Abstract
Background
Oligonucleotide therapeutics have emerged as a promising and dynamic class of pharmaceutical agents with remarkable potential for treating a wide spectrum of genetic and acquired diseases. These therapeutic entities, comprising short nucleic acid sequences of either ribonucleic acids (RNA) or deoxyribonucleic acids (DNA), offer the distinct advantage of precise targeting and the ability to interfere with disease-causing genes or proteins. Despite their inherent therapeutic potential, their clinical utility has been hampered by various challenges, including rapid degradation, limited cellular uptake, and unintended immune responses.
Area covered
Chemical modification strategies have been extensively explored to overcome these limitations and enhance their pharmacological properties. In this review, we provide a comprehensive overview of oligonucleotide therapeutics and their associated chemical modification approaches, highlighting their potential in the clinical realm.
Expert opinion
By elucidating the progress made in chemical modifications and their implications for clinical translation, we seek to highlight the pivotal role of these strategies in realizing the full therapeutic potential of oligonucleotide-based therapies for treating a wide range of diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oligonucleotide therapeutics represent a promising and versatile category of pharmaceutical agents, which display considerable potential for addressing several genetic and acquired diseases. This diverse class of therapeutics encompasses antisense oligonucleotides (ASO), small interfering RNA (siRNA), and synthetic miRNA, all of which are composed of abbreviated nucleic acid sequences, either ribonucleic acids (RNA) or deoxyribonucleic acids (DNA). The intrinsic characteristics of these therapeutics, including precise targeting and the ability to interfere with disease-associated genes or proteins, provide them with a unique advantage.
However, the therapeutic efficacy of natural oligonucleotides has been constrained by several challenges, including rapid degradation, limited cellular uptake, and unintended immune responses. The integration of chemical modification in sugar, base and or phosphate moieties in nucleotides has emerged as a potent and versatile toolkit for optimizing the properties of oligonucleotides. These alterations confer improvement in crucial properties of oligonucleotide therapeutics such as increasing stability in biological fluid or reducing off-targeting, thereby facilitates their successful clinical implementation. In this review, we offer a detailed overview of oligonucleotide therapeutics classified with their underlying mechanisms of actions in gene regulation. We also present a variety of chemical modification strategies tailored to the mechanisms of each oligonucleotide therapeutics. Furthermore, we underline the current status of clinical implementations and recent advancements in chemically modified oligonucleotide therapeutics. As researchers persist in refining and innovating these strategies, oligonucleotide-based therapies will assume a pivotal role in the therapeutics against untreated diseases in the coming years.
Synthetic oligonucleotide therapeutics and their mechanism of gene regulation
Chemically synthesized short oligonucleotides, which are classified into three main categories, as ASO, siRNA, and miRNA modulators, have demonstrated significant success in the field of therapeutic development. Each of the classes employs distinct approaches to trigger post-transcriptional gene regulation, making them valuable tools for targeted interventions in various genetic conditions and diseases. Ongoing research strives to refine the design of oligonucleotides to enhance their effectiveness and safety. The optimization of their design is based on a profound understanding of gene regulatory mechanisms. Therefore, to better understand the design of the chemical modification, which will be discussed later, we briefly depict the mode of action.
Antisense oligonucleotide (ASO)
ASOs are synthetic single-stranded oligonucleotides of 18 to 30nt in length, which regulate gene expression in various ways by complementary binding to target mRNA without the intervention of proteins that facilitate the gene regulatory pathway (Fig. 1A). The most commonly used mechanism of ASO action is (1) RNase H mRNA cleavage, which forms a heteroduplex with RNA to recruit RNaseH, resulting in RNA degradation (Wu et al. 2004). ASOs form DNA/RNA heteroduplexes to the target mRNA through Watson–Crick base pairing. These heteroduplexes serve as a substrate of RNaseH and are specifically removed by endonuclease activity (Kuciński et al. 2020). Two forms of RNaseH exist, H1 and H2, each requiring four and one ribonucleotide in the hybrid, respectively, to exhibit endonucleolytic activity (Wu et al. 2013). Among them, RNase H1 mainly plays an important role in the recognition of the DNA-RNA heteroduplex and cleavage of RNA. Several studies have shown a correlation between the expression level of RNaseH1 and the effectiveness of ASO, demonstrating the importance of RNaseH1 in ASO (Vickers and Crooke 2015). As RNaseH.
Mechanisms of action of oligonucleotide therapeutics. A Antisense oligonucleotides bind their complementary sequence of target mRNA to regulate gene expression through the following mechanisms: 1) RNase H1-mediated mRNA degradation; 2) inhibition of translation by steric blocking of ribosome binding to mRNA; and 3) modulation of alternative splicing of premature mRNA to facilitate the expression of functional protein. B miRNA processes and provokes gene silencing via the RNAi pathway, while siRNA and Dicer substrate siRNA induce gene silencing by incorporating into the RNAi process. C miRNA modulators sequester miRNAs from their target mRNAs and reactivate the expression of genes repressed by miRNA
cleaves the DNA-RNA heteroduplex, ASO is released and binds to another mRNA, thereby gradually decreasing the number of target mRNAs and eventually reducing the expression level of the target protein.
(2) Steric blocking is another mechanism that impairs protein complex assembly at the regulatory site of mRNA. The translation of mRNA is initiated by assembly of the initiation protein complex combined at the 5′ cap structure (Bush et al. 2009). The initiation complex scans down through the 5′ sequence, leading full ribosomes to combine when they recognize the AUG translational start site (Hinnebusch 2011). ASOs prevent the initiation of translation by hybridizing with the UTR region of mRNA and physically interfering with the progression of the initiation complex (Kurreck 2003). (3) Exon skipping and (4) Exon inclusion represents another steric hindrance-mediated ASO mechanism associated with the splicing process (Siva et al. 2014; van der Wal et al. 2017). The ASOs that bind to the Exonic Splicing Enhancer (ESE) sequence induce skipping of the exon containing a premature stop codon and proceed with translation, allowing the expression of short but functional proteins (Pramono et al. 1996). Exon inclusion ASOs suppress alternative splicing by interfering with the binding of splicing machinery proteins to Intronic Splicing Silencer (ISS) sequences, restoring specific exons that are crucial for the expression of functional proteins (Hua and Krainer 2012).
siRNA
siRNAs silence target genes through the RNA interference (RNAi) pathway, which is a conserved mechanism of post-transcriptional gene regulation in eukaryotes (Fig. 1B). RNAi initiates the transcription of primary-microRNAs (pri-miRNAs) by RNA polymerase II (Lee et al. 2004; Ha and Kim 2014). The pri-miRNAs are cleaved by the microprocessor, a complex of the nuclear RNase III enzyme Drosha and two double-strand RNA binding proteins (dsRBD) DGCR8, forming stem-loop structured precursor microRNAs (pre-miRNAs) (Lee et al. 2003). The pre-miRNAs are transferred to the cytoplasm through Exportin5 (Hutvagner et al. 2001), where they are further processed by RISC loading complex (RLC), the trimeric protein complex composed of Dicer, TRBP and Argonaute 2 (Ago2). Dicer-TRBP, the cytoplasmic RNaseIII and the dsRBD recognizes pre-miRNA and cleaves into 22-nucleotide mature miRNAs (Wilson et al. 2015; Lee and Doudna 2012). The mature miRNAs are then loaded on the Ago2 protein in the RNA-induced silencing complex (RISC) and inhibit the expression of the target mRNA (Sontheimer 2005).
siRNAs are short duplex RNAs with a 2-nt overhang structure at the 3′ end and mimic endogenous miRNA (Weng et al. 2019). miRNAs consist of single-stranded RNAs called guide and passenger strands; the passenger strand is cleaved and removed during RISC activation, leaving the guide strand in Ago2 (Rand et al. 2005). The mature RISC suppresses target mRNA expression by sequence-specific interaction of the guide strand initiated by matching with the seed region (sequence 2–8 of the guide strand) (Lewis et al. 2005; Meister et al. 2004). Due to the repeated mRNA degradation of RISC, siRNA shows sustained efficiency and requires less frequent dosing compared to RNaseH-based ASO with the same target. Recently, longer siRNAs (25 ~ 30 nt in length) have been proposed as alternative RNAi therapeutics. These longer siRNAs are categorized as Dicer substrate siRNAs, which have been proven to induce more potent gene silencing than conventional siRNA (Kim et al. 2005). The Dicer substrate siRNAs are cleaved by the Dicer enzyme, and the Dicer cleavage step facilitates the loading of antisense strands into the Ago2 protein (Taylor et al. 2013; Snead et al. 2013).
miRNA modulator
siRNA shares the same mechanism with miRNA but triggers more efficient gene silencing. However, slight differences in target determination mechanisms make miRNA another important therapeutic resource. Seed sites capable of binding to miRNA seed regions have been found in several mRNAs encoding various proteins, suggesting that a single miRNA can regulate multiple mRNAs that share the same seed sites. Characterization of this miRNA-mRNA interaction is possible by identifying the evolutionarily conserved 3'UTR region of the miRNA seed site (Lim et al. 2005; Lewis et al. 2005). Indeed, Increased expression of miRNAs has been observed at several discrete stages of T-lymphocyte development, through which miRNAs regulate thymocyte development, differentiation, and cell fate (Neilson et al. 2007; Kunze-Schumacher and Krueger 2020; Tay et al. 2008; Chen et al. 2010). Changes in miRNA expression also represent important triggers for the development of diseases such as cancer, whereby mutations in miRNA involved in the expression of oncogenes or tumor suppressor genes facilitate cancer development (Lee et al. 2015a, b; Chen et al. 2021). In addition, miRNAs play important roles as regulators for cardiovascular function, as well as being potential biomarkers of cardiovascular diseases such as heart failure and atherosclerosis (Gao et al. 2016; Zhou et al. 2018). Owing to the discoveries regarding miRNA regulation, various therapeutic agents that control miRNA levels are under development (Diener et al. 2022). Artificially increasing the amount of miRNA using a synthetic miRNA mimic can be used as a way to enhance the miRNA expression. In contrast, miRNA inhibitors (anti-miRs) suppress miRNA activity through complementary binding to miRNA (Rooij and Eva, and Sakari Kauppinen 2014).
Strategies for the chemical modification of oligonucleotide therapeutics
Early-stage unmodified oligonucleotides have had limited use for in vivo evaluation, which were not a clinically viable route and could not produce a sufficient therapeutic effect. Unmodified oligonucleotides are rapidly degraded by serum/intracellular nuclease (Layzer et al. 2004b). Exogenous oligonucleotides introduced in vivo are recognized as foreign substances by immune receptors such as retinoic acid-inducible gene 1 (RIG-1), melanoma differentiation associated gene 5 (MDA5), protein kinase receptor (PKR), and toll-like receptor subfamilies (TLR3, TLR7, and TLR8), following which, a signaling cascade is initiated, leading to the expression of proinflammatory cytokines such as interleukin-6 (IL-6), tumor necrosis factor-α (TNF-α), and interferon-α (IFN- α). In addition, the innate nature of oligonucleotides restricts their accessibility to various organs or tissues. Because of their small size and negative charge of the phosphodiester backbone, synthetic oligonucleotides are easily eliminated through renal filtration, thereby limiting their cell penetration. Such properties are coupled with susceptibility to nuclease and immune activating properties to promote blood clearance of synthetic oligonucleotides and reduce the amount of oligonucleotide therapeutics that reach the target site (Henry et al. 2000; Karikó et al. 2004; Judge et al. 2005; Jackson and Linsley 2010).
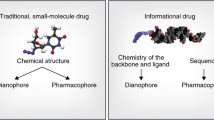
Chemical modification strategies have been developed to overcome these obstacles (Fig. 2). Modification of oligonucleotides can increase nuclease resistance and reduce immunostimulatory effects (Davis et al. 2009). Additionally, such strategies extend their duration of blood circulation through binding to plasma protein, such as albumin, enhance the uptake efficiency and prevent renal filtration, all of which lead to increased stability and a longer half-life in the bloodstream, allowing for better chances of reaching target cells (Huang et al. 2011; Gao et al. 2009). Targeted drug delivery is possible through conjugation of ligands to receptors expressed on specific cell types. The conjugation of mono or polyvalent synthetic triantennary N-acetylgalactosamine (GalNAc) enables the delivery of oligonucleotides into liver cells (Nair et al. 2017b).
Structures of nucleotide analogs used for chemical modification of oligonucleotide therapeutics. Oligonucleotide analogs are categorized by backbone modification, sugar modification, and conjugates. The modified portions of each analog are marked in red. PS phosphorothioate bond, MsPA mesylphosphoramidate bond, PMO phosphorodiamidate morpholino oligomer, 2′-OMe 2'-methoxy, 2'-MOE 2'-methoxyethyl, 2′-F 2′-Fluoro, LNA locked nucleic acid, cEt constrained ethyl LNA, GNA glycol nucleic acid, GalNAc N-acetylgalactosamine
ASO
The gapmer structure of RNaseH-mediated ASO has evolved from the first-generation ASO, which contains phosphorothioate (PS) linkages (Fig. 3A). Due to the larger atomic size of the PS linkage compared to the phosphodiester (PO) bond, PS modification increased resistance against the nucleases of ASO (Dowdy 2017). In addition, PS modification extended the serum half-life and enhanced cellular uptake of ASO by electrostatic and hydrophobic interactions between sulfur in the PS backbone and amino acid side chains within plasma proteins or cell surface proteins (Liang et al. 2015; Shen 2019; Hyjek-Skladanowska et al. 2020; Crooke et al. 2020). The modification methods were further investigated to compensate for the shortcomings of PS modifications, such as reduced hybridization with target RNA (Freier and Altmann 1997) and proinflammatory effects due to the increased binding of proteins associated with immune response (Yanai et al. 2011). The gapmer design takes advantage of PS and ribose modification by including the modification at the flanking ends. Gapmer design consists of DNA nucleotides in the central region and stretches of ribose 2′-OH modifications and PS linkages adjacent to both ends of the sequence. Substitution of the ribose 2ʹ-OH with methoxy (2ʹ-OMe) (Majlessi et al. 1998), methoxyethyl (2ʹ-MOE) (Monia 1997), or Fluoro (2ʹ-F)(Shen et al. 2018), improves resistance against exonuclease and immunostimulatory effects due to increased steric bulk in the vicinity of the 3′ phosphate linkage. In addition, the 2′-OH modification at the flanking region increases the binding affinity with target RNA (Manoharan 1999). As the ribose modification does not support RNaseH1-mediated ASO activity (Yazbeck et al. 2002), a DNA-based gap region is adopted into the center of ASO to serve as a substrate for RNaseH1 upon binding with target RNA. The central DNA gap regions require at least five consecutive deoxyribose residues, and the efficiency of target degradation is maximized when the gap regions are 8–11 nt in length (Kurreck et al. 2002; Grunweller et al. 2003).
Various modification designs applied for improving therapeutic potency of oligonucleotide therapeutics. Schematic illustration of modification designs for A Antisense oligonucleotides, B siRNA, and C miRNA modulator. Modifications are indicated by the symbols at the lower panel. DNA deoxyribonucleic acid, RNA ribonucleic acid, 2′-OMe 2'-methoxy, 2'-MOE 2'-methoxyethyl, 2′-F 2′-Fluoro, LNA locked nucleic acid, cEt constrained ethyl LNA, GNA glycol nucleic acid, PMO phosphorodiamidate morpholino oligomer, PO phosphodiester bond PS phosphorothioate bond, MsPA mesylphosphoramidate bond, GalNAc N-acetylgalactosamine
The modification pattern of the gapmer structure was further improved as additional nucleotide analogs were developed. Due to the covalent bonding between the ribose 2′ oxygen and 4′ carbon, bridged nucleic acid (BNA) oligomers display restricted conformation of C3′-endo sugar pukering, resulting in highly efficient complementary binding to the target RNA compared to the 2′ modified oligomers of the same length (Vester and Wengel 2004). In addition to improving stability and half-life in vivo, LNA inclusion in the gapmer could reduce the total length of the ASO while maintaining its efficacy (Grunweller et al. 2003). However, off-target mediated hepatotoxicity (Kasuya et al. 2016), which is relevant to an excessive increase in target affinity, has been reported as an adverse effect of LNA-modified gapmers (Swayze et al. 2007; Burdick et al. 2014; Kakiuchi-Kiyota et al. 2016). Moreover, the addition of constrained ethyl(cEt) at the covalent bonding between the ribose 2′ and 4′ carbons of LNA suggested a reduction in the potential hepatotoxicity of the LNA gapmer (Burel et al. 2016; Seth et al. 2009). Furthermore, the effect of expanding the range of targets and tissues has also been reported (Shin et al. 2022).
The critical immune stimulatory effects of PS modification, such as complement activation and thrombocytopenia (Crooke et al. 2021), urged the development of an alternative chemical approach for PS modification. Mesylphosphoramidate (MsPA) was initially suggested as an alternative to PS, but total replacement of PS with MsPA has been reported to reduce the efficiency of ASO (Miroshnichenko et al. 2019). Combinatory usage of PS with four consecutive MsPA at the 5′-termini was proposed as a new gapmer design for mitigating the toxicity of PS while maintaining potency (Anderson et al. 2021). Compared to single 2′-Ome inclusion at gap position 2 in the PS gapmer for reducing the cytotoxicity of ASO (Shen et al. 2019), the MsPA gapmer reported improved potency, suggesting minimal impairment of ASO activity.
The chemical modifications that support the effectiveness of ASOs have also evolved toward intensifying steric blocking of RNA–protein binding. Because the steric-blocking ASOs do not support RNaseH activity, 2′-OMe or 2′-MOE modifications were placed on the entire sequence without gap regions. Phosphorodiamidate morpholino (PMO) was developed for steric-blocking ASO by replacing the furanose ring with a morpholine ring and the phosphodiester backbone with a neutral phosphorodiamidate backbone (Hudziak et al. 1996). Unlike PS modification, PMO possesses a neutral charge, which is advantageous for improving the therapeutic efficacy of ASO by blocking electrostatic interactions with nonspecific binding of plasma proteins and subcellular proteins, resulting in efficient target RNA binding (Moulds et al. 1995). The PMO-modified ASO also displayed efficient targeted delivery to skeletal muscle, with such properties making them suitable for application as a treatment for DMD (Duchenne’s Muscular Dystrophy) (Sheng et al. 2020). In addition, the unique flexible phosphorodiamidate linkage made ASOs capable of forming excellent base stacking in aqueous solution (Kang et al. 1992). The conformation of the base stacking completely shields the hydrophobic regions of PMO, significantly increasing its solubility in aqueous environments (Summerton and Weller 1997). The improved water solubility facilitates systemic distribution upon intravenous injection of ASO and accelerates the renal clearance of ASO (Shadid et al. 2021). Furthermore, PMO also has the disadvantage that its uncharged nature reduces cellular uptake (Aoki and Wood 2021); the conjugation of a cell-penetrating peptide to PMO is a current trend to address this (Tsoumpra et al. 2019).
siRNA
The refinement of siRNAs aimed to address critical challenges associated with the in vivo application of siRNA (Fig. 3B). The initially attempted strategies involved the substitution of 2’-OH groups at the termini of siRNA duplex (Hoerter and Walter 2007; Czauderna et al. 2003; Soutschek et al. 2004). Blocking the 3′ termini of the sense strand with an NH2 or inverted abasic modification protected the siRNAs from serum-derived exonuclease activities without significant loss of RNAi activity. In addition, two 2′-OMe substitution at positions 1 and 2 of the 5’ termini of siRNA duplex protect 5’-end of guide strands that particularly vulnerable exonucleolytic degradation due to the thermodynamic asymmetry of the siRNA terminus in RNAi.In addition, substitutions of the ribose 2′-OH residue were introduced into the duplex region of siRNA to improve their immunogenicity and in vivo stability. Sequence-selective introduction of 2′-OMe and 2′-F within siRNA duplexes was achieved by simply adding chemically modified guanine/uridine or cytosine/uridine during phosphoroamidite-based RNA synthesis (Judge et al. 2006; Choung et al. 2006). A modification design for a site-specific rationale was first attempted by alternating 2′-OMe and 2′-F within the siRNA duplex (Hamm et al. 2010; Layzer et al. 2004a). The selectively 2′-OMe and 2′-F modified siRNAs of sense and antisense strand were markedly stable in human serum until 24 h and abolished the TLR7 immunostimulatory potential. However, a series of investigations revealed that the modifications could only be placed at very limited positions in the siRNA duplex (Amarzguioui et al. 2003; Prakash et al. 2005). Introduction of bulky alleles, such as 2′-OMe and 2′-MOE, in specific sites within siRNA could abrogate interactions with RNAi-associated proteins and further gene silencing (Manoharan et al. 2011).
Extensive research has proposed various designs to incorporate 2’-OH modifications into siRNA while avoiding mechanistic blocking of the RNAi pathway. Standard template chemistry (STC) was the first universal modification pattern established by Alnylam (Allerson et al. 2005). Alnylam optimized the siRNA modification pattern that advanced from their full-length alternating 2′-F and 2′-OMe modification. The two PS-bonds at the overhang structure, three consecutive 2′-F nucleotides at the sense strand, and three 2′-OMe nucleotidess at the opposite site of the antisense strand differentiate STC from the parent design. The 2′-OMe at position 9 from the 5’-terminus of the antisense strand blocks Ago2 cleavage during RISC activation (Leuschner et al. 2006). In contrast, the 2′-F at positions 9–11 from the 5’-terminus of the sense strand allows the removal of the sense strand by Ago2 and prevents passenger strand-mediated off-target effects (Song et al. 2017). The 2′-OMe residues at position 14 from the 5’-terminus of the sense strand blocks Ago2 piwi domain interaction with the sense strand and prevents passenger strand loading to RISC (Zheng et al. 2013).
Continuous improvement of Alnylam’s site-specific chemical modification has led to the enhancement of their siRNA design for clinical application. Enhanced stabilization chemistry (ESC) that adds two consecutive PS bonds at the 5′-termini of both sense and antisense strands is the next version of STC (Nair et al. 2014). Additional PO bond substitution significantly improved the stability and pharmacokinetic profile of ESC siRNA, which translated into enhanced in vivo efficacy and extended duration of effect (Nair et al. 2017a). The ESC pattern was further advanced by reducing the 2′-F content within the siRNA duplex. Moreover, in vitro screening across the various RNAi sequences identified minimal positions that require 2′-F replacement in the specific sites of the siRNA duplex (Foster et al. 2018). The increase in the 2′-OMe content enhanced metabolic stability with liver exposure to siRNA, leading to improvements in vivo RNAi activity in mice and non-human primates.
Aiming for high potency and target selectivity, the guide strand sequence is typically designed with perfect matching to the ORF region of target mRNA. However, siRNA suppresses hundreds of non-target mRNAs via miRNA-like post-transcriptional gene regulation (Echeverri et al. 2006; Jackson et al. 2006). The miRNA-like off-target effects are driven by partial matching between the 3′-UTR of mRNAs and the seed region of the guide strand and lead to undesired biological activity (Birmingham et al. 2006). Several chemical modifications have been developed to eliminate this guide strand-mediated off-target effect while retaining their on-target activity. Incorporation of unlocked nucleic acid (UNA) modification into position 7 from the 5’-terminus of the antisense strand has been shown to lower the thermostability of complementary binding of the seed region to the target (Bramsen et al. 2010). Furthermore, destabilization of the seed region pairing required guide strand additional base pairing for target RNA recognition and ruled out off-target recognition that relies on partial complementarity. Moreover, several RISC-associated guide strands initiate non-canonical off-target interactions by forming a transitional “nucleation bulge” at positions 5–6 from the 5’-terminus of the antisense strand and propagating the base pairing to the 3′-end for complete target recognition (Kim et al. 2013). Substitution of a nucleotide at the position 6 with abasic spacer (nucleotide without base) impaired the formation of nucleation bulge during target mRNA recognition and eliminated the miRNA-like off-target effect (Lee et al. 2015a, b). The most recently developed modification pattern from Alnylam aimed to reduce hepatotoxicity induced by the guide strand-mediated off-target effect of GalNAc-conjugated siRNA (Janas et al. 2018; Schlegel et al. 2022). As an extension of the previous design, ESC plus incorporates an additional (S)-isomer glycol nucleic acid ((S)-GNA) at position 7 from the 5’-terminus of the antisense strand. This duplex destabilizing nucleotide does not impair the geometry of siRNA for interaction of Ago2 (Schlegel et al. 2017), mitigates antisense seed region pairing with non-target mRNA, and minimizes the occurrence of off-target driven hepatotoxicity.
Dicer substrate siRNAs have a great potential for use in oligonucleotide therapeutics because they show enhanced RNAi potency compared to conventional siRNAs. However, the bulky moiety of the chemically modified nucleotides interferes with Dicer processing and further RISC loading of substrate RNA. Therefore, the modification pattern must be carefully designed considering the molecular interactions between Dicer and Dicer substrate siRNA. To maintain the functional potency of 25/27-mer Dicer substrate siRNA, a 2′-OMe or 2′-F modification pattern was introduced to avoid the 1–7 position from the 5’-terminus of the antisense strand (18–25 position of the sense strand), which was the predicted site of Dicer processing (Collingwood et al. 2008). Dicerna has been investigated a unique Dicer substrate siRNA platform containing a 5′-GAAA-3′ tetraloop conjugated with triple-GalNAc. Dicerna employed alternating 2′-F and 2′-OMe at the stem region of dicer substrate siRNA with three consecutive 2’-F moieties at the 9–11 position of the sense strand, while introducing a nick at the predicted Dicer cleavage site of the antisense strand to compensate for the inhibition of Dicer cleavage by chemical modification (Morrissey et al. 2005). The chemical modification pattern for Dicer substrate siRNA was further developed based on the position-specific criteria of RLC protein binding to siRNA (Jang et al. 2022). Moreover, a protein-RNA binding kinetic assay confirmed that the position-specific modification patterns retained the interaction of 25-mer siRNA with RLC proteins. Furthermore, the broad applicability of the position-specific modification was further confirmed by the chemically modified RNA nanostructure, which offered enhanced in vivo gene silencing without any immunostimulatory effect.
miRNA modulators
Anti-miR and ASO share a similar MOA in that they induce target inhibition through complementary binding to the target RNA, which implies that their potency is affinity dependent. Therefore, the chemical modification of anti-miR was developed with a similar strategy, which focused on improving target affinity and stability (Fig. 3C) (Lennox and Behlke 2010). PS modification combined with 2′-OH substitutions was used in the initial design of anti-miRs for systemic delivery in vivo (Braasch et al. 2003; Esau et al. 2006). The anti-miRs with a modification pattern containing a PS bond at both temini of 21 mer 2′-OMe were named antagomirs. Partial PS bonds incorporated at the end of the antagomir enhanced stability with enhanced anti-miR function compared to that observed after full-PS modification by supporting the thermodynamic stability of targeted miRNA duplexed with antagomir (Krützfeldt et al. 2005, 2007). In another study, a novel screening assay using a peptide nucleic acid (PNA) competitor was able to rule out the presence of abundant anti-miRs and compare the efficacy of anti-miRs administered at high dosages. In this study, PNA competitor screening compared miR-122 inhibition between 2′-MOE, 2′-OMe, 2′-MOE/LNA chimer, and 2′-F/MOE chimer, the results of which suggested that 2′-F/MOE anti-miR primarily acts by sequestering miRNA from the target site and shows enhanced potency over other modification designs (Davis et al. 2009).
Santaris Pharma has developed an anti-miR with eight LNAs incorporated into a 15-mer PS DNA strand to improve the miR-122 inhibition efficiency (Elmén et al. 2008). The LNA/PS-modified anti-miR122 was administered to a non-human primate through systemic injection, and as a result, showed accumulation in the liver without additional conjugation chemistry, as well as significant downregulation of the miR-122 level. They also observed miRNA antagonism using the 8-mer LNA/PS anti-miR (tiny LNA). Tiny LNAs not only have an anti-miR effect similar to that observed with the 15mer anti-miR, but also had the advantage of simultaneous regulation of overlapping seed regions of miRNA families with potential single biological function (Obad et al. 2011). Minimizing the off-target distribution is critical to maximize efficacy and reduce side effects. Indeed, triantennary GalNAc conjugated to the 5′ end of tiny LNA can be used to reduce spleen accumulation of liver-targeted tiny LNA (Yamamoto et al. 2021).
Regulus Therapeutics conducted a screening assay against a chemically diverse anti-miR library to identify the optimal chemical modification for anti-miR with the greatest miR-17 inhibition (Lee et al. 2019). The optimized 9-mer anti-miR consists of four cEt BNAs and two 2′-OMe at each terminus and three 2′-F in the middle region. The cEt/2′-OMe/2′-F chimeric anti-miR showed a preferential distribution to the kidney for recovery of miR-17-mediated PKD1 and PKD2 gene repression in collecting duct-derived cysts.
Currently developed synthetic oligonucleotide therapeutics and their clinical applications
Oligonucleotide therapeutics undergo rigorous clinical trials to determine their safety and efficacy before they can be approved for use in patients. Oligonucleotide therapeutics with chemical modifications, as mentioned earlier, have been extensively applied in clinical trials. Table 1 and 2 provide some examples of oligonucleotide therapeutics with chemical modifications that have been evaluated in clinical trials.
ASO
Eleven antisense oligonucleotide drugs have been approved thus far; five of them work with RNase H1-mediated RNA degradation and six with steric blocking mechanisms. Fomiversen (Vitravene, ISIS-2922, Ionis) is the first FDA-approved ASO that was developed for immunocompromised patients targeting cytomegalovirus retinitis (CMV) mRNA (Azad et al. 1993). Fomiversen adopted full PS modification and was administered by intravitreal injection without systemic distribution, thereby prolonging the half-life by up to 55 h (Geary et al. 2002). However, it was eventually withdrawn in 2002 following the development of HAARPT (highly active antiretroviral therapy), which combines reverse transcriptase inhibitor and protease inhibitor drugs into an antiviral therapy, and dramatically reduced the number of AIDS(Acquired Immune Deficiency Syndrome)-related CMV(Cytomegalovirus) cases (Duffy et al. 2020). Moreover, Mipomersen (Kynamro, Genzyme) was the first approved gapmer ASO to treat homozygous familial hypercholesterolemia by targeting apolipoprotein B mRNA to lower LDL-C and lipoprotein a level (McGowan et al. 2012). However, it was rejected by the EMA in 2012 because of the risk of increasing transaminase and fatty liver disease (Astaneh et al. 2021). In 2013, Mipomersen was approved by the FDA as only an adjuvant to lipid-lowering therapy for the treatment of homozygous FH; however, ultimately, for unknown reasons, the FDA withdrew its approval in 2019. Nusinersen (Spinraza, Ionis) is a 2′-MOE modified 18-mer developed by Biogen to treat spinal muscular atrophy (SMA), a genetic disorder that affects the motor neurons in the spinal cord, leading to muscle weakness and atrophy (Wurster and Ludolph 2018). Nusinersen, which was granted FDA approval in December 2016, has high specificity for the intron splicing silencer N1 (ISS-N1), which has an inhibitory effect on the inclusion of exon 7, thus inducing exon 7 inclusion in the SMN2 mRNA transcript (Ottesen 2017). As a result, the production of functional survival motor neuron protein, which is deficient in SMA, is increased (Singh and Singh 2018).
Phosphorodiamidate morpholino (PMO)-modified ASOs have been used to elicit the restoration of partially functional truncated dystrophin and treat DMD. Due to adverse side effects, low binding capacity, or low internalization efficiency, PMO has been the only modified ASO to make it through clinical intervention (Roberts et al. 2020). The four FDA-approved drugs currently approved for DMD are Eteplirsen, Golodirsen, Viltolarsen, and Casimersen, which target three exons. Eteplirsen, which is the first dystrophin-restoring, conditionally FDA-approved drug, is a 30-mer PMO designed to restore the reading frame by skipping of exon 51(Akpulat et al. 2018). Golodirsen and Viltolarsen are the second and third antisense PMOs, respectively, which induce exon 53 skipping for the treatment of DMD. Golodirsen(25-mer) is only four bases longer than Viltolarsen(21-mer), otherwise they are the same, but Viltolarsen is shorter and much more potent than Golodirsen (Aartsma-Rus and Corey 2020). Casimersen is an antisense 22-mer PMO, with a similar mechanism of action is to Golodirsen, but the target is exon 45 rather than exon 53. All four drugs have successfully completed initial phase III clinical trials, and their long-term clinical benefits will be evaluated via ongoing longitudinal phase III trials. (NCT02255552, NCT02500381, NCT04687020).
In addition to currently approved drugs, many ASOs are currently undergoing clinical trials targeting expanded indications, some of which will be introduced here. Danvatirsen (AZD9150, AstraZeneca) adopted the cET gapmer structure, which is a short and advanced version of the existing 2′MOE gapmer. Davatirsen is currently being tested in a clinical trial by targeting STAT3 mRNA to more than five indications. Among those indications indication of head and neck cancer is under phase 1/2 clinical study where Davatirsen was used in combination with the anti-PD-L1 antibody drug Durvalumab, developed by AstraZeneca (Ribrag et al. 2021). Along with two therapeutics, Ionis aims to expand the anti-tumor activity of immune checkpoint invitation by overcoming key immunosuppressive mechanisms. In addition, Ionis and other groups have aimed to increase the delivery efficacy of ASO by conjugating GalNAc, the ligand of the hepatocyte surface receptor ASGPR, as a target for hepatocytes. (NCT NCT02549651, NCT03794544, NCT03527147, NCT01839604, NCT03394144, NCT02499328) Pelacarsen (AKCEA-APO-LR, Ionis) is a GalNAc-conjugated ASO that aims to treat cardiovascular disease by reducing the accumulation of apoliopoprotein A in the liver (Yeang et al. 2022). A phase II study of Pelacarsen was completed, which showed reductions in Lp(a) levels in 98% participants (Aoki and Wood 2021), while the phase III study is ready to commence. (NCT05646381, NCT05305664, NCT05026996, NCT01713361) Among the drugs under clinical trials targeting DMD, NS-089/NCNP-02 is particularly notable. (NCT04129294) NS-089/NCNP-02 is the first ASO candidate to target exon 44, and it is assumed that this drug uses a PMO chemistry similar to that of the previous ASO drug, Viltolarsen (Ishizuka et al. 2023). If approved, NS-089/NCNP-02 would be the only available drug targeting exon 44. Recent drugs undergoing clinical trials using DMD as an indication may also conjugate peptides or antibodies to improve cellular uptake and targeted delivery. In particular, many drugs that conjugate cell-penetrating peptides have been developed, termed peptide-conjugate phosphorodiamidate morpholino oligomers (PPMOs) (Sully et al. 2017). SRP-5051 is the most clinically advanced PPMO candidate targeting exon 51 (Sheikh and Yokota 2022). (NCT03375255).
siRNA
The local administration route is sufficient to maintain the stability of siRNAs until they are delivered to target cells, as siRNAs can bypass many physiological barriers. Therefore, siRNAs employed for local administration have introduced simple modification patterns that enough to prevent host immune responses. Cosdosiran (QPI-1007, Quark) is a caspase-2-targeting siRNA having 2′-OMe modification alternating at the guide strand (Solano et al. 2014). Cosdosiran has completed a phase II study for acute primary angle-closure glaucoma (APACG), as well as a phase I study on non-arteritic anterior ischemic optic neuropathy (NAION) (NCT01965106, NCT01064505). Teprasiran (QPI-1002, Quark) was the first systemically administered siRNA to enter a clinical trial (Thielmann et al. 2021). The alternating 2′-OMe-modified Teprasiran is administered intravenously without delivery cargo and targets kidney tubular cells via renal excretion (Peddi et al. 2014). Teprasiran was tested in a completed phase II study for delayed graft function and acute kidney injury (AKI), as well as in a terminated phase III trial for the prevention of cardiac surgery-induced major adverse kidney events (MAKE) (NCT02610296, NCT02610283).
Lipid nanoparticles are a leading approach for the delivery of nucleic acids to targets. Lipid components assemble into LNPs with multilamellar structures and load siRNAs within hydrophilic vesicles (Dilliard and Siegwart 2023). LNPs deliver siRNAs to target cells while shielding unfavorable effects from outside the vesicles. Patisiran (ONPATTRO®, ALN-TTR02, Alnylam) is the first siRNA therapy approved for hereditary transthyretin-mediated amyloidosis (hATTR amyloidosis) treatment (Adams et al. 2018; Coelho et al. 2013). This TTR targeting siRNA contains 11 2′-OMe modified C and U sequence sites. Patisiran is manufactured with an LNP formulation composed of ionizable lipids (DLin-MC3-DMA, DSPC, cholesterol, and PEG2000-C-DMG) (Weng et al. 2019; Jayaraman et al. 2012). During systemic circulation of Patisiran LNPs, the cholesterol component binds to serum ApoE protein leading to selective hepatic accumulation (Akinc et al. 2010).
Various delivery molecules are covalently linked to siRNA for targeted delivery. Because conjugated siRNAs are delivered in naked form, stabilization chemistry should consider the interaction of siRNAs in the surrounding environment. Asymmetric-siRNA (cp-asiRNA, OLX10010, Olix) has a cholesterol conjugated at the 3′ end of the sense strand, enabling broad biodistribution of siRNA (Hwang et al. 2016). This unique structured siRNA contains a short sense strand with alternating 2′-OMe and a guide strand with flanking overhang that is fully modified with 2′-OMe. The consecutive phosphorothioate bonds at the 3′ end of the guide strand to affect the cellular uptake of hydrophobic moiety-conjugated siRNAs (Ly et al. 2020). Zifcasiran (ARO-HIF2, Arrowhead) is an alternating 2′-OMe and 2′-F stabilized siRNA that uses the Targeted RNAi Molecule (TRiM™) Platform (Wong et al. 2018). Moreover, the dynamic polyconjugate (DPC) HIF2α-siRNA consists of an integrin-binding Arg-Gly-Asp (RGD) peptide for renal carcinoma cell targeted delivery (Toth and Cho 2020).
GalNAc is the most successful approach for targeted siRNA delivery because of its excellent delivery efficiency and low toxicity (Zimmermann et al. 2017; Nair et al. 2017a, 2014). Alnylam and other groups introduced GalNAc to siRNAs targeting hepatic disorders (Srivastava et al. 2023; Hartford et al. 2022; O'Donoghue et al. 2022; Zimmermann et al. 2017; Liu et al. 2022). Revusiran (AD-51547) is the first-generation GalNAc-conjugated siRNA for the treatment of hATTR amyloidosis with cardiomyopathy (Zimmermann et al. 2017). However, Revusiran development was discontinued during a phase III study because of deaths caused by an unknown toxicity of siRNA (NCT02319005) (Judge et al. 2020). Currently, the commercial siRNAs used for the treatment of liver disease, Givosiran (ALN-AS1) (Ricci and Ventura 2022; Scott 2020), Inclisiran (ALN-PCSsc) (Frampton 2023; Lamb 2021), Lumasiran (ALN-GO1) (D'Ambrosio and Ferraro 2022; Scott and Keam 2021), and Vutrisiran (ALNTTRsc02) (Keam 2022) adopt the ESC or advanced ESC design. Zilevesiran (ALN-AGT01, Alnylam) employs the most up-to-date modification design, ESC + , and its safety and effectiveness as an add-on therapy of conventional antihypertensive medications has been evaluated in a phase I study (NCT03934307) (Huang et al. 2021). Nedosiran (DCR-PHXC, Dicerna) is the first GalNAc-conjugated Dicer substrate siRNA that has shown promising clinical outcomes, while Nedosiran has completed a phase II study for the treatment of primary hyperoxaluria (Liu et al. 2022) (NCT03847909).
miRNA
LNA modification with high nuclease resistance and PS bond leading to cellular uptake through protein binding has been applied for the delivery of anti-miR therapeutics without delivery cargo Miravirsen (SPC3649, Santaris Pharma) is an LNA/PS anti-miR122 that targets miRNA 122 for the treatment of hepatitis C virus (HCV), which progressed to a phase II through subcutaneous injection without the use of a transfection agent. The effect of reducing HCV RNA and cholesterol levels was confirmed without the need to stop treatment because of side effects. Additionally, a long-term safety and efficacy evaluation was conducted for 36 months after 12 months of Miravirsen monotherapy, although the results have not yet been published (NCT01200420) (Janssen et al. 2013; Ottosen et al. 2015; Lanford et al. 2010). Cobomarsen (MRG-106, miRagen) is an LNA/PS anti-miR155 that targets miRNA 155 for the treatment of cutaneous T-cell lymphoma (CTCL) and mycosis fungoides (MF), which progressed to a phase II clinical trial with intravenous or subcutaneous injection (NCT03713320) (Anastasiadou et al. 2021; Seto et al. 2018). Moreover, CDR132L (Cardior Pharmaceuticals GmbH), an LNA/PS anti-miR32 that targets miR-32 to treat heart failure, was subjected to a phase I clinical trial in which it was administered through intravenous injection. The results of the phase I trial showed that miR-32 expression was decreased in a dose-dependent manner by CDR132L. Phase II clinical trials are ongoing for patients with reduced left ventricular ejection fraction after myocardial infarction. Additionally, in the future, phase II clinical trials of CDR132L reverse remodeling effects will be conducted for patients with heart failure with mildly reduced or preserved ejection fraction and cardiac hypertrophy (NCT05953831) (Täubel et al. 2020). MRG-110 (miRagen) is an LNA/PS anti-miR92a that inhibits miR-92a to promote new blood vessel growth and heal wounds. miRagen progressed to a phase I clinical trial by intradermal injection, the results of which confirmed its ability to reduce miR-92a in a time-dose-dependent manner (NCT03603431) (Abplanalp et al. 2020; Gallant-Behm et al. 2018).
Chemical modification or conjugation has also been used to target anti-miR to specific organs. RG-125 (AZD4076, AstraZeneca) is an anti-miR103/107 targeting miR-103/107 for the treatment of type 2 diabetic subjects with non-alcoholic fatty liver disease. RG-125 is a GalNAc conjugated form that targets hepatocytes. A phase I clinical trial with subcutaneous injection of RG-125 is in progress (NCT02826525) (Vienberg et al. 2017). RGLS4326 (Regulus Therapeutics) is an anti-miR17 targeting miR-17 for the treatment of autosomal dominant polycystic kidney disease. RGLS4326 is a 9-mer PS anti-miR17 with cEt/2′-OMe/2′-F modification for preferential distribution in the kidney, for which a phase I clinical trial was conducted with subcutaneous injection, although the results are yet to be announced (NCT04536688) (Lee et al. 2019).
Conclusion
In this review, we highlight the promise of oligonucleotide therapeutics, as a rapidly evolving class of pharmaceutical agents, which are bestowed with unique advantages of precise targeting and the ability to interfere with disease-associated genes or proteins exhibited by ASO, siRNA, and synthetic miRNA. However, the full realization of their therapeutic potential has been hindered by challenges such as rapid degradation, limited cellular uptake, and unintended immune responses. In this comprehensive review, we report the crucial role of chemical modifications in enhancing the pharmacokinetic and pharmacodynamic properties of oligonucleotide therapeutics. The integration of diverse chemical modification strategies has emerged as a potent and versatile toolkit for optimizing their properties. Persistent refining and innovation of modification chemistry based on the mechanism of action underlying oligonucleotide therapeutics facilitates their translation from laboratory research to clinical applications.
The horizon for oligonucleotide-based treatments appears promising, but the potential drawbacks remain hurdles for oligonucleotide therapeutics to overcome to reach the clinic. The oligonucleotides themselves lack the ability for tissue targeting and are distributed primarily to the liver and kidney for elimination. So far, the efficacy of oligonucleotide therapeutics that require targeting to a specific organ outside the liver may decrease due to their off-target distribution. These drawbacks are realized by limiting pipelines of oligonucleotide therapeutic development to mostly aiming at treating hepatic disorders or rare diseases.
Two broad approaches have been used to overcome the disability of targeting the diseased organ. One such approach has been to create a bioconjugate in which the oligonucleotides are linked to an antibody or proteins that can bind with high affinity to specific biomarkers of target tissues. Another exciting frontier for oligonucleotide therapeutics is the construction of nucleic acid nanostructures through programmable assembly of multiple motifs (e.g., aptamer, ribozymes) for broadening the application range of oligonucleotides (Wu et al. 2020). These nanostructures are being used as molecular scaffolds to promote their accumulation in specific tissues (Yin et al. 2019) or to mount multiple therapeutics into a single molecule (Kim et al. 2022). By overcoming the current obstacles, oligonucleotide therapeutics can reshape the field of medicine. With ongoing research and innovative advancements, we are optimistic that these transformative therapies will eventually find their place in mainstream medical practice, bringing us closer to a new era of precision medicine.
References
Aartsma-Rus A, Corey DR (2020) The 10th oligonucleotide therapy approved: golodirsen for Duchenne muscular dystrophy. Nucleic Acid Ther 30:67–70
Abplanalp WT, Fischer A, John D, Zeiher AM, Gosgnach W, Darville H, Montgomery R, Pestano L, Allée G, Paty I (2020) Efficiency and target derepression of anti-miR-92a: results of a first in human study. Nucleic Acid Ther 30:335–345
Adams D, Gonzalez-Duarte A, O’Riordan WD, Yang CC, Ueda M, Kristen AV, Tournev I, Schmidt HH, Coelho T, Berk JL, Lin KP, Vita G, Attarian S, Plante-Bordeneuve V, Mezei MM, Campistol JM, Buades J, Brannagan TH 3rd, Kim BJ, Oh J, Parman Y, Sekijima Y, Hawkins PN, Solomon SD, Polydefkis M, Dyck PJ, Gandhi PJ, Goyal S, Chen J, Strahs AL, Nochur SV, Sweetser MT, Garg PP, Vaishnaw AK, Gollob JA, Suhr OB (2018) Patisiran, an RNAi therapeutic, for hereditary transthyretin amyloidosis. N Engl J Med 379:11–21
Akinc A, Querbes W, De S, Qin J, Frank-Kamenetsky M, Jayaprakash KN, Jayaraman M, Rajeev KG, Cantley WL, Dorkin JR, Butler JS, Qin L, Racie T, Sprague A, Fava E, Zeigerer A, Hope MJ, Zerial M, Sah DW, Fitzgerald K, Tracy MA, Manoharan M, Koteliansky V, Fougerolles Ad, Maier MA (2010) Targeted delivery of RNAi therapeutics with endogenous and exogenous ligand-based mechanisms. Mol Ther 18:1357–1364
Akpulat U, Wang H, Becker K, Contreras A, Partridge TA, Novak JS, Cirak S (2018) Shorter phosphorodiamidate morpholino splice-switching oligonucleotides may increase exon-skipping efficacy in DMD. Mol Ther-Nucleic Acids 13:534–542
Allerson CR, Sioufi N, Jarres R, Prakash TP, Naik N, Berdeja A, Wanders L, Griffey RH, Swayze EE, Bhat B (2005) Fully 2’-modified oligonucleotide duplexes with improved in vitro potency and stability compared to unmodified small interfering RNA. J Med Chem 48:901–904
Amarzguioui M, Holen T, Babaie E, Prydz H (2003) Tolerance for mutations and chemical modifications in a siRNA. Nucleic Acids Res 31:589–595
Anastasiadou E, Seto AG, Beatty X, Hermreck M, Gilles M-E, Stroopinsky D, Pinter-Brown LC, Pestano L, Marchese C, Avigan D, Trivedi P, Escolar DM, Jackson AL, Slack FJ (2021) Cobomarsen, an Oligonucleotide inhibitor of miR-155, slows DLBCL tumor cell growth in vitro and in vivo. Clin Cancer Res 27:1139–1149
Anderson BA, Freestone GC, Low A, De-Hoyos CL, Iii WJD, Ostergaard ME, Migawa MT, Fazio M, Wan WB, Berdeja A, Scandalis E, Burel SA, Vickers TA, Crooke ST, Swayze EE, Liang X, Seth PP (2021) Towards next generation antisense oligonucleotides: mesylphosphoramidate modification improves therapeutic index and duration of effect of gapmer antisense oligonucleotides. Nucleic Acids Res 49:9026–9041
Aoki Y, Wood MJA (2021) Emerging oligonucleotide therapeutics for rare neuromuscular diseases. J Neuromuscular Dis 8:869–884
Astaneh B, Makhdami N, Astaneh V, Guyatt G (2021) The effect of mipomersen in the management of patients with familial hypercholesterolemia: a systematic review and meta-analysis of clinical trials. J Cardiovasc Dev Dis 8:82
Azad RF, Driver VB, Tanaka K, Crooke RM, Anderson KP (1993) Antiviral activity of a phosphorothioate oligonucleotide complementary to RNA of the human cytomegalovirus major immediate-early region. Antimicrob Agents Chemother 37:1945–1954
Birmingham A, Anderson EM, Reynolds A, Ilsley-Tyree D, Leake D, Fedorov Y, Baskerville S, Maksimova E, Robinson K, Karpilow J, Marshall WS, Khvorova A (2006) 3’ UTR seed matches, but not overall identity, are associated with RNAi off-targets. Nat Methods 3:199–204
Braasch DA, Jensen S, Liu Y, Kaur K, Arar K, White MA, Corey DR (2003) RNA interference in mammalian cells by chemically-modified RNA. Biochemistry 42:7967–7975
Bramsen JB, Pakula MM, Hansen TB, Bus C, Langkjaer N, Odadzic D, Smicius R, Wengel SL, Chattopadhyaya J, Engels JW, Herdewijn P, Wengel J, Kjems J (2010) A screen of chemical modifications identifies position-specific modification by UNA to most potently reduce siRNA off-target effects. Nucleic Acids Res 38:5761–5773
Burdick AD, Sciabola S, Mantena SR, Hollingshead BD, Stanton R, Warneke JA, Zeng M, Martsen E, Medvedev A, Makarov SS, Reed LA, Davis JW 2nd, Whiteley LO (2014) Sequence motifs associated with hepatotoxicity of locked nucleic acid–modified antisense oligonucleotides. Nucleic Acids Res 42:4882–4891
Burel SA, Hart CE, Cauntay P, Hsiao J, Machemer T, Katz M, Watt A, Bui HH, Younis H, Sabripour M, Freier SM, Hung G, Dan A, Prakash TP, Seth PP, Swayze EE, Bennett CF, Crooke ST, Henry SP (2016) Hepatotoxicity of high affinity gapmer antisense oligonucleotides is mediated by RNase H1 dependent promiscuous reduction of very long pre-mRNA transcripts. Nucleic Acids Res 44:2093–2109
Bush MS, Hutchins AP, Jones AME, Naldrett MJ, Jarmolowski A, Lloyd CW, Doonan JH (2009) Selective recruitment of proteins to 5′ cap complexes during the growth cycle in Arabidopsis. Plant J 59:400–412
Chen D, Farwell MA, Zhang B (2010) MicroRNA as a new player in the cell cycle. J Cell Physiol 225:296–301
Chen D, Yang X, Liu M, Zhang Z, Xing E (2021) Roles of miRNA dysregulation in the pathogenesis of multiple myeloma. Cancer Gene Ther 28:1256–1268
Choung S, Kim YJ, Kim S, Park HO, Choi YC (2006) Chemical modification of siRNAs to improve serum stability without loss of efficacy. Biochem Biophys Res Commun 342:919–927
Coelho T, Adams D, Silva A, Lozeron P, Hawkins PN, Mant T, Perez J, Chiesa J, Warrington S, Tranter E, Munisamy M, Falzone R, Harrop J, Cehelsky J, Bettencourt BR, Geissler M, Butler JS, Sehgal A, Meyers RE, Chen Q, Borland T, Hutabarat RM, Clausen VA, Alvarez R, Fitzgerald K, Gamba-Vitalo C, Nochur SV, Vaishnaw AK, Sah DW, Gollob JA, Suhr OB (2013) Safety and efficacy of RNAi therapy for transthyretin amyloidosis. N Engl J Med 369:819–829
Collingwood MA, Rose SD, Huang L, Hillier C, Amarzguioui M, Wiiger MT, Soifer HS, Rossi JJ, Behlke MA (2008) Chemical modification patterns compatible with high potency dicer-substrate small interfering RNAs. Oligonucleotides 18:187–200
Crooke ST, Seth PP, Vickers TA, Liang XH (2020) The interaction of phosphorothioate-containing RNA targeted drugs with proteins is a critical determinant of the therapeutic effects of these agents. J Am Chem Soc 142:14754–14771
Crooke ST, Liang XH, Crooke RM, Baker BF, Geary RS (2021) Antisense drug discovery and development technology considered in a pharmacological context. Biochem Pharmacol 189:114196
Czauderna F, Fechtner M, Dames S, Aygun H, Klippel A, Pronk GJ, Giese K, Kaufmann J (2003) Structural variations and stabilising modifications of synthetic siRNAs in mammalian cells. Nucleic Acids Res 31:2705–2716
D’Ambrosio V, Ferraro PM (2022) Lumasiran in the management of patients with primary hyperoxaluria type 1: from bench to bedside. Int J Nephrol Renovasc Dis 15:197–206
Davis S, Propp S, Freier SM, Jones LE, Serra MJ, Kinberger G, Bhat B, Swayze EE, Frank Bennett C, Esau C (2009) Potent inhibition of microRNA in vivo without degradation. Nucleic Acids Res 37:70–77
Diener C, Keller A, Meese E (2022) Emerging concepts of miRNA therapeutics: from cells to clinic. Trends Genet 38:613–626
Dilliard SA, Siegwart DJ (2023) Passive, active and endogenous organ-targeted lipid and polymer nanoparticles for delivery of genetic drugs. Nat Rev Mater 8:282–300
Dowdy SF (2017) Overcoming cellular barriers for RNA therapeutics. Nat Biotechnol 35:222–229
Duffy K, Arangundy-Franklin S, Holliger P (2020) Modified nucleic acids: replication, evolution, and next-generation therapeutics. BMC Biol 18:112
Echeverri CJ, Beachy PA, Baum B, Boutros M, Buchholz F, Chanda SK, Downward J, Ellenberg J, Fraser AG, Hacohen N, Hahn WC, Jackson AL, Kiger A, Linsley PS, Lum L, Ma Y, Mathey-Prevot B, Root DE, Sabatini DM, Taipale J, Perrimon N, Bernards R (2006) Minimizing the risk of reporting false positives in large-scale RNAi screens. Nat Methods 3:777–779
Elmén J, Lindow M, Schütz S, Lawrence M, Petri A, Obad S, Lindholm M, Hedtjärn M, Hansen HF, Berger U (2008) LNA-mediated microRNA silencing in non-human primates. Nature 452:896–899
Esau C, Davis S, Murray SF, Xing Xian Yu, Pandey SK, Pear M, Watts L, Booten SL, Graham M, McKay R (2006) miR-122 regulation of lipid metabolism revealed by in vivo antisense targeting. Cell Metab 3:87–98
Foster DJ, Brown CR, Shaikh S, Trapp C, Schlegel MK, Qian K, Sehgal A, Rajeev KG, Jadhav V, Manoharan M, Kuchimanchi S, Maier MA, Milstein S (2018) Advanced siRNA designs further improve in vivo performance of GalNAc-siRNA conjugates. Mol Ther 26:708–717
Frampton JE (2023) Inclisiran: a review in hypercholesterolemia. Am J Cardiovasc Drugs 23:219–230
Freier SM, Altmann KH (1997) The ups and downs of nucleic acid duplex stability: structure-stability studies on chemically-modified DNA:RNA duplexes. Nucleic Acids Res 25:4429–4443
Gallant-Behm CL, Piper J, Dickinson BA, Dalby CM, Pestano LA, Jackson AL (2018) A synthetic microRNA-92a inhibitor (MRG-110) accelerates angiogenesis and wound healing in diabetic and nondiabetic wounds. Wound Repair and Regeneration 26:311–323
Gao S, Dagnaes-Hansen F, Nielsen EJB, Wengel J, Besenbacher F, Howard KA, Kjems J (2009) The effect of chemical modification and nanoparticle formulation on stability and biodistribution of siRNA in mice. Mol Ther 17:1225–1233
Gao Y, Peng J, Ren Z, He NY, Li Q, Zhao XS, Wang MM, Wen HY, Tang ZH, Jiang ZS, Wang GX, Liu LS (2016) Functional regulatory roles of microRNAs in atherosclerosis. Clin Chim Acta 460:164–171
Geary RS, Henry SP, Grillone LR (2002) Fomivirsen: clinical pharmacology and potential drug interactions. Clin Pharmacokinet 41:255–260
Grunweller A, Wyszko E, Bieber B, Jahnel R, Erdmann VA, Kurreck J (2003) Comparison of different antisense strategies in mammalian cells using locked nucleic acids, 2’-O-methyl RNA, phosphorothioates and small interfering RNA. Nucleic Acids Res 31:3185–3193
Ha M, Kim VN (2014) Regulation of microRNA biogenesis. Nat Rev Mol Cell Biol 15:509–524
Hamm S, Latz E, Hangel D, Muller T, Yu P, Golenbock D, Sparwasser T, Wagner H, Bauer S (2010) Alternating 2’-O-ribose methylation is a universal approach for generating non-stimulatory siRNA by acting as TLR7 antagonist. Immunobiology 215:559–569
Hartford C, Dain B, Sherman S, Zhang Y, Pavani R, Aurand L, Rofail D, Kelly R (2022) Patient-reported outcomes from a phase 2, randomized trial evaluating the safety and efficacy of Pozelimab and Cemdisiran in patients with paroxysmal nocturnal hemoglobinuria. Blood 140:10849–10850
Henry S, Stecker K, Brooks D, Monteith D, Conklin B, Frank Bennett C (2000) Chemically modified oligonucleotides exhibit decreased immune stimulation in mice. J Pharmacol Exp Ther 292:468–479
Hinnebusch AG (2011) Molecular mechanism of scanning and start codon selection in eukaryotes. Microbiol Mol Biol Rev 75:434–467
Hoerter JA, Walter NG (2007) Chemical modification resolves the asymmetry of siRNA strand degradation in human blood serum. RNA 13:1887–1893
Hua Y, Krainer AR (2012) Antisense-mediated exon inclusion. Exon Skipping: Methods and Protocols 867:307–323
Huang Y, Hong J, Zheng S, Ding Yi, Guo S, Zhang H, Zhang X, Quan Du, Liang Z (2011) Elimination pathways of systemically delivered siRNA. Mol Ther 19:381–385
Huang S, Taubel J, Casey S, Leung PM, Webb DJ, Desai AS, Cheng YS, Rhyee S, Harrop J, Habtemariam B, Bakris GL (2021) Durable reductions in circulating angiotensinogen and blood pressure six months after single doses of ALN-AGT, an RNA interference therapeutic targeting hepatic angiotensinogen synthesis, in hypertensive patients. Circulation. https://doi.org/10.1161/circ.144.suppl_1.10974
Hudziak RM, Barofsky E, Barofsky DF, Doreen l Weller, Sung-Ben Huang, and Dwight D Weller. (1996) Resistance of morpholino phosphorodiamidate oligomers to enzymatic degradation. Antisense Nucleic Acid Drug Develop 6:267–272
Hutvagner G, McLachlan J, Pasquinelli AE, Balint E, Tuschl T, Zamore PD (2001) A cellular function for the RNA-interference enzyme Dicer in the maturation of the let-7 small temporal RNA. Science 293:834–838
Hwang J, Chang C, Kim JH, Oh CT, Lee HN, Lee C, Oh D, Lee C, Kim B, Hong SW, Lee DK (2016) Development of cell-penetrating asymmetric interfering RNA targeting connective tissue growth factor. J Invest Dermatol 136:2305–2313
Hyjek-Skladanowska M, Vickers TA, Napiorkowska A, Anderson BA, Tanowitz M, Crooke ST, Liang XH, Seth PP, Nowotny M (2020) Origins of the increased affinity of phosphorothioate-modified therapeutic nucleic acids for proteins. J Am Chem Soc 142:7456–7468
Jackson AL, Linsley PS (2010) Recognizing and avoiding siRNA off-target effects for target identification and therapeutic application. Nat Rev Drug Discovery 9:57–67
Jackson AL, Burchard J, Schelter J, Chau BN, Cleary M, Lim L, Linsley PS (2006) Widespread siRNA “off-target” transcript silencing mediated by seed region sequence complementarity. RNA 12:1179–1187
Janas MM, Schlegel MK, Harbison CE, Yilmaz VO, Jiang Y, Parmar R, Zlatev I, Castoreno A, Xu H, Shulga-Morskaya S, Rajeev KG, Manoharan M, Keirstead ND, Maier MA, Jadhav V (2018) Selection of GalNAc-conjugated siRNAs with limited off-target-driven rat hepatotoxicity. Nat Commun 9:723
Jang B, Jang H, Kim H, Kim M, Jeong M, Lee GS, Lee K, Lee H (2022) Protein-RNA interaction guided chemical modification of Dicer substrate RNA nanostructures for superior in vivo gene silencing. J Control Release 343:57–65
Jayaraman M, Ansell SM, Mui BL, Tam YK, Chen J, Du X, Butler D, Eltepu L, Matsuda S, Narayanannair JK, Rajeev KG, Hafez IM, Akinc A, Maier MA, Tracy MA, Cullis PR, Madden TD, Manoharan M, Hope MJ (2012) Maximizing the potency of siRNA lipid nanoparticles for hepatic gene silencing in vivo. Angew Chem Int Ed Engl 51:8529–8533
Judge AD, Sood V, Shaw JR, Fang D, McClintock K, MacLachlan I (2005) Sequence-dependent stimulation of the mammalian innate immune response by synthetic siRNA. Nat Biotechnol 23:457–462
Judge AD, Bola G, Lee AC, MacLachlan I (2006) Design of noninflammatory synthetic siRNA mediating potent gene silencing in vivo. Mol Ther 13:494–505
Judge DP, Kristen AV, Grogan M, Maurer MS, Falk RH, Hanna M, Gillmore J, Garg P, Vaishnaw AK, Harrop J, Powell C, Karsten V, Zhang X, Sweetser MT, Vest J, Hawkins PN (2020) Phase 3 multicenter study of revusiran in patients with hereditary transthyretin-mediated (hATTR) Amyloidosis with Cardiomyopathy (ENDEAVOUR). Cardiovasc Drugs Ther 34:357–370
Kakiuchi-Kiyota S, Whiteley LO, Ryan AM, Mathialagan N (2016) Development of a method for profiling protein interactions with LNA-modified antisense oligonucleotides using protein microarrays. Nucleic Acid Ther 26:93–101
Kang H, Ping-Jung Chou W, Curtis Johnson JR, Weller D, Huang S-B, Summerton JE (1992) Stacking interactions of ApA analogues with modified backbones. Biopolymers 32:1351–1363
Karikó K, Bhuyan P, Capodici J, Weissman D (2004) Small interfering RNAs mediate sequence-independent gene suppression and induce immune activation by signaling through toll-like receptor 3. J Immunol 172:6545–6549
Kasuya T, Hori S, Watanabe A, Nakajima M, Gahara Y, Rokushima M, Yanagimoto T, Kugimiya A (2016) Ribonuclease H1-dependent hepatotoxicity caused by locked nucleic acid-modified gapmer antisense oligonucleotides. Sci Rep 6:30377
Keam SJ (2022) Vutrisiran: First approval. Drugs 82:1419–1425
Kim DH, Behlke MA, Rose SD, Chang MS, Choi S, Rossi JJ (2005) Synthetic dsRNA Dicer substrates enhance RNAi potency and efficacy. Nat Biotechnol 23:222–226
Kim KK, Ham J, Chi SW (2013) miRTCat: a comprehensive map of human and mouse microRNA target sites including non-canonical nucleation bulges. Bioinformatics 29:1898–1899
Kim H, Jang B, Lee D, Kwon SC, Lee H (2022) Artificial primary-miRNAs as a platform for simultaneous delivery of siRNA and antisense oligonucleotide for multimodal gene regulation. J Control Release 349:983–991
Krützfeldt J, Rajewsky N, Braich R, Rajeev KG, Tuschl T, Manoharan M, Stoffel M (2005) Silencing of microRNAs in vivo with ‘antagomirs.’ Nature 438:685–689
Krützfeldt J, Kuwajima S, Braich R, Rajeev KG, Pena J, Tuschl T, Manoharan M, Stoffel M (2007) Specificity, duplex degradation and subcellular localization of antagomirs. Nucleic Acids Res 35:2885–2892
Kuciński J, Chamera S, Aleksandra Kmera M, Rowley J, Fujii S, Khurana P, Nowotny M, Wierzbicki AT (2020) Evolutionary history and activity of RNase H1-like proteins in Arabidopsis thaliana. Plant Cell Physiol 61:1107–1119
Kunze-Schumacher H, Krueger A (2020) The Role of MicroRNAs in development and function of regulatory T cells - lessons for a better understanding of MicroRNA biology. Front Immunol 11:2185
Kurreck J (2003) Antisense technologies: improvement through novel chemical modifications. Eur J Biochem 270:1628–1644
Kurreck J, Wyszko E, Gillen C, Erdmann VA (2002) Design of antisense oligonucleotides stabilized by locked nucleic acids. Nucleic Acids Res 30:1911–1918
LA Janssen H, Reesink HW, Lawitz EJ, Zeuzem S, Rodriguez-Torres M, Patel K, Van Der Meer AJ, Patick AK, Chen A, Zhou Yi (2013) Treatment of HCV infection by targeting microRNA. N Engl J Med 368:1685–1694
Lamb YN (2021) Inclisiran: First Approval. Drugs 81:389–395
Lanford RE, Hildebrandt-Eriksen ES, Petri A, Persson R, Lindow M, Munk ME, Kauppinen S, Ørum H (2010) Therapeutic silencing of microRNA-122 in primates with chronic hepatitis C virus infection. Science 327:198–201
Layzer JM, McCaffrey AP, Tanner AK, Huang Z, Kay MA, Sullenger BA (2004a) In vivo activity of nuclease-resistant siRNAs. RNA 10:766–771
Lee HY, Doudna JA (2012) TRBP alters human precursor microRNA processing in vitro. RNA 18:2012–2019
Lee Y, Ahn C, Han J, Choi H, Kim J, Yim J, Lee J, Provost P, Radmark O, Kim S, Kim VN (2003) The nuclear RNase III Drosha initiates microRNA processing. Nature 425:415–419
Lee Y, Kim M, Han J, Yeom KH, Lee S, Baek SH, Kim VN (2004) MicroRNA genes are transcribed by RNA polymerase II. EMBO J 23:4051–4060
Lee HS, Seok H, Lee DH, Ham J, Lee W, Youm EM, Yoo JS, Lee YS, Jang ES, Chi SW (2015a) Abasic pivot substitution harnesses target specificity of RNA interference. Nat Commun 6:10154
Lee HY, Han SS, Rhee H, Park JH, Lee JS, Oh YM, Choi SS, Shin SH, Kim WJ (2015b) Differential expression of microRNAs and their target genes in non-small-cell lung cancer. Mol Med Rep 11:2034–2040
Lee EC, Valencia T, Allerson C, Schairer A, Flaten A, Yheskel M, Kersjes K, Li J, Gatto S, Takhar M (2019) Discovery and preclinical evaluation of anti-miR-17 oligonucleotide RGLS4326 for the treatment of polycystic kidney disease. Nat Commun 10:4148
Lennox KA, Behlke MA (2010) A direct comparison of anti-microRNA oligonucleotide potency. Pharm Res 27:1788–1799
Leuschner PJ, Ameres SL, Kueng S, Martinez J (2006) Cleavage of the siRNA passenger strand during RISC assembly in human cells. EMBO Rep 7:314–320
Lewis BP, Burge CB, Bartel DP (2005) Conserved seed pairing, often flanked by adenosines, indicates that thousands of human genes are microRNA targets. Cell 120:15–20
Liang XH, Sun H, Shen W, Crooke ST (2015) Identification and characterization of intracellular proteins that bind oligonucleotides with phosphorothioate linkages. Nucleic Acids Res 43:2927–2945
Lim LP, Lau NC, Garrett-Engele P, Grimson A, Schelter JM, Castle J, Bartel DP, Linsley PS, Johnson JM (2005) Microarray analysis shows that some microRNAs downregulate large numbers of target mRNAs. Nature 433:769–773
Liu A, Zhao J, Shah M, Migliorati JM, Tawfik SM, Bahal R, Rasmussen TP, Manautou JE, Zhong XB (2022) ’Nedosiran, a Candidate siRNA drug for the treatment of primary hyperoxaluria: design development, and clinical studies. ACS Pharmacol Transl Sci 5:1007–1016
Ly S, Echeverria D, Sousa J, Khvorova A (2020) Single-stranded phosphorothioated regions enhance cellular uptake of cholesterol-conjugated siRNA but not silencing efficacy. Mol Ther Nucleic Acids 21:991–1005
Majlessi M, Nelson NC, Becker MM (1998) Advantages of 2’-O-methyl oligoribonucleotide probes for detecting RNA targets. Nucleic Acids Res 26:2224–2229
Manoharan M (1999) 2’-carbohydrate modifications in antisense oligonucleotide therapy: importance of conformation, configuration and conjugation. Biochim Biophys Acta 1489:117–130
Manoharan M, Akinc A, Pandey RK, Qin J, Hadwiger P, John M, Mills K, Charisse K, Maier MA, Nechev L, Greene EM, Pallan PS, Rozners E, Rajeev KG, Egli M (2011) Unique gene-silencing and structural properties of 2’-fluoro-modified siRNAs. Angew Chem Int Ed Engl 50:2284–2288
McGowan MP, Tardif JC, Ceska R, Burgess LJ, Soran H, Gouni-Berthold I, Wagener G, Chasan-Taber S (2012) Randomized, placebo-controlled trial of mipomersen in patients with severe hypercholesterolemia receiving maximally tolerated lipid-lowering therapy. PLoS ONE 7:e49006
Meister G, Landthaler M, Patkaniowska A, Dorsett Y, Teng G, Tuschl T (2004) Human Argonaute2 mediates RNA cleavage targeted by miRNAs and siRNAs. Mol Cell 15:185–197
Miroshnichenko SK, Patutina OA, Burakova EA, Chelobanov BP, Fokina AA, Vlassov VV, Altman S, Zenkova MA, Stetsenko DA (2019) Mesyl phosphoramidate antisense oligonucleotides as an alternative to phosphorothioates with improved biochemical and biological properties. Proc Natl Acad Sci U S A 116:1229–1234
Monia BP (1997) First- and second-generation antisense inhibitors targeted to human c-raf kinase: in vitro and in vivo studies. Anticancer Drug Des 12:327–339
Morrissey DV, Lockridge JA, Shaw L, Blanchard K, Jensen K, Breen W, Hartsough K, Machemer L, Radka S, Jadhav V, Vaish N, Zinnen S, Vargeese C, Bowman K, Shaffer CS, Jeffs LB, Judge A, MacLachlan I, Polisky B (2005) Potent and persistent in vivo anti-HBV activity of chemically modified siRNAs. Nat Biotechnol 23:1002–1007
Moulds C, Lewis JG, Froehler BC, Grant D, Huang T, Milligan JF, Matteucci MD, Wagner RW (1995) Site and mechanism of antisense inhibition by C-5 propyne oligonucleotides. Biochemistry 34:5044–5053
Nair JK, Willoughby JL, Chan A, Charisse K, Alam MR, Wang Q, Hoekstra M, Kandasamy P, Kel’in AV, Milstein S, Taneja N, O’Shea J, Shaikh S, Zhang L, van der Sluis RJ, Jung ME, Akinc A, Hutabarat R, Kuchimanchi S, Fitzgerald K, Zimmermann T, van Berkel TJ, Maier MA, Rajeev KG, Manoharan M (2014) Multivalent N-acetylgalactosamine-conjugated siRNA localizes in hepatocytes and elicits robust RNAi-mediated gene silencing. J Am Chem Soc 136:16958–16961
Nair JK, Attarwala H, Sehgal A, Wang Q, Aluri K, Zhang X, Gao M, Liu J, Indrakanti R, Schofield S, Kretschmer P, Brown CR, Gupta S, Willoughby JLS, Boshar JA, Jadhav V, Charisse K, Zimmermann T, Fitzgerald K, Manoharan M, Rajeev KG, Akinc A, Hutabarat R, Maier MA (2017a) Impact of enhanced metabolic stability on pharmacokinetics and pharmacodynamics of GalNAc-siRNA conjugates. Nucleic Acids Res 45:10969–10977
Nair JK, Attarwala H, Sehgal A, Wang Q, Aluri K, Zhang X, Minggeng Gao Ju, Liu RI, Schofield S, Kretschmer P, Brown CR, Gupta S, Willoughby JLS, Boshar JA, Jadhav V, Charisse K, Zimmermann T, Fitzgerald K, Manoharan M, Rajeev KG, Akinc A, Hutabarat R, Maier MA (2017b) Impact of enhanced metabolic stability on pharmacokinetics and pharmacodynamics of GalNAc–siRNA conjugates. Nucleic Acids Res 45:10969–10977
Neilson JR, Zheng GX, Burge CB, Sharp PA (2007) Dynamic regulation of miRNA expression in ordered stages of cellular development. Genes Dev 21:578–589
Obad S, dos Santos CO, Petri A, Heidenblad M, Broom O, Ruse C, Cexiong Fu, Lindow M, Stenvang J, Straarup EM (2011) Silencing of microRNA families by seed-targeting tiny LNAs. Nat Genet 43:371–378
O’Donoghue ML, Rosenson RS, Gencer B, Lopez JAG, Lepor NE, Baum SJ, Stout E, Gaudet D, Knusel B, Kuder JF, Ran X, Murphy SA, Wang H, Wu Y, Kassahun H, Sabatine MS, Investigators O-D (2022) Small Interfering RNA to Reduce Lipoprotein(a) in Cardiovascular Disease. N Engl J Med 387:1855–1864
Ottesen EW (2017) ISS-N1 makes the first FDA-approved drug for spinal muscular atrophy. Transl Neurosci 8:1–6
Ottosen S, Parsley TB, Yang Lu, Zeh K, van Doorn L-J, van der Veer E, Raney AK, Hodges MR, Patick AK (2015) In vitro antiviral activity and preclinical and clinical resistance profile of miravirsen, a novel anti-hepatitis C virus therapeutic targeting the human factor miR-122. Antimicrob Agents Chemother 59:599–608
Peddi, V., L. Ratner, M. Cooper, O. Gaber, S. Feng, P. Tso, V. Bowers, R. Naraghi, K. Budde, M. Polinsky, E. Squiers, S. Erlich, and Study Investigators Grp (2014) Treatment with QPI-1002, a Short Interfering (SI) RNA for the Prophylaxis of Delayed Graft Function. Transplantation 98:153–253
Prakash TP, Allerson CR, Dande P, Vickers TA, Sioufi N, Jarres R, Baker BF, Swayze EE, Griffey RH, Bhat B (2005) Positional effect of chemical modifications on short interference RNA activity in mammalian cells. J Med Chem 48:4247–4253
Pramono ZA, Dwi YT, Alimsardjono H, Ishii A, Takeda S-I, Matsuo M (1996) Induction of exon skipping of the dystrophin transcript in lymphoblastoid cells by transfecting an antisense oligodeoxynucleotide complementary to an exon recognition sequence. Biochem Biophys Res Commun 226:445–449
Rand TA, Petersen S, Du F, Wang X (2005) Argonaute2 cleaves the anti-guide strand of siRNA during RISC activation. Cell 123:621–629
Ribrag V, Lee ST, Rizzieri D, Dyer MJS, Fayad L, Kurzrock R, Andritsos L, Bouabdallah R, Hayat A, Bacon L, Jiang Y, Miah K, Delafont B, Hamid O, Anyanwu S, Martinez P, Hess B (2021) A Phase 1b Study to Evaluate the Safety and Efficacy of Durvalumab in Combination With Tremelimumab or Danvatirsen in Patients With Relapsed or Refractory Diffuse Large B-Cell Lymphoma. Clin Lymphoma Myeloma Leuk 21(309–17):e3
Ricci A, Ventura P (2022) Givosiran for the treatment of acute hepatic porphyria. Expert Rev Clin Pharmacol 15:383–393
Roberts TC, Langer R, Wood MJA (2020) Advances in oligonucleotide drug delivery. Nat Rev Drug Discovery 19:673–694
Rooij V, Eva, and Sakari Kauppinen. (2014) Development of micro RNA therapeutics is coming of age. EMBO Mol Med 6:851–864
Schlegel MK, Foster DJ, Kel’in AV, Zlatev I, Bisbe A, Jayaraman M, Lackey JG, Rajeev KG, Charisse K, Harp J, Pallan PS, Maier MA, Egli M, Manoharan M (2017) Chirality Dependent Potency Enhancement and Structural Impact of Glycol Nucleic Acid Modification on siRNA. J Am Chem Soc 139:8537–8546
Schlegel MK, Janas MM, Jiang Y, Barry JD, Davis W, Agarwal S, Berman D, Brown CR, Castoreno A, LeBlanc S, Liebow A, Mayo T, Milstein S, Nguyen T, Shulga-Morskaya S, Hyde S, Schofield S, Szeto J, Woods LB, Yilmaz VO, Manoharan M, Egli M, Charisse K, Sepp-Lorenzino L, Haslett P, Fitzgerald K, Jadhav V, Maier MA (2022) From bench to bedside: Improving the clinical safety of GalNAc-siRNA conjugates using seed-pairing destabilization. Nucleic Acids Res 50:6656–6670
Scott LJ (2020) Givosiran: First Approval. Drugs 80:335–339
Scott LJ, Keam SJ (2021) Lumasiran: First Approval. Drugs 81:277–282
Seth PP, Siwkowski A, Allerson CR, Vasquez G, Lee S, Prakash TP, Wancewicz EV, Witchell D, Swayze EE (2009) Short antisense oligonucleotides with novel 2’-4’ conformationaly restricted nucleoside analogues show improved potency without increased toxicity in animals. J Med Chem 52:10–13
Seto AG, Beatty X, Lynch JM, Hermreck M, Tetzlaff M, Duvic M, Jackson AL (2018) Cobomarsen, an oligonucleotide inhibitor of miR-155, co-ordinately regulates multiple survival pathways to reduce cellular proliferation and survival in cutaneous T-cell lymphoma. Br J Haematol 183:428–444
Shadid M, Badawi M, Abulrob A (2021) Antisense oligonucleotides: absorption, distribution, metabolism, and excretion. Expert Opin Drug Metab Toxicol 17:1281–1292
Sheikh O, Yokota T (2022) Pharmacology and toxicology of eteplirsen and SRP-5051 for DMD exon 51 skipping: An update. Arch Toxicol 96:1–9
Shen W, De Hoyos CL, Sun H, Vickers TA, Liang XH, Crooke ST (2018) Acute hepatotoxicity of 2’ fluoro-modified 5–10-5 gapmer phosphorothioate oligonucleotides in mice correlates with intracellular protein binding and the loss of DBHS proteins. Nucleic Acids Res 46:2204–2217
Shen W, De Hoyos CL, Migawa MT et al (2019) Chemical modification of PS-ASO therapeutics reduces cellular protein-binding and improves the therapeutic index. Nat Biotechnol 37:640–650
Sheng L, Frank Rigo C, Bennett F, Krainer AR, Hua Y (2020) Comparison of the efficacy of MOE and PMO modifications of systemic antisense oligonucleotides in a severe SMA mouse model. Nucleic Acids Res 48:2853–2865
Shin M, Chan IL, Cao Y, Gruntman AM, Lee J, Sousa J, Rodriguez TC, Echeverria D, Devi G, Debacker AJ, Moazami MP, Krishnamurthy PM, Rembetsy-Brown JM, Kelly K, Yukselen O, Donnard E, Parsons TJ, Khvorova A, Sontheimer EJ, Maehr R, Garber M, Watts JK (2022) Intratracheally administered LNA gapmer antisense oligonucleotides induce robust gene silencing in mouse lung fibroblasts. Nucleic Acids Res 50:8418–8430
Singh, Ravindra N, and Natalia N Singh. 2018. 'Mechanism of splicing regulation of spinal muscular atrophy genes', RNA Metabolism in Neurodegenerative Diseases: 31–61.
Siva K, Covello G, Denti MA (2014) Exon-skipping antisense oligonucleotides to correct missplicing in neurogenetic diseases. Nucleic Acid Ther 24:69–86
Snead NM, Wu X, Li A, Cui Q, Sakurai K, Burnett JC, Rossi JJ (2013) Molecular basis for improved gene silencing by Dicer substrate interfering RNA compared with other siRNA variants. Nucleic Acids Res 41:6209–6221
Solano EC, Kornbrust DJ, Beaudry A, Foy JW, Schneider DJ, Thompson JD (2014) Toxicological and pharmacokinetic properties of QPI-1007, a chemically modified synthetic siRNA targeting caspase 2 mRNA, following intravitreal injection. Nucleic Acid Ther 24:258–266
Song X, Wang X, Ma Y, Liang Z, Yang Z, Cao H (2017) Site-Specific Modification Using the 2’-Methoxyethyl Group Improves the Specificity and Activity of siRNAs. Mol Ther Nucleic Acids 9:242–250
Sontheimer EJ (2005) Assembly and function of RNA silencing complexes. Nat Rev Mol Cell Biol 6:127–138
Soutschek J, Akinc A, Bramlage B, Charisse K, Constien R, Donoghue M, Elbashir S, Geick A, Hadwiger P, Harborth J, John M, Kesavan V, Lavine G, Pandey RK, Racie T, Rajeev KG, Rohl I, Toudjarska I, Wang G, Wuschko S, Bumcrot D, Koteliansky V, Limmer S, Manoharan M, Vornlocher HP (2004) Therapeutic silencing of an endogenous gene by systemic administration of modified siRNAs. Nature 432:173–178
Srivastava A, Rangarajan S, Kavakli K, Klamroth R, Kenet G, Khoo L, You CW, Xu WQ, Malan N, Frenzel L, Bagot CN, Stasyshyn O, Chang CY, Poloskey S, Qiu ZY, Andersson S, Mei BS, Pipe SW (2023) Fitusiran prophylaxis in people with severe haemophilia A or haemophilia B without inhibitors (ATLAS-A/B): a multicentre, open-label, randomised, phase 3 trial. Lancet Haematology 10:E322–E332
Sully EK, Geller BL, Li L, Moody CM, Bailey SM, Moore AL, Wong M, Nordmann P, Daly SM, Sturge CR (2017) Peptide-conjugated phosphorodiamidate morpholino oligomer (PPMO) restores carbapenem susceptibility to NDM-1-positive pathogens in vitro and in vivo. J Antimicrob Chemother 72:782–790
Summerton J, Weller D (1997) Morpholino antisense oligomers: design, preparation, and properties. Antisense Nucleic Acid Drug Dev 7:187–195
Swayze EE, Siwkowski AM, Wancewicz EV, Migawa MT, Wyrzykiewicz TK, Hung G, Monia BP, Bennett CF (2007) Antisense oligonucleotides containing locked nucleic acid improve potency but cause significant hepatotoxicity in animals. Nucleic Acids Res 35:687–700
Ishizuka, Takami, Hirofumi Komaki, Yasuko Asahina, Harumasa Nakamura, Norio Motohashi, Eri Takeshita, Yuko Shimizu‐Motohashi, Akihiko Ishiyama, Chihiro Yonee, and Shinsuke Maruyama. 2023. 'Systemic administration of the antisense oligonucleotide NS‐089/NCNP‐02 for skipping of exon 44 in patients with Duchenne muscular dystrophy: Study protocol for a phase I/II clinical trial', Neuropsychopharmacology reports.
Täubel J, Hauke W, Rump S, Viereck J, Batkai S, Poetzsch J, Rode L, Weigt H, Genschel C, Lorch U, Theek C, Levin AA, Bauersachs J, Solomon SD, Thum T (2020) Novel antisense therapy targeting microRNA-132 in patients with heart failure: results of a first-in-human Phase 1b randomized, double-blind, placebo-controlled study. Eur Heart J 42:178–188
Tay Y, Zhang J, Thomson AM, Lim B, Rigoutsos I (2008) MicroRNAs to Nanog, Oct4 and Sox2 coding regions modulate embryonic stem cell differentiation. Nature 455:1124–1128
Taylor DW, Ma E, Shigematsu H, Cianfrocco MA, Noland CL, Nagayama K, Nogales E, Doudna JA, Wang HW (2013) Substrate-specific structural rearrangements of human Dicer. Nat Struct Mol Biol 20:662–670
Thielmann M, Corteville D, Szabo G, Swaminathan M, Lamy A, Lehner LJ, Brown CD, Noiseux N, Atta MG, Squiers EC, Erlich S, Rothenstein D, Molitoris B, Mazer CD (2021) Teprasiran, a small interfering RNA, for the prevention of acute kidney injury in high-risk patients undergoing cardiac surgery: a randomized clinical study. Circulation 144:1133–1144
Toth AT, Cho DC (2020) Emerging therapies for advanced clear cell renal cell carcinoma. J Kidney Cancer VHL 7:17–26
Tsoumpra MK, Fukumoto S, Matsumoto T, Takeda S, Wood MJA, Aoki Y (2019) Peptide-conjugate antisense based splice-correction for Duchenne muscular dystrophy and other neuromuscular diseases. EBioMedicine 45:630–645
van der Wal E, Bergsma AJ, Pijnenburg JM, van der Ploeg AT, Pim WWM, Pijnappel. (2017) Antisense oligonucleotides promote exon inclusion and correct the common c.-32-13T> G GAA splicing variant in Pompe disease. Molecular Therapy-Nucleic Acids 7:90–100
Vester B, Wengel J (2004) LNA (locked nucleic acid): high-affinity targeting of complementary RNA and DNA. Biochemistry 43:13233–13241
Vickers TA, Crooke ST (2015) The rates of the major steps in the molecular mechanism of RNase H1-dependent antisense oligonucleotide induced degradation of RNA. Nucleic Acids Res 43:8955–8963
Vienberg S, Geiger J, Madsen S, Dalgaard LT (2017) MicroRNAs in metabolism. Acta Physiol 219:346–361
Weng Y, Xiao H, Zhang J, Liang XJ, Huang Y (2019) RNAi therapeutic and its innovative biotechnological evolution. Biotechnol Adv 37:801–825
Wilson RC, Tambe A, Kidwell MA, Noland CL, Schneider CP, Doudna JA (2015) Dicer-TRBP complex formation ensures accurate mammalian microRNA biogenesis. Mol Cell 57:397–407
Wong SC, Cheng W, Hamilton H, Nicholas AL, Wakefield DH, Almeida A, Blokhin AV, Carlson J, Neal ZC, Subbotin V, Zhang G, Hegge J, Bertin S, Trubetskoy VS, Rozema DB, Lewis DL, Kanner SB (2018) HIF2alpha-targeted RNAi therapeutic inhibits clear cell renal cell carcinoma. Mol Cancer Ther 17:140–149
Wu H, Lima WF, Zhang H, Fan A, Sun H, Crooke ST (2004) Determination of the role of the human RNase H1 in the pharmacology of DNA-like antisense drugs. J Biol Chem 279:17181–17189
Wu H, Sun H, Liang X, Lima WF, Crooke ST (2013) Human RNase H1 is associated with protein P32 and is involved in mitochondrial pre-rRNA processing. PLoS ONE 8:e71006
Wu X, Wu T, Liu J, Ding B (2020) Gene therapy based on nucleic acid nanostructure. Adv Healthc Mater 9:e2001046
Wurster, Claudia D, and Albert C Ludolph. 2018. "Nusinersen for spinal muscular atrophy." In, 1756285618754459. SAGE Publications Sage UK: London, England.
Yamamoto T, Mukai Y, Wada F, Terada C, Kayaba Y, Kaho Oh, Yamayoshi A, Obika S, Harada-Shiba M (2021) Highly potent GalNAc-conjugated tiny LNA anti-miRNA-122 antisense oligonucleotides. Pharmaceutics 13:817
Yanai H, Chiba S, Ban T, Nakaima Y, Onoe T, Honda K, Ohdan H, Taniguchi T (2011) Suppression of immune responses by nonimmunogenic oligodeoxynucleotides with high affinity for high-mobility group box proteins (HMGBs). Proc Natl Acad Sci U S A 108:11542–11547
Yazbeck DR, Min KL, Damha MJ (2002) Molecular requirements for degradation of a modified sense RNA strand by Escherichia coli ribonuclease H1. Nucleic Acids Res 30:3015–3025
Yeang C, Karwatowska-Prokopczuk E, Su F, Dinh B, Xia S, Witztum JL, Tsimikas S (2022) Effect of pelacarsen on Lipoprotein(a) cholesterol and corrected low-density lipoprotein cholesterol. J Am Coll Cardiol 79:1035–1046
Yin H, Xiong G, Guo S, Xu C, Xu R, Guo P, Shu D (2019) Delivery of Anti-miRNA for triple-negative breast cancer therapy using RNA nanoparticles targeting stem cell marker CD133. Mol Ther 27:1252–1261
Zheng J, Zhang L, Zhang J, Wang X, Ye K, Xi Z, Du Q, Liang Z (2013) Single modification at position 14 of siRNA strand abolishes its gene-silencing activity by decreasing both RISC loading and target degradation. FASEB J 27:4017–4026
Zhou SS, Jin JP, Wang JQ, Zhang ZG, Freedman JH, Zheng Y, Cai L (2018) miRNAS in cardiovascular diseases: potential biomarkers, therapeutic targets and challenges. Acta Pharmacol Sin 39:1073–1084
Zimmermann TS, Karsten V, Chan A, Chiesa J, Boyce M, Bettencourt BR, Hutabarat R, Nochur S, Vaishnaw A, Gollob J (2017) Clinical proof of concept for a novel hepatocyte-targeting GalNAc-siRNA conjugate. Mol Ther 25:71–78
Acknowledgements
This research was supported by the Bio & Medical Technology Development Program of the National Research Foundation (NRF) funded by the Korean government (MSIT) (No. 2018R1A5A2025286, 2022M3E5F1081328, RS-2023-00261343), the Ministry of Science & ICT (No. 2022M3A9H1014125), and the Korean government (Ministry of Food and Drug Safety) (No. 22203MFDS405).
Funding
Korea Health Industry Development Institute,22203MFDS405, Hyukjin Lee, National Research Foundation(NRF), 2018R1A5A2025286, Hyukjin Lee, 2022M3E5F1081328, Hyukjin Lee,National Research Foundation (NRF), RS-2023-00261343, Hyukjin Lee, 2022M3A9H1014125, Hyukjin Lee.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors (Hyunsook Kim, Sujeong Kim, Dayoung Lee, Dahye Lee, Jiyeon Yoon, and Hyukjin Lee) declare that they have no conflict of interest.
Research involving human or animal participants
This article does not contain any studies with human and animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, H., Kim, S., Lee, D. et al. Oligonucleotide therapeutics and their chemical modification strategies for clinical applications. J. Pharm. Investig. 54, 415–433 (2024). https://doi.org/10.1007/s40005-024-00669-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40005-024-00669-8