Abstract
Purpose of review
Pericardial pathology represent a spectrum of entities that should be properly recognized and treated when necessary. To reach an accurate diagnosis, clinicians have at their disposal an ample armamentarium that includes invasive and non-invasive methods, including echocardiography, computed tomography (CT) and magnetic resonance (MR).
Recent findings
CT and MR can be performed as complementary methods when echocardiographic results are inconclusive. These modalities can give not only detailed information on cardiac and pericardial anatomy but also can evaluate physiologic changes. To the extent that in some instances, MR or CT could be the preferred method of choice, i.e., constrictive pericarditis.
Summary
Many disease processes can affect the pericardium. CT and MR, although not representing the initial method of choice which is usually echocardiography, they do play a crucial complementary role when those first line studies are equivocal. Familiarity with the imaging appearance of pericardial disease particularly tamponade and constrictive pericarditis will help treat these patients in a more expeditious fashion.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pericardial pathology represents a spectrum of entities that should be properly recognized and treated when necessary. Moreover, the pericardial pathology represents a challenge for the clinician due to its unspecific symptoms and equivocal physical exam findings. To reach an accurate diagnosis, clinicians have at their disposal an ample armamentarium that includes invasive and noninvasive methods, including echocardiography, computed tomography (CT), and magnetic resonance (MR). The aim of this review is to illustrate the most common pericardial diseases, focusing on the pertinent role played by CT and MR.
Normal Anatomy
The pericardium is an avascular fibrous sac, which is composed of two membranes: the inner serous layer and the outer fibrous pericardium, which surround the heart and great vessels. The inner layer is composed of two layers as well: the visceral and the parietal, which are separated by a virtual space that normally contains up to 50 cc of clear liquid [1–4].
In CT, the pericardium is best evaluated in systole, being displayed as a thin dense line which can measure up to 2 mm [5]. Usually the pericardium is invisible above the lateral and posterior wall of the left ventricle.
In MR, the pericardium usually measures between 1.2 and 1.7 mm thickness, which slightly overestimates the pericardial measures done in cadaveric studies, because of limits of spatial resolution and chemical shift artifacts [6, 7•, 8]. Visualization of visceral pericardium is facilitated by the presence of mediastinal and epicardial fat. Contrast media administration assists in the identification when there is a lack of epicardial fat [1]. The pericardium usually is best visualized in the anterior portion, in juxtaposition to the right heart chambers [9]. The normal pericardium is smooth, thin, well delineated, and hypointense in both T1 and T2 black-blood sequences. The transverse, preaortic, and retroaortic sinus can be seen in the majority of patients [10, 11]. In SSFP techniques, pericardial layers show low signal intensity, whereas pericardial fluid usually presents high signal intensity.
Usually, it is important to understand the insertions of the parietal pericardium, defining the limits of the pericardial space. At the cephalic aspect, the parietal pericardium is attached to the proximal segment of large vessels, partially surrounding the ascending aorta and the pulmonary artery trunk, about 1 cm below the origin of the innominate artery. This upper attachment is called the “upper union line”. Caudally, the parietal pericardium is attached to the central tendon of the diaphragm [12••].
Due to the very close apposition of the parietal and visceral sheets of the pericardium, and their relationship to adjacent mediastinal structures, the pericardium creates sinuses which are composed of several recesses, representing a redundancy or sleeve that may contain small amounts of fluid. The superior pericardial recess (part of the transverse sinus) surrounds the right wall of the ascending aorta, and can be confused with aortic dissections, mediastinal masses, lymph nodes, or thymus when it is distended with fluid. The transverse pericardial recess, dorsal to the ascending aorta, can be confused with an aortic dissection or adenopathy. The oblique sinus located behind the left atrium can be misinterpreted as esophageal lesions or bronchogenic cyst [13–16] (Fig. 1).
Pericardial Disease: Study Techniques
Pericardial pathology represents a diagnostic challenge mainly because of its nonspecific clinical presentation. Usually the pericardial evaluation begins with an electrocardiogram and a transthoracic echocardiography because of their availability, cost, and diagnostic accuracy. Additionally, or if the former studies have shown inconclusive results, CT and MR can be performed due to their ability to show detailed information on cardiac and pericardial anatomy, and their larger “field of view” (FOV) compared with echocardiography that allows to determine etiologies, assess the extent of the disease, and the potential impact on adjacent structures and organs.
MR imaging provides not only morphological, but also functional evaluation of the pericardium, with high reproducibility, free of ionizing radiation, and iodinated contrast media administration [5]. Improvements on cardiac MR imaging have increased the utility of this technique in the pericardial evaluation and characterization, and also in its functional repercussion over the heart. For that reason, not only morphological evaluation based on T1 and T2 black-blood sequences are necessary, but also steady-state free precession (SSFP) sequences for depicting biventricular function and pericardial stiffness, tagging techniques for identification of pericardial adhesions, phase-contrast imaging for detecting diastolic dysfunction, and real-time imaging for identification of ventricular coupling are necessary in a stand-alone evaluation of the pericardium [7•, 17].
Although T2 short inversion recovery (STIR) sequences could depict edema of pericardial layers, also there are other “functional” MR-based techniques which could depict edema in the pericardium and adjacent myocardium, such as diffusion-weighted imaging (DWI) [18–20]. Late gadolinium enhancement (LGE) permits not only detection of the pericardium in the absence of epicardial fat, but also detection of active inflammation of the pericardium, tissue, and lesion characterization.
Congenital Pericardial Absence
It is a rare disease, with a prevalence reported in surgical and pathological series between 0.002 and 0.004 % of the population [21]. It is caused by an abnormal embryological development secondary to the decreased vascular supply of the pleuropericardial membrane that surrounds the ventral cardiac tube. It is subclassified into total absence of the pericardium; total or partial right pericardial defect; total or partial left pericardial defect, and diaphragmatic defect. The partial left pericardial defect is the most common abnormality, reported in up to 70 % of cases [5, 12••].
In a normal setting, the pericardium covers the aortopulmonary window, which also contains fat. When we have the presence of a partial left pericardial congenital defect, there may exist an interposition of lung parenchyma between the aorta and pulmonary artery. Moreover, it can be seen that there is passage of the left atrial appendage through the pericardial defect. Other suggestive findings are levorotation of the apex towards the left axilla, an exaggerated movement of the posterior wall of the heart, or a falsely elongated right ventricle. Complications include left atrial appendage entrapment, which can cause ischemic necrosis and compression of the left coronary artery, which can induce myocardial ischemia [7•]. Complete birth defects have virtually no clinical significance. The congenital absence of the pericardium is associated with other congenital malformations such as bicuspid aorta, patent ductus arteriosus, mitral stenosis, and atrial septal defect [1, 5, 22] (Fig. 2).
Acute Pericarditis (AP)
Acute inflammation of the pericardium can be caused by primary pericardial disease or a systemic pathology. AP may or may not be accompanied by pericardial effusion [1, 23]. Clinically, it may present with positional chest pain, which may be relieved in the “Mahommetan position”, usually preceded by a viral prodrome. Pericarditis could have an acute, subacute, recurrent, or chronic presentation. In the United States, most acute pericarditis are idiopathic, with viral being the most common etiology. Other common forms include iatrogenic or posttraumatic pericarditis. Globally, in underdeveloped countries, tuberculosis remains a common cause of pericarditis [24•].
In patients with ischemic disease pericarditis could appear early after the onset of acute transmural infarction, due to the spread of infarct-related inflammation (epistenocardic pericarditis) [17]. In patients with established myocardial infarction, also could present pericarditis due to autoimmune reaction without any temporal relation. This is known as Dressler syndrome [25].
Often, pericarditis is associated with some degree of myocardial involvement. Recognition of associated myocarditis is associated with negative prognosis often requiring hospitalization [26–28].
In CT, and in the appropriate clinical setting, a pericardial thickening of 4 mm is suggestive of acute pericarditis. In the subacute stage, pericardial contours can become irregular and may or may not be accompanied by pericardial effusion.
Similar morphologic findings could be seen in MR in T1-weighted imaging (T1WI) and SSFP sequences. Pericardial effusion could be present. T2-weighted imaging (T2WI)-based sequences, such as T2-STIR or DWI, could demonstrate edematous pericardial layers. Uptake of gadolinium on LGE is due to the presence of active inflammation constituted by granulomatous tissue and fibrin deposits [17]. Contrarily, the presence of collagen deposits and fibroblasts are responsible for the absence of enhancement in chronic forms. This behavior contrasts with fibrous myocardial tissue and it is due to inherent avascularity of the pericardium [29] (Figs. 3, 4).
A 28-year-old male with syncope and chest pain. In the Chest Radiography examination, there is cardiomegaly of new onset (a and b). Pericardial hyperintensity on T2 STIR (blue arrow in c) but also in b = 300 s/mm2 with no restriction in DWI (yellow arrows in d and e). Mild edema and positive LGE of the pericardium (red arrows) indicating active inflammation. It is suggestive of acute pericarditis (Color figure online)
Pericardial Effusion
Pericardial effusion could be secondary to venous or lymphatic obstruction of cardiac drainage. The most common causes are heart failure, renal failure, infections (bacterial, viral, or tuberculous), neoplasms (lung, breast, or lymphoma), and pericardial lesions (traumatic or secondary to myocardial infarction) [5].
CT is indicated in suspected hemopericardium, loculated effusion, pericardial thickening, or after an inconclusive echocardiography [30]. When pericardial effusion is evaluated, it is important to measure the fluid attenuation, because values higher than 25 Hounsfield Units (HU) suggest an exudate, worrisome of neoplasia, hemopericardium, pus or effusion associated with hypothyroidism. There are some case reports of pericardial effusions with low-HU in patients with chylopericardium [31, 32].
The amount of pericardial effusion can be estimated by measuring its size in centimeters, perpendicular to the ventricular wall; however, more important is the rate of accumulation of the effusion [22]. In an acute pericardial effusion, pericardial fluid of 150–250 cc may be sufficient to cause cardiac tamponade, while a slower accumulation of pericardial fluid, as for example, in thyroid myxedema, amounts up to 3 L of pericardial fluid can accumulate without tamponade [16, 33, 34].
In MR, transudate pericardial effusion is hypointense on T1WI and hyperintense on T2WI. Contrarily, exudates are intermediate on T1WI and T2WI [7•]. In the presence of flow-related artifacts, pericardial fluid characterization is not always feasible [8]. Cine SSFP are often more reliable for the evaluation of complexity and differentiation of septations and clots. Also, identification of a thickened or thinned pericardium could suggest the presence of an exudate or a transudate. Thickened irregular pericardium could be seen not only in malignant pleural effusions but also in infectious pericarditis such as tuberculosis [7•]. The combination of SSFP with dynamic contrast-enhanced MR could accurately depict neoplastic pericardial invasion [35].
Recently, DWI has shown utility in noninvasive characterization of pleural effusions. By applying an apparent diffusion coefficient (ADC), threshold between 3.39 and 3.6 × 10–3 mm2/s could differentiate exudates from transudates with a sensitivity and specificity of 90.6 and 85 %, respectively [36] (Fig. 5).
Constrictive Pericarditis
It is a fibrous and cicatricial thickening of the pericardium which determines a loss of the normal elasticity, and a difficulty in the normal ventricular filling [12••, 24•].
Patients develop symptoms of heart failure, dyspnea, fatigability, orthopnea, edema of extremities, ascites, or hepatomegaly.
The spectrum of etiologies causing pericardial constriction has changed over time moving from infectious causes (specially tuberculous) to postradiation and postoperative forms [17]. CT findings suggestive of constrictive pericarditis include pericardial thickening greater than 4 mm (diffuse or focal), tubular deformation and narrowing of the right ventricle; normal or decreased ventricular size and thinning and/or rectification of the interventricular septum, and pericardial calcifications. Secondary findings include signs of right ventricular diastolic failure: dilatation of the inferior vena cava, hepatic veins and right atrium; hepatosplenomegaly, ascites, and pleural effusion.
The absence of pericardial thickening does not rule out constrictive pericarditis. Moreover, the presence of pericardial calcifications is not a pathognomonic finding of this condition. About 50 % of the patients with pericardial calcifications will have constrictive physiology, and about 90 % of the patients with constrictive physiology will have pericardial calcifications [1, 34].
MR has the ability to show not only morphological findings mentioned above, except pericardial calcifications which are not pathognomonic, but also the functional and hemodynamic consequences which could enhance the diagnosis of pericardial constriction. Depiction of residual active inflammation on LGE could direct those patients with “reversible” or “transient” forms of constrictive pericarditis towards anti-inflammatory treatment instead of undergo pericardiectomy [37].
On phase-contrast sequences of the tricuspid valve, a restrictive physiology could be seen with increased E wave and decreased A wave. Flow in the inferior vena cava also shows restrictive physiology. This reflects increased cardiac filling pressures [17].
Also there is an increased ventricular coupling and dissociation between intracardiac and intrathoracic pressures. The lack of pericardial compliance leads to an increased ventricular coupling and an early diastolic leftwards ventricular septal bowing (“septal bounce”; paradoxical diastolic septal motion) [38]. This is enhanced in inspiration and best depicted in real-time cine imaging, which could differentiate pericardial constriction from restrictive cardiomyopathy [39, 40]. These abnormalities are more conspicuous in the basal septum, which adopts an S-like septal motion on four chamber views (Fig. 6).
Constrictive pericarditis in a 58-year-old male patient (a–e). Chest radiography (a–b) showing pericardial calcification better depicted in the lateral view (arrow) and enlargement of the left atrium. Axial contrast-enhanced CT images (c–e) show pericardial thickening and difuse calcification (white arrows) with tubular deformation and narrowing of the ventricles. Also noted S shaped of the interventricular septum (red arrow in d), enlargement of the right atrium (white star in d), and dilatation of the inferior vena cava (asterisk in e) (Color figure online)
MR tagging allows identifying fibrous fusion of the pericardium to the underlaying myocardium. In nonfused pericardium, tag lines rapidly become discontinuous, whereas in fibrotic fusion, these tag lines persist [41].
Pericardial Tamponade
Pericardial tamponade is a life-threatening condition secondary to fast or slow heart compression by accumulation of fluid, pus, blood, gas, or tissue in the pericardial cavity. This can result from a multitude of causes such as trauma, inflammation, wound healing, and neoplastic disease, among others.
Hemodynamically, an intracardiac volume decrease and an increased diastolic filling pressure occurs. The increase of the intrapericardial pressure determines an external cardiac compression [42]. As mentioned above, the rate of fluid accumulation in the pericardial cavity is more important than the quantity or type of pericardial content [43].
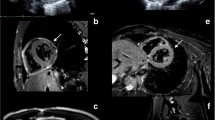
In an acute setting, the pericardium is rigid and not compliant, so a pericardial effusion that rapidly sets in can abruptly increase the intrapericardial pressure, and can cause cardiac tamponade with amounts as small as 100 or 200 cc of fluid. On the other hand, in a subacute or chronic setting, the pericardium becomes more elastic and more compliant, therefore gradual or slow pericardial fluid accumulations of up to 1000 or 1500 cc can be tolerated without hemodynamic compromise [42–44] (Fig. 7).
48-year-old male patient with a Type A intramural hematoma (asterisk in a and b), showing moderate hemopericardium (star in c and d). Due to the rapid onset of the effusion, the patient also had symptoms of pericardial tamponade demonstrated here by flattening of the anterior ventricular wall (arrow in d)
The term effusive constrictive pericarditis refers to an uncommon pericardic syndrome characterized by a cardiac tamponade and a concomitant constriction. Tamponade is produced by a tense pericardial effusion and the constriction is produce by the cicatrization and calcification of the visceral pericardium. These patients may be wrongly classified only as a pericardial tamponade; however, in patients with an associated constriction, the central venous pressure will remain high even after placing a pericardial drainage [45].
Clinical manifestations of cardiac tamponade will depend on the rate of accumulation of fluid and the effectiveness of compensatory mechanisms. Symptoms, although not specific, can range from tachypnea, and exercise dyspnea to anorexia, dysphagia, and cough. The physical examination findings are also unspecific and include tachycardia, decreased cardiac sound, hypotension, and distended jugular veins. A diagnostic key is a “paradoxical pulse” (pulsus paradoxus) defined as a drop in systolic pressure in inspiration of 10 mmHg or more during normal breathing.
Echocardiography remains the first line in the study of pericardial disease, particularly of the pericardial effusion; however, CT and MR play an important complementary role in clarifying both the extent and the physiological effects of pericardial disease. In CT, signs suggestive of cardiac tamponade are flattening of the anterior edge of the heart, compression of the right atrium and right ventricle, contrast reflux into the inferior vena cava and azygos vein; dilatation of the inferior vena cava and coronary sinus. Also, the increased caliber of the superior vena cava has been described with a diameter similar to or greater than the adjacent thoracic aorta and dilatation of the inferior vena cava with a diameter at least twice that of the adjacent abdominal aorta [42, 43, 46, 47].
In MR, added to the morphological signs observed in CT, typical features consist of diastolic collapse of RV free wall, suggesting higher pericardial pressure than ventricular pressures, right atrial compression during early systole, and diastolic flow reversal in phase-contrast imaging of inferior vena cava. Depiction of signs of constriction is mandatory in order to differentiate effusive constrictive pericarditis from cardiac tamponade, preventing the persistence of constrictive physiology after pericardiocentesis [17].
Once again, it may be useful to measure the pericardial fluid density to distinguish between a single effusion and hemorrhagic content. The treatment of cardiac tamponade is mainly drainage of the pericardial content.
Pericardial Tumors
In the adult population, most of the pericardial neoplastic diseases are malignant. The most frequent is metastatic disease. In autopsies series, about 10–20 % of patients with cancer have pericardial metastases [24•, 34]. Pericardial metastatic involvement can occur by direct invasion, hematogenous spread, lymphatic spread, and most frequent from lung, breast, lymphoma, or melanoma [24•].
Primary pericardial neoplasms are uncommon, with a prevalence estimated between 0.02 and 0.056 %. Mesothelioma is the most frequent primary malignant pericardial neoplasm. Other malignant neoplasms include sarcoma, lymphoma, and primitive neuroectodermal tumor (PNET).
Of the pericardial benign lesions, the most common are pericardial cysts and lipomas [48].
The symptoms of pericardial neoplasms are primarily the result of the presence of pericardial effusion, pericarditis, or invasion of adjacent structures. Symptoms include dyspnea on exercise, chest pain, cough, palpitations, fatigue, night sweats, fever, and facial or lower extremities edema. In an acute setting, two physiological effects may occur: a constrictive physiology with or without cardiac tamponade associated and alternatively a compression of the pulmonary or systemic veins can be produced, which can determine reduction of preload on the right and left heart, respectively [16].
It is not uncommon that neoplastic pericardial effusions would be hemorrhagic.
Sometimes, the neoplastic pericardial compromise determines a nodular thickening of the pericardium, frequently with an extension into the epicardial fat, while nonneoplastic inflammatory conditions usually produce a smooth thickening and a continuous uptake of the pericardium [48].
Pericardial neoplastic lesions can be studied with CT or a MR to assess the extent of the lesion, tumor dissemination, or evaluation of calcifications and lymph nodes. MR could characterize the target lesion by using T1- and T2-weighted images, but also, perfusion and LGE to assess angiogenesis and enhancement. DWI, as observed in other parts of the body, has the ability to differentiate malignant from benign lesions, but also, to delineate solid form cystic components of the tumor [35].
In MR, malignant lesions show low to intermediate signal intensity on T1WI and high signal intensity on T2WI. Melanoma metastasis also could show hyperintense T1WI signal intensity lesions due to the presence of paramagnetic substances (melanin). In DWI, they have a restrictive behavior and, usually, heterogeneous enhancement in LGE. SSFP and perfusion imaging could help to increase the accuracy of MR in the depiction of direct invasion of the pericardium from other thoracic malignancies [7•].
A pericardial cyst is a rare, benign congenital lesion, which represents an accumulation of fluid adjacent to the cardiac border, most of the times on the right costophrenic angle. Its size varies from 2 to 28 cm in diameter. In CT, pericardial cysts are seen as a well-defined hypodense structure that has a virtually imperceptible wall with a homogeneous content. Sometimes, it can have an intermediate density between 30 and 40 UH, suggestive of proteinaceous content or hemorrhagic complication [48]. In MR, they appear as a well-defined lesion, hypointense on T1WI and hyperintense on T2WI, without significant enhancement. Pericardial cysts with proteinaceous content could have hyperintense behavior on T1WI [17] (*Figs. 8, 9).
66-year-old male with a partly calcified pericardial cyst. Nonenhanced and enhanced chest CT (white arrow in a and b). c–e Morphologic cardiac MR sequences revealed a thick-walled pericardial cyst with hyperproteic content (yellow arrows). f LGE confirm the cystic nature of the lesion and showed some peripheral enhancement of the wall (blue arrow) (Color figure online)
The pericardial diverticulum is an outpouching of the pericardial space which can be differentiated from the cyst due to the presence of a communication with the pericardial space and the changes in size relative to the body position [22].
Similarly as the subcutaneous lipomas, the pericardial lipoma is an encapsulated tumor, however tend to be less circumscribed. Also it frequently presents a slow growth; therefore, it has very few associated symptoms, usually relating to the compression of adjacent structures. In CT, they will be seen as encapsulated lesions with fat density in the pericardial cavity. In MR, they typically are hyperintense on T1WI and have their signal intensity suppressed on T1 sequences with fat saturation [7•]. This also occurs in malignant pericardial tumors with fatty component, such as lyposarcomas [5, 7•].
The primary malignant pericardial mesothelioma is extremely rare, with a reported prevalence of 0.0022 % in autopsy series, however is the most common primary malignant pericardial neoplasm [48].
They tend to occur more frequently in men, mainly between the fifth and seventh decade of life. Three histological types have been described: epithelial, biphasic (mixed), and fibrous (spindle cell), of which the epithelial type is the most frequent [49].
Contrary to the pleural mesothelioma, the relationship with asbestos exposure is still controversial. The survival rate is about 6 weeks to 15 months, independently of the therapy. The clinical symptoms include those associated with constrictive pericarditis, pericardial effusion, cardiac tamponade, and infiltrative myocardial involvement, which can determine electrical conduction disorders (Fig. 10).
25-year-old patient with shortness of breath, showing a huge heterogenic pericardial mass (asterisk in a and b) with moderate contrast enhancement. Also note compression of the left ventricule and signs of possible myocardial invasion (arrow in b). c and d. Cardiac MRI Four chamber TRUE-FISP (c) again reveals the heterogeneous pericardial mass (asterisk) compressing the left ventricule. In the short axis TRUE-FISP (d), also noted a right atrial thrombus (star). Operative specimen revealed a primary pericardial sarcomatoid mesothelioma
Both CT and MR offer advantages over echocardiography, because they allow a more accurate evaluation of the extent of the disease. In CT and MR, pericardial mesothelioma is seen as a mass with heterogeneous enhancement that compromises both pericardial layers, with a possible invasion of vascular and anatomical adjacent structures. About 50 % of the patients will have metastatic disease at diagnosis, most commonly toward the local mediastinal lymph nodes and lungs [48, 50].
Conclusion
Many disease processes can affect the pericardium, and the list is rather long: congenital, traumatic or iatrogenic injury, infectious and neoplastic diseases among others. CT and MR, although not representing the initial method of choice which is usually echocardiography, they do play a crucial complementary role when those first-line studies are equivocal, particularly because of their inherent ability to provide both morphologic and physiologic information with a larger field of view.
Familiarity with the advantages and disadvantage of each imaging modality is a key factor when selecting the proper method from the imaging menu.
Moreover, familiarity with the imaging appearance of pericardial disease particularly tamponade and constrictive pericarditis will help treat these patients in a more expeditious fashion.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance, •• Of major importance
Yared K, Baggish AL, Picard MH, Hoffmann U, Hung J. Multimodality imaging of pericardial diseases. JACC Cardiovasc Imaging. 2010;3:650–60.
Edwards ED. Applied anatomy of the heart. In: Giuliani ER, Fuster V, editors. Cardiology: fundamentals and practice. 2nd ed. St Louis: Mosby-Year Book; 1991. p. 47–51.
Hutchison SJ, Nuyianes C. Pericardial diseases: clinical diagnostic imaging atlas. Philadelphia: Elsevier Health Sciences; 2008.
LeWinter MM, Kabbani S. Pericardial diseases. In: Zipes DP, Libby P, Bonow RO, Braunwald E, editors. Heart disease a text book cardiovascular medicine. 7th ed. Philadelphia: Elsevier Health Sciences; 2005. p. 1757–80.
Wang ZJ, Reddy GP, Gotway MB, Yeh BM, Hetts SW, Higgins CB. CT and MR imaging of pericardial disease. Radiographics. 2003;23:S167–80.
Sechtem U, Tscholakoff D, Higgins CB. MRI of the abnormal pericardium. Am J Roentgenol. 1986;147:245–52.
• Peebles CR, Shambrook JS, Harden SP. Pericardial disease–anatomy and function. Br. J. Radiol. 2011;84:S324–37. Good and important view of the pericaldial basics, in order to understand the distribution of diseases.
Bogaert J, Francone M. Cardiovascular magnetic resonance in pericardial diseases. J Cardiovasc Magn Reson. 2009;11:14.
Frank H, Globits S. Magnetic resonance imaging evaluation of myocardial and pericardial disease. J Magn Reson Imaging. 1999;10:617–26.
Im JG, Rosen A, Webb WR, Gamsu G. MR imaging of the transverse sinus of the pericardium. Am J Roentgenol. 1988;150:79–84.
Stark DD, Higgins CB, Lanzer P, Lipton MJ, Schiller N, Crooks LE, et al. Magnetic resonance imaging of the pericardium: normal and pathologic findings. Radiology. 1984;150:469–74.
•• Dexter I, Zalta B. Pericardial effusion. In: White CS, Haramati LB, Chen JJ, M LJ, editors. Rotations Radiol. Card. Imaging. New York: Oxford University Press; 2014. p. 430–434. Awesome aproach and book about not only pericardial but cardiac diseases, foccused in clinical and imaging aspects of diseases.
Chiles C, Baker ME, Silverman PM. Superior pericardial recess simulating aortic dissection on computed tomography. J Comput Assist Tomogr. 1986;10:421–3.
Levy-Ravetch M, Auh YH, Rubenstein WA, Whalen JP, Kazam E. CT of the pericardial recesses. Am J Roentgenol. 1985;144:707–14.
Batra P, Bigoni B, Manning J, Aberle DR, Brown K, Hart E, et al. Pitfalls in the diagnosis of thoracic aortic dissection at CT angiography 1. Radiographics. 2000;20:309–20.
Czum JM, Silas AM, Althoen MC. Evaluation of the pericardium with CT and MR. ISRN Cardiol. 2014;2014:174908.
Bogaert J, Francone M. Pericardial disease: value of CT and MR imaging. Radiology. 2013;267:340–56.
Potet J, Rahmouni A, Mayer J, Vignaud A, Lim P, Luciani A, et al. Detection of myocardial edema with low-b-value diffusion-weighted echo-planar imaging sequence in patients with acute myocarditis. Radiology. 2013;269:362–9.
Le Bihan D. Apparent diffusion coefficient and beyond: what diffusion MR imaging can tell us about tissue structure. Radiology. 2013;268:318–22.
Kociemba A, Pyda M, Katulska K, Łanocha M, Siniawski A, Janus M, et al. Comparison of diffusion-weighted with T2-weighted imaging for detection of edema in acute myocardial infarction. J Cardiovasc Magn Reson. 2013;15:90.
Yamano T, Sawada T, Sakamoto K, Nakamura T, Azuma A, Nakagawa M. Magnetic resonance imaging differentiated partial from complete absence of the left pericardium in a case of leftward displacement of the heart. Circ J. 2004;68:385–8.
Cosyns B, Plein S, Nihoyanopoulos P, Smiseth O, Achenbach S, Andrade MJ, et al. European Association of Cardiovascular Imaging (EACVI) position paper: multimodality imaging in pericardial disease. Eur Heart J Cardiovasc Imaging. 2015;16:12–31.
Maisch B, Seferović PM, Ristić AD, Erbel R, Rienmüller R, Adler Y, et al. Guidelines on the diagnosis and management of pericardial diseases executive summary; The task force on the diagnosis and management of pericardial diseases of the European society of cardiology. Eur Heart J. 2004;25:587–610.
• Cummings KW, Luna A, Atalay MK. MR Imaging of pericardial diseases. Appl Radiol. 2015;44:8–16. Excelent aproach to pericardial diseases, focused in MR.
Doulaptsis C, Goetschalckx K, Masci PG, Florian A, Janssens S, Bogaert J. Assessment of early post-infarction pericardial injury by CMR. JACC Cardiovasc Imaging. 2013;6:411–3.
Imazio M, Trinchero R. Myopericarditis: etiology, management, and prognosis. Int J Cardiol. 2008;127:17–26.
Little WC, Freeman GL. Pericardial disease. Circulation. 2006;113:1622–32.
Imazio M, Brucato A, Maestroni S, Cumetti D, Belli R, Trinchero R, et al. Risk of constrictive pericarditis after acute pericarditis. Circulation. 2011;124:1270–5.
Taylor AM, Dymarkowski S, Verbeken EK, Bogaert J. Detection of pericardial inflammation with late-enhancement cardiac magnetic resonance imaging: initial results. Eur Radiol. 2006;16:569–74.
Bull RK, Edwards PD, Dixon AK. CT dimensions of the normal pericardium. Br J Radiol. 1998;71:923–5.
Ordovas KG, Higgins CB. Pericardial diseases. In: McAllisster L, Barrett K, editors. MRI CT cardiovascular system. 1st ed. Philadelphia: Lippincott; 2006. p. 137–53.
Tomoda H, Hoshiai M, Furuya H, Oeda Y, Matsumoto S, Tanabe T, et al. Evaluation of pericardial effusion with computed tomography. Am Heart J. 1980;99:701–6.
Boxt L, Abbara S, Miller SW. Cardiac imaging: The Requisites. Philadelphia: Elsevier Health Sciences; 2009.
Rienmüller R, Gröll R, Lipton MJ. CT and MR imaging of pericardial disease. Radiol Clin N Am. 2004;42:587–601.
Broncano J, Luna A, Sánchez-González J, Alvarez-Kindelan A, Bhalla S. Functional MR imaging in chest malignancies. Magn Reson Imaging Clin N Am. 2016;24:135–55.
Inan N, Arslan A, Akansel G, Arslan Z, Elemen L, Eleman L, et al. Diffusion-weighted MRI in the characterization of pleural effusions. Diagn Interv Radiol. 2009;15:13–8.
Mark DB, Berman DS, Budoff MJ, Carr JJ, Gerber TC, Hecht HS, et al. ACCF/ACR/AHA/NASCI/SAIP/SCAI/SCCT 2010 expert consensus document on coronary computed tomographic angiography: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. Circulation. 2010;121:2509–43.
Méndez C, Soler R, Rodriguez E, López M, Alvarez L, Fernández N, et al. Magnetic resonance imaging of abnormal ventricular septal motion in heart diseases: a pictorial review. Insights Imaging. 2011;2:483–92.
Hundley WG, Bluemke DA, Finn JP, Flamm SD, Fogel MA, Friedrich MG, et al. ACCF/ACR/AHA/NASCI/SCMR 2010 expert consensus document on cardiovascular magnetic resonance: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. Circulation. 2010;121:2462–508.
Hundley WG, Bluemke D, Bogaert JG, Friedrich MG, Higgins CB, Lawson MA, et al. Society for cardiovascular magnetic resonance guidelines for reporting cardiovascular magnetic resonance examinations. J Cardiovasc Magn Reson. 2009;11:5.
Kojima S, Yamada N, Goto Y. Diagnosis of constrictive pericarditis by tagged cine magnetic resonance imaging. N Engl J Med. 1999;341:373–4.
Restrepo CS, Lemos DF, Lemos JA, Velasquez E, Diethelm L, Ovella TA, et al. Imaging findings in cardiac tamponade with emphasis on CT. Radiographics. 2007;27:1595–610.
Goldstein L, Mirvis SE, Kostrubiak IS, Turney SZ. CT diagnosis of acute pericardial tamponade after blunt chest trauma. Am J Roentgenol. 1989;152:739–41.
Ameli S, Shah PK. Cardiac tamponade. Pathophysiology, diagnosis, and management. Cardiol Clin. 1991;9:665–74.
Sagristà-Sauleda J, Angel J, Sánchez A, Permanyer-Miralda G, Soler-Soler J. Effusive-constrictive pericarditis. N Engl J Med. 2004;350:469–75.
Rotondo A, Scialpi M, Catalano O, Strada A, Grassi R, Angelelli G. Periportal lymphatic distension resulting from cardiac tamponade: CT findings and clinical-pathologic correlation. Emerg Radiol. 1999;6:85–93.
Gold M. Cardiac tamponade. In: White CS, Haramati LB, Chen JJ, Levsky JM, editors. Rotations radiology card imaging. New York: Oxford University Press; 2014. p. 439–41.
Restrepo CS, Vargas D, Ocazionez D, Martínez-Jiménez S, Betancourt Cuellar SL, Gutierrez FR. Primary pericardial tumors. Radiographics. 2013;33:1613–30.
Nilsson A, Rasmuson T. Primary pericardial mesothelioma: report of a patient and literature review. Case Rep Oncol. 2009;2:125–32.
Fazekas T, Tiszlavicz L, Ungi I. Primary malignant pericardial mesothelioma. Orv Hetil. 1991;132:2677–80.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Sebastian Yevenes, Jordi Broncano, and Fernando R. Gutierrez each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical collection on Cardiovascular Imaging.
Rights and permissions
About this article
Cite this article
Yevenes, S., Broncano, J. & Gutierrez, F.R. CT and MR Update of Pericardial Diseases: A Systematic Review. Curr Radiol Rep 4, 52 (2016). https://doi.org/10.1007/s40134-016-0180-x
Published:
DOI: https://doi.org/10.1007/s40134-016-0180-x