as well as cognitive impairment in general, poses a significant financial burden on global health systems and economies if left unchecked.
Hearing Loss as a Modifiable Risk Factor of Cognitive Impairment and Dementia
Given the multifactorial nature of dementia and the lack of effective medical therapies, a common public health strategy for addressing this disease is to focus on its modifiable risk factors, in hopes of curbing its development or progression. Prior studies have identified numerous risk factors for dementia, with a 2020 Lancet report suggesting that modifying 12 risk factors might prevent or delay the development of up to 40% of cases of dementia [2•]. This same report estimated that more cases of dementia (8.2%) were attributable to hearing loss compared to any other identified risk factor. Extensive studies have found evidence of an independent association between hearing loss and cognitive impairment [6,7,8,9]. A prospective community-based study of 3,777 participants aged ≥ 65 years found, after adjusting for multiple confounders, that individuals with self-reported hearing problems were found to have an 18% higher risk of dementia [10]. In another prospective observational study of 1984 adults with a mean age of 77 years, researchers found that 1,162 individuals with baseline hearing loss (pure tone-average > 25 dB) demonstrated annual decreases in scores on multiple tests of cognition (Modified Mini-Mental State Examination, Digital Symbol Substitution Test) compared to those with normal hearing [11]. In this same study, individuals with hearing loss were found to have a 24% higher risk of incident cognitive impairment compared to those with normal hearing. Based on these and other studies, there is robust evidence that hearing loss is independently associated with cognitive impairment and the progression of dementia.
Similar to dementia, hearing loss represents a significant financial burden on the global economy, estimated by the World Health Organization to be in the range of $750–790 billion annually [12]. Hearing loss is highly prevalent, with almost a quarter (23%) of Americans aged 12 years and older affected directly by hearing loss [13]. The elderly are disproportionately affected by this condition, with nearly two-thirds (63%) of adults aged 70 years or older estimated to have hearing loss [14]. Despite this high prevalence, only about 1 in 7 individuals (14%) with hearing loss actually wears hearing aids [15]. Because previous analyses have supported a dose–response relationship between hearing loss and dementia, addressing hearing loss in moderate to severe cases may be a prudent method of addressing dementia risk [16].
Proposed Mechanisms Between Hearing Loss and Cognitive Decline
Although studies have documented an association between hearing loss and cognitive decline, the mechanisms underlying this relationship remain somewhat opaque. Multiple mechanisms have been posited, including both causal and common pathways [17]. One potential causal pathway, known as the cognitive load hypothesis, is that hearing loss leads to increased cognitive burden as individuals work harder to interpret auditory inputs, thereby depleting their cognitive resources to perform other functions such as understanding and making memories [18]. Another hypothesis is that, due to neuroplasticity, reduced auditory input resulting from peripheral hearing loss may over time lead to synaptic pruning and structural brain changes causing dementia [18]. Similarly, hearing loss may lead to decreased social interaction, thereby decreasing cognitive stimulation and predisposing individuals to cognitive decline [19]. Another suggested mechanism is microvascular disease as a common cause of both hearing loss and dementia. There is also the possibility of overdiagnosis of hearing loss and/or dementia, as recognizing one may lead to increased testing of the other [17]. It is important to consider that the relationship between hearing loss and cognitive decline may be a combination of some or all of the factors described above, in addition to other pathways that have not yet been identified. Regardless of the mechanism(s) responsible for the association between hearing loss and cognitive decline, hearing rehabilitation has attracted interest as a possible target to reduce the risk of dementia.
Purpose of Review
The purpose of this review is to examine the role of hearing rehabilitation in mitigating the association between hearing loss and cognitive impairment. We examine studies at multiple levels of evidence, including cross-sectional and retrospective cohort studies, prospective cohort studies, and randomized controlled trials (RCTs).
Summary of Current Literature
Cross-Sectional and Retrospective Studies
Using a subsample of the UK Biobank dataset, a cross-sectional analysis of 164,770 UK adults aged 40 to 69 years was performed to examine the role of hearing aid usage in the association between hearing loss and cognition. Cognitive measures included card games to assess reaction time and match pairs, as well as multiple-choice questions to assess fluid intelligence [20]. The authors found that hearing aid usage was associated with better working memory performance, but not episodic long-term memory.
In 2016, a cross-sectional study of 100 participants (comprising 34 hearing aid users and 66 non-hearing aid users) examined the relationship between hearing aid usage and cognition. Cognitive function was assessed by (1) the Mini-Mental State Exam (MMSE) to measure global cognitive function and (2) the Trail-Making Test, Part B (TMT-B) to measure executive function [21]. Of note, hearing aid users demonstrated worse hearing at both low and high frequencies (p < 0.001) compared to non-hearing aid users. Compared to non-hearing aid users, hearing aid users performed significantly better on the MMSE (p = 0.008) but not the TMT-B (p = 0.7). Potential confounders such as socioeconomic status and education level were not controlled for in this study, limiting any conclusions about the association between hearing aid usage and cognition.
In 2021, a retrospective analysis of data from two ongoing longitudinal cohort studies in two areas of Japan (comprising 90 hearing aid users and 1512 non-hearing aid users) examined the association between hearing aid usage and cognition. Measures of cognition included (1) the delayed word recall task as a memory screening task and (2) the clock drawing test (CDT) as an executive function screening task [22]. Although there were no significant differences between the groups for the delayed word recall test, hearing aid users were less likely to properly draw the clock compared to non-hearing aid users. The authors noted that hearing aid users were more likely to have a frequent physical exercise habit compared to non-hearing aid users (p = 0.042), which they suggested could relate to having positive attitudes about health and a willingness to avoid social frailty, or possibly because of hearing aids having a mitigating effect on the cognitive decline [23]. Notably, the groups in this study demonstrated significantly different ages (median age 80 in hearing aid users, 73 in non-hearing aid users; p < 0.001) and were not controlled for other potential confounders such as socioeconomic status.
Prospective Cohort Studies
Prospective observational cohort studies offer evidence of a longitudinal association between hearing aid usage and cognitive function. In 2015, in a prospective population-based study using data from the Personnes Agées QUID study, a cohort study begun in 1989–1990, authors investigated the association between self-reported hearing loss, hearing aid usage, and cognitive decline. The authors analyzed the data of 1,276 participants with self-reported hearing loss (150 of which used hearing aids) aged > 65 years and assessed cognition with the MMSE at interval follow-up visits [24]. In comparing non-hearing aid users to a control group, the authors found that a faster decline in MMSE score over the 25-year follow-up period was observed (p < 0.001). In contrast, when comparing hearing aid users to a control group, the rate of change in MMSE score over the 25-year follow-up period was not significant (p = 0.08). The authors concluded that hearing aid usage attenuates cognitive decline in older adults. However, after controlling for potential confounding factors (including depressive symptoms, social network variables, dependency for independent activities of daily living, psychotropic drug use, and notably dementia), this difference in cognitive decline between hearing aid users and non-hearing aid users was not significant. It is worth noting that the study includes no direct comparison between hearing aid users and non-hearing aid users.
Another longitudinal study of 2,040 adults aged 50 and older participating in the Health and Retirement Study relied on an 18-year follow-up to examine the relationship between hearing aid usage and cognitive decline, specifically in episodic memory. Hearing aid use was a self-reported measure and only subjects who began using hearing aids after the first few waves of the study were included [25]. Episodic memory was measured using immediate and delayed word recall, and scores were calculated by adding the words remembered after the immediate and delayed recall phases, with a possible range of 0 to 20. After adjusting for demographics, socioeconomic characteristics, lifestyle behavior, and health status, the authors found that subjects had a slower rate of decline in episodic memory scores after using hearing aids (β = − 0.03, p < 0.001) compared to before using hearing aids (β = − 0.11, p < 0.001).
Other studies found no significant association between hearing aid usage and cognitive decline. For instance, an 8-year (2008–2016) longitudinal study of 10,107 men aged 62 years and older in the Health Professionals Follow-up Study found that in men with severe hearing loss (comprising 65 non-hearing aid users and 179 hearing aid users), subjects who wore hearing aids exhibited no significant attenuation (p = 0.4) of the rate of subjective cognitive decline [26].
Randomized Controlled Trials
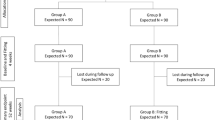
RCTs examining hearing aid usage and cognitive function are sparse and limited in follow-up or size. An RCT conducted in 1990 at primary care clinics at a Bureau of Veterans Affairs hospital examined 194 hearing-impaired elderly veterans. Subjects were randomly assigned to receive a hearing aid (n = 95) or join a waiting list (n = 99) [27]. Cognitive function was measured using the Short Portable Mental Status Questionnaire (SPMSQ), which was scored from 0 to 10, with higher scores indicating more cognitive impairment. Although both groups were determined to be demographically and medically similar, they exhibited different baseline scores on the SPMSQ (0.47 in the hearing aid group vs 0.18 in the waiting list group). After a 4-month follow-up, the authors found no significant change in SPMSQ in the waiting list group (0.18 to 0.28, p > 0.10) and a significant decrease in SPMSQ in the hearing aid group (0.47 to 0.29, p < 0.05), suggesting that hearing aids may improve cognition. Because this study used unilateral aids that were also less technologically sophisticated than current technology, it is likely that the observed effects are underestimates.
Authors of a 2021 systematic review noted that of the areas of cognitive function assessed in the literature, the executive function domain seems to have the largest evidence base of a benefit of hearing aid usage on cognition [28••]. In contrast, the least beneficial impact has been seen when measuring the complex attention domain of cognition. This study determined that frequently short follow-up times meant many existing studies had a high risk of bias and that, given the lack of conclusive evidence, the impact of hearing aid usage on cognitive function needs further study.
Cochlear Implants and Cognitive Impairment
In addressing the relationship between hearing loss and cognitive impairment, it is important to consider the potential role that cochlear implants may play in mitigating the risk of cognitive impairment for individuals with more severe hearing loss. In a 2016 longitudinal case series (n = 7), participants took a series of 20 tests assessing a variety of cognitive functions before and after cochlear implantation, with a mean follow-up time of 3.7 years. The participants demonstrated improvements in 14 (70%) and declines in 5 (25%) of the subtests administered, with the largest improvements in the verbal and memory domains [29]. In a longitudinal and cross-sectional cohort study comparing cochlear implant recipients aged ≥ 65 years to cochlear implant recipients aged ≤ 50 years and normal hearing participants aged ≥ 65 years, the authors found no significant difference in MMSE scores between elderly cochlear implant recipients and the normal-hearing participants (median, 28 vs. 28, p = 0.5) [30]. In a 2022 prospective interventional study comparing cochlear implant recipients pre- and post-implantation, participants demonstrated statistically significant improvements in concentration performance on the d2 Test of Attention, Hayling Sentence Completion Test, Hopkins Verbal Learning Test-Revised (total and delayed recall), Spatial Span (backward), and Stroop Color and Word Test. The authors noted that a subgroup analysis comparing 13 participants with preoperative cognitive impairment to 24 participants with normal preoperative cognition found a greater improvement in individuals with preoperatively impaired cognition [31]. However, due to studies often being limited by small sample size, short follow-up, or lack of randomization, further investigation is needed. A systematic review published in 2018 determined that there is a lack of conclusive evidence that cochlear implantation improves cognitive outcomes in older adults [32].
Ultimately, a clear causal relationship between hearing loss and cognitive decline has not yet been found but remains an area for future research. Further RCTs with standard measures of cognitive performance are required to determine if there is a causal relationship before offering definitive guidance on addressing hearing loss to reduce dementia risk.
Limitations
Analysis of how hearing rehabilitation may affect the relationship between hearing loss and cognitive decline is often limited by a variety of factors. Although some small to moderately sized RCTs of hearing aid provision exist, these trials are expensive and difficult to conduct. Further, testing for measures of cognitive decline requires conducting these trials over long periods of time to account for the long time course of cognitive change and development of dementia. As with much medical device research, blinding for experimental trials with hearing aids is essentially impossible in that participants would be able to detect a sham hearing aid that does not amplify. Even if control groups were given hearing aids that amplified subtherapeutically, the effect size would likely be reduced. Some researchers have also raised ethical concerns about the denial of hearing aid treatment for individuals with moderate-to-severe hearing loss that may limit RCTs primarily to analysis of individuals with mild hearing loss. To tackle this problem, researchers may conduct RCTs comparing a treatment group to a delayed treatment group, so both groups are ultimately provided hearing aids. However, this waitlist approach may be more difficult for trials requiring long periods of follow-up, as discussed above.
Additionally, a bias toward studying primarily high-income populations threatens our understanding of the relationship between hearing loss and dementia. Much of the understanding of risk factors of dementia comes from studies performed in high-income countries. Notably, risk factor profiles for the development of dementia in other environments may differ [2•]. Given that many risk factors like hearing loss are likely more prevalent among lower-income populations due to lower rates of education and access to healthcare resources, these biases may result in studies underestimating the role that hearing aid use might play in slowing or halting the development or progression of dementia. If the potential benefit of hearing aid use in low-income settings is underestimated, resource allocation based on these studies might fail to account for the full benefit of hearing aid provision on dementia-related outcomes in poor and marginalized populations.
Conclusions
More rigorous randomized controlled trials of hearing aid use are required to clarify whether a causal relationship between hearing aid use and attenuation of cognitive decline exists. Larger sample sizes and longer follow-ups are especially necessary to qualify this relationship. Because hearing aid provision comes with little risk and large theoretical benefit given the current body of literature, the authors recommend consideration of hearing aid use as one potential measure to lower the risk of cognitive decline or progression to dementia in at-risk populations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Collaborators GDF. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the Global Burden of Disease Study 2019. The Lancet Public Health. 2022;7(2): e105.
• Livingston G, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020;396(10248):413–446. This paper is a review of 12 potentially modifiable risk factors for dementia, including hearing impairment.
Wimo A, et al. The worldwide economic impact of dementia 2010. Alzheimers Dement. 2013;9(1):1–11e3.
Wimo A, et al. The worldwide costs of dementia 2015 and comparisons with 2010. Alzheimers Dement. 2017;13(1):1–7.
Prince MJ, et al. World Alzheimer Report 2015-The global impact of dementia: an analysis of prevalence, incidence, cost and trends. 2015.
Lin FR, et al. Hearing loss and cognition in the Baltimore Longitudinal Study of Aging. Neuropsychology. 2011;25(6):763–70.
Tay T, et al. Sensory and cognitive association in older persons: findings from an older Australian population. Gerontology. 2006;52(6):386–94.
Lin FR. Hearing loss and cognition among older adults in the United States. J Gerontol A Biol Sci Med Sci. 2011;66(10):1131–6.
Valentijn SA, et al. Change in sensory functioning predicts change in cognitive functioning: results from a 6-year follow-up in the maastricht aging study. J Am Geriatr Soc. 2005;53(3):374–80.
Amieva H, et al. Death, depression, disability, and dementia associated with self-reported hearing problems: a 25-year study. J Gerontol A Biol Sci Med Sci. 2018;73(10):1383–9.
Lin FR, et al. Hearing loss and cognitive decline in older adults. JAMA Intern Med. 2013;173(4):293–9.
WHO. Global costs of unaddressed hearing loss and cost-effectiveness of interventions: a WHO report. 2017.
Goman AM, Lin FR. Prevalence of hearing loss by severity in the United States. Am J Public Health. 2016;106(10):1820–2.
Lin FR, et al. Hearing loss prevalence and risk factors among older adults in the United States. J Gerontol A Biol Sci Med Sci. 2011;66(5):582–90.
Chien W, Lin FR. Prevalence of hearing aid use among older adults in the United States. Arch Intern Med. 2012;172(3):292–3.
Thomson RS, et al. Hearing loss as a risk factor for dementia: a systematic review. Laryngoscope Investig Otolaryngol. 2017;2(2):69–79.
Chern A, Golub JS. Age-related hearing loss and dementia. Alzheimer Dis Assoc Disord. 2019;33(3):285–90.
Sweller J. Cognitive load theory. In: Psychology of learning and motivation. Elsevier; 2011. p. 37–76.
Shukla A, et al. Hearing loss, loneliness, and social isolation: a systematic review. Otolaryngol Head Neck Surg. 2020;162(5):622–33.
Ronnberg J, et al. The effect of functional hearing loss and age on long- and short-term visuospatial memory: evidence from the UK Biobank resource. Front Aging Neurosci. 2014;6:326.
Qian ZJ, et al. Hearing aid use is associated with better mini-mental state exam performance. Am J Geriatr Psychiatry. 2016;24(9):694–702.
Saji N, et al. Hearing impairment is associated with cognitive function in community-dwelling older adults: a cross-sectional study. Arch Gerontol Geriatr. 2021;93: 104302.
Bae S, et al. The role of social frailty in explaining the association between hearing problems and mild cognitive impairment in older adults. Arch Gerontol Geriatr. 2018;78:45–50.
Amieva H, et al. Self-reported hearing loss, hearing aids, and cognitive decline in elderly adults: a 25-year study. J Am Geriatr Soc. 2015;63(10):2099–104.
Maharani A, et al. Longitudinal relationship between hearing aid use and cognitive function in older Americans. J Am Geriatr Soc. 2018.
Curhan SG, et al. Longitudinal study of hearing loss and subjective cognitive function decline in men. Alzheimers Dement. 2019;15(4):525–33.
Mulrow CD, et al. Quality-of-life changes and hearing impairment a randomized trial. Ann Intern Med. 1990;113(3):188–94.
•• Sanders ME, et al. The effect of hearing aids on cognitive function: a systematic review. PLoS One. 2021:16(12):e0261207. This paper provides a thorough systematic review of existing evidence for hearing aid use as a method of slowing the progression of cognitive decline.
Cosetti MK, et al. Neurocognitive testing and cochlear implantation: insights into performance in older adults. Clin Interv Aging. 2016;11:603–13.
Sorrentino T, et al. Cognitive function and quality of life in older adult patients with cochlear implants. Int J Audiol. 2020;59(4):316–22.
Gurgel RK, et al. Evaluating the impact of cochlear implantation on cognitive function in older adults. Laryngoscope. 2022;132:S1–15.
Claes AJ, et al. Cognitive performance of severely hearing-impaired older adults before and after cochlear implantation: preliminary results of a prospective, longitudinal cohort study using the RBANS-H. Otol Neurotol. 2018;39(9):e765–73.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Denham: none; Golub: Advisory board (Alcon), Consulting fees (Decibel Therapeutics). The authors have no other existing conflicts of interest.
Human and Animal Rights and Informed Consent Statement
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical collection on OTOLOGY: Advances in Otology
Rights and permissions
About this article
Cite this article
Denham, M., Golub, J.S. Does Hearing Rehabilitation Mitigate the Association Between Hearing Loss and Cognitive Impairment?. Curr Otorhinolaryngol Rep 10, 310–314 (2022). https://doi.org/10.1007/s40136-022-00412-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40136-022-00412-7