Abstract
The oral bioavailability of several clinically relevant drugs is compromised because of their limited absorption across the gastrointestinal tract. Active efflux of the drug by transporters such as P-glycoprotein (P-gp) present on the luminal side of the intestinal epithelial cells limits drug absorption. Encapsulation of drugs in nanoparticles can reduce transporter-mediated efflux and increase drug absorption. The purpose of this manuscript is to determine if the bioavailability of doxorubicin, a P-gp substrate, could be increased by encapsulation in nanoparticles. We synthesized polymer-surfactant nanoparticles comprised of a sodium alginate core complexed with doxorubicin and stabilized by the surfactant Aerosol OT (AOT). Encapsulation of doxorubicin in nanoparticles improved its transport across cell monolayers as evidenced by Transwell® studies. Drug uptake studies were carried out in cells overexpressing P-gp and those with basal levels of P-gp. These studies revealed that AOT inhibited P-gp activity and improved drug uptake in P-gp expressing cells by ~5-6-fold. Increase in drug uptake was found only in cells expressing P-gp and was limited to P-gp substrates. We also determined the in vivo oral bioavailability of the nanoparticle formulation of doxorubicin in mice. Doxorubicin delivered in the form of nanoparticles had a higher bioavailability relative to that with the free drug. This study shows that the oral bioavailability of P-gp substrates such as doxorubicin can be enhanced by delivering them in AOT-alginate nanoparticles.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
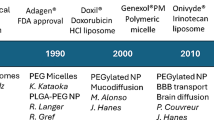
Introduction
Several chemotherapeutics are administered by the intravenous route. Their oral administration can allow self-medication, increase the ease of dosing, and decrease the overall healthcare costs (Findlay et al. 2008). However, poor solubility and/or permeability as well as extensive first pass metabolism result in poor bioavailability (Amidon et al. 1995; Hall et al. 1999), thereby limiting the use of oral route of administration for these drugs (DeMario and Ratain 1998; Findlay et al. 2008).
Efflux transporters present on the luminal (apical) side of the epithelial cells lining the gastrointestinal tract actively pump out the absorbed drug and reduce the amount of drug reaching the systemic circulation (Sparreboom et al. 1997; Hall et al. 1999). Inhibition of these transporters can increase drug absorption and bioavailability (Sparreboom et al. 1997). While many different transporters have been identified, P-glycoprotein (P-gp) is probably the most widely studied. Several drugs with remarkably different chemical structures are known to be substrates of P-gp (Sharom 1997; Aller et al. 2009).
Encapsulation of drugs in nanoparticles can evade P-gp-mediated efflux and enhance drug uptake (Jabr-Milane et al. 2008; Kirtane et al. 2013; Patel et al. 2013; Sosnik 2013). This effect can occur via two mechanisms (Kirtane et al. 2013). First, encapsulation in nanoparticles can protect the drug from interacting with the efflux transporters (Panyam et al. 2002; Murakami et al. 2011). Additionally, some excipients commonly used in nano-formulations inhibit P-gp and other transporters (Bogman et al. 2003; Lo 2003). Due to these potential benefits, several nanoparticle formulations have been tested and shown to improve the oral absorption of chemotherapeutics (Dong and Feng 2005; Das and Chaudhury 2011; Jain et al. 2011; Roger et al. 2012).
We have previously developed polymer-surfactant nanoparticles for the sustained delivery of water-soluble drugs (Chavanpatil et al. 2007b; Usacheva et al. 2014). These nanoparticles comprise an alginate core that allows for encapsulation of weakly basic drugs such as doxorubicin, and are stabilized with an anionic surfactant, dioctyl sodium sulfosuccinate [AerosolⓇ OT (AOT)]. Studies in our lab have shown that these nanoparticles can inhibit P-gp and improve drug uptake in multidrug resistant tumor cells (Chavanpatil et al. 2007a).
In this study, we determined whether AOT-alginate nanoparticles could be used to improve the oral bioavailability of doxorubicin. Our in vitro studies show that AOT inhibits P-gp activity and increases cell uptake of P-gp substrates such as doxorubicin. Our in vivo studies show that doxorubicin dosed in AOT-alginate nanoparticles had improved oral bioavailability relative to that with the free drug.
Materials and methods
Materials
AOT was purchased from Fisher Scientific (Chicago, IL). Doxorubicin was obtained from LKT labs (St Paul, MN). Sodium alginate (viscosity: 15–20 cP, 1% in water), calcium chloride, lucifer yellow and poly(vinyl alcohol) (molecular weight: 30–70 kDa) were purchased from Sigma Aldrich (St Louis, MO). Radioimmunoprecipitation assay (RIPA) buffer and bicinchoninic acid assay kit were purchased from Thermo Scientific (Rockford, IL). Gibco® Minimum Essential Media (MEM) was purchased from Life Technologies (Grand Island, NY). All other chemicals were purchased from Sigma Aldrich (St. Louis, MO).
Synthesis and physiochemical characterization nanoparticles
AOT-alginate nanoparticles loaded with doxorubicin were synthesized as described previously, with minor changes (Chavanpatil et al. 2007a). Briefly, doxorubicin hydrochloride (5 mg) was added to a solution of sodium alginate in water (1 mL, 10 mg/mL) and vortexed for 30 s. The polymer-drug mixture was emulsified in a solution of AOT in chloroform (2.5 mL, 2.5% w/v). The w/o emulsion was sonicated on an ice bath using a probe sonicator (Sonicator XL, Misonix, NY) at a power output of 18–21 W for 3 min. The resultant emulsion was added to aqueous poly(vinyl alcohol) (15 mL, 2.5% w/v) solution. The mixture was sonicated on an ice bath using a probe sonicator at 18–21 W for 5 min. The emulsion was then stirred on a magnetic stir plate (650 rpm), and aqueous calcium chloride solution (5 mL, 60% w/v) was added drop-wise into the emulsion. Chloroform was evaporated overnight under ambient conditions, and then for 2 h under vacuum. Nanoparticles were washed thrice, each time with ~30 mL deionized water by ultracentrifugation (45000 RPM, 45 min, 4 °C; Beckmann, Palo Alto, CA). After the third wash, the nanoparticle dispersion was centrifuged (1000 RPM, 5 min) to remove any aggregates. The supernatant was frozen below −50 °C and lyophilized (Labconco FreeZone 4.5, Kansas city, MO). Dried nanoparticles were stored at −20 °C, and protected from moisture and reconstituted just prior to use. Lyophilized nanoparticles were used in studies within 2–3 weeks after synthesis.
To determine particle size and zeta potential, nanoparticles were dispersed in deionized water (~1 mg/mL) and analyzed by dynamic light scattering (Delsa™ Nano C, Beckmann Coulter, Fullerton, CA).
To determine drug loading, nanoparticles were dispersed in methanol and drug was extracted overnight. The dispersion was then centrifuged (14000 rpm, 15 min) to separate the nanoparticles. Doxorubicin concentration in the supernatant was analyzed using HPLC. A Beckmann Coulter HPLC system with a Synergi Polar RP column (4.6 × 150 mm, 4 μm; Phenomenex, Torrance, CA) was used. The mobile phase was a 78:22 mixture of acetonitrile and 10 mM ammonium acetate with 0.25% v/v acetic acid eluted at a flow rate of mL/min. Sample (50 μL) was injected onto the column using a System Gold 508 Autosampler. Doxorubicin concentration was analyzed using a Jasco Fluoro fluorimeter at excitation/emission wavelengths of 505/550 nm.
To determine how much drug will be lost in the stomach and the systemic release of the drug from the nanoparticles, we examined drug release at acidic pH and physiological pH. Drug release studies were performed in an incubator shaker operating at 37 °C and 100 RPM [C24 incubator shaker, New Brunswick Scientific (now Eppendorf Inc. Enfield, CT)]. Both release studies were carried out under sink conditions. For drug release at pH 7.4, nanoparticles were dispersed in phosphate buffered saline (0.15 mM, pH 7.4; 1X PBS). At various time points, the dispersion was centrifuged to separate nanoparticles from released drug (14000 RPM, 15 min), and the supernatant was analyzed using HPLC. A similar protocol was used for drug release at acidic pH. Hydrochloric acid buffer (pH 1.2) was used instead of 1X PBS.
Cell culture
Madin-Darby Canine Kidney II cells (MDCK-WT) and MDCK cells transfected with human multidrug resistant gene (MDR1) (MDCK-MDR) were obtained from Dr. William Elmquist (University of Minnesota). These cells were used as they are known to form tight junctions (Agarwal et al. 2007), and for their ease of use over the colon carcinoma Caco-2 cell line. Additionally, availability of identical cells with and without P-gp allowed us to perform mechanistic studies (Putnam et al. 2002; Agarwal et al. 2007).
Cells were cultured in MEM media supplemented with 10%v/v fetal bovine serum, 80 ng/mL colchicine and 1% v/v penicillin–streptomycin. The cells were grown at 37 °C in a humidified environment consisting of 5% CO2/95% air.
Transport across MDCK-MDR monolayers
To determine the transport of drug across MDCK-MDR cell monolayers we used a Transwell® assay. About 5 × 105 MDCK-MDR cells were seeded in the upper inserts of a 12-well Transwell® plate (polycarbonate inserts, pore size 0.4 μm) (Corning Costar, Cambridge, MA). Media was changed every alternate day. After 1 week, the transepithelial electrical resistance (TEER) was measured (MilliCell ERS 2, Millipore Co., Bedford, MA). Monolayers having a resistance of >250 Ωcm2 were used for the study (Roger et al. 2012). On the day of the experiment, treatments (free drug or nanoparticles, 2 μg doxorubicin/mL) were added to the upper inserts. At 1, 2 and 4 h, media from the bottom well was sampled and replaced with fresh media. The aliquots were lyophilized, extracted overnight with methanol, and analyzed for doxorubicin concentration by HPLC. TEER values were measured at the end of the experiment, and were found to be unchanged.
Cell uptake of doxorubicin in MDCK-WT and MDCK-MDR cells
We compared the cellular uptake of free drug and nanoparticles in both MDCK-WT and MDCK-MDR cells. About 5 × 104 cells were seeded in a 24-well plate and allowed to adhere overnight. Cells were then treated with either free drug or nanoparticles (doxorubicin concentration: 1 μg/mL or 10 μg/mL). At various time points, treatments were removed, cells were washed twice with cold 1X PBS and then lysed with 0.1 mL RIPA buffer for 0.5 h. The cell lysate was divided into two parts. One part (80 μL) was extracted overnight with 0.5 mL methanol, and doxorubicin concentration in the methanolic extract was determined using HPLC. The second part (20 μL) was analyzed by bicinchoninic acid (BCA) assay to determine cell protein content (ELx800 absorbance microplate reader, Biotek Inc., Winooski, VT). Cell uptake was represented as doxorubicin amount normalized to cell protein content.
Effect of AOT on cellular uptake of doxorubicin or lucifer yellow was determined similarly. Cells were incubated with doxorubicin (0.5 μg/mL) or lucifer yellow (0.5 μM) and different concentrations of AOT. Doxorubicin concentration and cell protein content were analyzed as described before. Lucifer yellow concentration in the cell lysate was analyzed using a fluorescence plate reader (ex/em 485/528) (FLx800 fluorescence microplate reader, Biotek Inc., Winooski, VT) and was normalized to the cell protein concentration.
Oral pharmacokinetics of doxorubicin
The animal studies were performed after receiving approval of the Institutional Animal Care and Use Committee (IACUC) at the University of Minnesota (IACUC approval No. 1402-31304A). The oral absorption of doxorubicin administered either as an aqueous solution or encapsulated in nanoparticles was determined in female C57BL/6 mice (6–8 weeks old). Mice were fasted for 24 h prior to the experiment. Animals were then dosed with doxorubicin solution or nanoparticles (doxorubicin dose: 5 mg /kg, dosing volume: 10 mL/kg, doxorubicin concentration: 0.5 mg/mL). At various time points, cohorts of animals were sacrificed; 0.3–0.6 mL blood was collected by the cardiac stick and lyophilized. Doxorubicin was extracted from the dried samples with 1 mL of a mixture of chloroform (90% v/v) and methanol (10% v/v). The organic solution was separated by centrifugation (1000 RPM, 5 min, 4 °C) and dried under nitrogen. Samples were reconstituted in 0.3 mL methanol and centrifuged (14000 RPM, 15 min, 4 °C). The supernatant was transferred to HPLC vials and analyzed using LC-MS/MS.
LC-MS/MS was performed on an Acquity UPLC system coupled with a Waters/Micromass Quattro Ultima mass spectrometer. Agilent XDB ODS column (4.6 × 50 mm, 1.8 μm) was used as the stationary phase. The mobile phase consisted of 85:15 mixture of acetonitrile and 10 mM ammonium acetate with 0.25% v/v acetic acid eluted at a flow rate of 0.4 mL/min. Doxorubicin was analyzed in the positive ion mode by monitoring the m/z transition from 544→361. The collision voltage, cone voltage and dwell time were set at 20 V, 50 V and 0.4 s, respectively.
Statistical analysis
Differences in transcellular transport, cellular uptake, and blood concentrations following free drug and nanoparticle treatments were analyzed using Student’s t test. Differences in the cell uptake of doxorubicin and lucifer yellow in the presence of various concentrations of AOT were analyzed using one-way ANOVA and post-hoc Tukey test. Differences with p < 0.05 were considered to be statistically significant.
Results
Physicochemical characterization of doxorubicin nanoparticles
Nanoparticles had an average hydrodynamic diameter of 154.7 ± 14.3 nm and a net zeta potential of −16.2 ± 2.2 mV. Drug loading was found to be 4.4 ± 0.8% w/w.
Drug release from nanoparticles was studied under both physiological and acidic pH (Fig. 1). At physiological pH, there was a burst release over the initial 6–8 h. This was followed by a period of zero-order release for the remainder of the study. About 70–80% of the drug was released over 120 h. Drug release under acidic conditions was monitored for a shorter interval to reflect the short gastric transit time. About 20% of the drug was released over 2 h under acidic conditions.
In vitro drug release from nanoparticles. Drug release from nanoparticles was studied under a physiologic (7.4) and b gastric (1.2) pH. Nanoparticles were dispersed in the release buffer and incubated at 37 °C at 100 rpm. At various time points, nanoparticles were separated from released drug by centrifugation. Drug concentration in the release buffer was analyzed using HPLC. Data shown as mean ± S.D., n = 3
Transport of drug across MDCK-MDR monolayers
Transcellular transport of doxorubicin across cell monolayers was determined in a TranswellⓇ study (Fig. 2). We found that the transport of nanoparticle-encapsulated drug was 2–3-fold higher than the free drug at each time point. At the end of 4 h, ~100% of the nanoparticle encapsulated drug was transported to the bottom chamber. In contrast, only ~40% of the free drug was delivered to the bottom chamber over the same time period.
Drug transport across MDCK-MDR cell monolayers. Monolayers of MDCK-MDR cells were formed on Transwell® plate inserts. Nanoparticles or free drug were added to the cells and at various time points, media from the bottom chamber was collected. Drug concentration in the samples was determined using HPLC. Data shown as mean ± S.D., n = 3, *p < 0.05
Doxorubicin uptake in MDCK-MDR and MDCK-WT cells
We reasoned that presence of efflux transporters in cells decreased cellular uptake of doxorubicin, resulting in diminished flux across the cellular monolayer. Encapsulation of doxorubicin in nanoparticles likely overcomes this effect and hence improves flux across the cell monolayer. To test this hypothesis, we measured the cellular uptake of free and nanoparticle-encapsulated drug in MDCK-MDR and MDCK-WT cells. At both drug concentrations tested (1 and 10 μg/mL), nanoparticle-encapsulated drug was taken up better than the free drug in MDCK-MDR cells. At the lower concentration, cell uptake of nanoparticle-encapsulated doxorubicin was twofold higher than free drug (Fig. 3a). Difference in the cell uptake of the two formulations was larger at the higher doxorubicin concentration (Fig. 3b).
Cell uptake of doxorubicin in MDCK MDR and MDCK WT cells. Doxorubicin solution or nanoparticles were incubated with MDCK-MDR cells at a drug concentration of a 1 μg/mL or b 10 μg/mL. In c doxorubicin solution or nanoparticles were incubated with MDCK-WT cells for 0.5 or 2h. Intracellular concentration of doxorubicin was measured using HPLC and normalized to cell protein. Data represented as mean ± S.D., n = 5, *p < 0.05; N.S. indicates differences between groups are not statistically significant at α= 0.05
To determine if the enhanced uptake of nanoparticles was limited to P-gp expressing cells, we tested the cell uptake in MDCK-WT cells. Cell uptake of doxorubicin in MDCK-WT cells was greater than that in MDCK-MDR cells (compare Fig. 3a, c). However, there was no significant difference in the uptake of free drug and nanoparticles in MDCK-WT cells (Fig. 3c). This suggested that the enhanced uptake of nanoparticles in comparison to the free drug was a P-gp mediated effect.
Effect of co-incubation of AOT on cell uptake of doxorubicin and lucifer yellow
A major component of our nanoparticle formulation was the surfactant, AOT. Surfactants are known to improve drug uptake through cell membrane permeabilization (Karande et al. 2004) and inhibition of efflux transporters (Zhang et al. 2003). We therefore determined if AOT had such an effect.
Co-incubation of doxorubicin with AOT led to increased drug uptake in MDCK-MDR cells. AOT increased doxorubicin uptake in a concentration-dependent manner (Fig. 4a). When co-incubated with 10 or 100 μM AOT, drug uptake increased by 5-6-fold. AOT did not have an effect on doxorubicin uptake in MDCK-WT cells (Fig. 4b). Taken together, this data suggested that presence of AOT in nanoparticles likely contributed to the enhanced drug uptake seen in P-gp overexpressing MDCK-MDR cells.
Effect of co-incubation with AOT on cell uptake of doxorubicin in MDCK-MDR cells and MDCK WT cells. a MDCK-MDR cells or b MDCK WT cells were incubated with doxorubicin in solution (0.5 µg/mL) and increasing concentrations of AOT. At 0.5 and 2 h, treatments were removed and intracellular concentration of doxorubicin was analyzed using HPLC. Data represented as mean ± S.D., n = 3–4, *p < 0.05; N.S. indicates differences between groups are not statistically significant at α= 0.05
We also determined the effect of AOT on the uptake of lucifer yellow in MDCK-MDR cells. Due to its high water solubility, lucifer yellow exhibits minimal diffusion across an intact cell membrane (Hanani 2012). The dye accumulates predominantly in endo-lysosomes due its uptake by endocytosis (Sarthy et al. 1982). Hence, permeabilization of the cell membrane can enhance dye uptake. Co-incubation of lucifer yellow with AOT did not increase cell uptake of the dye (Fig. 5). This provided evidence that AOT did not have a membrane permeabilization effect, at least in the concentration range tested in our studies.
Effect of co-incubation of AOT on cell uptake of lucifer yellow in MDCK-MDR cells. MDCK-MDR cells were incubated with lucifer yellow and increasing concentrations of AOT. After 2 h, treatments were removed and intracellular lucifer yellow concentration was determined using a fluorescence plate reader. Data represents mean ± S.D., n = 4, N.S. indicates differences between groups are not statistically significant at α= 0.05
Oral absorption of doxorubicin
We evaluated the pharmacokinetics of doxorubicin following oral dosing (Fig. 6). The absorption of both free and nanoparticle-encapsulated drug was rapid. Tmax was achieved at ~1 h post dose. Animals treated with doxorubicin solution showed low drug levels in the blood as compared to those treated with doxorubicin nanoparticles. Interestingly, higher drug levels in nanoparticle treated animals were observed in the absorption phase (~twofold higher at 0.5 h and ~threefold higher at 1 h). However, drug levels were identical at later time points. Based on the blood concentration–time profile, we calculated the area under the curve (AUC) of doxorubicin in blood. AUC of doxorubicin in animals treated with the solution formulation was ~721 ng × h/mL. When dosed in the form of nanoparticles, the AUC of doxorubicin increased to ~974 ng × h/mL. Pharmacokinetic parameters are listed in Table 1.
Oral pharmacokinetics of doxorubicin. Doxorubicin (as aqueous solution or encapsulated in nanoparticles) was orally administered to mice. At various time points, mice were sacrificed and blood was collected. Doxorubicin concentration in the blood was analyzed using LC-MS/MS. Data represented as mean ± S.E.M., n = 3–4, *p < 0.05
Discussion
The oral route continues to be the most popular route of drug administration (Sastry et al. 2000). Ease of dosing and potential decrease in storage and medical costs are important reasons for its popularity (Borner et al. 2002). However, many drugs suffer from poor solubility, limited permeability, and high first pass metabolism (Aungst 1993; Bardelmeijer et al. 2002; Stegemann et al. 2007; Smith et al. 2011), which renders them unsuitable for oral delivery.
Doxorubicin is a potent chemotherapeutic that is used intravenously to treat many types of cancers (Aubel-Sadron and Londos-Gagliardi 1984). One of the factors limiting the oral use of doxorubicin is its low bioavailability (Ke et al. 2008). There have been two major strategies used to increase the oral bioavailability of doxorubicin. The first strategy utilizes pharmacological inhibitors of P-gp to improve the oral absorption of doxorubicin. For example, Choi et al. found that co-administration of quercetin with doxorubicin increased its bioavailability by ~1.5–2.5 fold (Choi et al. 2011a). Similar results were obtained when myricetin was co-administered with doxorubicin (Choi et al. 2011b). However, the use of small molecule P-gp inhibitors is associated with the potential for severe side effects, limiting the use of this approach (Huang et al. 2010).
Encapsulation of doxorubicin in nanoparticles has also been shown to improve its oral bioavailability. Ke et al. showed that encapsulating doxorubicin in poly(amido amine) (PAMAM) dendrimers led to increased permeability across Caco-2 cell monolayers (Ke et al. 2008). In rats, doxorubicin administered in the dendrimer formulation had a ~300 fold higher bioavailability than the free drug. Kalaria et al. showed that doxorubicin delivered in poly(lactide-co-glycolide) (PLGA) nanoparticles resulted in improved transport across cell monolayers and an increased in vivo oral bioavailability compared to the free drug (Kalaria et al. 2009). Jain and colleagues showed that doxorubicin encapsulated in liposomes coated with polyelectrolytes had a ~5–6 fold higher oral bioavailability than drug in solution in rats (Jain et al. 2012). The increase in bioavailability of doxorubicin upon nano-encapsulation has been attributed to two factors. First, encapsulating doxorubicin in nanoparticles can protect the drug from hepatic enzymes, thereby decreasing its first-pass metabolism. Additionally, nanoparticles can inhibit P-gp mediated efflux of the drug and increased its absorption.
In this report, we studied the oral absorption of doxorubicin encapsulated in nanoparticles composed of a calcium-cross-linked alginate core, surrounded by the anionic surfactant AOT. A key advantage of this delivery system is that both AOT and alginate are approved for oral use. Previous studies in our lab showed that weakly basic, hydrophilic drugs could be loaded efficiently into these nanoparticles, and released over a period of days (Chavanpatil et al. 2007b; Usacheva et al. 2014). We conducted drug release studies at both acidic and physiological pH. In both media, the release of the drug occurred in two phases, an initial burst, followed by a slower constant release phase. The initial burst is not favorable as it may result in significant drug loss before the nanoparticles reach their site of action. Approaches that help minimize burst release will be valuable in further improving the effectiveness of the nanoparticle formulation.
Our previous studies showed that cellular uptake of P-gp substrates such as doxorubicin was dramatically increased when encapsulated in alginate-AOT nanoparticles (Chavanpatil et al. 2007a). Consequently, polymer-surfactant nanoparticles showed potent anti-cancer activity in multi-drug resistant tumors (Khdair et al. 2010). However, the mechanism by which these nanoparticles overcame P-gp efflux was unclear. We compared the uptake of nanoparticles and free drug in MDCK-WT and MDCK-MDR cells. Improved drug uptake with nanoparticles was found only in cells expressing P-gp. Additionally, the increase in drug uptake with nanoparticles was higher at higher concentrations of nanoparticles. We reasoned that higher nanoparticle concentrations led to higher concentration of excipients and hence improved drug uptake. Since surfactants have been shown to improve drug uptake, we investigated the role of AOT on the uptake of doxorubicin. Co-incubation of doxorubicin with AOT led to a dose dependent increase in drug uptake. To determine if the effect of AOT is because of inhibition of P-gp activity or is non-specific (i.e., cell membrane permeabilization), we measured the uptake of doxorubicin in non-P-gp expressing cells. AOT had no effect on the uptake of doxorubicin in non-P-gp expressing cells. Additionally, the uptake of lucifer yellow (a non-substrate of P-gp) in MDCK-MDR cells was also unaffected by the presence of AOT. This provided strong evidence that improved uptake of doxorubicin was mediated by AOT and was facilitated through inhibition of P-gp.
Our in vivo studies show that the relative bioavailability of nanoparticles was higher compared to that with drug in solution. While our in vitro studies show that cell uptake of nanoparticle-encapsulated doxorubicin is enhanced through inhibition of P-gp, it is unclear if the enhanced bioavailability is because of P-gp inhibition. Bioavailability is affected by both drug absorption and first pass metabolism. Nano-encapsulation of doxorubicin can affect both these processes (Jain et al. 2012). The relative contribution of each of these processes is difficult to measure. Using non-biodegradable polystyrene nanoparticles, Reineke et al. showed that nanoparticles are indeed absorbed upon oral administration (Reineke et al. 2013). However, it is unclear if doxorubicin encapsulated in biodegradable nanoparticles (such as those used in our study) is taken up via endocytosis of nanoparticles or upon its release in the gut. It is likely that both pathways occur simultaneously. In such a case, the released drug is susceptible to first pass metabolism and efflux, while nano-encapsulated drug is likely protected from both clearance pathways.
We report here the relative bioavailability of nanoparticles compared to the free drug. Since, both nanoparticles and free drug have different pharmacokinetic profiles, determining absolute bioavailability (F) will require comparison of oral and systemic pharmacokinetics of each formulation. These experiments were beyond the scope of the current study. While relative bioavailability provides information of greater practical importance, determining F can provide better mechanistic insights.
Further enhancement in nanoparticle absorption can potentially be achieved by altering the nanoparticle size and charge. The effect of particle size on the absorption of nanoparticles and microparticles has been explored in great detail. In vitro studies in Caco2 cell monolayers have shown that ~200 nm PLGA nanoparticles have a greater permeability than ~1000 nm particles (Derakhshandeh et al. 2011). Similar size dependency is observed ex vivo in rat intestines as well (He et al. 2012). The in vivo absorption of biodegradable PLGA particles (Desai et al. 1996) and non-biodegradable polystyrene nanoparticles (Reineke et al. 2013) also decreases with an increase in particle size. The effect of charge on oral absorption of nanoparticle is less well studied. However, work with gold nanoparticles suggests that negatively charged nanoparticles have a higher absorption as compared to positively charged nanoparticles of the same size (Schleh et al. 2012). Future studies will determine the effect of size and surface charge of AOT-alginate nanoparticles on oral absorption of encapsulated drugs in detail.
Conclusion
In this study, we reported the use of AOT-alginate nanoparticles for the oral delivery of doxorubicin. AOT-alginate nanoparticles inhibited P-gp activity and improved the cellular uptake of doxorubicin. Nanoparticle-encapsulated doxorubicin demonstrated improved oral bioavailability in vivo compared to the drug in solution.
References
Agarwal S, Jain R, Pal D, Mitra AK (2007) “Functional characterization of peptide transporters in MDCKII-MDR1 cell line as a model for oral absorption studies”. Int J Pharm 332(1–2):147–152
Aller SG, Yu J, Ward A, Weng Y, Chittaboina S, Zhuo R, Harrell PM, Trinh YT, Zhang Q, Urbatsch IL, Chang G (2009) “Structure of P-glycoprotein reveals a molecular basis for poly-specific drug binding”. Science 323(5922):1718–1722
Amidon GL, Lennernas H, Shah VP, Crison JR (1995) “A theoretical basis for a biopharmaceutic drug classification: the correlation of in vitro drug product dissolution and in vivo bioavailability”. Pharm Res 12(3):413–420
Aubel-Sadron G, Londos-Gagliardi D (1984) “Daunorubicin and doxorubicin, anthracycline antibiotics, a physicochemical and biological review”. Biochimie 66(5):333–352
Aungst BJ (1993) “Novel formulation strategies for improving oral bioavailability of drugs with poor membrane permeation or presystemic metabolism”. J Pharm Sci 82(10):979–987
Bardelmeijer HA, Ouwehand M, Buckle T, Huisman MT, Schellens JH, Beijnen JH, van Tellingen O (2002) “Low systemic exposure of oral docetaxel in mice resulting from extensive first-pass metabolism is boosted by ritonavir”. Cancer Res 62(21):6158–6164
Bogman K, Erne-Brand F, Alsenz J, Drewe J (2003) “The role of surfactants in the reversal of active transport mediated by multidrug resistance proteins”. J Pharm Sci 92(6):1250–1261
Borner MM, Schoffski P, de Wit R, Caponigro F, Comella G, Sulkes A, Greim G, Peters GJ, van der Born K, Wanders J, de Boer RF, Martin C, Fumoleau P (2002) “Patient preference and pharmacokinetics of oral modulated UFT versus intravenous fluorouracil and leucovorin: a randomised crossover trial in advanced colorectal cancer”. Eur J Cancer 38(3):349–358
Chavanpatil MD, Khdair A, Gerard B, Bachmeier C, Miller DW, Shekhar MP, Panyam J (2007a) “Surfactant-polymer nanoparticles overcome P-glycoprotein-mediated drug efflux”. Mol Pharm 4(5):730–738
Chavanpatil MD, Khdair A, Panyam J (2007b) “Surfactant-polymer nanoparticles: a novel platform for sustained and enhanced cellular delivery of water-soluble molecules”. Pharm Res 24(4):803–810
Choi JS, Piao YJ, Kang KW (2011a) “Effects of quercetin on the bioavailability of doxorubicin in rats: role of CYP3A4 and P-gp inhibition by quercetin.” Arch Pharm Res 34(4):607–13
Choi SJ, Shin SC, Choi JS (2011b) “Effects of myricetin on the bioavailability of doxorubicin for oral drug delivery in rats: possible role of CYP3A4 and P-glycoprotein inhibition by myricetin.” Arch Pharm Res 34(2):309–15
Das S, Chaudhury A (2011) “Recent advances in lipid nanoparticle formulations with solid matrix for oral drug delivery”. AAPS Pharmscitech 12(1):62–76
DeMario MD, Ratain MJ (1998) “Oral chemotherapy: rationale and future directions”. J Clin Oncol 16(7):2557–2567
Derakhshandeh K, Hochhaus G, Dadashzadeh S (2011) “In-vitro cellular uptake and transport study of 9-nitrocamptothecin PLGA nanoparticles across Caco-2 cell monolayer model”. Iran J Pharm Res 10(3):425–434
Desai MP, Labhasetwar V, Amidon GL, Levy RJ (1996) “Gastrointestinal uptake of biodegradable microparticles: effect of particle size”. Pharm Res 13(12):1838–1845
Dong Y, Feng SS (2005) “Poly(d,l-lactide-co-glycolide)/montmorillonite nanoparticles for oral delivery of anticancer drugs”. Biomaterials 26(30):6068–6076
Findlay M, von Minckwitz G, Wardley A (2008) “Effective oral chemotherapy for breast cancer: pillars of strength”. Ann Oncol 19(2):212–222
Hall SD, Thummel KE, Watkins PB, Lown KS, Benet LZ, Paine MF, Mayo RR, Turgeon DK, Bailey DG, Fontana RJ, Wrighton SA (1999) “Molecular and physical mechanisms of first-pass extraction”. Drug Metab Dispos 27(2):161–166
Hanani M (2012) “Lucifer yellow—an angel rather than the devil”. J Cell Mol Med 16(1):22–31
He C, Yin L, Tang C, Yin C (2012) “Size-dependent absorption mechanism of polymeric nanoparticles for oral delivery of protein drugs”. Biomaterials 33(33):8569–8578
Huang RY, Yu YL, Cheng WC, OuYang CN, Fu E, Chu CL “Immunosuppressive effect of quercetin on dendritic cell activation and function.” (2010) J Immunol 184(12):6815–21
Jabr-Milane LS, van Vlerken LE, Yadav S, Amiji MM (2008) “Multi-functional nanocarriers to overcome tumor drug resistance”. Cancer Treat Rev 34(7):592–602
Jain AK, Swarnakar NK, Godugu C, Singh RP, Jain S (2011) “The effect of the oral administration of polymeric nanoparticles on the efficacy and toxicity of tamoxifen”. Biomaterials 32(2):503–515
Jain S, Patil SR, Swarnakar NK, Agrawal AK (2012) “Oral delivery of doxorubicin using novel polyelectrolyte-stabilized liposomes (layersomes)”. Mol Pharm 9(9):2626–2635
Kalaria DR, Sharma G, Beniwal V, Ravi Kumar MN (2009) “Design of biodegradable nanoparticles for oral delivery of doxorubicin: in vivo pharmacokinetics and toxicity studies in rats”. Pharm Res 26(3):492–501
Karande P, Jain A, Mitragotri S (2004) “Discovery of transdermal penetration enhancers by high-throughput screening”. Nat Biotechnol 22(2):192–197
Ke W, Zhao Y, Huang R, Jiang C, Pei Y (2008) “Enhanced oral bioavailability of doxorubicin in a dendrimer drug delivery system”. J Pharm Sci 97(6):2208–2216
Khdair A, Chen D, Patil Y, Ma L, Dou QP, Shekhar MP, Panyam J (2010) “Nanoparticle-mediated combination chemotherapy and photodynamic therapy overcomes tumor drug resistance”. J Control Release 141(2):137–144
Kirtane AR, Kalscheuer SM, Panyam J (2013) “Exploiting nanotechnology to overcome tumor drug resistance: challenges and opportunities”. Adv Drug Deliv Rev 65(13–14):1731–1747
Lo YL (2003) “Relationships between the hydrophilic-lipophilic balance values of pharmaceutical excipients and their multidrug resistance modulating effect in Caco-2 cells and rat intestines”. J Control Release 90(1):37–48
Murakami M, Cabral H, Matsumoto Y, Wu S, Kano MR, Yamori T, Nishiyama N, Kataoka K (2011) “Improving drug potency and efficacy by nanocarrier-mediated subcellular targeting”. Sci Transl Med 3(64):64ra2
Panyam J, Zhou WZ, Prabha S, Sahoo SK, Labhasetwar V (2002) “Rapid endo-lysosomal escape of poly(DL-lactide-co-glycolide) nanoparticles: implications for drug and gene delivery”. FASEB J 16(10):1217–1226
Patel NR, Pattni BS, Abouzeid AH, Torchilin VP (2013) “Nanopreparations to overcome multidrug resistance in cancer”. Adv Drug Deliv Rev 65(13–14):1748–1762
Putnam WS, Ramanathan S, Pan L, Takahashi LH, Benet LZ (2002) “Functional characterization of monocarboxylic acid, large neutral amino acid, bile acid and peptide transporters, and P-glycoprotein in MDCK and Caco-2 cells”. J Pharm Sci 91(12):2622–2635
Reineke JJ, Cho DY, Dingle YT, Morello AP 3rd, Jacob J, Thanos CG, Mathiowitz E (2013) “Unique insights into the intestinal absorption, transit, and subsequent biodistribution of polymer-derived microspheres”. Proc Natl Acad Sci USA 110(34):13803–8
Roger E, Kalscheuer S, Kirtane A, Guru BR, Grill AE, Whittum-Hudson J, Panyam J (2012) “Folic acid functionalized nanoparticles for enhanced oral drug delivery”. Mol Pharm 9(7):2103–2110
Sarthy PV, Johnson SM, Detwiler PB (1982) “Selective uptake of lucifer yellow by retinal cells”. J Comp Neurol 206(4):371–378
Sastry SV, Nyshadham JR, Fix JA (2000) “Recent technological advances in oral drug delivery—a review”. Pharm Sci Technol Today 3(4):138–145
Schleh C, Semmler-Behnke M, Lipka J, Wenk A, Hirn S, Schaffler M, Schmid G, Simon U, Kreyling WG (2012) “Size and surface charge of gold nanoparticles determine absorption across intestinal barriers and accumulation in secondary target organs after oral administration”. Nanotoxicology 6(1):36–46
Sharom FJ (1997) “The P-glycoprotein efflux pump: how does it transport drugs?” J Membr Biol 160(3):161–175
Smith AJ, Kavuru P, Wojtas L, Zaworotko MJ, Shytle RD (2011) “Cocrystals of quercetin with improved solubility and oral bioavailability”. Mol Pharm 8(5):1867–1876
Sosnik A (2013) “Reversal of multidrug resistance by the inhibition of ATP-binding cassette pumps employing “Generally Recognized As Safe” (GRAS) nanopharmaceuticals: a review”. Adv Drug Deliv Rev 65(13–14):1828–1851
Sparreboom A, van Asperen J, Mayer U, Schinkel AH, Smit JW, Meijer DK, Borst P, Nooijen WJ, Beijnen JH, van Tellingen O (1997) “Limited oral bioavailability and active epithelial excretion of paclitaxel (Taxol) caused by P-glycoprotein in the intestine”. Proc Natl Acad Sci USA 94(5):2031–2035
Stegemann S, Leveiller F, Franchi D, de Jong H, Linden H (2007) “When poor solubility becomes an issue: from early stage to proof of concept”. Eur J Pharm Sci 31(5):249–261
Usacheva M, Swaminathan SK, Kirtane AR, Panyam J (2014) “Enhanced photodynamic therapy and effective elimination of cancer stem cells using surfactant-polymer nanoparticles”. Mol Pharm 11(9):3186–3195
Zhang H, Yao M, Morrison RA, Chong S (2003) “Commonly used surfactant, Tween 80, improves absorption of P-glycoprotein substrate, digoxin, in rats”. Arch Pharm Res 26(9):768–772
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they have no conflict of interest.
Additional information
Ameya R. Kirtane and Priyanka Narayan have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Kirtane, A.R., Narayan, P., Liu, G. et al. Polymer-surfactant nanoparticles for improving oral bioavailability of doxorubicin. Journal of Pharmaceutical Investigation 47, 65–73 (2017). https://doi.org/10.1007/s40005-016-0293-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40005-016-0293-5