Abstract
Purpose of Review
West syndrome (WS) is a rare disorder consisting of developmental regression, hypsarrhythmia, and infantile spasms. Over time, the clinical approach to this frequently debilitating epileptic encephalopathy has evolved considerably; however, the relative rarity of WS has made it challenging to study its evaluation, treatment, and neurodevelopmental outcome. The purpose of this review is to provide the practicing clinician with an evidence-based approach to WS.
Recent Findings
We focus on recent evidence that informs the clinician of the expected yield of diagnostic testing, including genetic evaluation, and a tiered approach both to the initial treatment and to treatment after relapse.
Summary
Hormonal therapy or vigabatrin remains the most effective therapies for the treatment of WS, particularly when treatment is initiated promptly. While history, examination, and neuroimaging can identify an etiology for the majority of cases of IS, genetic testing is the highest yield investigation for the remainder of patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Among the early onset epileptic encephalopathies, West syndrome (WS) is common, impacting 0.25–0.42 per 1000 live births, and emerging most frequently between the ages of 4 and 6 months [1]. This syndrome composed of the triad of developmental regression, hypsarrhythmia, and infantile spasms (IS), was named for Dr. West in 1841, who first described its classic seizure type in his son. The causes of the syndrome are quite diverse, which has prevented discovery of a clear unifying hypothesis for its pathophysiology. Unfortunately, despite treatment, many infants subsequently develop treatment-resistant epilepsy and neurodevelopmental impairments [1].
In this review, we summarize the recent advances in the diagnosis and treatment of WS, with the goal of providing a practical, evidence-based framework for approaching this condition. This straightforward summary highlights both the advancements made in recent years and topics for additional study in the future.
Historical Overview
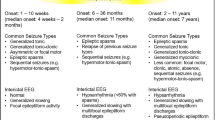
Natural History and Etiological Classification
In the years following the initial clinical description of IS by Dr. West, there were few references in the literature until the first description of hypsarrhythmia in 1952 [2]. Several years later, the first report emerged about the effectiveness of hormonal therapy with adrenocorticotropic hormone (ACTH) in treating IS [3]. Despite subsequent treatment with ACTH, the general outlook for infants with IS remained poor, with epidemiological studies in the early 1990s reporting a case fatality rate of 10–20%, abnormal mental development in the majority of infants (30–95% depending upon etiology), and evolution to Lennox-Gastaut syndrome in 23–61% [1]. Moreover, relapse after successful therapy was frequent, occurring in approximately 1/3 of infants [4].
Etiologically, the causes of IS were classified as symptomatic or cryptogenic. Those infants with a clear cause for IS were referred to as symptomatic, including etiologies such as neonatal hypoxic-ischemic encephalopathy, acquired brain injuries, neonatal infections, cortical malformations, and tuberous sclerosis. These infants had a poorer outcome than those for whom no etiology could be elucidated, and the cause was presumed to be genetic, referred to as cryptogenic [4]. Recent advances in neuroimaging and genetic testing have enabled the identification of additional etiologies for infants previously classified as cryptogenic. In an effort to better represent the changing diagnostic landscape, the International League Against Epilepsy (ILAE) proposed modifications to the classification scheme in 2010. Rather than referring to the etiology of IS as symptomatic or cryptogenic, the ILAE proposed reclassifying patients with IS as having a structural, genetic/metabolic, or unknown cause [5].
Initial Therapeutic Advances
In light of the promising response to ACTH in the treatment of IS, investigators hypothesized that prednisone might also be efficacious. Early studies were limited by variability in dosing schedules, lack of control groups, or lack of blinding (referenced in [6]). The first double-blind, crossover study of ACTH and prednisone was conducted in 1983, using both clinical cessation of spasms and resolution of hypsarrhythmia as outcome measures [7]. This small study found no difference between low-dose ACTH gel (20 U/day) and prednisone (2 mg/kg/day) [7]. Several years later, Baram et al. published another small randomized trial demonstrating that high-dose ACTH (150 U/m2/day) was dramatically superior than that to prednisone (2 mg/kg/day), resulting in cessation of spasms and resolution of hypsarrhythmia in 86.6% of patients, compared with those of 28.6% of patients receiving prednisone [8]. An alternative medication, vigabatrin (VGB), began receiving attention for its efficacy in treating IS in tuberous sclerosis (TS), and a small prospective randomized trial demonstrated that VGB was superior to steroids as a first-line treatment in this population [9]. These findings were corroborated by several additional studies, reviewed by Hancock et al. [10]. Mackay et al., on behalf of the American Academy of Neurology and the Child Neurology Society, developed practice parameters for the treatment of IS in 2004. These guidelines indicated that ACTH was probably effective and VGB was possibly effective, particularly in patients with TS, for the short-term treatment of IS, but there was insufficient evidence to recommend oral corticosteroids (OCS) or other anti-seizure medications for this purpose. The guidelines indicated that there was insufficient evidence to recommend any therapy to improve the long-term outcomes of children with IS or to recommend early treatment of IS to improve outcomes [11].
The first study comparing long-term neurodevelopmental and epilepsy outcomes in IS was the United Kingdom infantile spasms study (UKISS), which compared hormonal treatment (synthetic ACTH 40 IU every other day or prednisone 10 mg four times daily) to VGB, with a primary outcome measure of clinical cessation of IS and neurodevelopmental outcome at 14 days, 14 months, and 4 years. Results of the UKISS demonstrated that early clinical response was more likely with hormonal therapy (76% with ACTH, 70% with prednisone) compared with VGB (54%) [12]; however, sustained clinical response at 14 months was similar between the two (hormonal therapy 40% versus VGB 37%) [13]. Non-responders who subsequently received the alternative therapy had a high likelihood of response (hormonal therapy 74%, vigabatrin 75%), underscoring the importance of close monitoring and prompt therapy for relapses [13]. In terms of short-term neurodevelopmental outcome at 14 months, infants with a symptomatic etiology performed poorly compared with those with an unknown etiology. Moreover, infants with an unknown etiology treated with hormonal therapy had a better outcome than all other groups [13]. Similar results were noted in long-term follow-up at 4 years [14]. Longer time initiating treatment was associated with worse long-term developmental outcome, which underscores the importance of prompt recognition and treatment of infants with IS [15].
While the UKISS remains the largest randomized trial of treatments for IS, it was not without its limitations. Notably, UKISS did not include patients with TS, thus, its findings are not applicable to this population. Response to therapy was not verified by electrographic absence of hypsarrhythmia; thus, it is possible that the estimates of immediate effectiveness are inaccurate given the high relapse rate. Finally, UKISS did not establish which hormonal therapy was superior for successful treatment of IS, but it did again raise questions about the possible effectiveness of OCS.
New Developments: Establishing an Etiology
Using Evidence to Inform the Diagnostic Evaluation
As discussed above, children without an identifiable cause for IS may respond more favorably to treatment and may have better neurodevelopmental outcomes [16]. Some patient groups, such as those with TS, may also respond better to certain treatments. Thus, correct identification of an underlying etiology has the potential to impact therapeutic decisions as well as parental counseling and expectation-setting.
As with most neurological conditions, a thorough history and physical examination are paramount. Prenatal or perinatal risk factors for infection, hypoxia, or stroke may portend an acquired structural etiology. Multi-system organ involvement might suggest a metabolic or mitochondrial disorder. Family history of early onset epilepsy syndromes might suggest a genetic etiology. Finally, focal neurological findings on examination, including stigmata of a neurocutaneous syndrome, might suggest a specific structural cause such as TS. In many cases, history and examination are not sufficient, and additional testing is necessary. It would appear intuitive that EEG and neuroimaging, particularly MRI, would play important roles in the diagnostic workup, but if these are unrevealing, what are the next best steps?
Recently, a study by Wirrell et al. utilized the National Infantile Spasms Consortium database to address this question by prospectively evaluating the diagnostic yield of individual studies in infants with newly diagnosed WS from 2012 to 2014 [17•]. This database represents patients enrolled across 21 pediatric epilepsy centers that participate in the Pediatric Epilepsy Research Consortium (PERC). A summary of these results is displayed in Table 1. The highest yield overall was obtained by combining clinical assessment with MRI, which identified an etiology in 55.2% of patients, including cortical malformations, acquired structural brain abnormalities, and stigmata of inborn errors of metabolism or TORCH infections [17•]. Of the remaining infants without an obvious etiology based on these studies, genetic testing was high yield, with causative mutations identified in 31% by epilepsy gene panel and another 11% by array comparative genomic hybridization (CGH) [17•]. The lowest yield studies included specialized metabolic testing, such as serum, urine, and CSF evaluation. These studies identified causative abnormalities in only 4.5% of patients without an obvious etiology by clinical assessment and MRI. The only metabolic studies to yield positive results were serum lactate and pyruvate, serum amino acids, urine organic acids, CSF glycine, and CSF lactate (with concomitant abnormalities in serum lactate) [17•].
We advocate a tiered approach to investigation of infants with newly diagnosed IS. The first tier should entail a thorough history, examination, EEG, and MRI, which would be expected to yield an etiology in greater than 50% of cases. It is important that this EEG include the asleep state, as hypsarrhythmia may be most prominent in non-REM sleep [18]. If an etiology is not identified, then genetic testing, including an array CGH and epilepsy gene panel, should be sent, followed by specific metabolic testing if the genetic testing is not informative. One should be mindful that this framework does not exclude targeted testing if the initial evaluation strongly suggests a cause. For example, if history and MRI are suspicious for metabolic disease, then specific metabolic testing would be an appropriate next step. While it may be tempting to perform multiple tiers of testing simultaneously, including CSF sampling, in a patient without an obvious etiology, the above evidence suggests that this approach would result in costly and unnecessary testing for little additional yield.
How Genetics Has Changed the Meaning of Cryptogenic
Perhaps the most remarkable advancement in the past 10 years has been the rapid growth in the field of epilepsy genetics and the identification of many causative genes for the epileptic encephalopathies, such as IS. In the wake of the identification of ARX as the first genetic etiology of IS in a patient previously classified as cryptogenic, a number of additional single-gene mutations have been identified [19]. Moreover, it has become increasingly clear that mutations in single genes may cause more than one presentation of epileptic encephalopathy, and even within a particular disorder, there may be phenotypic variability depending on the mutation or the gene involved [20]. This degree of complexity raises interesting questions about the neurobiological underpinnings of IS.
More recently, whole exome sequencing (WES) has proven valuable in the identification of causative mutations in patients with IS of unknown cause, yielding pathogenic mutations in novel genes or known epilepsy genes in 25–45% of cases [21, 22]. While this potential yield is promising, WES has not yet supplanted targeted gene panels clinically due to a variety of factors, such as concerns about the interpretation of variants of unknown significance, incidental findings, and cost [23]. As additional experience in the clinical arena is obtained and these concerns are allayed, WES will likely acquire a more prominent role in the evaluation of patients with IS. At this time, we suggest considering WES on a case-by-case basis if initial genetic and metabolic testing does not reveal an etiology (see Table 1).
New Developments: Choosing a Therapy
ACTH or Prednisone: the Post-UKISS Debate
In the years since the UKISS, there has been considerable interest in comparing the efficacy of ACTH and OCS such as prednisone in the treatment of IS. This interest is driven by multiple factors, including the high cost of ACTH in the USA, use of an intramuscular injection in children, and concerns about the side effects of ACTH [24]. Shortly after the UKISS results were published, Go et al. updated the 2004 practice parameters for the treatment of infantile spasms. Their analysis of the literature indicated that there remained insufficient evidence to recommend OCS as an equivalent therapy to ACTH [25]. The new recommendations did note that some evidence supported the equivalence of low-dose and high-dose ACTH protocols in the short-term treatment of IS. Moreover, the guidelines confirmed that ACTH is superior to VGB for the short-term treatment of IS not caused by TS, and that insufficient evidence existed to recommend any other anti-seizure medication for the treatment of IS [25]. A meta-analysis by Arya et al. in 2012 further evaluated the existing clinical trials of OCS, finding that the short-term efficacy of steroids, defined as clinical resolution of IS and electrographic resolution of hypsarrhythmia, was 42%, a figure equivalent to the published efficacy of low-dose ACTH but inferior to that of high-dose ACTH [26].
Unfortunately, for the practicing clinician, the above evidence is both contradictory and, at times, confusing. The reasons for this are multifactorial. First, there are few prospective, randomized clinical trials on the topic; the remainder are uncontrolled or are retrospective in their design. Second, the majority of studies, including the randomized trials, are small in size, rendering them underpowered to detect small differences and prone to variability in their estimates of efficacy. Third, variability exists in ACTH formulation (natural ACTH in the USA, and synthetic ACTH elsewhere) and in dosing regimens across studies, limiting comparability. Because of these limitations, there remains a debate over whether ACTH or OCS is equivalent, and if not, then which agent is the most appropriate for which group of patients.
The Role of Conventional Anti-Seizure Medications
In addition to ACTH, OCS, and VGB, other anti-seizure medications have been evaluated for use in the treatment of IS. The more commonly used agents include topiramate (TPM), zonisamide (ZNS), valproic acid (VPA), the ketogenic diet (KD), and levetiracetam (LEV) [27]. These studies are primarily open-label and uncontrolled, include small numbers of patients, and use variable outcome measures which further limits their generalizability and may account for some of the differences in reported efficacy.
High-dose topiramate (up to 24 mg/kg/day) became a popular choice for treatment of IS after a small pilot study in 1998 demonstrated a > 50% reduction in spasms in 81% of patients, as well as a spasm-free rate of 45%, using clinical and electrographic measures of efficacy over an average follow-up period of 4.5 months [28]. Subsequent studies have been less promising, demonstrating spasm-free rates of 20–30% [29]. Even more pessimistically, a recent small retrospective study reported a spasm-free rate of only 9.7%, all of whom eventually relapsed [30]. Zonisamide has been studied by several groups and has been reported to have a response rate of 20–30%, though relapse rates ranged from 30 to 50% [29, 31, 32]. Valproic acid has been used over a wide range of doses from 30 to 300 mg/kg/day, with a response rate ranging from 40 to 78% [29, 33, 34]. Very high doses were required to obtain response rates at the high end of that range, which resulted in a high rate of side effects [34]. Levetiracetam has been evaluated in limited case reports, both as an initial therapy and an adjunctive therapy. One case series of LEV as an initial therapy demonstrated spasm freedom and resolution of hypsarrhythmia in 2/5 patients, with sustained seizure freedom 6 months later [35]. Another case series in patients with refractory infantile spasms demonstrated that LEV in doses as high as 117 mg/kg/day led to spasm freedom in 1/7 children and a > 50% reduction in spasms in 5/7 infants [36].
The ketogenic diet (KD) was evaluated in a large, prospective cohort of 104 infants as an adjunctive therapy for refractory IS in 2010, demonstrating a > 50% reduction in spasms in 64% of patients at 6 months and 77% at 1–2 years [37]. This included spasm freedom in 36% of infants for a period of at least 6 months. Additional benefits to KD included an improvement in development in 62%, EEG improvement in 35%, and reduction in the doses of other anti-seizure medications in 29%. While the KD has not been evaluated as a primary treatment for IS, this evidence does suggest that it can be a valuable adjunctive therapy in the difficult to treat population of patients with refractory IS.
Nitrazepam, a member of the benzodiazepine family, has also received some attention for the treatment of IS. In observational studies, nitrazepam has been effective for the reduction of spasms in as high as 35% of infants; however, spasm freedom was achieved in fewer than 25% of infants [29]. This data has led some to consider using clobazam in cases of refractory IS; however, no studies of clobazam for this purpose have been performed to date.
Just as the most recent guidelines for treatment of IS have indicated, it is our recommendation that the conventional anti-seizure medications discussed above not be used except in the treatment of refractory IS, due to a lack of rigorous evidence in their favor. Despite this, a recent survey of child neurologists demonstrated that conventional anti-seizure medications are often used as the first- and second-line therapies. In particular, 12% of responders reported using TPM as an initial therapy for infants with a non-TS structural etiology for their IS, while 6% were using other agents [38].
Using Evidence to Inform a Therapeutic Approach
As discussed above, studies of the optimal treatment regimen for IS have been limited by a combination of small samples, retrospective study designs, or lack of direct comparisons between agents. These limitations are partly responsible for the variability in treatment choices for individual patients. In an effort to address some of these limitations, Knupp and colleagues, on behalf of the National Infantile Spasms Consortium, recently published a pair of multi-center, prospective studies on responsiveness of infants with newly diagnosed IS to an initial treatment and to treatment after relapse. These studies included 230 infants receiving an initial therapy and 118 infants receiving additional therapy after relapse. While adherence to specific dosing regimens was not an enrollment criterion for these studies, recommendations were made to clinicians at the participating centers, which were followed in the majority of cases. These recommendations included high-dose ACTH at 150 IU/m2, divided twice daily, high-dose OCS starting at 40 mg/day (similar to the UKISS protocol), and VGB starting at 50 mg/kg/day with a goal dose of 150 mg/kg/day after 1 week. The choice of therapy was determined by the treating clinician at each study site.
With regard to the initial treatment of IS, 86% of infants received one of the standard therapies (either ACTH, OCS, or VGB), while 14% received non-standard therapies (any other anti-seizure medication). Response to therapy, defined by clinical resolution of spasms and electrographic resolution of hypsarrhythmia that was sustained for 3 months, was achieved by 46% of children receiving standard therapy and only 9% of children receiving non-standard therapy [39••]. Of the standard therapies, response to ACTH occurred in 55% of infants, response to OCS occurred in 39%, and response to VGB occurred in 36%. Statistically, response to ACTH was superior to that of VGB, but the difference between ACTH and OCS did not achieve statistical significance (p = 0.06). Relapse rates were similar among treatments [39••]. Interestingly, infants were less likely to receive ACTH if they had a history of prior seizures, prior anti-seizure medication usage, or severe developmental issues, which exposes a potential bias in prescribing practices that may not be warranted based on the available data.
With regard to treatment of relapsed IS, 37% responded to their second treatment, with 46% responding to a standard treatment with a different mechanism of action (i.e., ACTH or OCS after VGB, and vice versa) and 21% responding to a non-standard medication. Moreover, infants who had received their initial treatment within 4 weeks of clinical onset of spasms, even though that treatment was not ultimately successful, were more likely to respond to their second treatment [40•]. These findings offer further support that treatment of IS should be initiated and responsiveness evaluated promptly in order to maximize the response of the infants to therapy. Whether this rapid approach to therapy translates into better neurodevelopmental outcomes remains a matter of debate; however, there are several lines of evidence suggesting that shorter time to treatment does improve developmental outcome (reviewed in [16]).
In light of the above evidence, we advocate for the treatment approach depicted in Fig. 1. For clinicians taking this approach, it is critical to initiate the diagnostic evaluation and initial therapy promptly, ideally within 4 weeks of clinical onset of spasms. First, we suggest differentiating infants with a structural etiology from those with a genetic/metabolic or unknown etiology. This can be done with a careful history, examination, EEG, and MRI. If TS is suspected, then VGB is the most appropriate first therapy. We recommend starting at 50 mg/kg/day and increasing by 50 mg/kg every 3 days to a goal of 150 mg/kg/day. If this treatment is ineffective in achieving clinical cessation of spasms and resolution of hypsarrhythmia on EEG, or if the patient relapses after successful therapy, we recommend subsequent treatment with hormonal therapy with ACTH. At this time, the evidence does not clearly demonstrate equivalence of OCS to ACTH; though there is some indication that very high dose prednisone (8 mg/kg/day, maximum of 60 mg/day) may be more effective than previous prednisone regimens, such as the 40 mg/day used in the UKISS [41]. Should these agents prove ineffective, then additional anti-seizure medications or the KD should be considered. For those infants with a non-TS structural etiology, or for those with a genetic/metabolic or unknown etiology, we recommend an initial treatment with ACTH, though OCS may be considered. When using either ACTH or OCS, we recommend high dose therapy as described in the studies of Knupp et al. [39••, 40•]. If hormonal therapy is not effective, or if relapse occurs after successful therapy, then we recommend subsequent therapy with VGB. If the patient remains refractory to treatment, then additional anti-seizure medications or the KD should be considered (see “Fig. 1”). Based upon the available evidence, clinical and electrographic response typically occurs within the first 2 weeks; however, response to VGB in particular may take longer [12, 39••, 42]. In terms of the duration of therapy, both ACTH and OCS are typically weaned off over a 4-week period; however, a longer course can be considered for patients who have a partial response initially. The evidence is not clear regarding the optimal length of treatment with VGB for IS. Given the known risk of peripheral vision loss with VGB, it would be appropriate to limit exposure if possible; however, a recent study has suggested that the risk of vision loss in children, as measured by electroretinogram, may be lower than that of previously thought (5% at 6 months, 13% at 1 year) [43].
Conclusions
In summary, we hope to have provided an up-to-date, evidence-based approach to the evaluation and treatment of WS. We recognize that this approach is not complete, as there remain a number of unanswered questions in the field, including the equivalence of OCS and ACTH, the appropriate role for other anti-seizure medications and the KD, and the long-term impact of these therapies on the neurodevelopmental and epilepsy outcomes for these patients. In order to answer these important questions, future studies must continue to focus on prospective evaluation of sufficiently large samples of patients, ideally obtained through multi-center collaboration. For a rare disorder such as WS, the power is in the numbers.
References
Papers of particular interest, published recently, have been higlighted as: • Of importance •• Of major importance
Cowan LD, Hudson LS. The epidemiology and natural history of infantile spasms. J Child Neurol. 1991;6:355–64.
Fukuyama Y. History of clinical identification of West syndrome—in quest after the classic. Brain and Development. 2001;23:779–87.
Sorel L, Dusaucy-Bauloye A. Findings in 21 cases of Gibbs’ hypsarrhythmia; spectacular effectiveness of ACTH. Acta Neurol Psychiatr Belg. 1958;58:130–41.
Riikonen R. A long-term follow-up study of 214 children with the syndrome of infantile spasms. Neuropediatrics. 1982;13:14–23.
Berg AT, Berkovic SF, Brodie MJ, et al. Revised terminology and concepts for organization of seizures and epilepsies: report of the ILAE commission on classification and terminology, 2005-2009. Epilepsia. 2010;51:676–85.
Hrachovy RA, Frost JD, Kellaway P, Zion T. A controlled study of prednisone therapy in infantile spasms. Epilepsia. 1979;20:403–7.
Hrachovy RA, Frost JD, Kellaway P, Zion TE. Double-blind study of ACTH vs prednisone therapy in infantile spasms. J Pediatr. 1983;103:641–5.
Baram TZ, Mitchell WG, Tournay A, Snead OC, Hanson RA, Horton EJ. High-dose corticotropin (ACTH) versus prednisone for infantile spasms: a prospective, randomized, blinded study. Pediatrics. 1996;97:375–9.
Chiron C, Dumas C, Jambaqué I, Mumford J, Dulac O. Randomized trial comparing vigabatrin and hydrocortisone in infantile spasms due to tuberous sclerosis. Epilepsy Res. 1997;26:389–95.
Hancock E, Osborne JP. Vigabatrin in the treatment of infantile spasms in tuberous sclerosis: literature review. J Child Neurol. 1999;14:71–4.
Mackay MT, Weiss SK, Adams-Webber T, et al. Practice parameter: medical treatment of infantile spasms: report of the American Academy of Neurology and the Child Neurology Society. Neurology. 2004;62:1668–81.
Lux AL, Edwards SW, Hancock E, Johnson AL, Kennedy CR, Newton RW, O’Callaghan FJ, Verity CM, Osborne JP. The United Kingdom infantile spasms study comparing vigabatrin with prednisolone or tetracosactide at 14 days: a multicentre, randomised controlled trial. Lancet. 2004;364:1773–8.
Lux AL, Edwards SW, Hancock E, Johnson AL, Kennedy CR, Newton RW, O’Callaghan FJK, Verity CM, Osborne JP, United Kingdom Infantile Spasms Study. The United Kingdom infantile spasms study (UKISS) comparing hormone treatment with vigabatrin on developmental and epilepsy outcomes to age 14 months: a multicentre randomised trial. Lancet Neurol. 2005;4:712–7.
Darke K, Edwards SW, Hancock E, Johnson AL, Kennedy CR, Lux AL, Newton RW, O’Callaghan FJK, Verity CM, Osborne JP. Developmental and epilepsy outcomes at age 4 years in the UKISS trial comparing hormonal treatments to vigabatrin for infantile spasms: a multi-centre randomised trial. Arch Dis Child. 2010;95:382–6.
O’Callaghan FJK, Lux AL, Darke K, Edwards SW, Hancock E, Johnson AL, Kennedy CR, Newton RW, Verity CM, Osborne JP. The effect of lead time to treatment and of age of onset on developmental outcome at 4 years in infantile spasms: evidence from the United Kingdom infantile spasms study. Epilepsia. 2011;52:1359–64.
Widjaja E, Go C, McCoy B, Snead OC. Neurodevelopmental outcome of infantile spasms: a systematic review and meta-analysis. Epilepsy Res. 2015;109:155–62.
• Wirrell EC, Shellhaas RA, Joshi C, Keator C, Kumar S, Mitchell WG, Pediatric Epilepsy Research Consortium. How should children with West syndrome be efficiently and accurately investigated? Results from the national infantile spasms consortium. Epilepsia. 2015;56:617–25. This study addresses the expected diagnostic yield of neuroimaging, genetics, and metabolic testing in the evaluation of infants diagnosed with West Syndrome
Hrachovy RA, Frost JD. Infantile spasms. Handb Clin Neurol. 2013;111:611–8.
Paciorkowski AR, Thio LL, Dobyns WB. Genetic and biologic classification of infantile spasms. Pediatr Neurol. 2011;45:355–67.
Epi4K Consortium, Epilepsy Phenome/Genome Project, Allen AS, et al. De novo mutations in epileptic encephalopathies. Nature. 2013;501:217–21.
Michaud JL, Lachance M, Hamdan FF, et al. The genetic landscape of infantile spasms. Hum Mol Genet. 2014;23:4846–58.
Boutry-Kryza N, Labalme A, Ville D, et al. Molecular characterization of a cohort of 73 patients with infantile spasms syndrome. Eur J Med Genet. 2015;58:51–8.
Bertier G, Hétu M, Joly Y, et al. Unsolved challenges of clinical whole-exome sequencing: a systematic literature review of end-users’ views. BMC Med Genet. 2016;9:52.
Gettig J, Cummings JP, Matuszewski K. H.P. Acthar gel and cosyntropin review: clinical and financial implications. P T. 2009;34:250–7.
Go CY, Mackay MT, Weiss SK, Stephens D, Adams-Webber T, Ashwal S, Snead OC. Evidence-based guideline update: medical treatment of infantile spasms: report of the guideline development subcommittee of the American Academy of Neurology and the practice Committee of the Child Neurology Society. Neurology. 2012;78:1974–80.
Arya R, Shinnar S, Glauser T a. Corticosteroids for the treatment of infantile spasms: a systematic review. J Child Neurol. 2012;27:1284–8.
Riikonen R. Recent advances in the pharmacotherapy of infantile spasms. CNS Drugs. 2014;28:279–90.
Glauser TA, Clark PO, Strawsburg R. A pilot study of topiramate in the treatment of infantile spasms. Epilepsia. 1998;39:1324–8.
Iyer A, Appleton R. Improving outcomes in infantile spasms: role of pharmacotherapy. Paediatr Drugs. 2016;18:357–66.
Weber A, Cole JW, Mytinger JR. Infantile spasms respond poorly to topiramate. Pediatr Neurol. 2015;53:130–4.
Suzuki Y, Nagai T, Ono J, Imai K, Otani K, Tagawa T, Abe J, Shiomi M, Okada S. Zonisamide monotherapy in newly diagnosed infantile spasms. Epilepsia. 1997;38:1035–8.
Suzuki Y. Zonisamide in West syndrome. Brain and Development. 2001;23:658–61.
Chandra S, Bhave A, Bhargava R, Kumar C, Kumar R. West syndrome: response to valproate. Front Neurol. 2012;3:166.
Prats JM, Garaizar C, Rua MJ, Garcia-Nieto ML, Madoz P. Infantile spasms treated with high doses of sodium valproate: initial response and follow-up. Dev Med Child Neurol. 1991;33:617–25.
Gümüş H, Kumandaş S, Per H. Levetiracetam monotherapy in newly diagnosed cryptogenic West syndrome. Pediatr Neurol. 2007;37:350–3.
Mikati MA, El Banna D, Sinno D, Mroueh S. Response of infantile spasms to levetiracetam. Neurology. 2008;70:574–5.
Hong AM, Turner Z, Hamdy RF, Kossoff EH. Infantile spasms treated with the ketogenic diet: prospective single-center experience in 104 consecutive infants. Epilepsia. 2010;51:1403–7.
Mytinger JR, Joshi S, Pediatric Epilepsy Research Consortium S on IS. The current evaluation and treatment of infantile spasms among members of the Child Neurology Society. J Child Neurol. 2012;27:1289–94.
•• Knupp KG, Coryell J, Nickels KC, et al. Response to treatment in a prospective national infantile spasms cohort. Ann Neurol. 2016;79:475–84. This prospective study evaluates response to therapy in a large cohort of patients diagnosed with infantile spasms, and suggests a treatment strategy depending upon the etiology of infantile spasms
• Knupp KG, Leister E, Coryell J, et al. Response to second treatment after initial failed treatment in a multicenter prospective infantile spasms cohort. Epilepsia. 2016; doi:10.1111/epi.13557. This prospective study evaluates response to therapy after relapse of infantile spasms, and suggests a treatment strategy for relapses depending upon which first line treatment was ineffective
Hussain SA, Shinnar S, Kwong G, Lerner JT, Matsumoto JH, Wu JY, Shields WD, Sankar R. Treatment of infantile spasms with very high dose prednisolone before high dose adrenocorticotropic hormone. Epilepsia. 2014;55:103–7.
Mytinger JR, Weber A, Heyer GL. The response to ACTH is determined early in the treatment of infantile spasms. Epileptic Disord. 2015;17:52–7.
Westall C a, Wright T, Cortese F, Kumarappah A, Snead OC, Buncic JR. Vigabatrin retinal toxicity in children with infantile spasms: an observational cohort study. Neurology. 2014;83:2262–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Mark P. Fitzgerald and Nicole Ryan declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Neurology
Rights and permissions
About this article
Cite this article
Fitzgerald, M.P., Ryan, N. An Updated, Evidence-Based Clinician’s Guide to the Evaluation and Treatment of West Syndrome. Curr Pediatr Rep 5, 17–23 (2017). https://doi.org/10.1007/s40124-017-0123-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40124-017-0123-x