Abstract
Purpose of Review
This article reviews recent updates in the imaging for diagnosis and characterization of upper extremity nerve entrapments (UENE). We examine in detail the use of ultrasound and MRI, including state-of-the-art techniques such as dynamic nerve motion assessment, tissue elasticity measurement, and MR neurography.
Recent Findings
Ultrasound and MRI are the two advanced modalities most frequently used to assess UENE. MRI remains technically challenging, though techniques of MR neurography have steadily improved. Ultrasound is operator-dependent, but has dynamic and realtime imaging capabilities and no contraindications. New comparative techniques of measurement and elasticity assessment show promise for improved diagnostic accuracy.
Summary
Up-to-date imaging techniques for peripheral nerves in the upper extremity from the shoulder to the hand are discussed, with a focus on the most common UENE such as carpal tunnel syndrome and cubital tunnel syndromes. Technical challenges and limitations are reviewed, with a focus on the current and future state of imaging for UENE.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Upper extremity entrapment neuropathies (UENE) are a relatively common cause of peripheral nerve pain, typically caused by mechanical or repetitive impingement of a nerve within a tight anatomic space or fibrous tunnel [1]. There are many UENE which can involve peripheral nerves ranging from the brachial plexus to small distal branches of the radial, median, and ulnar nerves, and can be categorized by affected nerve(s), the location of the entrapment or compression, and the typical clinical presentation, summarized in Table 1.
Various mechanisms of injury have been proposed to explain the pathophysiology of UENE, a detailed discussion of which is beyond the scope of this review [2–4]. In general, the symptoms of UENE typically include pain or paresthesias in the distribution of the involved nerve. In chronic or severe cases, there can be more severe morbidity including weakness, motor dysfunction, and muscle atrophy [1, 5]. Clinical examination, supplemented with electrodiagnostic testing (electromyography, nerve conduction studies) when necessary, is the most common initial approach to UENE evaluation, although diagnosis is often inconclusive [2, 6]. In these cases, imaging is the next step in the diagnostic pathway.
The goals of imaging in the workup of UENE are to detect and localize abnormal changes in nerves to help stage the degree of nerve injury and to exclude more significant motor neuron disease [7•, 8]. Even in routine cases, imaging can offer a useful complement to physical exam and electrodiagnostic studies [9]. Imaging can also be useful to reveal space-occupying lesions, such as cystic or solid masses or other abnormalities, that may compress the involved nerve [7•, 10].
This article will describe the current state of diagnostic imaging for the assessment and characterization of UENE, and review associated new and emerging techniques. The first section on diagnostic technique focuses on a detailed description of the strengths and weakness of the imaging modalities themselves, while the second section assesses more detailed evaluations of specific nerve entrapments and anatomic areas of interest within the upper extremity.
Diagnostic Techniques
Radiographs
X-rays have a relatively limited role in evaluation of UENE, though they do have utility in the setting of acute trauma and to delineate possible aberrant osseous anatomy, such as a supracondylar process or osteochondroma [11, 12].
Magnetic Resonance Imaging (MRI)
MRI provides excellent contrast resolution and soft tissue detail, especially on newer high field strength scanners and modern receiver coils that allow acquisition of higher spatial resolution while preserving signal-to-noise ratio [13]. Although there is some variability in the literature regarding the overall accuracy of MRI, certain findings such as nerve contour or caliber changes and T2 or STIR signal hyperintensity can directly relate to nerve pathology [14, 15]. Muscle edema or fatty atrophy due to denervation can also be visualized, though this is typically a late finding in peripheral neuropathies [10]. Mapping these areas of denervation edema can be extremely useful in characterizing entrapment neuropathies, especially when the nerve or site of impingement cannot otherwise be visualized [16•]. Gadolinium-based contrast is not typically required for nerve imaging; however, some studies have reported the utility of dynamic contrast-enhanced examinations. In the postoperative setting, when there is concern for re-entrapment, abnormal nerve enhancement has been correlated with abnormal findings on EMG [17].
Limitations of MRI include its generally high cost and study length. Field of view may be restricted by coil selection, permitting only partial visualization of peripheral nerves. MRI also has limited capability for dynamic imaging, which can lead to difficulty in diagnosing intermittent or positional UENE.
Recent developments in MR imaging primarily include advancements in MR neurographic (MRN) imaging techniques [13, 18•–20]. While MRN has historically been used to evaluate large nerve groups such as the sciatic nerve and brachial plexus, wider availability of 3T scanners, as well as improved receiver coils and parallel imaging techniques, have made MRN more practical for peripheral nerves [13, 18•]. Most MRN protocols are based on high-resolution axial 2D images, including both non-fat-suppressed T1 W and fat-suppressed T2 W imaging to depict anatomy and pathology, respectively [21•]. 3D T2 W sequences, yielding isotropic high spatial resolution as well as T2 contrast, are useful for longitudinal depiction of nerves and also allow for additional reconstruction techniques, which can improve visualization and demonstration of nerve abnormalities [20, 21•].
Alternate methods of MRN are based on diffusion weighted imaging (DWI), which offers benefits including increased nerve conspicuity, suppression of vascular signals, and quantitative measurements [13]. However, DWI-based MRN can be technically challenging, with limited SNR and spatial resolution [13, 19]. Diffusion tensor imaging (DTI) is also based on DWI, and can be used to characterize changes along nerve bundles and axons, analyzing the directional diffusion of free water protons and the differences in diffusivity when parallel or perpendicular to nerve fibers [20, 22]. To date, DTI has primarily been used in the central nervous system, but is starting to be explored as a tool for peripheral nerve evaluation; DTI shows promise as a biomarker for axonal and myelin sheath integrity and for its ability to potentially assess nerve regeneration after injury [18•–20, 23]. Lastly, a new sequence called diffusion weighted reversed fast imaging with steady-state free precession (DW-PSIF) combines elements of both T2 W and DWI and has been described as having benefits in peripheral MRN because it can selectively suppress fluid signal and vascular flow [24]. Especially when examining small nerves in the distal extremities, DW-PSIF may offer benefits over T2 W techniques as it can selectively suppress subcutaneous edema [25].
Ultrasound
Sonography, particularly with newer high-resolution transducers operating with frequency up to 18 MHz or higher can readily demonstrate nerve architecture and anatomy. In many cases, sonographic resolution is higher than MRI and can highlight characteristic enlargement and abnormal echogenicity within nerves. With improving spatial resolution, enlargement of individual nerve fascicles may also be evident, with caliber changes or abrupt tapering of the nerve proximal to the level of entrapment. Advantages of ultrasound include its relatively low cost and dynamic capabilities, which may demonstrate nerve compression or entrapment with real-time patient motion [26]. Interrogating the contralateral side can also provide a useful internal comparison or control. Color and power Doppler techniques can be used to evaluate for vascular flow and hyperemia that may be present in UENE, either within or around nerves [27]. When appropriate, ultrasound may be used to guide diagnostic or therapeutic injections to targeted areas of entrapment, and has also shown promise for intraoperative guidance [28].
Some limitations of ultrasound include difficulty penetrating into deeper tissues or through significant body habitus. Calcifications, skin changes, or other soft tissue abnormalities may inhibit acoustic transmission and interfere with imaging. Musculoskeletal ultrasound also remains relatively specialized and operator dependent, and depending on local practice patterns, may not be available at all institutions.
Advances in ultrasound include the increased use of dynamic methods to assess nerve motion, as well as comparative methods that examine for changes in size between different anatomic locations [29, 30•, 31–33]. Dynamic methods can demonstrate subluxation of the ulnar nerve over the medial epicondyle with elbow flexion/extension, which may contribute to ulnar neuropathy, and can also visualize reduced median nerve motion within the carpal tunnel [34, 35]. This has been postulated to occur as a result of abnormal changes in the subsynovial connective tissue, and similar perineural changes have also been observed [35, 36]. Comparative methods, either assessing differences in nerve architecture between two anatomic landmarks, or to the contralateral side, have shown increased accuracy compared to standard measurement techniques [30•, 32, 33].
Various sonoelastography techniques can non-invasively measure tissue stiffness and elasticity and have also shown promise for evaluating certain UENE [37•–39]. The two most commonly used elastography techniques in clinical practice are strain (compression) elastography and shear wave elastography (SWE), which have seen a variety of applications in musculoskeletal ultrasound, though somewhat less commonly for nerve entrapments [39]. Both techniques have shown some promise for evaluating the median nerve in carpal tunnel syndrome [40, 41]. However, elastography is not yet widely available in clinical scanners, and questions about standardization of the interpretation and display of data and the reproducibility and reliability of the technique have yet to be answered [39]. Strain elastography, in particular, relies on repeated manual compressions, which can be unreliable and technically challenging [39].
Specific UENE
Shoulder and Upper Arm
In the shoulder and upper arm, the most commonly encountered nerve entrapments involve the axillary nerve, the suprascapular nerve, and the brachial plexus, with the long thoracic and spinal accessory nerves more rarely affected [42]. More distally in the upper arm, the radial nerve can be entrapped at the level of the spiral groove [43].
MRI has generally been the modality of choice for evaluating UENE in these areas, both for direct nerve evaluation and for characterizing patterns of muscle edema that may relate to specific locations of nerve entrapment [8, 42, 44–46•]. Characteristic patterns of muscle edema related to nerve entrapments at the quadrilateral space and suprascapular/spinoglenoid notches are well described on shoulder MRI [24]. MRI and MRN evaluation of the brachial plexus has been available for many years, and steady improvements in technology have allowed for better visualization and detail of the brachial plexus [13, 42, 47]. MRN brachial plexus protocols typically rely on high-resolution fast spin echo (FSE) T1-weighted images for assessing anatomic detail and STIR or FSE T2-weighted images for assessing nerve pathology [13, 42, 47]. In particular, use of a sagittal STIR sequence allows for comparison of dorsal nerve roots at multiple levels, and isotropic 3D sequences can be used to generate longitudinal images of the nerves in the brachial plexus or to create MIP images to emphasize abnormalities [13]. DWI- and DTI-based techniques can also be applied, and have shown some potential use in the setting of neurogenic thoracic outlet syndrome, though they should not replace standard anatomic MRN sequences [20, 47]. DTI remains technically challenging for peripheral nerve evaluation, though a recent report did show success demonstrating radial nerve signal changes in acute compression at the spiral groove [48].
Ultrasound of the brachial plexus can be performed based on anatomic landmarks, from both a cervical and axillary approach [42]. Sonography has been used for many years to guide procedures, such as regional injections for anesthesia, and similar procedures have been described as therapeutic for neurogenic thoracic outlet syndrome [47, 49, 50]. Although there have been few recent developments regarding the use of ultrasound in these areas, the use of three-dimensional ultrasound to acquire a spatial map of the brachial plexus has been previously described and may have implications for procedural planning as 3D and 4D ultrasound further develops [51].
Elbow and Forearm
In the elbow and forearm, the nerves prone to entrapment include the ulnar nerve, the radial nerve, and its deep branch which becomes the posterior interosseous nerve, and the median nerve and its branch, the anterior interosseous nerve (AIN).
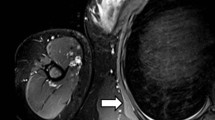
MRI/MRN and ultrasound are both useful for ulnar nerve evaluation, especially at the cubital tunnel, which is the second most common site of nerve entrapment in the upper extremity [24]. Direct findings of ulnar nerve injury can be seen with both MR and ultrasound imaging, including abnormal nerve signal/echotexture, edematous or enlarged fascicles, and nerve displacement and/or angulation. MRN also has utility assessing re-entrapment after surgical transposition [24]. Although MRI is the most commonly employed imaging tool in the diagnosis of ulnar nerve entrapment, there are specific limitations at the elbow related to patient positioning. Since the elbow typically must be scanned in extension in order to fit within cylindrical extremity coils, dynamic compression of the ulnar nerve due to dislocation over the medial epicondyle or snapping triceps will not be well visualized [10, 34].
In contrast, ultrasound provides a dynamic field of view through which the nerve can be traced along its entire course and in various anatomic positions [32, 34]. Typical ultrasound appearance of ulnar nerve entrapment in this area, i.e., “cubital tunnel syndrome” are shown in Fig. 3. Dynamic evaluation is also useful to demonstrate subluxation or dislocation of the ulnar nerve over the medial epicondyle, as seen in Fig. 4 [34]. Ultrasound has also shown nerve enlargement in ulnar neuropathy compared with control subjects; some authors advocate comparison with the patient’s contralateral asymptomatic nerve, while others advocate comparison using a ratio of the cross-sectional area at the location of maximal nerve swelling relative to the cross-sectional area at a non-swollen location [10]. A recent study of 25 patients found that cross-sectional area measurements were significantly different between patients with ulnar nerve entrapment and healthy controls [32].
Although less common than ulnar nerve entrapment, there are multiple additional sites of potential nerve entrapments at the elbow. The most common include the posterior interosseous nerve as it passes through the arcade of Frohse (PIN syndrome), the median nerve as it passes between the two heads of the pronator teres muscle (pronator syndrome), and AIN syndrome, which has myriad causes [10].
MRN findings in these entities also include direct signal changes within the affected nerve at the area of entrapment, as well as regional muscle denervation changes in the forearm [24]. Sonography may reveal similar changes characterized by hypoechoic edematous nerves, as well as hyperemia of the nerve on color Doppler imaging [10]. While ultrasound currently has advantages in terms of resolution for evaluating small peripheral nerve branches, identification of the normal AIN may be difficult because of the deep location and small size of the nerve [52]. Technological advances may allow MRN to increase its diagnostic role in the future [24].
Hand and Wrist
Compression of the median nerve at the carpal tunnel (carpal tunnel syndrome) is the most common and well recognized peripheral entrapment neuropathy [1, 24, 53•]. Distal branches of the ulnar nerve and superficial radial nerve can also be compressed at the wrist.
MRI may show anatomic changes, such as signal and caliber or contour changes, in the median nerve at the wrist [5]. As in other areas of the upper extremity, MRI has utility in excluding and/or characterizing an extrinsic mass at the wrist. There has been increasing interest in using MRN and in particular, DTI to evaluate the median nerve at the carpal tunnel, though this continues to be technically challenging and inter-subject variation remains high [23, 54].
The median nerve in the carpal tunnel is well evaluated with ultrasound and objective diagnostic criteria based on nerve cross-sectional area and other sonographic features have been established (Fig. 1). Overall, ultrasound is considered an accurate modality for diagnosis of carpal tunnel syndrome, with a sensitivity and specificity of 87 and 83 %, respectively, characterized in a recent meta-analysis [55]. Normal median nerve cross-sectional area typically measures 0.08–0.11 cm2 at the carpal tunnel, with increased cross-sectional area, as well as changes in longitudinal displacement of the median nerve in the carpal tunnel correlating with clinical symptoms of carpal tunnel syndrome [26]. Change in cross-sectional area measured between the median nerve at the level of the pronator quadratus and at the level of the carpal tunnel has shown promise as a sensitive and specific technique for assessing median neuropathy, demonstrated in (Fig. 2) [30•]. Calculations involving the ratio and difference between median nerve measurements in these two locations have also been recently shown to have utility in predicting CTS severity, compared to nerve conduction studies [33] (Figs. 3, 4).
A 44-year-old female with symptoms of carpal tunnel syndrome in the right wrist. a Transverse sonographic image of the median nerve at the level of the carpal tunnel shows abnormal hypoechoic echotexture, with loss of normal nerve “honeycomb” architecture. When best-fit ellipse (b) is drawn around the nerve at the same level, cross-sectional area can be measured to give a quantitative assessment of median neuropathy
A 57-year-old female with clinical concern for carpal tunnel syndrome. Transverse sonographic image demonstrates technique for localizing the median nerve proximal to the wrist, at the level of the middle third of the pronator quadratus (Pro Q). The pronator quadratus can be identified in the distal forearm by recognizing muscle fibers running perpendicular to the long axis of the arm. Comparative measurements between the median nerve in this location, and the carpal tunnel, have been shown to increase diagnostic sensitivity [30•, 33]
A 67-year-old male with clinical symptoms and EMG findings of ulnar neuropathy. a Transverse sonographic image demonstrates ulnar nerve enlargement and abnormal hypoechoic echotexture and loss of normal fascicular architecture at the level of the cubital tunnel (arrows). Adjacent landmarks include the medial epicondyle (Me), and the tip of the olecranon (Ol). b best-fit ellipse drawn around the nerve confirms marked enlargement, with cross-sectional area measuring 0.35 cm2
Ulnar nerve dislocation at the level of the elbow in a 44-year-old female with posterior right elbow pain. Static images starting from (a) extension and moving to (b) flexion demonstrate abnormal displacement of the ulnar nerve (arrows) medially over the medial epicondyle (Me). Although this finding can be present in asymptomatic population, it should be recognized and reported. It should also be distinguished from snapping triceps syndrome, in which the medial head of the triceps also moves abnormally with the ulnar nerve over the medial epicondyle [34]
Newer technologies involving sonoelastography techniques appear to show some promise for improving the ultrasound assessment of carpal tunnel syndrome, especially in early or subclinical cases where the median nerve may not yet show caliber or contour changes. Reports of success using both the strain-compression and SWE methods have been described [37•, 40]. Shear wave elastography technique may have more clinical applicability since it does not require as careful a manual compression technique [37•, 40]. Nevertheless, some questions about repeatability and reliability for these techniques still exist, and there remains no good reference standard for median nerve stiffness.
Other nerve entrapments at the wrist are relatively rare, but include ulnar nerve compression at Guyon’s canal (ulnar tunnel syndrome, cyclist’s palsy) and compression of the superficial radial nerve (Wartenberg’s syndrome). In general, imaging of these small peripheral nerve branches can be difficult due to their small size, lack of objective values for normal reference, and other conditions which may mimic the diagnosis [32, 56]. Diagnosis is typically clinical, but can be confirmed with ultrasound, as the superficial locations of these nerves does allow good US visualization [52, 57]. Ultrasound has intrinsically high spatial resolution and, with small footprint high-resolution (e.g., “hockey stick”) transducers, is easily adapted to imaging peripheral anatomy, such as the hand and wrist. Extrinsic masses, such as the commonly encountered ganglion cyst, are easily demonstrated and characterized. The dynamic capabilities of ultrasound can be useful in assessment of abnormal motion or entrapment of small peripheral nerves, and the contralateral side is readily available for comparison. While secondary changes may be absent or difficult to visualize, ultrasound has been described as being able to see focal areas of nerve thickening in the setting of Wartenberg’s syndrome [57].
MRI can be helpful to assess adjacent structures, exclude osseous or soft tissue mass, and can provide indirect evidence for compression if there is regional edema in a nerve distribution [44]. However, performing good-quality MRI and especially MRN of these small distal peripheral nerves is not easy. Even with high field strength, good receiver coils, and parallel imaging techniques, MRI acquisition with a small enough field of view, high enough resolution, and adequate SNR can be quite challenging [18•]. MRI or MRN findings in Wartenberg syndrome, to our knowledge, have not been reported, and given the purely sensory function of the superficial radial nerve, indirect signs of compression (i.e., muscle edema or atrophy) would not be expected to be seen on MRI [57, 58].
Conclusions
Upper extremity nerve entrapments represent a diverse group of syndromes, many of which are quite common and should be routinely encountered in clinical practice. Clinical examination remains integral to the workup and diagnosis, with imaging playing an important complementary role, especially when the presentation is complicated or the diagnosis is uncertain. Ultrasound and MRI continue to be the primary diagnostic tools for investigating UENE. Depending on operator comfort and experience, US and MRI are generally interchangeable as diagnostic tools, although there are advantages and disadvantages to each in certain areas. Regardless of modality, detailed anatomic knowledge is key to optimally planning and performing these studies, and is crucial to recognizing and delineating relevant nerve compression and secondary pathophysiology.
New technological developments in ultrasound and MRI show promise for improving diagnostic ease and accuracy. Improvements in both modalities have allowed for steadily improving spatial resolution, permitting imaging of smaller and more peripheral areas of interest, essential for accurately depicting the anatomy and pathophysiology of peripheral nerve entrapments. Novel techniques such as ultrasound elastography and DTI offer the potential to reveal more physiologic information about peripheral neuropathy. There is much work yet to be done, but continued investigation, development, and refinement of these and other techniques should lead to further standardization and more widespread acceptance of imaging techniques in the workup and diagnosis of upper extremity nerve entrapments.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Bayramoglu M. Entrapment neuropathies of the upper extremity. Neuroanatomy. 2004;3:18–24.
Keith MW, Masear V, Chung KC, Amadio PC, Andary M, Barth RW, et al. American Academy of Orthopaedic Surgeons clinical practice guideline on the treatment of carpal tunnel syndrome. J Bone Joint Surg Am. 2010;92:218–9.
Seddon HJ. Three types of nerve injury. Brain. 1943;66:237–88.
Rempel D, Dahlin L, Lundborg G. Pathophysiology of nerve compression syndromes: response of peripheral nerves to loading. J Bone Joint Surg Am. 1999;81:1600–10.
Beltran J, Rosenberg ZS. Diagnosis of compressive and entrapment neuropathies of the upper extremity: value of MR imaging. AJR Am J Roentgenol. 1994;163:525–31.
Neal S, Fields KB. Peripheral nerve entrapment and injury in the upper extremity. Am Fam Physician. 2010;81:147–55.
• Tang DT, Barbour JR, Davidge KM, Yee A, Mackinnon SE. Nerve entrapment: update. Plast Reconstr Surg. 2015;135:199e–215e. Review of nerve entrapment syndromes including pathophysiology, clinical examination findings, and diagnostic tests; also reviews surgical candidate selection criteria and common surgical techniques.
Dong Q, Jacobson JA, Jamadar DA, Gandikota G, Brandon C, Morag Y, et al. Entrapment neuropathies in the upper and lower limbs: anatomy and MRI features. Radiol Res Pract. 2012;2012:1–12.
Padua L, Liotta G, Di Pasquale A, Granata G, Pazzaglia C, Caliandro P, et al. Contribution of ultrasound in the assessment of nerve diseases: ultrasound and nerve diseases. Eur J Neurol. 2012;19:47–54.
Miller TT, Reinus WR. Nerve entrapment syndromes of the elbow, forearm, and wrist. Am J Roentgenol. 2010;195:585–94.
Opanova MI, Atkinson RE. Supracondylar process syndrome: case report and literature review. J Hand Surg. 2014;39:1130–5.
Dang AC, Rodner CM. Unusual compression neuropathies of the forearm, part I: radial nerve. J Hand Surg. 2009;34:1906–14.
Chhabra A, Lee PP, Bizzell C, Soldatos T. 3 Tesla MR neurography—technique, interpretation, and pitfalls. Skelet Radiol. 2011;40:1249–60.
Kwee RM, Chhabra A, Wang KC, Marker DR, Carrino JA. Accuracy of MRI in diagnosing peripheral nerve disease: a systematic review of the literature. Am J Roentgenol. 2014;203:1303–9.
Hof JJ, Kliot M, Slimp J, Haynor DR. What’s new in MRI of peripheral nerve entrapment? Neurosurg Clin N Am. 2008;19:583–95.
• Kim S-J, Hong SH, Jun WS, Choi J-Y, Myung JS, Jacobson JA, et al. MR imaging mapping of skeletal muscle denervation in entrapment and compressive neuropathies. RadioGraphics. 2011;31:319–32. Comprehensive overview of the various patterns of muscle edema that can be seen in entrapment neuropathies. Includes both upper and lower extremity examples.
Campagna R, Pessis E, Feydy A, Guerini H, Le Viet D, Corlobé P, et al. MRI assessment of recurrent carpal tunnel syndrome after open surgical release of the median nerve. Am J Roentgenol. 2009;193:644–50.
• Chalian M, Behzadi AH, Williams EH, Shores JT, Chhabra A. High-resolution magnetic resonance neurography in upper extremity neuropathy. Neuroimaging Clin N Am. 2014;24:109–25. Review focused on the use of MRN in upper extremity peripheral nerves. Presents an image-based guide to the most common upper extremity entrapment neuropathies, focused on the clinical abnormalities and imaging findings evident using MRN technique.
Chhabra A. Peripheral MR neurography. Neuroimaging Clin N Am. 2014;24:79–89.
Eppenberger P, Andreisek G, Chhabra A. Magnetic resonance neurography. Neuroimaging Clin N Am. 2014;24:245–56.
• Chhabra A, Flammang A, Padua A, Carrino JA, Andreisek G. Magnetic resonance neurography. Neuroimaging Clin N Am. 2014;24:67–78. Practical and up to date review of the technical details and specifics of MR neurography sequences and protocols. Includes discussion of 2D imaging, 3D imaging, more advanced tools and specific guidelines for how to apply MRN to various body parts.
Heckel A, Weiler M, Xia A, Ruetters M, Pham M, Bendszus M, et al. Peripheral nerve diffusion tensor imaging: assessment of axon and myelin sheath integrity. PLoS One. 2015;10:e0130833.
Hiltunen J, Kirveskari E, Numminen J, Lindfors N, Göransson H, Hari R. Pre- and post-operative diffusion tensor imaging of the median nerve in carpal tunnel syndrome. Eur Radiol. 2012;22:1310–9.
Subhawong TK, Wang KC, Thawait SK, Williams EH, Hashemi SS, Machado AJ, et al. High resolution imaging of tunnels by magnetic resonance neurography. Skeletal Radiol. 2012;41:15–31.
Chhabra A, Subhawong TK, Bizzell C, Flammang A, Soldatos T. 3T MR neurography using three-dimensional diffusion-weighted PSIF: technical issues and advantages. Skeletal Radiol. 2011;40:1355–60.
Filius A, Scheltens M, Bosch HG, van Doorn PA, Stam HJ, Hovius SER, et al. Multidimensional ultrasound imaging of the wrist: changes of shape and displacement of the median nerve and tendons in carpal tunnel syndrome: changed biomechanics in CTS. J Orthop Res. 2015;33:1332–40.
Mallouhi A, Pültzl P, Trieb T, Piza H, Bodner G. Predictors of carpal tunnel syndrome: accuracy of gray-scale and color Doppler sonography. Am J Roentgenol. 2006;186:1240–5.
Lee FC, Singh H, Nazarian LN, Ratliff JK. High-resolution ultrasonography in the diagnosis and intraoperative management of peripheral nerve lesions: clinical article. J Neurosurg. 2011;114:206–11.
van Doesburg MHM, Yoshii Y, Villarraga HR, Henderson J, Cha SS, An K-N, et al. Median nerve deformation and displacement in the carpal tunnel during index finger and thumb motion. J Orthop Res. 2010;28:1387–90.
• Klauser AS, Halpern EJ, De Zordo T, Feuchtner GM, Arora R, Gruber J, et al. Carpal tunnel syndrome assessment with US: value of additional cross-sectional area measurements of the median nerve in patients versus healthy volunteers 1. Radiology. 2009;250:171–7. Case-control study examined technique of “delta-CSA” by acquiring comparative measurements of the median nerve in the carpal tunnel and at the level of the pronator quadratus muscle. Results indicate improved accuracy in the diagnosis of CTS.
van Doesburg MHM, Henderson J, van der Molen ABM, An K-N, Amadio PC. Transverse plane tendon and median nerve motion in the carpal tunnel: ultrasound comparison of carpal tunnel syndrome patients and healthy volunteers. PLoS One. 2012;7:e37081.
Roodt T, Van Dyk B, Jacobs S. Ultrasound diagnosis of ulnar nerve entrapment by confirming baseline cross-sectional area measurement for normal and abnormal nerves. S Afr J Radiol. 2015;19. http://www.sajr.org.za/index.php/sajr/article/view/747.
Klauser AS, Abd Ellah MMH, Halpern EJ, Siedentopf C, Auer T, Eberle G, et al. Sonographic cross-sectional area measurement in carpal tunnel syndrome patients: can delta and ratio calculations predict severity compared to nerve conduction studies? Eur Radiol. 2015;25:2419–27.
Jacobson JA, Jebson PJL, Jeffers AW, Fessell DP, Hayes CW. Ulnar nerve dislocation and snapping triceps syndrome: diagnosis with dynamic sonography—report of three cases 1. Radiology. 2001;220:601–5.
Korstanje J-WH, Boer MS-D, Blok JH, Amadio PC, Hovius SER, Stam HJ, et al. Ultrasonographic assessment of longitudinal median nerve and hand flexor tendon dynamics in carpal tunnel syndrome. Muscle Nerve. 2012;45:721–9.
Plaikner M, Loizides A, Loescher W, Spiss V, Gruber H, Djurdjevic T, et al. Thickened hyperechoic outer epineurium, a sonographic sign suggesting snapping ulnar nerve syndrome? Eur J Ultrasound. 2012;34:58–63.
• Miyamoto H, Halpern EJ, Kastlunger M, Gabl M, Arora R, Bellmann-Weiler R, et al. Carpal tunnel syndrome: diagnosis by means of median nerve elasticity—improved diagnostic accuracy of US with sonoelastography. Radiology. 2014. http://pubs.rsna.org/doi/10.1148/radiol.13122901. Prospective case-control study investigating elasticity of the median nerve compared between normal volunteers and patients with symptomatic CTS, measured by the acoustic coupler (AC)/median nerve strain ratio. Results indicate improved diagnostic accuracy for CTS using the AC/MN strain ratio, compared to cross-sectional area measurements alone.
Liao Y-Y, Lee W-N, Lee M-R, Chen W-S, Chiou H-J, Kuo T-T, et al. Carpal tunnel syndrome: US strain imaging for diagnosis. Radiology. 2015;275:205–14.
Drakonaki EE, Allen GM, Wilson DJ. Ultrasound elastography for musculoskeletal applications. Br J Radiol. 2012;85:1435–45.
Kantarci F, Ustabasioglu FE, Delil S, Olgun DC, Korkmazer B, Dikici AS, et al. Median nerve stiffness measurement by shear wave elastography: a potential sonographic method in the diagnosis of carpal tunnel syndrome. Eur Radiol. 2014;24:434–40.
Orman G, Ozben S, Huseyinoglu N, Duymus M, Orman KG. Ultrasound elastographic evaluation in the diagnosis of carpal tunnel syndrome: initial findings. Ultrasound Med Biol. 2013;39:1184–9.
Martinoli C, Gandolfo N, Perez MM, Klauser A, Palmieri F, Padua L, et al. Brachial plexus and nerves about the shoulder. Semin Musculoskelet Radiol. 2010;14:523–46.
Floranda EE, Jacobs BC. Evaluation and treatment of upper extremity nerve entrapment syndromes. Prim Care Clin Off Pract. 2013;40:925–43.
Cass S. Upper extremity nerve entrapment syndromes in sports: an update. Curr Sports Med Rep. 2014;13:16–21.
Ombregt L. Nerve lesions and entrapment neuropathies of the upper limb. Syst Orthop Med. 2013:e119–56. http://linkinghub.elsevier.com/retrieve/pii/B9780702031458000740.
• Carpenter EL, Bencardino JT. Focus on advanced magnetic resonance techniques in clinical practice. Radiol Clin North Am. 2015;53:513–29. Practical review of MRN, focused on peripheral nerves. Discusses protocol design and technical considerations, with application towards imaging of common peripheral nerve disorders throughout the body.
Magill ST, Brus-Ramer M, Weinstein PR, Chin CT, Jacques L. Neurogenic thoracic outlet syndrome: current diagnostic criteria and advances in MRI diagnostics. Neurosurg Focus. 2015;39:E7.
Jengojan S, Kovar F, Breitenseher J, Weber M, Prayer D, Kasprian G. Acute radial nerve entrapment at the spiral groove: detection by DTI-based neurography. Eur Radiol. 2015;25:1678–83.
Kuhn JE, Bible JE. Thoracic outlet syndrome. J Am Acad Orthop Surg. 2015;23:222–32.
Foley J, Finlayson H, Travlos A. A review of thoracic outlet syndrome and the possible role of botulinum toxin in the treatment of this syndrome. Toxins. 2012;4:1223–35.
Cash CJC, Sardesai AM, Berman LH, Herrick MJ, Treece GM, Prager RW, et al. Spatial mapping of the brachial plexus using three-dimensional ultrasound. Br J Radiol. 2005;78:1086–94.
Choi S-J, Ahn JH, Ryu DS, Kang CH, Jung SM, Park MS, et al. Ultrasonography for nerve compression syndromes of the upper extremity. Ultrasonography. 2015;34:275–91.
• Ponnappan RK, Khan M, Matzon JL, Sheikh ES, Tucker BS, Pepe MD, et al. Clinical differentiation of upper extremity pain etiologies. J Am Acad Orthop Surg. 2015;23:492–500. Review article of upper extremity pain resulting from neurologic etiologies (cervical spine pathology, peripheral nerve compression, noncompressive peripheral neuropathy) and musculoskeletal etiologies at the shoulder and elbow with focus on clinical diagnosis and selecting the appropriate confirmatory diagnostic test.
Kwon BC, Koh SH, Hwang SY. Optimal parameters and location for diffusion-tensor imaging in the diagnosis of carpal tunnel syndrome: a prospective matched case-control study. Am J Roentgenol. 2015;204:1248–54.
Tai T-W, Wu C-Y, Su F-C, Chern T-C, Jou I-M. Ultrasonography for diagnosing carpal tunnel syndrome: a meta-analysis of diagnostic test accuracy. Ultrasound Med Biol. 2012;38:1121–8.
Howe BM, Spinner RJ, Felmlee JP, Frick MA. MR imaging of the nerves of the upper extremity. Magn Reson Imaging Clin N Am. 2015;23:469–78.
De Maeseneer M, Marcelis S, Jager T, Girard C, Gest T, Jamadar D. Spectrum of normal and pathologic findings in the region of the first extensor compartment of the wrist: sonographic findings and correlations with dissections. J Ultrasound Med. 2009;28:779–86.
Linda DD, Harish S, Stewart BG, Finlay K, Parasu N, Rebello RP. Multimodality imaging of peripheral neuropathies of the upper limb and brachial plexus 1. RadioGraphics. 2010;30:1373–400.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Daniel Siegal, Leah Davis, Mitchell Scheer, and Lisa Walker each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical collection on Musculoskeletal Imaging.
Rights and permissions
About this article
Cite this article
Siegal, D., Davis, L., Scheer, M. et al. Entrapment Neuropathies of the Upper Extremity Nerves. Curr Radiol Rep 4, 63 (2016). https://doi.org/10.1007/s40134-016-0190-8
Published:
DOI: https://doi.org/10.1007/s40134-016-0190-8