Abstract
Purpose of Review
Acute kidney injury (AKI) is common among the infants admitted in the NICU, particularly the preterm infants. Very little is known about this disease in this vulnerable population.
Recent Findings
AWAKEN (Assessment of Worldwide Acute Kidney injury Epidemiology in Neonates) study conducted by Neonatal Kidney Consortium (NKC) and other recent studies during the last decade have added to the knowledge of AKI in preterm infants regarding its definition, epidemiology, risk factors, association, and outcomes.
Summary
The lack of uniform definitions of AKI has been one of the biggest hurdles in knowing the true incidence of the disease and its risk factors. This, in turn, is related to delayed recognition and prevention of AKI. Furthermore, with the advances in technology, there has been an increase in renal replacement therapy (RRT) for the management of AKI in preterm infants. In this review, we will detail the development of kidney function in the preterm infant, definition of AKI, newly reported risk factors, association with dysfunction of other organs, recurrent AKI, and possible progression to chronic kidney disease. We will also discuss the increasing role of omics in early identification and effects of management of AKI in preterm infants.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acute kidney Injury (AKI) is common among the infants admitted in the NICU, particularly the preterm infants. The lack of uniform definitions of AKI has been one of the biggest hurdles in knowing the true incidence of the disease and its risk factors. This, in turn, is related to delayed recognition and overall prevention of AKI. In the last decade, there has been a tremendous increase in the knowledge of AKI in infants, especially preterm infants. This has led to improved disease definition and related prevention. Furthermore, with the advances in technology, there has been an increase in renal replacement therapy (RRT). In this review, we will detail the development of kidney function in the preterm infant, definition of AKI, newly reported risk factors, association with dysfunction of other organs, recurrent AKI, and possible progression to chronic kidney disease. We will also discuss the increasing role of omics in early identification of AKI and recent technological advancements related to RRT. Many of these advancements are related to the AWAKEN (Assessment of Worldwide Acute Kidney injury Epidemiology in Neonates) study conducted by Neonatal Kidney Consortium (NKC) [1••].
Development of Kidney Function in Preterm Infants
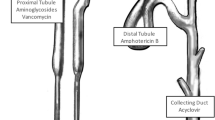
Nephrogenesis is complete in term infants at birth, but in preterm infants, it continues in the extrauterine life until 36 weeks. This development may be influenced by the extrauterine environment leading to a decreased number of nephrons [2]. The number of nephrons in an infant varies due to genetic, intrauterine, and extrauterine life influences and is in the range of 0.5 to 3.5 million in both kidneys [3]. Both glomerular and tubular functions start at about 10 weeks of intrauterine life and continue to mature until 2 years of age. Glomerular filtration rate (GFR) increases from 5 to 40 ml/kg/1.73 m2 at birth in a term infant, to an adult level of 120 ml/kg/1.73 m2 at 2 years of life and so does renal blood flow, from 3 to 5% at birth to 20% in adults by 2 years of life [4]. This increase is related to the delicate balance of vasoactive forces such as angiotensin 2, prostaglandins, nitric oxide, and catecholamines [5••]. Urine output also increases in the fetal life from 6 ml/h at 20 weeks to 60 ml/h at 40 weeks but it is hypotonic at 700 mOsm and gradually increases to adult levels of 1400 mOsm by 1 year of life [6]. This is related to changes in the tubular insensitivity to ADH, low number of aquaporin channels, and decreased osmolality in the medullary interstitium. Other contributing changes include tubular immaturity, which is more pronounced in preterm infants and is associated with decreased serum sodium due to increased sodium loss from the tubules, increased serum potassium related to intracellular to extracellular shift and increase peritubular leak from the tubules to the interstitium, and low serum bicarbonate levels due to decreased threshold of tubular reabsorption [5••, 6].
Definition and Staging of AKI in Preterm Infants
Different definitions of AKI have been used in the past. Some are based on clinical criteria and others from adult or pediatric patients. There is no specific consideration to maturing kidney function and the effect of the extrauterine environment that may prevent the kidneys from reaching its full potential. Most use the clinical definition of AKI based on serum creatinine levels (SCr) and urine output (UO). SCr value of > 1.5 mg/dl was used to define AKI, but a sudden increase in the concentration of SCr is often cited as AKI, such as a daily increase of SCr on day 1 of > 0.5 mg/dl in preterm infants [7]. Similarly, UO of < 1 ml/kg/h was defined as oliguria. Clinical definitions have included one or both SCr and UO.
The definition and staging of AKI in neonates, per the Acute Kidney Injury in Neonates (AKIN) and Neonatal Risk, Injury, Failure, Loss of function and End stage kidney disease (nRIFLE) studies, have been modified from the adult and pediatric population [8]. These definitions, however, are arbitrary and have not been extensively studied to validation [8]. More recently, a multicenter, multinational consortium studied the incidence and the outcomes of neonatal acute kidney injury (AWAKEN study) using the Kidney Disease: Improving Global Outcome (KDIGO) definition, which has also been modified and widely used as the accepted definition in adult and pediatric populations [9••]. Table 1 shows the KDIGO definition of AKI in neonates. This has been used among preterm infants based on the National Institute of Health – National Institute of Diabetes, Digestive and Kidney Diseases (NIH-NIDDK) Neonatal AKI definition working group. This definition, now widely used, has similar issues faced by other definitions that are related to the postnatal changes in SCr and normal level cutoffs of SCr, especially in preterm infants. Though the definition and its staging have been related to mortality and length of stay, as in pediatric and adult populations [9••], it was optimized by comparing the modified KDIGO definition to outcomes based on SCr concentrations and rate of rise of SCr [10]. This enhanced definition showed slight improvements by correlating the absolute and highest SCr increase with outcomes. Nevertheless, this optimization added little clinical value and made the definition more complex.
Epidemiology of AKI in Preterm Infants
Until recently, there have been few case series that have reported the incidence of AKI in preterm neonates, and it varied based on the definition, level of care of the neonatal intensive care unit, and the population selection. It varied from 8 to 24% [5••]. In retrospective data, the incidence of AKI may be spuriously low due to decreased recognition of AKI by the clinician despite high SCr levels. AWAKEN reported the incidence of AKI in < 29-week preterm infants to be 48% and 18% in infants 29 to 35 6/7 weeks gestational age [9••]. This might be the true representation of the incidence of AKI among preterm infants as the inclusion criteria for the study were all the preterm infants admitted in the NICU over a 3-month period. It excluded all with chromosomal aberrations, congenital anomalies of the kidney and those with congenital heart disease that required surgery as these populations are known to be related to a high incidence of AKI.
Another clinical issue that confounds the use of UO for defining AKI in preterm infants is the occurrence of non-oliguric renal failure. Non-oliguric renal failure is defined as per rising SCr concentrations but without decreasing UO as it is > 1 ml/kg/h. The absence of oliguria is related to increased total body water content and decreased tubular functions, leading to less tubular reabsorption and/or a higher glomerular filtration rate. For non-oliguric renal failure, SCr is used to guide for the diagnosis and management of AKI [11].
Risk Factors for AKI in Preterm Infants
Due to the reduced number of nephrons, a less mature renal tubular function, and prolonged stay in the hospital, preterm infants face increased risks for acute kidney injury with evolving risk factors over time. Risk factors of AKI in preterm infants can be further stratified by time. Early AKI occurs within the first 7 days after birth and late neonatal AKI typically occurs after 7 days of life [12•, 13•, 14]. The risk factors classified as those linked to early AKI are typically associated with maternal and perinatal conditions while those in late AKI are associated with events linked to the preterm neonates’ stay in the NICU, specifically events such as sepsis and/or use of nephrotoxic medications. In neonates, the risk of AKI is bimodal, higher in those preterm less than 28 weeks and those near term and at term as compared to gestational ages between 28 and 34 weeks [6, 9••]. In preterm neonates between 28 and 34 weeks, the risk of AKI is low as they have reached a near full complement of nephrons and modern neonatal care prevents major complications associated with this level of prematurity as compared to those born extremely premature before 28 weeks of GA.
Early Risk and Protective Factors in Preterm Infants [12•]
From the largest study on risk factors in preterm infants, several maternal factors such as oligohydroamnios, meconium-stained amniotic fluid, and vaginal mode of delivery were found to have increased risk of early AKI with odds ratios ranging from 1 to 2, though they were not statistically significant after correction for different epidemioloical factors. Moreover, maternal diabetes could influence AKI with associated hypercoagulable state and need for umbilical catheterization. Of the neonatal factors, there is increased risk of early AKI being outborn, large for gestational age, receiving epinephrine and normal saline bolus during resuscitation, having encephalopathy, hyperbilirubinemia, and inborn errors of metabolism. AKI is associated with congenital heart disease (CHD), necrotizing enterocolitis (NEC), kidney abnormalities, and any surgery by an increased odds ratio of 2- to threefold. It is more often diagnosed when admitted to a children’s hospital and when more frequent serum creatinine levels are measured. Maternal hypertensive disease [15] and antenatal steroids have a protective effect against early onset AKI. In this epidemiological study, factors that were associated with decrease AKI risk were use of methylxanthines, antimicrobials, diuretics, and vasopressors [12•]. These associations maybe the reflection of improvement of the patient’s general health because of these medications and hence by improving oxygenation and perfusion to the kidneys rather than the direct effect of the medications themselves.
Late AKI Risk and Protective Factors in Preterm Infants [13•]
Late AKI risk factors were similar to those of early and also included different diagnoses and medication use. The diagnosis associated with increased incidence of late onset AKI on admission were CHD, NEC, and need for surgery while those at discharge were patent ductus arteriosus (PDA), NEC, and sepsis with odds ratios ranging from 1.7 to 4 [13•]. Detailed association of renal injury in the presence NEC [16] and PDA [14] has been described from this cohort. The association is related to the direct effect on the kidneys related to the effect of cytokines, poor oxygenation, and perfusion secondary to the primary disease process. The medicines associated with late onset AKI were diuretics, vasopressors, and NSAIDS, which increase the odds of having AKI by 2- to threefold.
More recently, it was reported that those preterm infants who had early AKI were at higher risk of developing repeat AKI, particularly if the initial AKI was stage 2 or 3 and was within the first few weeks of life [17••].
Associations of AKI with Other Organ Dysfunction
There are significant associations between AKI and chronic lung disease (CLD), intraventricular hemorrhage (IVH), and hypertension (Fig. 1). These associations are stronger with increasing severity of AKI. A possible common mechanism shared among these diseases is increased hypoxia, infection, inflammation, and decreased perfusion which all play a role in the increased morbidity associated with these organs. This dysfunction maybe further affected by decreased kidney function and its associated fluid and electrolyte imbalance which can further worsen CLD, IVH, and hypertension of both systemic and pulmonary circulations. Dependence of kidney function on adequate perfusion and oxygenation make it likely to be directly affected by worsening CLD, IVH, and hypertension.
Continuum of kidney disease from normal kidneys to death. Increased risk factors can lead to AKI which can further deteriorate to failure and death. If managed, there can be a complete recovery. On the contrary, if poorly or not managed at all, chronic renal failure may develop, requiring renal replacement therapy or can lead to death. (Modified from the NKC’s AWAKEN study.) All the stages, at risk, AKI and ARF are associated with different complications such as fluid and electrolyte imbalance, IVH, BPD, and PDA complications, anemia, and recurrent episodes of AKI which can complicate the management of AKI and may be related to increased mortality and morbidities
Recurrent AKI
Recurrent AKI has been previously described as occurring in about one fifth of all AKI cases but no studies have elaborated on the definition of AKI until recently [17••]. The new definition differentiates it from a continuation of initial AKI with recurrent episodes. Since poor outcomes are associated with recurrent AKI, its early recognition may prevent it from becoming worse and prevent increased morbidity and mortality. The incidence among preterm infants with GA < 28 weeks was 24% (40% of the 60% of infants who developed AKI). This was more among those who had early AKI and had a more severe KDIGO staging of AKI. It was also associated with higher mortality and increased length of stay as compared to those with single episode of AKI.
Clinical Presentation in AKI Preterm Infants
The presentation of AKI in preterm infants is similar to term infants but more often, there is no oliguria which makes early recognition difficult and requires a high index of suspicion and frequent serum creatinine measurements [11, 18]. Associated newer early diagnostic markers (see below) and imaging, such as the measurement of renal size and quantification of nephrons, need to be studied in greater detail before a definitive diagnostic criterion can be used to identify early AKI. It is important as there are increasing complications and an increased mortality associated with higher stages of AKI than with lower ones. A recent study showed use of near infrared spectroscopy (NIRS) to assess renal perfusion maybe helpful in early recognition of AKI among preterm infants with renal hypoperfusion [19]. This has been demonstrated in term infants during cardiac postoperative care and in infants being treated with neonatal hypothermia [19].
OMICS in Study of Neonatal AKI
Omics are collective technologies (proteomics, metabolomics, transcriptomics, genomics, and epigenomics) used to study the roles of different molecules that determine phenotype. The interactions of these molecules to form network models are known as systems biology [20, 21]. These approaches may provide an important method for early detection, response to management, and prognosis of AKI in the preterm infant. One of the limitations in the definition of AKI based on the changes in the Scr and UO, is the time lag between SCr increase and renal injury, difficulty in studying the progress of the injury as Cr is also secreted from the renal tubules, inability to differentiate the site of injury in the tubule, and the effect of management on SCr makes it difficult to be used for prognosis [11, 22]. To overcome these issues, proteomics and metabolomics have been used to study novel markers that may be helpful in early diagnosis. Several markers such as kidney injury molecule-1 (KIM-1) [23], neutrophil gelatinase-associated lipocalin (NGAL) [24], and N-acetyl-β-D glucoseaminidase (NAG) [25] have been studied in adult and pediatric populations but data in neonates and specifically in preterm infants have not been established. The advantage of using these molecules as a single marker or as a group [26] is that they are produced in the kidneys and have a baseline value which increases with a specific site of injury and returns to normal when recovery occurs. Injury by specific medications has been related to a very specific urinary metabolic profile, which might help in early recognition and adjustment of the dose to prevent further renal injury [22].
Progression of AKI to CKD
Though firmly established in adult patients and with increasing evidence among the pediatric population, some with AKI develop chronic kidney disease (CKD), this has not been studied in neonates, particularly preterm neonates [27]. Physiological and developmental aspects such as increasing nephron numbers and maturity, disordered repair mechanism, and high risk for AKI make preterm neonates even more susceptible to developing CKD [28•]. Despite the biological plausibility of developing CKD in neonates, especially in preterm neonates, the clinical evidence is equivocal and is dependent on retrospective studies. The association of AKI and CKD requires a planned long-term follow-up study with better predefined starting points of AKI and end points for abnormalities in kidney function. More recently, the quantification of nephrons using cationic ferritin-enhanced MRI would help in identifying those preterm infants with and without AKI who would have a higher risk of developing CKD [29].
Prevention of AKI Among Preterm Infants
Preventing preterm births is the primary prevention of AKI but on a secondary level, early recognition, and correction of factors, both maternal and neonatal that may be associated with AKI is necessary. Tertiary prevention can be achieved by early treatment of the associated co-morbidities as these correlate well with the occurrence and the severity of the AKI. Methylxanthines such as theophylline have been observed to decrease AKI and have been endorsed for use within the first 6 h of hypoxic ischemic encephalopathic infants who are undergoing therapeutic hypothermia [30]. More recently, the early use of caffeine has been associated with a decrease incidence of AKI in preterm infants [31]. These effects can be associated with adenosine receptor antagonism, hence preventing adenosine-induced renal vasoconstriction. Other methods that have been used in adults include remote ischemic reconditioning [32] and use of steroids and erythropoietin [33].
Treatment
Detailed maternal and birth history is needed to identify risk factors in the preterm neonate. Physical examination for neonatal risk factors and strict fluid balance would also help provide clues to the presence and severity of AKI as classified by KDIGO. Though there are no specific markers, SCr can be helpful in defining AKI. Newer markers, as discussed above, and fractional excretion of sodium may also be helpful in the diagnosis, cause, and severity of the disease.
Treatment consists of maintaining careful fluid balance as positive fluid balance is associated with increased morbidities and mortality [34]. Maintaining optimal renal perfusion and eliminating or minimizing risk factors are also treatment goals of AKI. One of the most common risk factors of AKI is continued use of nephrotoxic medication. A recent study revealed that using proactive nephrotoxic injury negated by just-in-time action (NINJA) prevents and/or improves ongoing AKI [35•].
Renal Replacement Therapy
Renal replacement therapy (RRT) remains the primary therapy for the treatment of severe AKI and its complications [36]. Commonly used RRT is peritoneal dialysis (PD), as it does not require a complex procedure to place the catheters and can be performed in small patients (~ 1000 g) depending on the size of the catheter used. Continuous renal replacement therapy (CRRT) is technically more difficult to perform and is limited by the size of the circuit. It is indicated when there are abdominal pathologies associated with AKI or those where the neonate is hemodynamically unstable, especially when there is a fluid imbalance [37]. Recently, some of the machines used for many years in Europe have been approved by the Federal Drug Administration (FDA) for the use in neonates but still are limited weight of 1500 g. Some of these machines are Cardio-Renal Pediatric Dialysis Emergency Machine (Medtronic, Minneapolis MN) [38], Aquadex (CHF solutions, Eden Prairie, MN) [39•], and Newcastle Infant Dialysis and Ultrafiltration System (Newcastle NHS Foundation Trust, Newcastle, UK) [40].
Conclusion
AKI in the preterm infant is a complex disease process that affects and is affected by multiple organs, gestation, and chronological age and is influenced by the intrauterine and extrauterine environment. What is known about AKI in preterm infants is extrapolated from adults and children. Treatment of AKI continues to focus on prevention first followed by fluid balance management, eliminating the offending agent, and lastly resorting to dialysis if the infant’s weight permits. Despite the advancements in the last decade in the knowledge of AKI among preterm infants, more research is required to better define the disease which would allow for early diagnosis, removal/ mitigation of risk factors, management of established disease, and prevention of progression to chronic kidney disease.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Jetton JG, Guillet R, Askenazi DJ, Dill L, Jacobs J, Kent AL, et al. Assessment of worldwide acute kidney injury epidemiology in neonates: design of a retrospective cohort study. Front Pediatr. 2016;4:68. AWAKEN study design.
Drukker A, Guignard JP. Renal aspects of the term and preterm infant: a selective update. Curr Opin Pediatr. 2002;14:175–82.
Rosenblum ND. Developmental biology of the human kidney. Semin Fetal Neonatal Med. 2008;13:125–32.
Vieux R, Hascoet JM, Merdariu D, Fresson J, Guillemin F. Glomerular filtration rate reference values in very preterm infants. Pediatrics. 2010;125:e1186–92.
•• Nada A, Bonachea EM, Askenazi DJ. Acute kidney injury in the fetus and neonate. Semin Fetal Neonatal Med. 2017;22:90–7. Review of AKI and managemnt in infants.
Brophy PDRJ. Functional development of the kidney in utero. 4th ed. Philadelphia: WB Saunders; 2004.
Gouyon JB, Guignard JP. Management of acute renal failure in newborns. Pediatr Nephrol. 2000;14:1037–44.
Sutherland SM, Byrnes JJ, Kothari M, Longhurst CA, Dutta S, Garcia P, Goldstein SL. AKI in hospitalized children: comparing the pRIFLE, AKIN, and KDIGO definitions. Clin J Am Soc Nephrol. 2015;10:554–61.
•• Jetton JG, Boohaker LJ, Sethi SK, Wazir S, Rohatgi S, Soranno DE, et al. Incidence and outcomes of neonatal acute kidney injury (AWAKEN): a multicentre, multinational, observational cohort study. Lancet Child Adolesc Health. 2017;1:184–94. AWAKEN study: description of KDIGO definition and outcomes in infants.
Askenazi D, Abitbol C, Boohaker L, Griffin R, Raina R, Dower J, Davis TK, Ray PE, Perazzo S, DeFreitas M, Milner L, Ambalavanan N, Cole FS, Rademacher E, Zappitelli M, Mhanna M, Neonatal Kidney C. Optimizing the AKI definition during first postnatal week using assessment of worldwide acute kidney injury epidemiology in neonates (AWAKEN) cohort. Pediatr Res. 2019;85:329–38.
Liborio AB, Branco KM. Torres de Melo Bezerra C: Acute kidney injury in neonates: from urine output to new biomarkers. Biomed Res Int. 2014;2014: 601568.
• Charlton JR, Boohaker L, Askenazi D, Brophy PD, D’Angio C, Fuloria M, et al. Incidence and risk factors of early onset neonatal AKI. Clin J Am Soc Nephrol. 2019;14:184–95. Early risk factors in infants.
• Charlton JR, Boohaker L, Askenazi D, Brophy PD, Fuloria M, Gien J, et al. Late onset neonatal acute kidney injury: results from the AWAKEN Study. Pediatr Res. 2019;85:339–48. Late risk factors in infants.
Guillet R, Selewski DT, Griffin R, Rastogi S, Askenazi DJ, D’Angio CT, Neonatal Kidney C. Relationship of patent ductus arteriosus management with neonatal AKI. J Perinatol. 2021;41:1441–7.
DeFreitas MJ, Griffin R, Sanderson K, Nada A, Charlton JR, Jetton JG, et al. Maternal hypertension disorders and neonatal acute kidney injury: Results from the AWAKEN Study. Am J Perinatol. 2022 Feb 25. https://doi.org/10.1055/a-1780-2249.
Bakhoum CY, Basalely A, Koppel RI, Sethna CB. Acute kidney injury in preterm infants with necrotizing enterocolitis. J Matern Fetal Neonatal Med. 2019;32:3185–90.
•• Adegboyega OO, Singh Y, Bhutada A, Kupferman JC, Rastogi S. Recurrent acute kidney injury in preterm neonates is common and associated with worse outcomes and higher mortality. Pediatr Res. 2021 Sep 30. https://doi.org/10.1038/s41390-021-01740-y.
Grylack L, Medani C, Hultzen C, Sivasubramanian K, Davitt MK, Jose P, Scanlon JW. Nonoliguric acute renal failure in the newborn: a prospective evaluation of diagnostic indexes. Am J Dis Child. 1982;136:518–20.
Harer MW, Chock VY. Renal tissue oxygenation monitoring-an opportunity to improve kidney outcomes in the vulnerable neonatal population. Front Pediatr. 2020;8:241.
Kupferman JC, Yitayew M, Rastogi S. Acute kidney injury in term neonates. Curr Treat Options Pediatr. 2018;4(3):386–403.
Riccio S, Valentino MS, Passaro AP, Izzo M, Guarino S, Miraglia Del Giudice E, Marzuillo P, Di Sessa A. New insights from metabolomics in pediatric renal diseases. Children (Basel). 2022;9(1):118.
Askenazi DJ, Koralkar R, Hundley HE, Montesanti A, Parwar P, Sonjara S, Ambalavanan N. Urine biomarkers predict acute kidney injury in newborns. J Pediatr. 2012;161:270-5 e1.
Stojanovic VD, Barisic NA, Vuckovic NM, Doronjski AD, Peco Antic AE. Urinary kidney injury molecule-1 rapid test predicts acute kidney injury in extremely low-birth-weight neonates. Pediatr Res. 2015;78:430–5.
Lavery AP, Meinzen-Derr JK, Anderson E, Ma Q, Bennett MR, Devarajan P, Schibler KR. Urinary NGAL in premature infants. Pediatr Res. 2008;64:423–8.
Jansen D, Peters E, Heemskerk S, Koster-Kamphuis L, Bouw MP, Roelofs HM, van Oeveren W, van Heijst AF, Pickkers P. Tubular injury biomarkers to detect gentamicin-induced acute kidney injury in the neonatal intensive care unit. Am J Perinatol. 2016;33:180–7.
Muhle-Goll C, Eisenmann P, Luy B, Kolker S, Tonshoff B, Fichtner A, et al. Urinary NMR profiling in pediatric acute kidney injury-a pilot study. Int J Mol Sci. 2020 Feb 11;21(4):1187
Greenberg JH, Coca S, Parikh CR. Long-term risk of chronic kidney disease and mortality in children after acute kidney injury: a systematic review. BMC Nephrol. 2014;15:184.
• Chawla LS, Eggers PW, Star RA, Kimmel PL. Acute kidney injury and chronic kidney disease as interconnected syndromes. N Engl J Med. 2014;371:58–66. Conceptual idea of pregression of AKI to CKD.
Baldelomar EJ, Charlton JR, Beeman SC, Bennett KM. Measuring rat kidney glomerular number and size in vivo with MRI. Am J Physiol Renal Physiol. 2018;314:F399–406.
Kellum JA, Lameire N, Group KAGW. Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (Part 1). Crit Care. 2013;17:204.
Harer MW, Askenazi DJ, Boohaker LJ, Carmody JB, Griffin RL, Guillet R, Selewski DT, Swanson JR, Charlton JR, Neonatal Kidney C. Association Between early caffeine citrate administration and risk of acute kidney injury in preterm neonates: results from the AWAKEN study. JAMA Pediatr. 2018;172: e180322.
Gassanov N, Nia AM, Caglayan E, Er F. Remote ischemic preconditioning and renoprotection: from myth to a novel therapeutic option? J Am Soc Nephrol. 2014;25:216–24.
Askenazi DJ, Heagerty PJ, Schmicker RH, Brophy P, Juul SE, Goldstein SL, et al. The Impact of erythropoietin on short- and long-term kidney-related outcomes in neonates of extremely low gestational age. results of a multicenter, double-blind, placebo-controlled randomized clinical trial. J Pediatr. 2021;232:65–72 e7.
Selewski DT, Gist KM, Nathan AT, Goldstein SL, Boohaker LJ, Akcan-Arikan A, Bonachea EM, Hanna M, Joseph C, Mahan JD, Mammen C, Nada A, Reidy K, Staples A, Wintermark P, Griffin R, Askenazi DJ, Guillet R, Neonatal Kidney C. The impact of fluid balance on outcomes in premature neonates: a report from the AWAKEN study group. Pediatr Res. 2020;87:550–7.
• Stoops C, Stone S, Evans E, Dill L, Henderson T, Griffin R, et al. Baby NINJA (Nephrotoxic Injury Negated by Just-in-Time Action): Reduction of nephrotoxic medication-associated acute kidney injury in the neonatal intensive care unit. J Pediatr. 2019;215:223–8 e6. Recognition and prevention of AKI by medications among infants.
Kaddourah A, Goldstein SL. Renal replacement therapy in neonates. Clin Perinatol. 2014;41:517–27.
Sanderson KR, Harshman LA. Renal replacement therapies for infants and children in the ICU. Curr Opin Pediatr. 2020;32:360–6.
Ronco C, Garzotto F, Brendolan A, Zanella M, Bellettato M, Vedovato S, Chiarenza F, Ricci Z, Goldstein SL. Continuous renal replacement therapy in neonates and small infants: development and first-in-human use of a miniaturised machine (CARPEDIEM). Lancet. 2014;383:1807–13.
• Raina R, McCulloch M, Nourse P, Sethi SK, Yap HK. Advances in kidney replacement therapy in infants. Adv Chronic Kidney Dis. 2021;28:91–104. CRRT in infants.
Coulthard MG, Crosier J, Griffiths C, Smith J, Drinnan M, Whitaker M, Beckwith R, Matthews JN, Flecknell P, Lambert HJ. Haemodialysing babies weighing <8 kg with the Newcastle infant dialysis and ultrafiltration system (Nidus): comparison with peritoneal and conventional haemodialysis. Pediatr Nephrol. 2014;29:1873–81.
Author information
Authors and Affiliations
Contributions
SR had the idea for the article; SR and BM-B performed the literature search, drafted, and critically revised the work.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Renal
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Massa-Buck, B., Rastogi, S. Recent Advances in Acute Kidney Injury in Preterm Infants. Curr Pediatr Rep 10, 165–171 (2022). https://doi.org/10.1007/s40124-022-00271-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40124-022-00271-2