Abstract
Purpose of Review
The purpose of this review is illustrating most common bone tumors of the spine, emphasizing features that can be useful in the differential diagnosis.
Recent Findings
CT and MR imaging are indispensable to determine the extension and the relationship with the spinal canal structures, thus planning the optimal management.
Summary
Imaging modalities can provide useful tools for narrowing the differential diagnosis and directing biopsy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Primary tumors of the spine are infrequent lesions, representing less than 5% of all bone tumors [1, 2•]. Clinical manifestation and symptomatology of spine bone tumors can vary immensely, from asymptomatic to severe back pain, including mass effect with epidural or paravertebral soft tissue involvement, simulating other diseases with radiculopathy and myelopathy. Pain is the most prevalent symptom, accounting in 85% of patients with primary spinal tumors [3]. Other symptoms are nonspecific, which may often be attributed to degenerative disease, including back pain, weakness, radicular pain, and paresthesia [4••]. Imaging features of the primary spinal lesions are often nonspecific.
Differences in characteristic location and knowledge of the typical radiographic, scintigraphic, computed tomographic, or magnetic resonance imaging appearances may suggest diagnosis [5].
Imaging modalities can provide useful tools for narrowing the differential diagnosis and directing biopsy. In this article, the authors illustrate most common benign and malignant bone tumors of the spine, emphasizing features that can be useful in establishing a reasonable diagnosis.
Benign Lesions
Enostosis
Enostoses, also known as endosteomas, or more commonly, bone islands, were first described in 1905 [6]. These lesions have a propensity to occur in the axial skeleton, particularly the pelvis, spine, and ribs. Resnick and colleagues [7] reported enostoses in 14% of cadavers, making bone islands along with hemangiomas (11% of all cadavers [8]) one of the two most common lesions to involve the spine. Enostoses of the spine occur most frequently in the thoracic and lumbar vertebral bodies [7]. Usually, they are asymptomatic lesions and discovered incidentally.
Radiographic or computed tomographic (CT) findings are often characteristic, consisting of elongated or circular shape of osteoid matrix lesion with an irregular and spiculated margin surrounded by normal trabecular bone. Vertebral biopsy, although rarely necessary, should be considered if the lesion increases in diameter by more than 25% within 6 months or 50% within 1 year [9].
Bone scintigraphic appearance of enostoses is normal in the majority of the cases; however, uptake in some cases has been observed, especially in cases of long lesions.
On magnetic resonance imaging (MRI), enostoses show markedly low signal intensity on T1-weighted and T2-weighted images with no enhancement after intravenous paramagnetic injection.
Hemangioma
Hemangiomas in the vertebras account for 75% of all osseous hemangiomas [1]. These lesions are multiple in up to 30% of patients, occurring predominately in the lower thoracic and lumbar spine [8, 11]. Usually present in middle-aged individuals, affecting women over men in a 2:1 proportion. Most lesions occur in the vertebral body [12] (Fig. 1), but they may extend into the posterior osseous arc and less frequent into surrounding soft tissue [11] (Fig. 2).
Typical appearance of vertebral hemangioma in the vertebral body and posterior elements of L1 on MR imaging. High signal intensity on T2-weighted (a), T1-weighted (b), and STIR (c) sagittal imaging. The classic “polka-dot” on axial gadolinium-enhanced T1-weighted fat-suppression (d) and axial T2-weighted imaging (e), with paraspinal soft tissue (arrows) and epidural (arrow heads) content
Hemangiomas are usually asymptomatic but sometimes can cause pain secondary to fracture, epidural hemorrhage, or spinal cord compression.
On plain radiographs, vertebral hemangiomas exhibit the characteristic corduroy appearance, with coarsened vertical trabeculae [8]. With CT, the thickened trabeculae appear as radiodense foci, assuming the characteristic “polka-dot” appearance [11].
On MRI, hemangiomas display variable signal intensity on T1-weighted and T2-weighted images, depending on the fatty and vascular components of the lesion [11,12,13] with enhancement after intravenous paramagnetic injection.
Giant Cell Tumor
Giant cell tumor (GCT) is mostly a benign lesion with aggressive characteristics and it may rarely metastasize. Malignant GCTs occur in 5–10% of cases and are usually related to previous irradiation. Spinal GCTs correspond to 7% of all GCTs, representing the fourth most common location, and are more common in women than in men. The majority is located in the sacrum and when in other spinal segments, it typically involves the vertebral body and can extend to posterior elements [2, 5].
Pain and neurologic deficits are the most common symptoms.
Plain radiography shows a destructive lytic lesion, without mineralized matrix. CT imaging reveals a well-defined lytic lesion with soft tissue density, heterogeneous because of necrosis and hemorrhage. MRI shows heterogeneous signal intensity with low signal intensity on T2-weighted images due to fibrous components and hemosiderin. There can also be a low signal intensity pseudocapsule. There is enhancement after intravenous paramagnetic injection.
In the sacrum, lesions are frequently large and extension across the sacroiliac joint is not infrequent. In other spinal locations, the tumor can cause vertebral collapse and extend through the space disk [2, 5].
Complete surgical resection is difficult depending on size and location, requiring radiation therapy. Recurrence rates can reach up to 60% (Fig. 3).
A 32-year-old woman with back pain. CT imaging (a and e) demonstrating osteolytic lesion affecting right pedicle of L4, extending into vertebral body and posterior osseous elements. Note very thin sclerotic rim (arrows) on CT imaging and fat changes (arrow heads) on MR imaging. Sagittal MRI showing low signal intensity on T1-weighted (b) and T2-weighted imaging (c), with gadolinium-enhanced (asterisk) T1-weighted fat-suppression imaging (d). The giant cell tumor was confirmed by biopsy
Aneurysmal Bone Cyst
The term aneurysmal bone cyst (ABC) was first introduced in 142 [14] to describe the radiographic appearance of unicameral bone cysts which contained blood-filled spaces. Most ABCs occur in young individuals, especially under 30 years of age, and there is a mild female predilection. Involvement of spinal segments in the order of decreasing frequency includes the thoracic, lumbar, and cervical spine where the posterior vertebral elements are usually affected [2, 10]. Sacrum involvement is rare [15, 16].
Back pain and neurologic symptoms resulting from encroachment on the spinal canal are frequent [2].
ABCs consist of arteriovenous fistulae and can be primary, with no underlying neoplasm, or secondary to neoplasm [17]. The majority of ABCs are considered primary lesions [17].
Radiographs show a well-defined, radiolucent, and occasionally trabeculated expansile lesion surrounded by a thin sclerotic margin. Soft tissue extension or a compression fracture may be apparent. Scintigraphy frequently demonstrates peripheral increased uptake of radionuclide.
CT confirms the expansile appearance of the lesion and defines soft tissue extension.
On MRI, ABC appears as a lobulated or septated mass surrounded by a thin rim of low signal intensity on both T1-weighted and T2-weighted images, containing multiple fluid–fluid levels indicating hematic content. Although multiple fluid–fluid levels are a typical appearance of ABC, they are not a specific feature [16, 18].
Lesions containing multiple fluid–fluid levels are very suggestive of ABC, particularly if the entire lesion is filled with this type of tissue [19]. After intravenous paramagnetic injection, the septations and rim generally enhance (Figs. 4, 5).
A 13-year-old girl with back pain and lower limb weakness. CT imaging showing expansile osteolytic lesion (arrows) affecting the right side of the posterior elements of T5 and T6 on sagittal bone window (a) and soft tissue window (b), with spinal canal involvement better seen on axial images (d and f). There are areas of heterogeneous high density (arrow heads) on the soft tissue window axial (e and f) consistent, in this case, with hematic content. The diagnosis of aneurysmal bone cyst was confirmed after spinal surgery decompression
A 45-year-old man with back pain and right lower limb paresthesia and weakness. MR imaging demonstrating aggressive mass in the paraspinal soft tissue involving vertebral body (asterisks) and right posterior elements of thoracic vertebras, with spinal canal extension. On T2-weighted imaging (a, b, and e) there are several liquid–liquid levels (arrow heads) anteriorly and more posteriorly a heterogeneous low signal intensity area (arrows) with heterogeneous enhancement (curved arrows) after gadolinium injection on T1-weighted fat-suppression imaging (c, d, and f). Those findings were under suspicion for secondary bone cyst or aneurysmal bone cyst with solid content. The diagnostic of aneurysmal bone cyst with solid areas was proven by pathology
Eosinophilic Granuloma
Eosinophilic granuloma (EG) is the localized form of Langerhans cell histiocytosis. Spinal EG account for up to 15% of all EGs and most lesions affect children between 3 and 12 years, boys being more affected than girls. Most EGs arise in the thoracic spine, affecting primarily vertebral body instead of posterior elements. Clinically EG presents with pain which may be accompanied by infectious symptoms; neurologic deficits have been reported following vertebral compression [32].
Radiographic studies reveal typically a compression fracture of a vertebral body, resulting in wedging and later vertebra plana morphology. In every vertebral compression fracture of a child, EG should be presumed, except in cases of severe spinal trauma.
At CT, lytic destruction of the vertebral body can be appreciated and often is associated with a paravertebral soft tissue mass. On MRI, EG shows low to intermediate signal intensity on T1-weighted and high signal intensity on T2-weighted images. Because of the predominance of red marrow in this population, detection can be limited. However, MRI is more specific in demonstrating soft tissue masses. After contrast administration, there is marked enhancement. Treatment is controversial, ranging from curettage, resection, intratumoral injection of steroids to radiation therapy and immobilization. With healing, a reconstruction of the vertebra occurs and reestablishes an almost normal appearance [32] (Figs. 6, 7).
A 2-year-old boy relating neck pain. Anteroposterior view on plain radiographic (a) and coronal CT imaging (b) showing osteolytic lesion (arrows) affecting right pedicle of C5 with cortical destruction (arrow heads). On axial CT imaging with bone window (c) and soft tissue window (d) demonstrating the pedicle involvement. Eosinophilic granuloma was confirmed by biopsy
Same patient of Fig. 6 demonstrating eosinophilic granuloma involvement in the pedicle of C5 on MR imaging. On axial T2-weighted imaging (a) the lesion (arrow) has intermediate to high signal intensity and on sagittal T1-weighted imaging it exhibits low signal intensity. There is intense enhancement (arrow heads) after gadolinium injection on axial (b) and sagittal (d) T1-weighted fat-suppression imaging
Osteochondromas
Osteochondromas are uncommon in the spine, accounting for <5% of solitary osteochondromas and present in <10% of the patients with hereditary multiple exostoses. There is male predominance and diagnosis is usually made in the 3rd decade for solitary osteochondromas and in the 2nd decade in patients with osteochondromatosis. Osteochondromas can occur in any spine level, but there’s a predilection for the cervical spine, especially C2. Most arise from the posterior elements [2, 32].
Clinically, spinal osteochondromas present mostly with myelopathy.
As in other locations, osteochondromas are composed of normal bone (cortex and marrow space) with a cartilage cap, responsible for the growth of the lesion. The pathologic and radiologic hallmark of this entity is the continuity of the lesion with the marrow and cortex of the underlying bone. They can be sessile or pedunculated.
Radiography can make a definite diagnosis only in the minority of cases. CT is the modality of choice to evaluate the osseous characteristics. Both CT and MRI are able to evaluate the relationship of the lesion to the surrounding soft tissues and encroaching of the spinal canal and intervertebral foramina. At MRI, the lesion is seen with high signal intensity in T1-weighted (normal yellow marrow) marginated by a thin low signal intensity cortex. The cartilage cap exhibits low to intermediate signal intensity on T1-weighted and high signal intensity on T2-weighted. MRI is the best modality to assess the cartilage cap.
Thickening of the cartilage cap larger than 2 cm is suspicious of malignant transformation to chondrosarcoma [2, 32].
Surgical excision is usually curative (must include the entire cartilage cap) and improves the symptomatology in nearly 90% of patients. Recurrence is rare and can occur following incomplete resection (Fig. 8).
Osteoid Osteoma
Osteoid osteoma of the spine is less common than the appendicular skeleton, constituting about 10% of all osteoid osteomas [1, 18]. Osteoid osteoma affects young individuals, generally under 25 years of age, while men are affected two to three times more frequently than women. Most cases of osteoid osteomas in the spine affect the posterior osseous arc [18], accounting for 75% of the cases, while only 7% occurs in the vertebral body [20, 21].
Clinical symptoms include painful scoliosis, gait disturbance, paraspinal muscle atrophy, and focal or radicular pain. Young individuals with painful scoliosis are important and should alert to the possibility of osteoid osteoma in the spine, particularly because idiopathic scoliosis are usually asymptomatic. The pain is characteristically worse at night and usually ameliorated by salicylates or nonsteroidal anti-inflammatory drugs.
On radiographs, osteoma osteoid appears as an oval or rounded osteolytic area less than 2 cm in diameter, representing the nidus, with variable surrounding sclerosis. Central calcification may be present. Bone scintigraphy shows significant radionuclide uptake by the nidus.
CT is particularly useful for detecting the nidus, particularly in small lesions or areas obscured by imaging overlap [16].
On MR images, the best clue for the diagnostic is extensive osseous or surrounding soft tissue edema in young individuals with no evidence of trauma or infection. The nidus has markedly enhanced after intravenous paramagnetic injection, which can be more conspicuous if compared to the MRI before contrast (Fig. 9).
A 9-year-old boy with back pain with left gluteal irritation. Low signal intensity ill-defined area (asterisk) on T1-weighted imaging (a) in the lower aspect of the left sacrum close to the sacroiliac joint. There is a rounded low signal intensity lesion (arrow head) with central high signal intensity on T2-weighted fat-suppression imaging (b) compatible with osteoid osteoma. Note the surrounding peritumoral inflammatory changes (arrows)
Osteoblastoma
It is a rare benign osteoid matrix tumor also known as giant osteoid osteoma and osteogenic fibroma. Spinal osteoblastoma accounts for approximately 40% of all osteoblastoma [10, 23], and occurs with equal distribution in the spinal segments.
Osteoblastoma frequently originates from the posterior osseous arc (85% of lesions) with 42% extending into the vertebral body. Osteoblastomas usually present in young adults between the second and third decades of life. Men are affected two times more than women. They may present with pain, paresthesias, paraparesis, or even paraplegia [24].
Osteoblastoma and osteoid osteoma are variants of the same benign process and histologically indistinguishable from each other. Only the size is used as a differential criterion, in which lesions <2 cm are considered as osteoid osteomas, and lesions >2 cm are classified as osteoblastomas. Malignant transformation to osteosarcoma is rare. Osteoblastomas are more aggressive than osteoid osteomas, with a higher recurrence rate, ranging from 10 to 50% lesions. Spinal osteoblastomas may present with variable radiologic appearances. The first pattern is similar to osteoid osteomas and composed of a radiolucent nidus and surrounding sclerosis. Therefore, the most common appearance of spinal osteoblastoma is an expansile lesion with a prominent sclerotic rim and multiple small calcifications. Multifocal calcifications are present in 55% of cases. Aneurysmal bone cysts are present in 10–15% of cases [25].
Bone scintigraphy reveals marked accumulation of the radionuclide.
Radiography and CT are useful to better appreciate matrix calcification and sclerotic margin; however, MRI effectively delineates the extent of tumor in surrounding soft tissues and the spinal canal. Peritumoral edema in bone marrow and soft tissues, reflecting inflammatory reaction is a characteristic feature. Like osteoid osteoma, osteoblastoma shows marked enhancement after intravenous paramagnetic injection (Figs. 10, 11).
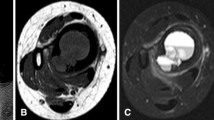
Same patient of the Fig. 10. MR imaging demonstrating expansile lesion affecting right lamina of the T3 vertebra with liquid–liquid level (curved arrows) in sagittal T2-weighted imaging (b), sagittal STIR (D), and axial T2-weighted imaging (h). Note extensive inflammatory changes in the vertebral body (arrow heads), posterior osseous elements (asterisks), and paraspinal soft tissue (arrows); better seen on gadolinium-enhanced T1-weighted fat-suppression imaging (e, f, and i)
Malignant Lesions
Chordoma
Chordoma is the most common nonlymphoproliferative primary malignant neoplasm of the spine in adults. It arises from the embryonic remnants of the notochord that extend from Rathke's pouch to the coccyx. Histologic identification of physaliphorous cells confirms the diagnosis. It commonly affects middle-age individuals and has a peak incidence in the fifth decade. Chordomas are almost exclusively seen in the midline, accounting approximately 50% to the sacrum and 35% to the clivus. Sacral chordomas are most frequently centered in the lower levels. Rarely, chordomas can arise in a paracentral location, in the paraspinal soft tissue, and they are called “parachordoma” [27, 28].
On plain radiographic and CT images, the bone destruction predominates, with intratumoral calcification seen commonly [29]. Paraspinal soft tissues and spinal canal involvement are frequent.
Chordomas show signal characteristics similar to the notochord remnants on MR imaging, characterized by low to intermediate signal on T1-weighted and very high signal on T2-weighted MR images. Contrast enhancement is usually in a thick peripheral nodular and septal pattern. The location and thus resectability of the lesion usually determines the patient’s prognosis, with high rate of recurrence (Figs. 12, 13).
Typical location of chordoma in a 32-year-old woman with buttock pain for several months. CT imaging (a) demonstrating osteolytic aggressive lesion determining sacral and coccyx erosion from S3. Typical appearance of chordoma on MRI, showing low signal intensity on T1-weighted (b), very high signal intensity on T2-weighted fat-suppression (c), and heterogeneous enhancement on T1-weighted fat-suppression imaging (d) after contrast injection, predominantly peripheral nodular (arrows) and septal (arrow heads)
Cervical chordoma in a 57-year-old man with lower limb weakness and right cervicobrachialgia. CT imaging (a, f, and g) showing aggressive osteolytic lesion determining bone destruction of the body and right transverse process of C6 and C7, with spinal canal extension (arrow). On MR imaging, the lesion appearance is typical, with low signal intensity on T1-weighted (b), very high signal intensity on T2-weighted (c, d, h, and i), and heterogeneous enhancement on T1-weighted fat-suppression imaging (e) after contrast injection
Chondrosarcoma
It is the second most common nonlymphoproliferative primary malignant tumor of the spine in adults [4]. The spine represents the primary site in 3–12% of chondrosarcomas [26]. Men are affected two to four times more than women, and the mean age of presentation is 45 years. Although chondrosarcomas can be located at any level, the thoracic segments of the spine are the most commonly affected. These tumors can present as primary chondrosarcomas or as malignant transformation of osteochondromas or enchondromas. Most spinal chondrosarcomas are histologically low-grade lesions and they may be centered in the vertebral body or posterior elements with destruction of these structures.
Mineralized chondroid matrix with typical ring and arc pattern is best visualized on radiographs and CT images [26]. On MR imaging the nonmineralized areas of cartilage typically demonstrate low signal intensity on T1-weighted images and high signal intensity on T2-weighted images and frequently reveal a peripheral nodular and septal enhancement pattern after intravenous paramagnetic injection.
Ewing Sarcoma and Primitive Neuroectodermal Tumor
Ewing sarcoma and Primitive Neuroectodermal Tumor (PNET) are indistinct entities with very similar pathologic, clinical, and radiologic characteristics.
They represent the most common nonlymphoproliferative primary malignant tumors of the spine in children and adolescents.
Lesions affecting the spine account less than 10% of all primary sites of Ewing sarcoma/PNET [26, 30]. Secondary involvement of the spine from other foci of primary Ewing sarcoma/PNET is much more common than primary lesions. The most common location for primary lesions is the sacrococcygeal region, followed by the lumbar and the thoracic spine, with rarely involvement of the cervical spine [30].
Ewing Sarcoma/PNET has various radiologic patterns of presentations most demonstrating bone morphology destruction, lytic lesions, and extensive paraspinal soft tissue components.
On MRI, intermediate signal intensity on T1-weighted and intermediate to high signal intensity on T2-weighted MR images can be seen. Similar to other aggressive malignant osseous tumor, post-contrast images show marked enhancement after intravenous paramagnetic injection, with central areas of necrosis. Surgical resection are often not feasible because of the lesion location and the large size of the soft tissue components [4] (Figs. 14, 15).
A 21-year-old patient with history of progressive back pain for 9 months, just 1 month after the pregnancy diagnosis. Lower limb paresthesia, intestinal constipation, and urinary discharges from 6th month of pregnancy. CT imaging demonstrating aggressive osteolytic lesion in the sacrum with large heterogeneous soft tissue mass extending to the pelvic cavity and exhibiting extensive central areas of necrosis (asterisks). Soft tissue window (a, b, and c) and bone window images (d, e, and f). Uterus (U) enlarged in this case related to post-partum changes. The diagnostic of Ewing sarcoma/PNET was confirmed by immunohistochemistry
Same patient of Fig. 14. MR imaging demonstrating extensive involvement of the sacrum (arrows) with large heterogeneous soft tissue mass extending to the cavity and exhibiting extensive areas of necrosis (asterisks) on T1-weighted fat-suppression imaging (d) after contrast injection. T2-weighted fat-suppression imaging (a, b, and c). Uterus (U) enlarged in this case related to post-partum changes
Osteosarcoma
Osteosarcoma of the spine is rare, representing less than 3% of all osteosarcomas and 5% of all primary malignant tumors of the spine [31]. Osteosarcomas of the spine occur at an older age than those with appendicular lesions [10], affecting more men than women. Spinal osteosarcomas may be associated with Paget’s disease or previous irradiation [22]. The lumbosacral spine is the site of involvement in 60–70% of the cases. Tumors most typically arise from the vertebral body. These individuals often present with pain and a palpable mass, and 70–80% have neurologic symptoms ranging from sensory deficits to paresis [31]. Radiographs and CT images reveal a predominantly osteosclerotic, mixed, or purely osteolytic lesion with extensive osseous destruction [22], that may extend to the epidural space and paraspinal region. The MR imaging appearance of spinal osteosarcoma is nonspecific, with destructive osseous morphology and heterogeneous signal intensity on T1- and T2-weighted image. Heterogeneous enhancement is seen after intravenous paramagnetic agent injection, extending to soft tissue or to the spinal canal (Figs. 16, 17).
A 20-year-old woman with abdominal pain and intestinal constipation for two weeks. On CT imaging, bone window (a, b, and c) and soft tissue window (d, e, and f) demonstrating aggressive osteolytic lesion (arrows) determine the extensive erosion of the sacrum. There is a large soft tissue mass (arrow heads) invading sacral foramen and sacral roots. Note central areas of necrosis (asterisks). The osteosarcoma diagnosis was made by pathology
Same patient of Fig. 16. MR imaging demonstrating extensive erosion of the sacrum and large heterogeneous soft tissue mass with central areas of necrosis (arrow heads) on T1-weighted fat-suppression imaging (e and f) after contrast injection. T1-weighted (a and b) and T2-weighted fat-suppression imaging (c and d)
Conclusion
Spinal tumors are frequently detected on imaging studies performed for several indications. We have reviewed some of the imaging features of common spinal tumors in this article and summarize them in Tables 1 and 2. Multiple spinal lesions are suspicious for metastatic disease and lymphoproliferative malignant disease and combine with history and clinical manifestations, thus often don’t leave any doubt about the diagnosis. However, solitary lesions of the spine can be challenging, and primary neoplasms should be considered. Radiologists should be aware of imaging features to help suggest a specific diagnosis or conduct the indicated cases to biopsy. CT or MR imaging is indispensable to determine the extension and the relationship with the spinal canal structures, thus planning the optimal management.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Llauger J, Palmer J, Amores S, Bague S, Camins A. Primary tumors of the sacrum: diagnostic imaging. AJR Am J Roentgenol. 2000;174:417–24.
• Murphey M, Andrews C, Flemming D, Temple T, Smith S, Smirniotopoulos J. Primary tumors of the spine. Radiographics. 1996;16:1131–58. This article correlates radiologic and pathologic features of benign and malignant tumors of the spine with several cases, gross, and microscopic images.
Smith J, Wixon D, Watson RC. Giant-cell tumor of the sacrum. Clinical and radiologic features in 13 patients. J Can Assoc Radiol. 1979;30(1):34–9.
•• Orguc S, Remide A. Primary tumors of the spine. Semin Musculoskelet Radiol. 2014;18:280–99.This article describes in an extremely organized and didactic form many cases of primary bone tumors of the spine with high-resolution images.
Theodorou D, Theodorou S, Sartoris D. An imaging overview of primary tumors of the spine: part 1: benign tumors. Clin Imaging. 2008;32:196–203.
Stieda A. Uber umschriebene knochen verdichtungen in lerech der substantia spongiosa in rontgenbilde. Bruns Beitr Klin Chir Tubing. 1905;45:700–3.
Resnick D, Nemcek AA, Haghighi F. Spinal enostoses (bone islands). Radiology. 1983;147:373–6.
Murphey MD, Fairbairn KJ, Parman LM, Baxter KG, Parsa MB, Smith WS. Muscuboskeletal angiomatous lesions: radiologic-pathologic correlation. RadioGraphics. 1995;15:893–917.
Greenspan A, Steiner G, Knutzon R. Bone island (enostosis): clinical significance and radiologic and pathologic correlations. Skelet Radiol. 1991;20:85–90.
Motamedi K, Ilaslan H, Seeger L. Imaging of the lumbar spine neoplasms. Semin Ultrasound CT MRI. 2004;25:474–89.
Wenger D, Wold L. Benign vascular lesions of bone: radiologic and pathologic features. Skelet Radiol. 2000;29:63–74.
Vilanova J, Barcelo J, Smirniotopoulos J, Perez-Andres R, Villalon M, Miro J, Martin F, Capellades J, Ros P. Hemangioma fromhead to toe: MR imaging with pathologic correlation. Radiographics. 2004;24:367–85.
Baudrez V, Galant C, Vande Berg B. Benign vertebral hemangioma: MR–histological correlation. Skelet Radiol. 2001;30:442–6.
Jaffe HL, Lichtenstein L. Solitary unicameral bone cyst with emphasis on the roentgen picture, the pathologic appearance, and the pathogenesis. Arch Surg. 1942;44:1004–25.
Capanna R, Van Horn J, Biagini R, Ruggieri P. Aneurysmal bone cyst of the sacrum. Skelet Radiol. 1989;18:109–13.
Diel J, Ortiz O, Losada R, Price D, Hayt M, Katz D. The sacrum: pathologic spectrum, multimodality imaging, and subspecialty approach. Radiographics. 2001;21:83–104.
Kransdorf MJ, Sweet DE. Aneurysmal bone cyst: concept, controversy, clinical presentation, and imaging. AJR. 1995;164(573–580):42.
Faingold R, Saigal G, Azouz EM, Morales A, Albuquerque P. Imaging of low back pain in children and adolescents. Semin Ultrasound CT MRI. 2004;25:490–505.
Tsai JC, Dalinka MK, Falbon MD, Zbatkin MB, Kressel HY. Fluid-fluid level: a nonspecific finding in tumors of bone and soft tissue. Radiology. 1990;175(3):779–82.
Azouz EM, Kozbowski K, Marton D, Sprague P, Zerhouni A, Asselah F. Osteoid osteoma and osteoblastoma of the spine in children: report of 22 cases with brief literature review. Pediatr Radiol. 1986;16:25–31.
Swank SM, Barnes RA. Osteoid osteoma in a vertebral body: case report. Spine. 1987;12:602–5.
Patel D, Hammer R, Levin B, Fisher M. Primary osteogenic sarcoma of the spine. Skelet Radiol. 1984;12:276–9.
Shaikh M, Saiffudin A, Pringle J, Natali C, Sherazi Z. Spinal osteoblastoma: CT and MR imaging with pathological correlation. Skelet Radiol. 1999;28:33–40.
Kroon HM, Schurmans J. Osteoblastoma: clinical and radiologic findings in 98 new cases. Radiology. 1990;175(3):783–90.
McLeod RA, Dahlin DC, Beabout JW. The spectrum of osteoblastoma. AJR Am J Roentgenol. 1976;126(2):321–5.
Flemming DJ, Murphey MD, Carmichael BB, Bernard SA. Primary tumors of the spine. Semin Musculoskelet Radiol. 2000;4(3):299–320.
Sung MS, Lee GK, Kang HS, et al. Sacrococcygeal chordoma: MR imaging in 30 patients. Skelet Radiol. 2005;34(2):87–94.
Rosenthal DI, Scott JA, Mankin HJ, Wismer GL, Brady TJ. Sacrococcygeal chordoma: magnetic resonance imaging and computed tomography. AJR Am J Roentgenol. 1985;145(1):143–7.
de Bruïne FT, Kroon HM. Spinal chordoma: radiologic features in 14 cases. AJR Am J Roentgenol. 1988;150(4):861–3.
Ilaslan H, Sundaram M, Unni KK, Dekutoski MB. Primary Ewing’s sarcoma of the vertebral column. Skelet Radiol. 2004;33(9):506–13.
Barwick KW, Huvos AG, Smith J. Primary osteogenic sarcoma of the vertebral column: a clinicopathobogic correlation of ten patients. Cancer. 1980;46:595–604.
Erlemann R. Imaging and differential diagnosis of primary bone tumors and tumor-like lesions of the spine. Eur J Radiol. 2006;58(1):48–67.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Diego Avila Lessa Garcia, Laís Uyeda Aivazoglou, Lucas Avila Lessa Garcia, Fernando Bernardes Maia Diniz Ferreira, Sabrina Mendes França, and Artur da Rocha Corrêa Fernandes each declare no potential conflicts of interest. Julio Brandão Guimarães is a section editor for Current Radiology Reports.
Research Involving Human and Animal Rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Musculoskeletal Imaging.
Rights and permissions
About this article
Cite this article
Garcia, D.A.L., Aivazoglou, L.U., Garcia, L.A.L. et al. Diagnostic Imaging of Primary Bone Tumors of the Spine. Curr Radiol Rep 5, 30 (2017). https://doi.org/10.1007/s40134-017-0220-1
Published:
DOI: https://doi.org/10.1007/s40134-017-0220-1