Abstract
Purpose of Review
The aim of this review is to discuss the evaluation, workup, indications, and outcomes of sialendoscopy in children. Many factors contribute to salivary gland disease in children including autoimmune disease, genetic defects, viral or bacterial infections, and congenital ductal abnormalities. Sialadenitis is acute swelling of the major salivary glands. In children, parotid sialadenitis is more common than submandibular sialadenitis and sialolithiasis (saliva gland stone) is rare. Before widespread use of the MMR vaccine, mumps, a paromyxovirus, was the most common cause of parotitis in children. In the current era, the most common cause of parotitis in children is juvenile recurrent parotitis (JRP). JRP is a nonspecific sialadenitis associated with recurrent inflammation of the parotid glands. The first episode of JRP generally occurs between the age of 3 and 6 years of age. The interval between acute episodes is variable, with an average from 15 days to 2 months. The treatment of acute sialadenitis includes analgesics, antibiotics, and other conservative measures such as sialogogues, warm compresses, hydration, and massage. Historically, for JRP patients who failed conservative measures, parotidectomy was offered but was associated with significant potential morbidity. Sialendoscopy has emerged as a safe and effective diagnostic and therapeutic option for recurrent sialadenitis with and without stones.
Recent Findings
Sialendoscopy is safe and effective for removal of small, distal salivary stones in the pediatric population. It can also lead to less frequent and severe episodes of acute sialadenitis in patients with JRP.
Summary
Sialendoscopy is a safe and effective procedure for recurrent sialadenitis in the carefully selected pediatric patient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sialendoscopy involves the use of miniature endoscopes that are introduced into the main salivary ducts of the parotid or submandibular glands. Salivary duct endoscopy was first described in 1990 by Katz [1]. The equipment for sialendoscopy has continued to be modified and improved, enhancing minimally invasive approaches to the salivary duct [2]. Sialendoscopy can be performed for both diagnostic and therapeutic purposes including to evaluate the main salivary ducts for sources of salivary flow obstruction and to help manage salivary duct stones, stenosis, mucus plugs, or strictures. In the pediatric population, sialendoscopy is most commonly used to help in patients with sialadenitis and to avoid more invasive treatments such as sialadenectomy [3].
Potential appropriate patients for consideration for sialendoscopy include those presenting with recurrent sialadenitis. These patients typically describe recurrent pain or swelling of the major salivary glands which can be exacerbated during eating. Some patients will note foul-tasting discharge in the mouth. Acute sialadenitis is typically managed with hydration, gland massage, sialogogues, and oral or intravenous antibiotics. Acute infection is a relative contraindication for sialendoscopy.
The most common pathologies treated with sialendoscopy in the pediatric population are recurrent sialadenitis with or without stones. The aim of this review is to discuss evaluation, workup, indications, and outcomes for sialendoscopy in children.
Patient Evaluation
Careful selection of patients who may benefit from sialendoscopy is key to successful outcomes. During evaluation, a complete history is taken to assess disease severity including symptom frequency and duration and number of courses of antibiotic therapy. A family history of autoimmune disease may lead to referral to an immunologist for further workup to rule out such disease processes as Sjogren’s syndrome.
Clinical exam includes a thorough evaluation of the head and neck with palpation of the glands, assessment of salivary flow from Wharton’s and Stensen’s ducts, and bimanual palpation for palpable salivary duct stones.
Imaging is also an important part of the evaluation of a child presenting with recurrent sialadenitis. Ultrasound is the imaging modality of choice for the pediatric population, since it avoids radiation and can be performed without sedation [4]. Sialolithiasis in the parotid or submandibular ducts will appear as hyperechoic lesions with posterior shadow. Sialoliths smaller than 2 mm and those located in distal submandibular ducts within the anterior floor of mouth may not be visualized on ultrasound [5]. Findings of gland heterogeneity or dilation of the main parotid duct are associated with JRP. Ultrasound of the salivary glands is operator dependent and further cross-sectional imaging is sometimes desired. Computed tomography (CT) imaging is used to identify calcifications and evaluate for acute inflammation and abscess formation. Diffuse microcalcifications in the gland parenchyma is typical in JRP. Magnetic resonance imaging (MRI) may be more useful to evaluate for vascular malformations, lymphadenopathy, salivary neoplasms, or branchial cleft cysts but in young children has the disadvantage of requiring general anesthesia [6]. Children presenting with recurrent unilateral parotid abscess should be evaluated for possible first branchial cleft cyst.
Sialendoscopy Setup
Sialendoscopy is typically performed under general anesthesia. Nasotracheal intubation should be considered for access to salivary stones located in the posterior floor of mouth near the hilum of the submandibular gland. For Stensen’s duct, the lip and buccal mucosa are retracted toward the surgeon to straighten the course of the parotid duct. For Wharton’s duct, a bite block is placed to open the oral cavity and care is taken to identify the papilla adjacent to the lingual frenulum. Wharton’s duct papilla is smaller and more difficult to cannulate than Stensen’s duct papilla. The papilla is serially dilated using dilator sets, lacrimal probes, or silastic dilators over a guidewire, taking care to avoid trauma to the mucosa around the papilla. Sialendoscope outer diameter sizes range from 0.89, 1.1, 1.3, to 1.6 mm (Karl Storz Endoscopy, El Segundo, CA). Each scope has an irrigation channel. The scopes 1.1 mm or larger have a working channel that allows for various microinstruments to be placed into the duct lumen. During sialendoscopy, saline irrigation through the scope is used to dilate the ducts. Care should be taken to avoid excessive irrigation to prevent soft tissue swelling that may lead to soft tissue edema and airway obstruction especially in young children.
Diagnostic Sialendoscopy
For diagnostic evaluation, the smallest 0.89 mm sialendoscope without a working channel may be used. Pathology within the salivary ducts may include thick debris or mucus plugs indicative of duct inflammation or chronic obstruction. Salivary duct calculi are found within the ducts and may be mobile or impacted against the duct walls. Focal strictures can be seen and webs or diaphragmatic membranes across a portion of the duct.
Sialolithiasis
Sialolithiasis is an uncommon cause of sialadenitis in children and the pathogenesis is not well understood [7,8,9,10,11,12,13,14,15]. Theories including intermittent secretion of microcalculi or migration of food debris and bacteria into the salivary ducts have been proposed. These substances then may act as a nidus for stone formation, especially in the milieu of decreased salivary flow and/or inflammation of the ductal system. Factors felt to favor submandibular sialolithiasis include the longer course of Wharton’s versus Stensen’s duct and the increased viscosity of saliva produced in the submandibular gland.
Workup
Multiple modalities have been used in the diagnosis of salivary stones including plain radiographs, CT, MR, cone-beam CT, sialography with iodinated contrast, and ultrasound [16]. Successful identification depends on the chemical composition of the stone contents as well as the size and location of the stone. Studies have shown variable rates of sensitivity and specificity with ultrasound, but there is consensus that in experienced hands, ultrasound can identify stones down to 1.5 mm [5]. The current gold standard for diagnosis of sialolithiasis remains the CT scan [13].
Treatment
In the acute setting, sialolithiasis is treated with conservative measures and antibiotics when indicated. Salivary stone removal is recommended for long-term management. Traditionally, this required sialadenectomy. Sialendoscopes have allowed gland-preserving approaches for sialolith removal with favorable stones. Sialoliths are visualized endoscopically in the Stensen’s or Wharton’s duct and captured by specialized baskets introduced through a working channel in the endoscope. For small sialoliths, the stone may be able to be removed with gentle traction through the duct papilla. For larger or impacted sialoliths, a combined transoral or more rarely, transfacial incision may be required to remove the sialolith from the duct [17]. Sialolith location can also predict the necessity for use of combined techniques for successful stone removal. Specifically, for the parotid duct, sialoliths located posterior to the masseter muscle within the hilum of the gland are difficult to access with purely endoscopic techniques and are more likely to require combined approach [18].
Outcomes
Successful sialendoscopic sialolith removal rates vary in the literature from 35 to 89% and depend on stone size, shape, location, ductal anatomy, and experience of the surgeon [19, 20]. Sialendoscopy with or without limited sialodochotomy has become the mainstay of sialolithiasis treatment [21].
Sialadenitis Without Stones or Juvenile Recurrent Parotitis
Juvenile recurrent parotitis (JRP) is the second most common salivary gland disorder in children, behind mumps [22,23,24,25,26,27]. JRP is diagnosed clinically based on recurrent episodes of nonsuppurative parotid swelling without other identifiable etiology. The clinical presentation is variable in severity and frequency. Children typically present with painful swelling of the parotid gland without overlying erythema and low-grade fever. Saliva may have a foul taste and may contain white particulates or debris on exam. Symptoms typically resolve over days to weeks. There is usually a dominance of one side, though it may be bilateral. Boys are more often affected than girls.
Etiology
Recurrent parotitis has also been associated with hypogammaglobulinemia, isolated immunoglobulin G3 deficiency, and immunoglobulin A deficiency as was seen in one patient in our study [28,29,30,31,32,33,34]. High concentrations of Streptococcus pneumoniae and Haemophilus influenzae have been isolated in the saliva of patients with JRP [35].
Some investigators have theorized that there is compromised vascularity in the salivary ducts of patients with JRP, leading to a compromise in salivary flow, stasis, and chronic inflammation [23]. Subsets of patients have been found to have mutations in a serine protease inhibitor (SPINK1) thought to be important in inhibiting proteolytic trypsin activity and tissue destruction [25]. There is also an association with HLA-B27 seropositivity [36]. Matrix metalloproteinases (MMP) 2 and 9 have been found to be elevated in saliva of JRP patients [37]. MMPs have been implicated in a variety of degenerative diseases associated with tissue destruction and remodeling.
Workup
Ultrasound and/or magnetic resonance imaging (MRI) have replaced sialography as imaging studies of choice for diagnosis of JRP [6]. Ultrasound is especially attractive in the pediatric population with the absence of need for sedation or anesthesia and the lack of radiation exposure when compared to computed tomography. Diffuse microcalcifications can be seen on imaging (Fig. 1). Sjogren’s syndrome can occur in childhood and has a presentation similar to JRP [30,31,32,33]. Typically, these children are older and have a female predominance. Laboratory testing, including ANA, SSA/SSB, and RF, may aid in diagnosis.
Treatment
To date, no preventive therapy for JRP has been identified. Historically, there was a paucity of treatment options for patients with JRP [38]. Development of sialendoscopy equipment specifically tailored to pediatric patients has the ability to offer a minimally invasive treatment for JRP. Sialendoscopy allows for confirmation of the diagnosis as well as the ability to flush the ducts and/or dilate to reduce future episodes. JRP is usually self-limiting with spontaneous regression during puberty. Conservative therapies are the first line approach, including analgesia, gland massage, hydration, warm compress, and sialogogues. For persistent or severe acute episodes, antibiotics may be helpful. Sialendoscopy is also an attractive, minimally invasive option. Intraductal steroids can be applied at the completion of the procedure; however, corticosteroid use has not been well studied and the degree of improvement and time course of benefit is not known. The optimal sialendoscopic flushing solution for JRP is an area of ongoing investigation. As the etiology of JRP is further elucidated, addition of MMP inhibitors or other target-specific anti-inflammatory mediators may increase therapeutic efficacy of sialendoscopy. Pro-angiogenic agents could also potentially have a beneficial therapeutic role to improve compromised ductal vascularity.
Outcomes
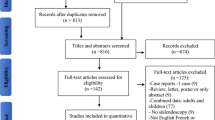
Several meta-analyses and systematic reviews have confirmed feasibility of and overall clinical improvement with sialendoscopy for patients with JRP, with success rates ranging from 73 to 93% [39,40,41,42,43,44,45, 46••, 47, 48, 49••, 50••, 51]. Most studies evaluating the treatment of JRP are limited by small patient population, retrospective design, and lack of control group. Further studies comparing treatment options and long-term outcomes are necessary.
Postoperative Care, Surgical Risks, and Complications
Postoperative antibiotics are not routinely prescribed except in the rare case that pus is encountered during sialendoscopy, in which case a broad-spectrum antibiotic is generally prescribed for 7–10 days. Complication rates of sialendoscopy vary throughout the literature (2–25%) and range from temporary gland swelling to duct avulsion requiring gland removal [19]. Other surgical risks can include perforation, stenosis, recurrence of obstruction, failure to remove salivary stone or all fragments, or injury to the papilla and should be discussed with parents prior to the procedure.
Swelling of the gland after sialendoscopy is expected and can take a few days to weeks to resolve, although the majority resolve within a few hours by the time the child is discharged from the recovery room. Most children are discharged the same day as the procedure. In young children, there is a small risk of airway obstruction with excessive irrigation into the deep parotid gland or of floor of mouth edema from excessive irrigation into the submandibular gland which may warrant overnight admission for airway monitoring. Tylenol and ibuprofen and generally sufficient for postoperative pain management. Parents are also encouraged to keep their child well hydrated.
Conclusions
Pediatric salivary gland disease remains relatively rare with JRP being the most common etiology. Characteristic findings on imaging and sialendoscopy can be used for diagnosis of JRP. Sialendoscopy appears to offer a safe, minimally invasive therapeutic option for those patients in whom the frequency and severity of episodes are impacting quality of life (QOL). It enhances our diagnostic capabilities beyond traditional imaging modalities of ultrasound, CT, and MRI. It can allow for the delivery of therapeutics—irrigation of medication, dilation of stenosis, intraductal fragmentation, or localization for stone removal. Finally, sialendoscopy helps avoid more invasive treatments and the associated morbidities.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Katz P. New method of examination of the salivary glands: the fiberscope. Inf Dent. 1990;72(10):785–6.
Marchal F, Dulguerov P. Sialolithiasis management: the state of the art. Arch Otolaryngol Head Neck Surg. 2003;129(9):951–6.
Faure F, Querin S, Dulguerov P, et al. Pediatric salivary gland obstructive swelling: sialendoscopic approach. Laryngoscope. 2007;117(8):1364–7.
Thomas WW, Douglas JE, Rassekh CH. Accuracy of ultrasound and computed tomography in the evaluation of patients undergoing sialendoscopy for sialolithiasis. Otolaryngol Head Neck Surg. 2017;156(5):834–9.
Terraz S, Poletti P, Dulguerov P, et al. How reliable is sonography in the assessment of sialolothiasis? AJR. 2013;201:W104–9.
Gadodia A, Seith A, Sharma R, Thakar A. MRI and mr sialography of juvenile recurrent parotitis. Pediatr Radiol. 2010;40:1405–10.
Zenk J, Koch M, Klintworth N, et al. Sialendoscopy in the diagnosis and treatment of sialolithiasis: a study on more than 1000 patients. Otolaryngol Head Neck Surg. 2013;147(5):858–63.
Harrison J. Causes, natural history, and incidence of salivary stones and obstructions. Otolaryngol Clin N Am. 2009;42(6):927–47.
Huoh K, Eisele D. Etiologic factors in sialolithiasis. Otolaryngol Head Neck Surg. 2011;145(6):935–9.
Harrison J, Epivantianos A, Bhatia S. Role of microliths in the aetiology of chronic submandibular sialadenitis: a clinicopathological investigation of 154 cases. Histopathology. 1997;31(3):237–51.
Epivatianos A, Harrison J, Dimitriou T. Ultrastructural and histochemical observations on microcalculi in chronic submandibular sialadenitis. J Oral Pathol. 1987;16(10):514–7.
Marchal F, Kurt A, Dulguerov P, et al. Retrograde theory in sialolithiasis formation. Arch Otolaryngol Head Neck Surg. 2001;127(1):66–8.
Kopec T, Wierzbicka M, Szyfter W, Leszczynska M. Algorithm changes in treatment of submandibular gland sialolithiasis. Eur Arch Otorhinolaryngol. 2013;270:2089–93.
Luers J, Grosheva M, Stenner M, Beutner D. Sialoendoscopy: prognostic factors for endoscopic removal of salivary stones. Arch Otolaryngol Head Neck Surg. 2011;137(4):325–9.
Witt R, Iro H, Kock M, et al. Minimally invasive options for salivary calculi. Laryngoscope. 2012;122:1306–11.
Galili D, Marmary Y. Juvenile recurrent parotitis: clinicoradiologic follow-up study and the beneficial effect of sialography. Oral Surg Oral Med Oral Pathol. 1986;61(6):550–6.
Carroll WW, Walvekar RR, Gillespie MB. Transfacial ultrasound-guided gland-preserving resection of parotid sialoliths. Otolaryngol Head Neck Surg. 2013;148(2):229–34.
Kiringoda R, Eisele DW, Chang JL. A comparison of parotid imaging characteristics and sialendoscopic findings in obstructive salivary disorders. Laryngoscope. 2014;124(12):2696–701.
Walvekar R, Razfar A, Carrau R, Schaitkin B. Sialendoscopy and associated complications: a preliminary experience. Laryngoscope. 2008;118:776–9.
Sigismund PE, Zenk J, Koch M, Schapher M, Rudes M, Iro H. Nearly 3,000 salivary stones: some clinical and epidemiologic aspects. Laryngoscope. 2015;125(8):1879–82.
Chang J, Eisele D. Limited distal sialodochotomy to facilitate sialendoscopy of the submandibular duct. Laryngoscope. 2013;123:1163–7.
Quenin S, Plouin-Gaudon I, Marchal F, et al. Juvenile recurrent parotitis: sialendoscopic approach. Arch Otolaryngol Head Neck Surg. 2008;134(7):715–9.
Nahlieli O, Shacham R, Shlesinger M, Eliav E. Juvenile recurrent parotitis: a new method of diagnosis and treatment. Pediatrics. 2004;114(1):9–12.
Shacham R, Droma E, London D, Bar T, Nahlieli O. Long-term experience with endoscopic diagnosis and treatment of juvenile recurrent parotitis. J Oral Maxillofac Surg. 2009;67(1):162–7.
Kohlo K, Saarinen R, Paju A, Stenman J, Stenman U, Pitkaranta A. New insights into juvenile parotitis. Acta Pediatr. 2005;94:1566–70.
Saarinen R, Kolho K, Davidkin I, Pitkaranta A. The clinical picture of juvenile parotitis in a prospective setup. Acta Pediatrica. 2012;102:177–81.
Capaccio P, Sigismund P, Luca N, Marchisio P, Pignataro L. Modern management of juvenile recurrent parotitis. J Laryngol Otol. 2012;126(12):1254–60.
Fazekas T, Wiesbauer P, Schroth B, et al. Selective IgA deficiency in children with recurrent parotitis of childhood. Ped Inf Dis J. 2005;24(5):461.
Banks G, Kirse D, Anthony E, Bergman S, Shetty A. Bilateral parotitis as the initial presentation of childhood sarcoidosis. Am J Otolaryngol. 2013;34(2):142–4.
Civilibal M, Canpolat N, Yurt A, et al. A child with primary Sjogren syndrome and a review of the literature. Clin Pediatr. 2007;46(8):738–42.
Kulkarni K. Unusual presentation of Sjogren syndrome. South Med J. 2005;98(12):1210–1.
de Souza T, Silva I, Carvalho A, et al. Juvenile Sjogren syndrome: distinctive age, unique findings. Pediatr Dent. 2012;34(5):427–30.
Peri Y, Agmon-Levi N, Theodor E, Shoenfield Y. Sjogren’s syndrome, the old and the new. Best Prac Res Clin Rheumatol. 2012;26:105–17.
Coca A, Sanz I. Updates on B-cell immunotherapies for systemic lupus erythematosus and Sjogren’s syndrome. Curr Opin Rheumatol. 2012;24:451–6.
Giglio M, Landaeta M, Pinto M. Microbiology of recurrent parotitis. Pediatr Infect Dis J. 1997;16(4):386–90.
Nguyen A, Francis C, Larsen C. Salivary endoscopy in a pediatric patient with HLA-B27 seropositivity and recurrent submandibular sialadenitis. Int J Pediatr Otorhinolaryngol. 2013;77:1045–7.
Morales-Bozo I, Landaeta M, Urzua-Orellana B, Retamales P. Association between the occurrence of matrix metalloproteinases 2 and 9 in parotid saliva with the degree of parotid gland damage in juvenile recurrent parotitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:377–83.
Katz P, Hartl D, Guerre A. Treatment of juvenile recurrent parotitis. Otolaryngol Clin N Am. 2009;42(6):1087–91.
Jabbour N, Tibesar R, Lander T, Sidman J. Sialendoscopy in children. Int J Pediatr Otorhinolaryngol. 2010;74(4):347–50.
Hackett A, Baranano C, Reed M, et al. Sialendoscopy for the treatment of pediatric salivary gland disorders. Arch Otolaryngol Head Neck Surg. 2012;138(10):912–5.
Martins-Carvalho C, Plouin-Gaudon I, Quenin S, et al. Pediatric sialendoscopy: a 5-year experience at a single institution. Arch Otolaryngol Head Neck Surg. 2010;136(1):33–6.
Strychowsky J, Sommer D, Gupta M, Cohen N, Nahieli O. Sialendoscopy for the management of obstructive salivary gland disease: a systematic review and meta-analysis sialendoscopy for salivary gland obstruction. Arch Otolaryngol Head Neck Surg. 2012;138:541–7.
Gary C, Kluka EA, Schaitkin B, Walvekar R. Interventional sialendoscopy for treatment of juvenile recurrent parotitis. J Indian Assoc Pediatr Surg. 2011;16(4):132–6.
Berta E, Angel G, Lagarde F et al. Role of sialendoscopy in juvenile recurrent parotitis (JRP). Eur Ann Otorhinolaryngol Head Neck Dis 2017;(17)30101–1. https://doi.org/10.1016/j.anorl.2017.06.004.
Schneider H, Kock M, Kunzel J, et al. Juvenile recurrent parotitis: a retrospective comparison of sialendoscopy versus conservative therapy. Laryngoscope. 2014;124:451–5.
•• Rosbe KW, Milev D, Chang JL. Effectiveness and costs of sialendoscopy in pediatric patients with salivary gland disorders. Laryngoscope. 2015;125(12):2805–9. Only review in the current literature to compare costs of medical therapy versus sialendoscopy for obstructive sialadenitis in children demonstrating equal effectiveness but much greater costs for sialendoscopy
Ogden MA, Rosbe KW, Chang JL. Pediatric sialendoscopy indications and outcomes. Curr Opin Otolaryngol Head Neck Surg. 2016;24(6):529–35.
Silva L, Babicsak G, Dolci RL. Salivary gland endoscopy in children: a systematic review. Rev Assoc Med Bras. 2016;62(8):795–9.
•• Capaccio P, Canzi P, Gaffuri M, et al. Modern management of paediatric obstructive salivary disorders: long-term clinical experience. Acta Otorhinolaryngol Ital. 2017;37:160–7. One of the largest reviews of pediatric patients undergoing sialendoscopy for obstructive sialadenitis with a reported success rate of 91% and mean follow-up of almost 2 years
•• Ramakrishna J, Strychowsky J, Gupta M, Sommer DD. Sialendoscopy for the management of juvenile recurrent parotitis: a systematic review and meta-analysis. Laryngoscope. 2015;125(6):1472–9. Meta-analysis of current literature on sialendoscopy for JRP. 7 studies included with conclusions that sialendoscopy is effective and safe
Roby BB, Mattingly J, Jensen EL, Gao D, Chan KH. Treatment of juvenile recurrent parotitis of childhood: an analysis of effectiveness. JAMA Otolaryngol Head Neck Surg. 2015;141(2):126–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Rosbe declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Pediatric Otolaryngology
Rights and permissions
About this article
Cite this article
Rosbe, K.W. Pediatric Sialendoscopy and Its Role in Pediatric Salivary Gland Disease. Curr Otorhinolaryngol Rep 5, 235–239 (2017). https://doi.org/10.1007/s40136-017-0162-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40136-017-0162-4