Abstract
Purpose of Review
The purpose of this paper is to review the presentation, mechanism and acute management of pediatric tachyarrhythmias and to discuss current updates in the literature.
Recent Findings
In 2015, the AHA updated the PALS guidelines to include lidocaine as a first line agent alongside amiodarone in the management of ventricular tachycardia. A recent study re-addressed the safety of the use of adenosine on heart transplant patients with supraventricular tachycardia (SVT). Also, there have been recent studies which explored alternative prevention modalities for postoperative junctional ectopic tachycardia such as the use of dexmedetomidine and higher magnesium levels.
Summary
This review discusses the mechanism, presentation, and management of pediatric tachyarrhythmias. It focuses on SVT, as it is the most common cardiac arrhythmia in children requiring intervention, but also discusses other life-threatening arrhythmias including ventricular arrhythmias and Wolff-Parkinson-White syndrome. It reviews the current updates in acute management and discusses future directions of prophylactic management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tachyarrhythmias in the pediatric population are common and can be life-threatening. Supraventricular tachycardia (SVT) is the most common cardiac arrhythmia in infants and children requiring intervention, occurring in up to 1 in 250 children [1,2,3,4]. “SVT” is a catch-all term that describes several types of arrhythmias arising from above the ventricles that have different physiologies and treatment strategies. The purpose of this article is to discuss the presentation of SVT, differentiate the various types, and discuss their acute management and epidemiology. We will also discuss the different mechanisms of tachyarrhythmias, specifically automatic versus pathway mediated, since that will play a role in guiding management. We will briefly discuss Wolff-Parkinson-White syndrome (WPW), which may present during childhood, and ventricular arrhythmias, which are uncommon in pediatrics but have a high risk of mortality. Lastly, we will review recently published literature regarding arrhythmia management and future directions.
Presentation
Presentation of pediatric tachyarrhythmias varies depending on age. Pediatric primary care providers and emergency room physicians are on the forefront of recognition and initial management of these patients, and pediatric critical care physicians must be able to recognize new arrhythmias and continue management of previously recognized arrhythmias in their critically ill population. Symptoms in infants are often nonspecific and may include poor feeding, tachypnea, irritability, and excessive crying [2]. Abdominal pain may be the only presenting symptom of SVT in young children, likely secondary to sustained arrhythmia leading to biventricular heart failure and poor cardiac output to the splanchnic and hepatic circulation. Older children will likely present with chest pain, palpitations, lightheadedness, pallor, or diaphoresis. These episodes are often paroxysmal, with a mean duration of 10 min, making the diagnosis more challenging [3]. With early recognition in older children, the tachycardia rarely leads to congestive heart failure [1].
Ventricular tachycardia (VT) is typically less well tolerated. It can present with a myriad of symptoms ranging from signs of poor cardiac output (decreased blood pressure, diminished peripheral pulses, and delayed capillary refill) to cardiac arrest, depending on the severity and duration of the tachycardia. Pulseless ventricular tachycardia (pVT) or ventricular fibrillation (VF) on the other hand, present in pulseless arrest requiring immediate treatment.
Mechanism
SVT is a narrow QRS tachycardia that may be due to an automatic focus or an abnormal reentrant pathway which short circuits the normal conduction pathways, suppresses the sinus node, and elevates the heart rate above the sinus rate. Normally, sinus nodal cells spontaneously depolarize, and the electrical impulse spreads through the atria and to the fibrous, non-conductive AV groove tissue which prevents direct depolarization to the ventricles. In the usual circumstance, the AV node transmits the electrical impulse to the ventricles via the His-purkinje system, causing ventricular depolarization. An accessory pathway is a defect in the AV groove that allows the electrical current to be directly transmitted from the atria to the ventricles or from the ventricles to the atria, bypassing the AV node. SVT can often be differentiated from sinus tachycardia by abnormal p waves on electrocardiogram (ECG) and a heart rate that is not variable. It exceeds 180 beats per minute in children and 220 beats per minute in infants. SVT may be classified into pathway-mediated tachycardias and automatic tachycardias. Pathway-mediated tachycardia is the most common type, and must have two distinct conducting pathways linked around an area of non-conducting tissue. It can be terminated if one or both limbs of the tachycardia are disrupted. Automaticity however, is the ability of a myocyte to depolarize spontaneously, and these types of arrhythmias are generally refractory to direct cardioversion.
Pathway-Mediated Tachycardia
Reentrant pathway-mediated tachycardias initiate SVT in up to 90% of infants and 50% of older children. Characteristics of pathway-mediated tachycardias may include anterograde conduction via the AV node and retrograde via the accessory pathway (orthodromic reentrant tachycardia or ORT, Fig. 1), or anterograde via the accessory pathway and retrograde via the AV node (antidromic reentrant tachycardia). ORT is the most common arrhythmia in children, and makes up to 82% of arrhythmias in infancy [5].
AV node reentrant tachycardia (AVNRT) is also composed of a reentry circuit but composed of a fast and slow pathway within the AV node. AVNRT rarely presents in infancy but its incidence increases with age compared to accessory pathway-mediated SVT, whose frequency decreases with age. One study showed AVNRT in 18% of patients 0–7 years old with SVT and up to 36% in those 12–21 years old [6]. It is often precipitated by a premature atrial contraction conducted through the slow pathway within the AV node when the fast conduction pathway is still refractory. By the time the impulse reaches the end of the slow conduction pathway, the fast pathway is no longer refractory and thus the impulse cycles retrograde up the fast pathway and simultaneously down to the ventricle. This creates an impulse that continuously cycles around the two pathways leading to retrograde depolarization of the atria and anterograde depolarization of the ventricles via the His-Purkinje system. Pathway-mediated tachycardias respond well to SVT management with vagal maneuvers and/or adenosine.
It is important to note that these accessory pathways are present at birth. If the tissue is not ready for depolarization, patients are asymptomatic and in normal sinus rhythm. Factors that lead to a decreased refractory time across the myocardium and lead to the initiation of the tachyarrhythmia include premature atrial contractions, or any catecholamine increased state, such as fever.
Non-pathway Mediated
In the pediatric population, SVT is less commonly caused by an automatic focus. In infancy, patients with automatic tachycardias often present in heart failure due to the persistent and often refractory nature of the tachyarrhythmia, and will likely require rate controlling medications such as amiodarone to manage the symptoms acutely. Non-pathway-mediated tachyarrhythmias include ectopic atrial tachycardia (EAT), atrial flutter, and atrial fibrillation.
EAT is an automatic tachycardia that comprises about 10% of pediatric tachyarrhythmias and is defined by a single or multiple foci in the atria outside of the sinus node (Fig. 2). It often has a warm-up phase upon initiation and a cool-down phase prior to termination [7].
Atrial flutter is composed of a reentry circuit that usually originates around the borders of the tricuspid valve leading to an atrial rate of 240–360 bpm and a ventricular rate of 120–240 bpm (Fig. 3). The severity of hemodynamic compromise depends on the degree of AV conduction with 1:1 AV conduction, or every atrial beat leading to depolarization of the ventricles, being the most unstable. If the AV node is unable to conduct every atrial impulse to the ventricles, the ventricular rate will be slower than the flutter rate and the patient will be more hemodynamically stable.
Atrial fibrillation, another automatic tachycardia, is a rapid, irregularly irregular tachycardia mediated by multiple micro-reentry circuits throughout the atria, absence of an isoelectric baseline and a variable ventricular rate (Fig. 4). It is rarer in children. If a patient has been in atrial fibrillation or flutter for more than 48 h, an echocardiogram should be performed prior to conversion to sinus rhythm to evaluate for an atrial thrombus, as conversion to sinus rhythm in the setting of a thrombus may lead to embolization. Both atrial flutter and atrial fibrillation are more commonly seen after heart surgery, particularly in patients who have atrial enlargement, or those who are status post atriotomy [8].
Junctional ectopic tachycardia (JET) is a rhythm disturbance observed almost exclusively during and after pediatric surgery of congenital cardiac defects (Fig. 5) [9]. It is characterized by AV dissociation with a normal QRS and a ventricular rate faster than the atrial rate, which can lead to severe hemodynamic instability from loss of AV synchrony and decreased diastolic filling time. This may be hemodynamically significant, as one third of cardiac output is composed of the atrial kick, which only occurs in the setting of appropriate AV synchrony. Early recognition is imperative, which can be aided with an atrial electrocardiogram, canon “A” waves on the central venous pressure monitor, and perhaps a trial of adenosine to unmask asynchrony.
Management is aimed at decreasing the heart rate to allow for overdrive atrial pacing, restoration of AV synchrony, and thus cardiac output until the arrhythmia “burns out,” which typically occurs within a few days. Initial management includes maintenance of normal electrolyte levels, particularly calcium, potassium and magnesium, maintenance of normothermia or slight hypothermia; ensure adequate sedation, and consideration of paralysis to avoid increased metabolic demand. Weaning inotropes, especially dopamine, in order to minimize exogenous catecholamine administration may aid in termination of the arrhythmia [10]. If the heart rate continues to be accelerated with poor cardiac output, amiodarone is given to slow the heart rate and allow overdrive pacing. Recently, studies have shown an increased dose administration of magnesium in the operating room (50 mg/kg) while re-warming from bypass and the use of dexmedetomidine perioperatively can significantly decrease the occurrence of JET [11, 12]. Rarely, patients will be severely hemodynamically unstable and require extracorporeal life support, which occurs at a greater incidence than those who do not develop JET after congenital heart disease surgery [9].
Wolff-Parkinson-White Syndrome
WPW refers to the presence of an anterograde accessory AV pathway evident during sinus rhythm that results in a shortened PR interval and slurring of the QRS complex upstroke on ECG, known as a “delta wave” (Fig. 6). WPW may be asymptomatic, or associated with reentrant tachycardia. SVT due to WPW that begins in infancy may disappear, but often recurs later in childhood [13]. It is an entity worth discussing in this review due to the potential for rapid ventricular response during atrial fibrillation, which can lead to ventricular fibrillation and sudden death. Adenosine and any AV nodal blocking agents are contraindicated in these patients when presenting with atrial fibrillation since blocking the AV node may increase conduction via the accessory pathway and lead to an increased ventricular rate and clinical deterioration [7]. Due to the availability of catheter ablation, patients with WPW should be evaluated for risk of sudden death characterized by the presence of symptoms and a shorter pre- excited R-R interval during induced atrial fibrillation [14].
Acute Management
The acute management of SVT is dependent on the stability of the patient. Hemodynamically stable patients with adequate perfusion should be managed with vagal maneuvers, either via the Valsalva maneuver or via induction of a diving reflex. If vagal maneuvers are ineffective, administration of adenosine is indicated. If the patient is unstable, they should be emergently cardioverted. In either case, a continuous ECG should be in place to record the rhythm during the intervention, not just before and after, to aid in the diagnosis and further management.
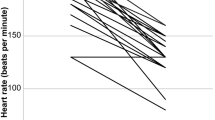
The Valsalva maneuver is forced expiration against a closed glottis. At the termination of the maneuver, arterial pressure increases resulting in stimulation of the vagal nerve center by the carotid sinus, leading to a reflex bradycardia. This results in a decreased conductance through the AV node, which may be effective in terminating the reentry circuit and converting to sinus rhythm. Increasing vagal tone via induction of the diving reflex is more feasible in infants. Cold water stimulation of the afferent ophthalmic and mandibular branches of the trigeminal nerve results in efferent stimulation of the vagus nerve, leading to slowed conduction through the AV node and sinus bradycardia [1, 15].
Adenosine is an adenine nucleoside that works by transiently blocking the AV node, thereby interrupting the reentrant pathway and terminating pathway-mediated tachycardias. There is no direct effect on the cause of the arrhythmia. Because automatic tachycardias do not involve the AV node, both adenosine and vagal maneuvers will not be effective, as the degradation of adenosine or cessation of vagal response allows for the tachycardia to resume. It may however be diagnostic by allowing for evaluation of the baseline atrial activity as opposed to the therapeutic effect it has in pathway-mediated tachycardias. It does so by interrupting a ventricular response by transiently blocking the AVN, but the primary atrial arrhythmia would not be affected. This may unmask underlying flutter waves or AV dyssynchrony; however, it will not terminate a non-pathway-mediated arrhythmia.
Adenosine has a very short half-life (10–15 s) and must be administered via reliable venous access, preferably in an upper limb, with a three-way stopcock. One syringe should contain adenosine at a dose of 0.1 mg/kg and the other a normal saline bolus of 3-5 mL to be administered immediately after the adenosine by an assistant after changing the direction of the stopcock. A repeated dose of 0.2 mg/kg up to a maximum of 0.3 mg/kg may be given. Resuscitation equipment should be readily available as adenosine may rarely precipitate atrial fibrillation or wide complex tachycardia [16].
Contraindications to adenosine include WPW with atrial fibrillation, patients on dipyridamole, and post cardiac transplant patients. As discussed above, patients who have WPW with atrial fibrillation can convert to a rapid ventricular rhythm if adenosine is administered, as the resultant AV node block allows all impulses through the accessory pathway, which lacks a refractory period. Dipyridamole is a medication that is used for its antithrombotic and vasodilatory effects. It works by inhibiting phosphodiesterases and inhibiting the reuptake of adenosine by red blood cells. It can therefore prevent reuptake of exogenously administered adenosine leading to persistent heart block [17]. In post-transplant patients there is a presumed risk of prolonged AV block since the transplanted heart is denervated. A recent study conversely showed safety of low dose administration of adenosine with gradual increase in the dose producing effective AV block without persistent asystole in heart transplanted patients, so the safety of adenosine in this population warrants reconsideration, especially because SVT is common after heart transplantation [18].
There are several reasons for a failed dose of adenosine. They include: inappropriate method of administration, or the presence of an automatic or ventricular tachyarrhythmia. It is also possible that the patient converted to sinus rhythm but returned to the tachyarrhythmia, and the response was not noted. Finally, if the patient has poor cardiac function it is possible that the adenosine was unable to get to the heart before being broken down, given the short half-life.
Amiodarone and procainamide have both been used in the management of refractory or recurrent SVT. Procainamide slows the upstroke of the cardiac action potential by blocking sodium channels. It slows conduction and suppresses automaticity, leading to an increased PR interval, widened QRS complex, and prolonged QTc interval. Similar to amiodarone, it should be used with caution in patients with prolonged QTc or on other medications which prolong QTc. The loading dose of procainamide is 15 mg/kg. A study by Chang et al. compared the two agents on infants and children with SVT, excluding junctional ectopic tachycardia, which found greater success with procainamide when compared to amiodarone in management of recurrent SVT with no difference in frequency of adverse events [19]. Further studies to evaluate the safety and efficacy of the two agents in this population are warranted; however, both are reasonable management options at this time. Amiodarone will be discussed in detail later in the review under management of ventricular tachycardias.
If the patient is hemodynamically unstable or intravenous access is not readily accessible, direct synchronized cardioversion should be performed. The recommended dose of energy is 0.5–1 J/kg, up to 2 J/kg. If possible, procedural sedation is recommended; however, cardioversion should not be delayed in an unstable patient. Preferred sedation in these patients would have rapid onset and rapid recovery with limited effect on hemodynamics. Emergency airway equipment and trained personnel should be readily available. Adult electrode paddles should be used once the chest size permits, usually for children greater than 10 kg, since use of pediatric electrode paddles results in higher transthoracic impedance and lower peak current flow [20].
Atrial overdrive pacing may be used to terminate reentrant SVT such as AVNRT or ORT, or may be used to improve hemodynamics in cases of JET. Temporary pacing with epicardial pacing wires in postoperative cardiac patients is most commonly used in the pediatric intensive care unit. If epicardial wires are not available, transcutaneous pacing may be used. However, due to the risk of burns from transcutaneous pacing, efforts should be made to obtain a transvenous pacing lead or epicardial pacing leads [21].
Refractory tachycardia leading to cardiogenic shock may rarely require mechanical support such as extracorporeal membrane oxygenation (ECMO) or a ventricular assist device (VAD). Younger patients are more likely to require mechanical support than older patients. The most common arrhythmia requiring mechanical support is SVT. Most patients are treated with at least one anti-arrhythmic agent prior to initiation of mechanical support, most commonly amiodarone [22•]. Once on ECMO or a VAD the patient can be hemodynamically supported while utilizing anti-arrhythmic medications to control the arrhythmia. In persistently refractory arrhythmias, several patients have undergone successful ablation while on full flow, and several patients have been successfully bridged to transplant [22•].
Cardiac arrest due to poor function from long standing SVT or from ventricular arrhythmias has been resuscitated with extracorporeal cardiopulmonary resuscitation (eCPR). A meta-analysis done by Debaty et al. of adult patients revealed survival or favorable neurologic outcome in 15% of patients who underwent eCPR after out-of-hospital cardiac arrest. They found that patients presenting with a shockable rhythm (pVT or VF) had favorable outcomes compared to those who did not. Other favorable prognostic factors found were shorter low-flow duration, higher pH, and lower lactate. There are several limitations to this study due to the observational retrospective design of it, which is prone to confounding and selection bias, and the meta-analysis design, which leads to variable inclusion criteria, study design, and statistical methods [23•]. There is a significant lack of data with regards to pediatric dysrhythmias and eCPR. This supports the need for investigations into criteria for implementation of eCPR as well as prognostic factors such as presenting rhythm in pediatric patients of this continuously evolving intervention.
Ventricular Arrhythmia
Ventricular arrhythmias are less common in the pediatric population compared to SVT, however has been reported as up to 18% of arrhythmias in pediatric cardiac intensive care units, and are the most common rhythm disturbances in patients with myocarditis [8, 24]. Ventricular tachycardia is a wide complex QRS tachyarrhythmia that originates below the bundle of His and can be classified into non-sustained (lasting less than 30 s) and sustained (greater than 30 s) (Fig. 7). Furthermore, it can be classified into monomorphic, which has a single QRS morphology with regular rate, or polymorphic, with variable QRS morphology and rate. Management depends on the patient’s clinical status.
If the patient is hemodynamically stable, then amiodarone or lidocaine may be considered as first-line therapy while monitoring ECG and blood pressure closely [7, 25, 26••]. If they become unstable (hypotension, poor perfusion, altered mental status) and remain in VT with a pulse, synchronized cardioversion is indicated based on AHA guidelines, initially with 0.5–1 J/kg, up to 2 J/kg on repeat shocks [27].
Amiodarone has been shown to be safe and efficacious in infants and children in various scenarios including both atrial and ventricular tachyarrhythmias as well as junctional ectopic tachycardia [28, 29]. The published data on amiodarone in the pediatric population is sparse and mostly derived from adult studies, but case reports and case studies have supported its use. The mechanism of action of amiodarone is multiple. It blocks outward potassium channels leading to prolongation of the cardiac action potential and a prolonged refractory period. It also has both α and β blockade, calcium channel blockade, and affects inward sodium current. These influences lead to decreased conduction across the AVN and increased effective refractory period. It does often lead to a prolonged QTc interval and so caution should be taken in the setting of Long QT syndrome, when used in combination with other QTc prolonging medications, or in cases of hypomagnesemia. However serious pro-arrhythmic effects have not been reported in children [29, 30]. Vasodilation may occur, likely secondary to α blockade, which can be resolved with a slower infusion rate, fluid resuscitation, and appropriate calcium repletion if indicated. Standard loading dose is 5 mg/kg, given as a bolus for ventricular fibrillation (VF) or pulseless ventricular tachycardia (pVT), or over 20–60 min for SVT or VT with a pulse.
Amiodarone has historically been the drug of choice for life-threatening arrhythmias based on limited pediatric data. Valdes et al. evaluated amiodarone compared to lidocaine use in children with in-hospital cardiac arrest with pVT and VF, and found that lidocaine use was independently associated with improved return of spontaneous circulation (ROSC) and 24 h survival, while neither drug was associated with survival to hospital discharge compared to placebo. This led to the inclusion of lidocaine alongside amiodarone as a first-line agent in the 2015 American Heart Association (AHA) guidelines for pVT or VF [26••, 31]. A later study by Kudenchuk et al. in adults showed no difference in amiodarone or lidocaine on survival or favorable neurologic outcome, further supporting the inclusion of both in management of pVT or VF [32]. Lidocaine inhibits fast inward sodium current, primarily affecting the ventricular myocardium and decreasing automaticity. A loading dose is 1 mg/kg but there is decreased efficacy with hypokalemia. It does not prolong the QTc interval, making it a good alternative in patients with underlying prolonged QTc.
Torsades de pointes is a life-threatening ventricular tachycardia characterized by polymorphic QRS complexes twisting around an isoelectric baseline that develops in the setting of a prolonged QTc interval (Fig. 8). It can last seconds and resolve spontaneously or deteriorate into a uniform ventricular tachycardia or ventricular fibrillation, with a high likelihood to recur. Intravenous magnesium sulfate has proved effective in terminating and suppressing torsades de pointes because it contributes to the ion channel transport processes in myocytes [33]. However, prolonged torsades de pointes is always poorly tolerated and if it does not spontaneously convert to sinus rhythm prompt cardioversion should be performed as it will ultimately degenerate into ventricular fibrillation [21].
A wide complex tachyarrhythmia may be difficult to differentiate between ventricular tachycardia and SVT with aberrant conduction. A trial of adenosine may be used if the rhythm is regular and monomorphic and the patient is clinically stable in order to help differentiation, because it causes atrioventricular dissociation; a sinus rate slower than the ventricular rate will become apparent in VT, but not in SVT with aberrancy.
If at any time the patient deteriorates to pulseless ventricular tachycardia (pVT) or ventricular fibrillation (VF), start cardiopulmonary resuscitation (CPR) per PALS guidelines and initially defibrillate with 2 J/kg, and then continue CPR. A second shock if indicated should be 4 J/kg followed by CPR, with subsequent shocks may be ≥ 4 J/kg up to a maximum of 10 J/kg or adult dose [26••]. If the arrest is witnessed and a defibrillator is immediately available, defibrillation is very effective at converting the tachyarrhythmia to normal sinus rhythm. However, with delay in defibrillation, success declines by 7–10% every minute. Effective CPR is the best method of restoring myocardial energy stores in the interim until a defibrillator is available, to best increase the likelihood of successful defibrillation [34].
Conclusion
Tachyarrhythmias in children can be life-threatening. Initial management of SVT is well-known to be vagal maneuvers and adenosine. Historically, adenosine was contraindicated in post-transplant patients but there is a new evidence to support its safety in this population. Additionally, lidocaine is recognized as a first-line agent in the management of ventricular tachycardia alongside amiodarone based on the 2015 AHA guidelines. There are updates in prevention and management of junctional ectopic tachycardia in pediatric cardiac surgical patients, which include the use of dexmedetomidine and magnesium. Finally, there is emerging data to evaluate the use of extracorporeal life support in pediatric patients with dysrhythmias, but more information on patient selection and prognosis are essential for this evolving intervention. This reminds us to continuously re-evaluate what the standard of care is defined as in management of pediatric patients with tachyarrhythmias.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Manole MD, Saladino RA. Emergency department management of the pediatric patient with supraventricular tachycardia. Pediatr Emerg Care. 2007;23(3):176–85. quiz 186-9
Venugopalan P, et al. Supraventricular tachycardia in children: a report of three cases, diagnosis and current management. Journal for scientific research Medical sciences / Sultan Qaboos University. 2000;2(1):59–64.
Schlechte EA, Boramanand N, Funk M. Supraventricular tachycardia in the pediatric primary care setting: age-related presentation, diagnosis, and management. J Pediatr Health Care. 2008;22(5):289–99.
Clausen H, et al. Paediatric arrhythmias in the emergency department. Emerg Med J. 2012;29(9):732–7.
Ko JK, et al. Supraventricular tachycardia mechanisms and their age distribution in pediatric patients. Am J Cardiol. 1992;69(12):1028–32.
Anand RG, et al. Is the mechanism of supraventricular tachycardia in pediatrics influenced by age, gender or ethnicity? Congenit Heart Dis. 2009;4(6):464–8.
Hanash CR, Crosson JE. Emergency diagnosis and management of pediatric arrhythmias. Journal of Emergencies, Trauma and Shock. 2010;3(3):251–60.
Hoffman TM, et al. The incidence of arrhythmias in a pediatric cardiac intensive care unit. Pediatr Cardiol. 2002;23(6):598–604.
Zampi JD, et al. Junctional ectopic tachycardia after infant heart surgery: incidence and outcomes. Pediatr Cardiol. 2012;33(8):1362–9.
Hoffman TM, et al. Postoperative junctional ectopic tachycardia in children: incidence, risk factors, and treatment. Ann Thorac Surg. 2002;74(5):1607–11.
Manrique AM, et al. Magnesium supplementation during cardiopulmonary bypass to prevent junctional ectopic tachycardia after pediatric cardiac surgery: a randomized controlled study. J Thorac Cardiovasc Surg. 2010;139(1):162–169.e2.
El Amrousy DM, et al. Efficacy of prophylactic dexmedetomidine in preventing postoperative junctional ectopic tachycardia after pediatric cardiac surgery. J Am Heart Assoc. 2017;6(3):e004780.
Perry JC, Garson A Jr. Supraventricular tachycardia due to Wolff-Parkinson-White syndrome in children: early disappearance and late recurrence. J Am Coll Cardiol. 1990;16(5):1215–20.
Benson DW, Cohen MI. Wolff-Parkinson-White syndrome: lessons learnt and lessons remaining. Cardiol Young. 2017;27(S1):S62–s67.
Muller G, Deal BJ, Benson DW Jr. “Vagal maneuvers” and adenosine for termination of atrioventricular reentrant tachycardia. Am J Cardiol. 1994;74(5):500–3.
Rankin AC, Rae AP, Houston A. Acceleration of ventricular response to atrial flutter after intravenous adenosine. Br Heart J. 1993;69(3):263–5.
Ciacciarelli M, et al. Dipyridamole: a drug with unrecognized antioxidant activity. Curr Top Med Chem. 2015;15(9):822–9.
Flyer JN, et al. Prospective study of adenosine on atrioventricular nodal conduction in pediatric and young adult patients after heart transplantation. Circulation. 2017;135(25):2485–93.
Chang PM, et al. Amiodarone versus procainamide for the acute treatment of recurrent supraventricular tachycardia in pediatric patients. Circ Arrhythm Electrophysiol. 2010;3(2):134–40.
Atkins DL, Kerber RE. Pediatric defibrillation: current flow is improved by using “adult” electrode paddles. Pediatrics. 1994;94(1):90–3.
Nichols DG. Critical heart disease in infants and children. Philadelphia: Mosby; 2006.
• Silva JN, et al. Management of pediatric tachyarrhythmias on mechanical support. Circ Arrhythm Electrophysiol. 2014;7(4):658–63. Discusses the implementation of ECMO and VADs in children with refractory arrhythmias.
• Debaty G, et al. Prognostic factors for extracorporeal cardiopulmonary resuscitation recipients following out-of-hospital refractory cardiac arrest. A systematic review and meta-analysis. Resuscitation. 2016;112:1–10. A review of adult studies to determine the prognostic factors of those who undergo eCPR emphasizes the need for similar investigations in children.
Miyake CY, et al. In-hospital arrhythmia development and outcomes in pediatric patients with acute myocarditis. Am J Cardiol. 2014;113(3):535–40.
Jat KR, Lodha R, Kabra SK. Arrhythmias in children. Indian J Pediatr. 2011;78(2):211–8.
•• de Caen AR, et al. Part 12: pediatric advanced life support: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18 Suppl 2):S526–42. This article discusses the most current guideline in pediatric-advanced life support and cardiopulmonary resuscitation. Based on prior studies, the use of both amiodarone and lidocaine are recommended as first line agents in the management of ventricular tachycardia.
American Heart Association. 2005 American Heart Association (AHA) guidelines for cardiopulmonary resuscitation (CPR) and emergency cardiovascular care (ECC) of pediatric and neonatal patients: pediatric basic life support. Pediatrics. 2006;117(5):e989-1004.
Perry JC, et al. Pediatric use of intravenous amiodarone: efficacy and safety in critically ill patients from a multicenter protocol. J Am Coll Cardiol. 1996;27(5):1246–50.
Burri S, Hug MI, Bauersfeld U. Efficacy and safety of intravenous amiodarone for incessant tachycardias in infants. Eur J Pediatr. 2003;162(12):880–4.
Etheridge SP, Craig JE, Compton SJ. Amiodarone is safe and highly effective therapy for supraventricular tachycardia in infants. Am Heart J. 2001;141(1):105–10.
Valdes SO, et al. Outcomes associated with amiodarone and lidocaine in the treatment of in-hospital pediatric cardiac arrest with pulseless ventricular tachycardia or ventricular fibrillation. Resuscitation. 2014;85(3):381–6.
Kudenchuk PJ, et al. Amiodarone, lidocaine, or placebo in out-of-hospital cardiac arrest. N Engl J Med. 2016;374(18):1711–22.
Hoshino K, et al. Successful uses of magnesium sulfate for torsades de pointes in children with long QT syndrome. Pediatr Int. 2006;48(2):112–7.
Link MS, et al. Part 7: adult advanced cardiovascular life support: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18 Suppl 2):S444–64.
Acknowledgements
We appreciate the help with revisions from Dr. Aaron Kessel, division of pediatric critical care at Cohen Children’s hospital, and contribution of electrocardiograms from Dr. Eric Silver, division of pediatric cardiology at New York-Presbyterian hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Intensive Care Medicine
Rights and permissions
About this article
Cite this article
Mokhateb-Rafii, T., Bakar, A.M. Pediatric Tachyarrhythmias: Diagnosis and Management. Curr Pediatr Rep 5, 242–250 (2017). https://doi.org/10.1007/s40124-017-0148-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40124-017-0148-1