Abstract
Purpose of Review
We reviewed recently published literature around the care of transgender and gender-nonconforming youth. In this nascent area of medicine, there are few randomized controlled trials, but there are treatment guidelines that include expert opinion and best practices for a more standardized approach to care.
Recent Findings
The most significant article published the past year is the updated standards of care—“Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent Persons: An Endocrine Society Clinical Practice Guideline”—which establishes a care framework with special emphasis on the importance of interdisciplinary care. However, there are several other important articles that review health-care utilization and outcomes after treatment in the transgender population.
Summary
As gender dysphoria and nonconformity become more visible and prevalent, health-care providers will deliver care for these patients and will need to understand common health concerns and treatment options. The ability to provide culturally competent and appropriate care can improve psychosocial outcomes for these patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Gender dysphoria and gender nonconformity (TGN) are not new conditions, but recently, public awareness has increased. Previously known as gender identity disorder and transsexualism, new definitions associated with this condition are reviewed in Table 1. Treatment guidelines, including those from the World Professional Association for Transgender Health (WPATH) and the Endocrine Society, have been published since 1979. The most recent WPATH guidelines were updated in 2012, and the Endocrine Society Clinical Practice guideline was revised in late 2017 [1•, 2••]. As awareness and prevalence have increased, health-care providers are more likely to be offering care to this population. This nascent area of medicine has little evidence-based guidance and care is often based on expert opinion. This literature review will review the current practice guidelines and other supporting evidences to assist providers in understanding the specific health-care needs of this population. Competence in the care of TGN youth decreases barriers to care and can improve health outcomes for this population.
Prevalence
The prevalence of TGN youth is difficult to determine due to a lack of standardized definitions, nonbinary categories, and some fluidity of the condition. Health-care providers are not routinely asking about gender or gender experiences, and these may be sensitive questions that youth do not feel comfortable answering, especially in front of their caregivers.
The Williams Institute, using data from the CDC’s Behavioral Risk Factor Surveillance System in 2014, found that 0.6% of US adults (1.4 million) identify as transgender. They found that younger people, ages 18–24, had higher rates, at 0.7% [3].
In a study in the Netherlands, mothers completed the Child Behavior Checklist to assess for cross-gender behavior. Prevalence of behaving like or wishing to be of the opposite sex ranged from 3.2 to 5.7% for 7-year-olds and decreased to 2.4 to 3.3% in 10-year-olds [4]. This decrease is not surprising, as we know that for many young people, gender can be fluid and can change over time.
In 2012, the Human Rights Campaign completed an online survey where self-selected students (ages 13–17) responded, and of the 10,000 respondents, 9% reported being transgender or gender nonconforming [5].
In 2015, the Gay Lesbian Straight Education Network (GLSEN) reported the results of their annual National School Climate Survey. Of the 10,000 self-selected participants, ages 13–21, 15.2% described themselves as transgender, 11.4% described themselves as genderqueer, and 11.7% described themselves as another gender (agender, gender fluid, etc.) [6].
Stability of Gender Identity over Time
Gender is often seen as binary (male or female) and static, but many children and adolescents may be more gender fluid and may change their gender identification over time. Youth who are TGN are thought to follow one of two natural courses—they either persist (continue with their gender variance), or desist (revert back to natal gender). Rates of persistence can be difficult to determine, and wide ranges have been reported. Persistence of TGN identity in natal males ranges from 2.2 to 30%, and in natal females from 12 to 50%. It is known that most children ages 5–12 years who are diagnosed with gender dysphoria do not persist as adolescents, and no longer consider themselves transgender. For children who desist, 63 to 100% of natal males will identify as gay, and 32 to 50% of natal females will identify as lesbian [7, 8].
From our clinical observations, many caregivers of TGN youth have reviewed these statistics and are hopeful that their child is going through a phase and will desist. However, we are finding that, perhaps due to self-selection (family finding the issue serious enough to seek care), most of the patients that we see in our clinic do not desist.
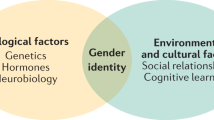
Etiology
Etiology of gender dysphoria is thought to be multifactorial with biologic, social, and psychological factors playing a part in the development of gender identity. Some evidences from brain neuroimaging studies show that adolescents with gender dysphoria have structural characteristics resembling peers of their preferred gender [9]. Genetic factors may also contribute to gender development [10]. There are also thoughts about the hormonal influences that may occur in utero, which have been studied with disorders of sexual development [11]. Environmental factors, such as social relationships and cultural norms, may also play a part in gender development and expression.
Clinically, when we speak to families, we discuss the fact that gender identity is not a choice. When reviewing family history, our team asks if anyone in the family is lesbian, gay, bisexual, or transgender, and say that we are asking because we know that just like other heritable conditions (hypertension, asthma, etc.), these conditions run in families as well. We also specifically tell caregivers that there is no evidence that parenting style, abuse, or other events influence sexual orientation or gender, as sometimes parents worry that they did something wrong.
Presentation
Children can present as transgender or gender nonconforming when they are very young, and we commonly hear that they have known they were transgender, “their whole life.” Parents will often state that they have always known their young child was another gender. We know children as young as the age of 2 can label themselves as a boy or girl, and can describe their own and other’s gender. By age 4, they are able to use gendered words—he/him and she/her. Some children are quite clear about their gender identity, and say, “I am a girl” instead of, “I wish I were a girl.” Others may have more difficulty verbalizing or conceptualizing their gender, and may present with mood or behavior problems.
Our clinical approach for younger children is to view the development of gender identity as flexible and fluid and as a normal part of exploration of cultural roles. We screen for gender experiences and ask families of these children about the child’s preferred style of dress (including underwear and swimwear), bathroom behavior, and choice of toys. Families often ask if gender dysphoria is a phase, and we explain that we are looking for the child to be consistent, insistent, and persistent to let us know that it is not. We find that even young children, when asked directly, are usually able to tell us if they are a boy or a girl. For the most part, our team works with the patient and family to let the child take the lead in their self-expression (the way they dress, their interests, etc.).
For older children and adolescents, knowledge of their gender and presentation may occur separately. They often present around the time of or just after puberty. Some give a history of knowing that something was different, but it took time for them to figure out what it was. Many do not tell family members when they do determine that they are transgender, but may wait to come out when they feel safe.
Our clinical approach for older children and adolescents is to ask about several milestones in the history. We ask about how long they have known they were TGN, and how long their families have known. We ask if the patient considers themselves male, female, somewhere in between, or some other gender. We also ask who they are attracted to (males, females, everyone, no one, if they are unsure, or have other attractions). Finally, we ask about sexual experiences, as gender identity and expression, sexual attraction, and sexual activity may be different for each person. Children and adolescents who have gender dysphoria are often anxious or frightened about the physical exam, especially if a genital exam is needed. We find that it may require extra time and effort for them to be more comfortable, and we may not do the more sensitive parts of the exam at the first visit.
In our experience, we feel that the most important thing that we have done is to create a safe environment for our patients and their families so they feel comfortable discussing sensitive issues. We make sure our paperwork is inclusive and provides more than just male/female options when asking about sex. We are continually training our staff to make sure they are asking for and using the correct pronouns and preferred name. One small study found that youth who were able to use their chosen name reported fewer depressive symptoms and less suicidal ideation, as it was affirming to their gender identity [12].
Common Health Issues
Transgender and gender-nonconforming youth face numerous health concerns, and some are related to their gender identity. Very few LGBTQ youth (16% in one study) have discussed their sexual orientation or gender identity with their health-care provider [5].
Compared to cisgender youth, TGN youth have significantly poorer health and lower rates of preventive care and are more likely to report their general health as poor, fair, or good as opposed to very good or excellent [13•].
Risk of victimization is common, including being bullied, harassed, and physically and emotionally abused, at home, at school, and in the community [14]. These youth are at risk for family rejection and may end up homeless or in the foster care system. Health concerns that may be related to homelessness and extreme poverty include higher rates of substance abuse and HIV and other sexually transmitted infections. Patients may postpone medical care or be unable to afford it [14]. Higher levels of family rejection during adolescence have been linked to negative health outcomes for LGBTQ youth, while family acceptance has a protective effect [14].
Mental health issues include anxiety, depression, self-harm, and eating disorders (both anorexia nervosa and morbid obesity) [15, 16]. TGN youth have higher rates of depression, suicidality, and self-harm [5, 6, 15]. One matched retrospective cohort study found that transgender youth had a twofold to threefold increased risk of depression, anxiety disorder, suicidal ideation, suicide attempt, and self-harm without lethal intent [16].
The most concerning health issue for TGN youth is risk of suicide attempt. One study of TGN adults found that 41% had attempted suicide, compared to 1.6% of the general population [17].
Another study of TGN youth presenting for gender dysphoria found that 20% had moderate to severe depression, 51% had thought about suicide, and 30% had attempted suicide [18].
Racial and ethnic minority TGN youth have higher rates of the aforementioned health concerns due to both transphobia and racism [19].
It is not uncommon to see patients with a diagnosis on the autism spectrum (ASD) who also have gender dysphoria or are gender nonconforming. One retrospective chart review found that parents of children with an ASD diagnosis were 7.76 times more likely to report gender variance than parents of a sample of children without autism [20].
In our clinical experience, we discuss mood at every visit and make sure that we are assessing for body image concerns, risk for sexually transmitted infections, and substance abuse at regular intervals. We also evaluate all of the environments that the patient is in and assess for safety concerns, bullying, and violence.
Treatment
There is an increasing demand for safe and effective multidisciplinary care of transgender youth who experience gender dysphoria based upon incongruence between sex assigned at birth and gender identity. Recommendations call for patients to be followed by a team consisting of primary care providers, mental health providers, and subspecialists (including endocrinologists, gynecologists, and adolescent medicine providers) who are knowledgeable about the use of medications to assist with transition.
Social Transition
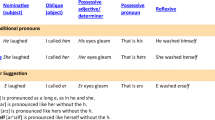
Social transitioning is externally presenting in one’s authentic gender. For example, a child who was assigned male at birth (AMAB) may socially transition to appear more feminine, by growing her hair out, wearing more feminine clothing, going by a more feminine name, and using female pronouns (she, her, hers). This transition is entirely reversible if the child desists. There are no long-term outcome studies on use of social transition with gender dysphoria [1•, 2••].
For younger children, social transition is the only recommended treatment. There is no medical intervention for the young child until they progress through puberty to Tanner II or III. Children may work with a therapist to help explore gender, and support and resources are provided for the patient and caregivers.
Medical Transition
Medical management of gender dysphoria includes suppression of endogenous sex hormone secretion and administration of affirming hormone therapy to influence secondary sex characteristics and establish hormone levels more congruent with experienced gender.
In recognition of emerging evidence and evolving trends in clinical practice and care of transgender youth and adults, the Endocrinology Society recently updated the Clinical Practice Guidelines, Endocrine Treatment of Gender dysphoria/Gender-incongruent Persons [2••]. These guidelines detail updated consensus from 2009 and reflect the existing strength of recommendations based on available evidence commissioned from two systematic reviews.
In our clinical experience, although initiation of hormone treatment is not recommended for pre-pubertal children, our pediatric endocrinologist often meets with families of younger children to provide anticipatory guidance about the typical timing and tempo of puberty. For children who have expressed gender dysphoria or gender incongruence at a young age, there is an opportunity to meet with a family to counsel on potential benefits, risks, and limitations of puberty-blocking options.
Puberty Blockade
Between the ages of 8–12 for patients assigned female at birth (AFAB) and ages 9–13 for patients assigned male at birth (AMAB) who have identified as gender incongruent, it is reasonable for an annual physical exam including pubertal staging to be performed by either a primary care physician or endocrinologist. Adolescents who meet diagnostic criteria for gender dysphoria/gender incongruence fulfill criteria for treatment, and who request treatment should be considered as candidates for gonadotropin-releasing hormone (GnRH) analogue (leuprolide acetate or histrelin in the USA), to suppress endogenous puberty after exhibiting physical signs of puberty consistent with Tanner II staging or beyond. Suppression of endogenous puberty with a reversible GnRH agonist allows for social transitioning, time for maturation, and ongoing exploration of gender identity without the distress of developing secondary sexual characteristics that are incongruent with self-identity. This treatment is felt to be completely reversible.
Duration of treatment with GnRH varies depending upon age and pubertal stage at presentation, but frequently can last multiple years. During this interval, the patient is monitored for physical signs of adequate pubertal suppression, evaluated for bone age to help determine predicted adult height, which can be of importance to adolescents wishing to pass as their affirmed gender as adults. Bone mineral density is monitored by DXA, and the patient is encouraged to obtain adequate weight-bearing exercise and vitamin D to mitigate any potential adverse impact on bone health.
Non-intervention is not a neutral option—if families are not able to decide if they want to start puberty blockers—they have essentially decided to let the child go through the puberty of the gender they were assigned at birth, with which they do not identify [1•, 2••].
Gender-Affirming Hormone Therapy
The decision to initiate gender-affirming hormone therapy (GAHT) should follow evaluation by a multidisciplinary medical and mental health-care team that has confirmed persistence of gender dysphoria and sufficient capacity to give informed consent. Given that GAHT causes some bodily changes that are only partially irreversible (e.g., voice changes after exposure to testosterone), a thorough discussion of expectations is indicated prior to the initiation of treatment. Adolescents should be informed of the predicted onset of common changes and usual duration to see the full effects of feminizing or masculinizing treatments. Additionally, potential consequences for future fertility and options for fertility preservation should be discussed. Notable changes in the updated Endocrine Society guidelines include recognition that even in the face of minimal published studies of GAHT administered in younger adolescents (13–14 years), there may be compelling reasons to initiate sex hormone therapy in some adolescents prior to age 16, in part due to potential for psychosocial adverse impact of prolonged delay of puberty [2••].
For induction of puberty in transgender youth, clinicians can follow a gradually increasing dose plan, similar to that for cisgender adolescents with hypogonadism (e.g., such as premature ovarian insufficiency in Turner syndrome girls). For some individuals, puberty blockade will be continued while a slow progression of GAHT proceeds to mimic as close as possible to an endogenous tempo of puberty. Dosing may be individualized depending upon specific clinical considerations such as low bone density for age or adult height prediction. Ongoing clinical follow-up with physical exam including monitoring of growth and development of desired secondary sexual characteristics every 3–6 months as well as intermittent laboratory evaluation every 6–12 months is indicated. Once physiologic hormone levels are achieved, GnRH analogues can be discontinued because GAHT will suppress the endogenous hypothalamic-gonadal axis. For patients AFAB, menstrual suppression and contraception are important considerations of a comprehensive treatment plan. Once adult height is achieved and transgender individuals are on a stable hormone regimen, frequency of office visits and laboratory evaluations decreases.
Despite growing evidence and standards of care, there are financial barriers for medical care related to transgender health based upon frequent insurance denials, particularly for GnRH analogues [1•, 2••]. Therefore, cost-effective treatment paradigms are a relevant consideration and advocacy is often required to ensure individuals have access to treatments that provide optimal physical outcomes and promote psychological well-being.
In the USA, GAHT that is usually prescribed for patients desiring more masculine attributes is testosterone, by injection or the transdermal route. Those patients who desire more feminine attributes are estrogen (orally, transdermal, via injection), usually with an antiandrogen such as oral spironolactone. Estrogen is given either orally or transdermally. Physical changes in those using testosterone include cessation of menses, increased facial and body hair, increased muscle mass, deepening of the voice, and clitoromegaly. Physical changes in those using estrogen include decreased facial and body hair, breast tissue growth, and decreased spontaneous erections [1•, 2••].
Menstrual Management/Suppression
Discussing the psychologic and physical impact of menstruation is important as menses may be associated with significant anxiety. In some patients with gender dysphoria, depressive symptoms and self-harming behaviors may peak during menstrual bleeding [21]. Hormonal options for menstrual lightening or suppression should be discussed and offered for those who desire it [22]. Realistic goals and expectations should be discussed with any patient seeking menstrual management options and complete amenorrhea should not be guaranteed as it may be difficult to achieve [23]. Although menstrual management is a common presenting concern, data on menstrual suppression for this population are lacking [21].
In our clinical practice, progestin-only options including progesterone-only pills, depot medroxyprogesterone acetate (DMPA) injections, or progestin intrauterine system (IUS) are often used. We often recommend the 52 mg levonorgestrel-containing IUS for menstrual management in this population, especially when they are in need of reliable contraception. We have generally avoided the use of the etonorgestrel subdermal implant due to the unpredictable bleeding profile among users. Depending on patient preference and medical history, estrogen-containing options such as combined hormonal contraceptives may also be acceptable [22]. When a patient desires a combined hormonal contraceptive pill, we usually prescribe a 3-month extended cycle product for menstrual suppression.
For adolescents who have met criteria for gender-affirming hormone treatment with testosterone, cessation of menses is typically achieved within 6 months and greater than 90% will achieve complete amenorrhea by 1 year [21, 24].
Surgical methods of menstrual suppression include endometrial ablation and hysterectomy. Endometrial ablation is not recommended in adolescents due to the high failure rate, the overall lack of data in adolescents, and the increased risk if subsequent pregnancy occurs [23]. Hysterectomy is a definitive option for the elimination of uterine bleeding and may be performed abdominally, laparoscopically, robotically, or transvaginally [25]. However, if considered solely for the purpose of menstrual suppression, it is not recommended due to the comparatively high risk of morbidity and mortality compared to other available hormonal methods [23]. Moreover, it is recommended that the patient be the age of majority before hysterectomy is considered [1•, 2••].
Surgery
A variety of gender-affirming surgical options are available for transgender men and women including chest surgery (mastectomy or breast augmentation), gonadectomy, genital surgery including hysterectomy, facial surgery, and other cosmetic procedures such as tracheal shave [26]. Studies have supported the safety and feasibility of these surgical procedures in the transgender population [26,27,28,29,30,31]. It has been shown that among adults who seek gender-affirming surgery, the percentage of patients who go on to regret the procedure is low with rates regret reported in less than 1% of patients [32]. Although exact estimates are difficult to obtain, the prevalence of surgical management is thought to be low. One retrospective review of 99 patients found that only 35% of patients had undergone at least one gender-affirming surgery with few patients opting for genital surgery or gonadectomy [26].
For adolescents, mastectomy may be considered and performed prior to the age of 18, but genital surgery be considered after the patient is a legal adult [1•, 2••, 22]. Since surgery is considered irreversible, it is recommended that variance from the treatment guidelines must be done with extreme caution and involve a thorough discussion of ethical principles of performing irreversible surgical procedures on minors [33].
In our clinical practice, families are concerned about the irreversibility of mastectomy, and often want to delay this procedure until the adolescent is an adult. However, a recent study found that chest dysphoria was higher for those who had not had this surgery, and regret was negligible [34].
Fertility
As transgender youth face potential infertility as a result of medical treatments intended to facilitate transition to their affirmed gender, guidelines recommend discussing fertility prior to initiating the initiation of puberty blockers, gender-affirming hormones, and surgical management [2••, 35]. The effects of gender-affirming hormone therapy on natal gonads are not completely understood and appear partially reversible. The threshold for which fertility is impaired is unknown. Although reversible, GnRHa prevents maturation of oocytes and spermatogonia. Estrogen use may lead to impairment of spermatogenesis and an absence of Leydig cells, and testosterone use may result in ovarian stromal hyperplasia and follicular atresia [2••, 35]. Current established options for fertility preservation are sperm banking and embryo/oocyte cryopreservation. Ovarian tissue and testicular tissue cryopreservation are experimental options which are currently being investigated only under research protocols [35].
Although many transgender adults express desire for biological children and fertility preservation had it been offered, fertility desires among adolescents are less straightforward [36,37,38]. The limited studies available on fertility desires and parenthood goals for transgender youth reveal knowledge of fertility risks associated with treatment, with low rates of fertility preservation utilization and overall lack of desire for biological children [39,40,41]. However, it is unclear if the desire for family building changes later in life, as the adolescent matures or after transitioning to their affirmed gender [38]. Furthermore, it is unknown what role perceived or actual barriers may play in fertility desires for TGN youth. It is known that cost is often prohibitive, as in many cases, insurance coverage is not available for often pricey fertility preservation options, particularly for transgender males. In addition, the increased stress that may be associated with a delay in initiating gender-affirming hormones, the process for ovarian stimulation and oocyte retrieval, or the act of sperm extraction or masturbation should be considered [35].
In our clinical practice, we discuss fertility at each visit, and we often find that patients and their caregivers have differing opinions on fertility preservation. In our experience, many patients state that they do not desire biological children, while parents often request more information on available options. Due to cost and the invasiveness of the procedure, we have had more AMAB patients complete sperm banking than AFAB patients who have completed oocyte preservation.
Outcomes
One recent cohort study looked at the association between gender-affirming treatments and perceived gender congruence, body image satisfaction, and mental health in an adult transgender population. They found that gender congruence and body image satisfaction were higher in those people who had had more gender-affirming treatment, and levels of anxiety and depression were lower in this group [42••].
Outcome data are lacking for gender transition in young people, but one small study from the Netherlands followed 55 young transgender adults through their transitions. They were assessed prior to pubertal suppression, at the start of gender-affirming hormones, and at least 1 year after surgery. Gender dysphoria had resolved, psychological functioning had improved, and well-being was similar to or better than cisgender peers [43•].
There are more data surrounding social support of transgender youth. Unsurprisingly, these studies have found that parental support and acceptance can decrease negative health outcomes, such as suicide and HIV. Family acceptance predicts better general health and protects against depression, substance abuse, and suicide [5, 44•].
Conclusions
As pediatric providers begin to see more transgender and gender-nonconforming children and adolescents in their practices, it is important to be knowledgeable about this condition in order to provide culturally competent care. Although there is not robust evidence on outcomes, there are recently updated clinical guidelines that were developed using evidence-based research and expert opinion to define a standard of care. Providers should be aware that transgender youth may present for health care, but may not disclose their gender identity unless they are asked, and should recognize common health concerns and barriers to care for these individuals. As supporting evidence suggests, we should continue to discuss menstrual suppression and fertility on a regular basis. As this is a nascent area of medicine, the current literature is suggesting that we follow the treatment guidelines, but closely assess the individual needs of each patient to maximize health.
References
Papers of particular interest, published recently, have been highlighted as: •Of importance, ••Of major importance
• Coleman E, Bockting W, Botzer M, et al. Standards of care for the health of transsexual, transgender and gender-nonconforming people, version 7. Int J Transgend. 2012;13(4):165–232. Treatment guidelines from WPATH (World Professional Association for Transgender Health).
•• Hembree WC, Cohen-Kettenis PT, Gooren L, Hannema SE, Meyer WJ, Murad MH, et al. Endocrine treatment of gender-dysphoric/gender-incongruent persons: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2017;102(11):3869–903. Most current guidelines for treatment of transgender persons
Flores AR, Herman JL, Gates GJ, Brown TNT. How many adults identify as transgender in the United States? The Williams Institute. 2016. Available at: https://williamsinstitute.law.ucla.edu/wp-content/uploads/How-Many-Adults-Identify-as-Transgender-in-the-United-States.pdf. Accessed May 8, 2018.
van Beijsterveldt CE, Hudziak JJ, Boomsma DI. Genetic and environmental influences on cross-gender behavior and relation to behavior problems: a study of Dutch twins at ages 7 and 10 years. Arch Sex Behav. 2006;35(6):647–58.
Human Rights Campaign. Growing up LGBT in America. In: May; 2012.
Kosciw JG, Greytak EA, Giga NM, Villenas C, Danischewski DJ. The 2015 National School Climate Survey: the experiences of lesbian, gay, bisexual, transgender, and queer youth in our nation’s schools. New York: GLSEN; 2016.
American Psychiatric Association. (2013). Gender dysphoria. In Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing, 2013; https://doi.org/10.1176/appi.books.9780890425596.dsm14.
Steensma TD, Biemond R, de Boer F, Cohen-Kettenis PT. Desisting and persisting gender dysphoria after childhood: a qualitative follow-up study. Clin Child Psychol Psychiatr. 2011;16(4):499–516.
Hoekzema E, Schagen SE, Kreukels BP, et al. Regional volumes and spatial volumetric distribution of gray matter in the gender dysphoric brain. Psychoneuroendocrinology. 2015 May;55:59–71.
Green R. Family co-occurrence of gender dysphoria: ten sibling or parent-child pairs. Arch Sex Behav. 2000;29:499–507.
Bao A-M, Swaab DF. Sexual differentiation of the human brain: relation to gender identity, sexual orientation and neuropsychiatric disorders. Front Neuroendocrinol. 2011;32:214–26.
Russell ST, Pollitt AM, Li G, et al. Chosen name use is linked to reduced depressive symptoms, suicidal ideation, and suicide behavior among transgender youth. J Adolesc Health. 2018; https://doi.org/10.1016/j.jadohealth.2018.02.003.
• Rider GN, BJ MM, Gower AL, et al. Health and care utilization of transgender and gender nonconforming youth: a population-based study. Pediatrics. 2018;141(3):e20171683. This article reviews variability in health care use based on gender identity.
Grant J, Mottet L, Tanis J, et al. Injustice at every turn: a report of the national transgender discrimination survery. Washington DC: National Center for Transgender Equality and National Gay and Lesbian Task Force; 2011.
Connolly MD, Zervos MK, Barone CJ, et al. The mental health of transgender youth: advances in understanding. J Adolesc Health. 2016 Nov;59(5):489–95.
Reisner SL, Vetters R, Leclerc M, Zaslow S, Wolfrum S, Shumer D, et al. Mental health of transgender youth in care at an adolescent urban community health center; a matched retrospective cohort study. J Adolesc Health. 2015 Mar;56(3):274–9.
Haas A, Rodgers P, Herman J. Suicide attempts among transgender and gender non-conforming adults: findings of the National Transgender Discrimination Survey. Los Angeles: UCLA, Williams Institute and American Foundation for Suicide Prevention; 2014.
Olson J, Schrager SM, Belzer M, Simons LK, Clark LF. Baseline physiologic and psychosocial characteristics of transgender youth seeing care for gender dysphoria. J Adolesc Health. 2015 Oct;57(4):374–80.
Singh AA. Transgender youth of color and resilience: negotiating oppression and finding support. Sex Roles. 2013 Jun;68(11):690–702.
Janssen A, Huang H, Duncan C. Gender variance among youth with autism spectrum disorders: a retrospective chart review. Transgend Health. 2016;1:63–8.
Carswell J, Roberts S. Induction and maintenance of amenorrhea in transmasculine and nonbinary adolescents. Transgend Health. 2017;2(1):195–201.
Committee on Adolescent Health Care. Care for transgender adolescents. Committee Opinion No 685. Obstet Gynecol. 2017;129:e11–6.
Committee on Adolescent Health Care. Committee Opinion No. 668: menstrual manipulation for adolescents with physical and developmental disabilities. Obstet Gynecol. 2016;128:e20–5.
Ahmad S, Leinung M. The response of the menstrual cycle to initiation of hormonal therapy in transgender men. Transgend Health. 2017;2:176–9.
ACOG Committee Opinion No. 701 Summary: Choosing the route of hysterectomy for benign disease. Obstet Gynecol. 129(6):1149–1150.
Kailas M, Lu HMS, Rothman EF, Safer JD. Prevalence and types of gender-affirming surgery among a sample of transgender endocrinology patients prior to state expansion of insurance coverage. Endocr Pract. 2017;23(7):780–6.
Buncamper ME, van der Sluis WB, de Vries M, Witte BI, Bouman MB, Mullender MG. Penile inversion vaginoplasty with or without additional full-thickness skin graft: to graft or not to graft? Plast Reconstr Surg. 2017;139(3):649e–56e.
Cizek S, Nguyen N, Lyon L, Zaritsky E, Weiss E. Combined hysterectomy and mastectomy surgery for transgender patients in an integrated health care setting. Int J Transgend. 2017;18:382–8.
Obedin-Maliver J, Light A, de Haan G, Jackson RA. Feasibility of vaginal hysterectomy for female to male transgender men. Obstet Gynecol. 2017;129:457–63.
Capitan L, Simon D, Meyer T, et al. Facial feminization surgery: simultaneous hair transplant during forehead reconstruction. Plast Reconsty Surg. 2017;139(3):573–84.
Papadopulos NA, Zavlin D, Lelle JD, et al. Male to female sex reassignment surgery using the combined technique leads to increased quality of life in a prospective study. Plast Reconstr Surg. 2017;140(2):286–94.
Wiepejes CM, Nota NM, de Blok CJM, et al. The Amsterdam cohort of gender dysphoria study (1972-2015): trends in prevalence, treatment and regrets. J Sex Med. 2018;15(4):582–90.
Milrod C. How young is too young: ethical concerns in genital surgery of the transgender MTF adolescent. J Sex Med. 2014;11(2):338–46.
Olson-Kennedy J, Warus J, Okonta V, et al. Chest reconstruction and chest dysphoria in transmasculine minors and young adults—comparisons of nonsurgical and postsurgical cohorts. JAMA Pediatr. 2018; https://doi.org/10.1001/jamapediatrics.2017.5440.
Finlayson C, Johnson E, Chen D, et al. Proceedings of the working group session on fertility preservation for individuals with gender and sex diversity. Transgend Health. 2016;1:99–107.
Wierckx K, Caenegem E, Pennings G. Reproductive wish in transsexual men. Hum Reprod. 2012;27:483–7.
De Roo C, Tilleman K, T’Sjoen G, et al. Fertility options in transgender people. Int Rev Psychiatry. 2016;28:112–9.
Nahata L, Tishelman AC, Caltabellotta NM, Quinn GP. Low fertility preservation utilization among transgender youth. J Adolsc Health. 2017 Jul;61(1):40–4.
Chen D, Simons L, Johnson E, et al. Fertility preservation for transgender adolescents. J Adolesc Health. 2017;6:120–3.
Strang J, Jarin J, Call D, et al. Transgender youth fertility attitudes questionnaire: measure development in nonautistic and autistic transgender youth and their parents. J Adolesc Health. 2018 Feb;62(2):128–35.
Chen D, Matson M, Macapagal K, et al. Attitudes toward fertility and reproductive health among transgender and gender-nonconforming adolescents. J Adolesc Health. 2018; https://doi.org/10.1016/j.jadohealth.2017.11.306.
•• Owen-Smith AA, Gerth J, Sineath RC, et al. Association between gender confirmation treatments and perceived gender congruence, body image satisfaction, and mental health in a cohort of transgender individuals. J Sex Med. 2018;15(4):591–600. Larger study of the correlation between medical intervention and outcomes for transgender adults.
• de Vries AL, McGuire JK, Steensma TD, et al. Young adult psychological outcome after puberty suppression and gender reassignment. Pediatrics. 2014;134(4):696–704. First description of transition outcomes for transgender youth
• Ryan C, Russell ST, Huebner D, et al. Family acceptance in adolescence and the health of LGBT young adults. J Child Adolesc Psychiatr Nurs. 2010;23(4):205–13. Description of best practices for suicide prevention in sexual minority youth.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Adolescent Medicine
Rights and permissions
About this article
Cite this article
Conard, L.A.E., Corathers, S.D. & Trotman, G. Caring for Transgender and Gender-Nonconforming Youth. Curr Pediatr Rep 6, 139–146 (2018). https://doi.org/10.1007/s40124-018-0173-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40124-018-0173-8