Abstract
Stunting is a complex issue in India that has deep-seated health, social, and economic causes. The problem of stunting is a clear indicator of chronic undernutrition and has long-term impacts on both individuals and society. Identifying hot-spot areas with the highest stunting prevalence among children is important for addressing the multifaceted issue of childhood stunting in India. Therefore, we conducted a study to analyze the spatial distribution and identify the predictors of stunted children in India using spatial and multilevel analysis. We analyzed data from the National Family Health Survey-5 and included a sample size of 201,276 children (aged 0–59 months) in 707 districts, 28 states, 8 union territories, and 30,198 clusters throughout India. From Getis-Ord hot spot analysis, we identified Meghalaya, Bihar, Uttar Pradesh, Jharkhand, Assam, Gujarat, Odisha, Madhya Pradesh, Rajasthan, Chhattisgarh, Karnataka, Telangana, and Andhra Pradesh as the hot-spot areas in India for childhood stunting. The study’s findings could be used to develop targeted interventions and strategies to reduce stunting in identified hot-spot areas of India. From multilevel logistic regression analysis, we found that stunting prevalence was greater among male children aged 12–59 months in India, especially those born to young, underweight, uneducated mothers, households with poor sanitation facilities, larger family sizes, and the poorest wealth index. We must prioritize the effective implementation of policies aimed at improving maternal education and basic sanitation facilities, reducing family size, and enhancing the socioeconomic conditions of the poorest households to significantly reduce stunting in India.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Malnutrition continues to be a primary global health challenge affecting millions across countries [11]. The global prevalence of undernourishment increased from 777 million in 2015 to 815 million in 2016 [21]. To address this grave global health challenge, the United Nations declared the 2016–2025 period as the “Decade of Action on Nutrition” [11]. Children are highly vulnerable to malnutrition, leading to stunted growth [8]. Severely malnourished children have a ninefold higher risk of mortality compared to healthy children [25]. Stunting is a low height-for-age in children and can cause permanent physical and mental damage. It is not only linked to child-level factors, such as higher rates of illness and death, but also family and community-level factors [14, 26]. As a result, stunting received global awareness and was included as a target indicator in Sustainable Development Goal 2.
India is a country that is highly affected by malnutrition but is putting immense effort into tackling it; however, the country faces challenges in evaluating progress [15]. Between 2015 and 2021, the number of children in India suffering from stunting, wasting, and underweight slightly decreased. Stunting has gone down from 38 to 36%, wasting from 21 to 19%, and underweight from 36 to 32%. However, malnutrition was responsible for almost 68% of child deaths in 2017 [31]. The severity of the issue necessitates deeper investigations for better understanding [33]. Across different states and districts in India, children face significant differences in their nutritional outcomes, especially stunting [27]. Assessing the spatial variations of stunting across clusters within different states of India could help identify inequities and call for targeted actions. Several studies have been undertaken on the spatial distribution of children’s anthropometric measures in different nations [3, 6, 7, 20, 36]. No prior research has used a spatial and multilevel analysis approach to examine childhood stunting across clusters, utilizing data from the 2019–21 Demographic and Health Survey (DHS) for India. Hence, the study’s main aim was to examine the spatial pattern of stunting prevalence among Indian children and identify the factors that contribute to it.
Materials and Methods
Data Source and Sampling Procedure
The study utilized data from the DHS Program, which offers household-level data on the NFHS-5 (National Family Health Survey-5). A two-stage stratified sample design was used, and the survey was done in two stages. Phase I took place from June 17, 2019, to January 30, 2020, and covered 17 states and 5 union territories. Phase II occurred from January 2, 2020, to April 30, 2021, and included the remaining 11 states and 3 union territories. We used the DHS website (https://dhsprogram.com/data/dataset_admin/index.cfm) to acquire the STATA format data sets. The present study focused on children aged 0–59 months in India. This survey offered reliable estimates to gauge the childhood anthropometric status in India. Details regarding the instruments and protocol utilized for anthropometric measurements during NFHS-5 can be found at http://www.rchiips.org/nfhs. The study examined data from 201,276 children in 707 districts, 28 states, 8 union territories, and 30,198 PSUs (Primary Sampling Units) throughout India. However, we utilized data only from 29,369 PSUs as the information on GPS coordinates was missing for the rest.
Outcome and Independent Variables
Stunting is defined as a height-for-age z-score below − 2 standard deviation (SD). The outcome variable was categorical and coded as 1 for stunted and 0 for non-stunted children. Based on the variables’ theoretical and practical significance and the availability in the DHS dataset, we considered both individual and contextual level factors in our study. Individual-level factors included in this study were the child’s age (0–11, 12–23, 24–35, and ≥ 36 months), sex (male and female), number of children under age five (1, 2, and 3 children), birth order (1–2, 3–4, 5–6, and > 6), maternal body mass index (normal and underweight), the mother’s education (no education, primary, secondary and higher education), maternal age at first birth (< 20, 20–34, and 35–49 years), family size (1–3, 4–5, and ≥ 6), type of sanitation facility (improved and unimproved), and wealth index (poorest, poorer, middle, richer, and richest). The contextual factors included in this study were the place of residence (urban and rural) and regions (northern, central, western, eastern, northeastern, and southern) of India.
Statistical Analysis
We examined the data using spatial analysis, which aids in identifying discrepancies in the distribution of childhood stunting and directing resources to where they are needed. GIS and spatial evaluation tools were utilized to investigate disease prevalence and enhance the application of mapping techniques and data visualization tools to show a better picture of the persisting issue of stunting [29]. By utilizing spatial analysis techniques, it is possible to identify geographic regions with a significant prevalence of stunting and their degree of variation across the administrative zones [10].
Spatial Autocorrelation Analysis
To ascertain whether the spatial distribution of stunting among children in India would be arbitrary, spatial autocorrelation analysis was implemented. The Moran’s Index was a spatial statistic employed to quantify spatial autocorrelation. The output provided the Global Moran’s I value, Z-score, and P value, which could be used to determine if the data exhibited dispersion (-1), randomness (0), or clustering (1). A Moran’s I test with a statistically significant result (P < 0.05) indicated that the null hypothesis (which stated that stunting among children was randomly distributed) could be rejected. This suggested the existence of spatial autocorrelation. Global Moran’s Index can be mathematically represented as
where I denote Moran’s I, \({x}_{i}\) is a size measurement of the ith element in a geographical spatial system (i = 1,2,…,n), μ denotes the mean of \({x}_{i}\), \({v}_{ij}\) denotes the elements in a spatial contiguity matrix (SCM), V [3, 10, 20, 30].
The symbols can be developed in the following manner:
Hot Spot Analysis
In hot spot analysis, the Getis-Ord Gi* statistic was estimated for each feature present in a given dataset. This instrument evaluated each feature in relation to its adjoining features. The statistic Gi* represented a z-score. The p values and z-scores revealed the spatial clustering of features with high or low values.
In the following contexts: xj represents the attribute value for feature j; wi,j denotes the spatial weight that separates features i and j; n signifies the total number of features; and:
A region with a high GI* value indicated hot spot areas (high stunting prevalence), while regions with a low GI* value indicated cool spot areas (low stunting prevalence).
Multilevel Logistic Regression Analysis
Because of the hierarchical structure exhibited by NFHS data (children were arranged in households, which in turn were arranged in clusters), conventional models might underestimate the frequency of frequent errors in effect magnitudes, which could subsequently impact null hypothesis determination. Consequently, a multilevel logistic regression analysis was carried out in lieu of standard logistic regression. Four models were utilized to evaluate the fixed impacts of particular community-level characteristics and the random effects of between-cluster variance [6, 18]. Model 0 was constructed without any independent variables. Hence, measurements of random effects (change among communities) were computed as the ICC (intraclass correlation coefficient) at a statistically significant P value. Model I accounted for variables at the individual level, while Model II incorporated variables at the community level, and Model III accounted for both individual and community-level factors. The fourth model was implemented to examine the potential independent effects of community-level and individual factors on childhood stunting. The study used AOR (adjusted odds ratio) with a 95%CI (confidence interval) to assess how individual factors and community differences affect stunting prevalence in India. Using AIC (Akaike’s information criterion) and BIC (Bayesian information criteria), the quality of fit was evaluated. Upon contrasting the values of each AIC and BIC model, the one with the lowest value was deemed to be the most effective explanatory model.
Sample weights were computed to adjust the unequal probability of selection between each stratum after downloading data. The data were managed and statistically analyzed using the software programs EXCEL, STATA 14.2, and ArcGIS 10.8.
Results
Prevalence of Childhood Stunting in India
Figure 1 depicts the trends in the incidence of stunting among Indian children between NFHS-4 (2015–16) and NFHS-5 (2019–21). The country had seen an overall improvement in nutritional outcomes, with a considerable decrease in stunted children from 38.4% in 2015–16 to 35.5% in 2019–21. However, the stunting prevalence was still high in rural regions, with around 37.30% of children suffering from stunting, while the percentage was relatively lower in urban areas, with 30.10% of children affected.
Figure 2 provides a visual representation of the varying trends in the prevalence of stunted children across various states in India from 2014–15 to 2019–21. The stunting prevalence among children showed significant differences across the states, with some states experiencing a higher percentage of stunting than others. While the prevalence of stunting had slightly reduced in India overall, the states of Meghalaya, Maharashtra, West Bengal, Nagaland, Mizoram, Telangana, Himachal Pradesh, Tripura, and Kerala had recorded a higher percentage of stunting than their previous survey. States in India such as Meghalaya, Maharashtra, West Bengal, Nagaland, Mizoram, Telangana, Himachal Pradesh, Tripura, and Kerala, where food production has been increasing over the years, are also showing a higher prevalence of stunting. This illustrates that the problem cannot be solved solely through increased food production. However, it is also crucial to consider many factors such as consumption, income, accessibility of nutritious and biofortified food, access to healthcare facilities, maternal education, and basic household sanitation facilities [1, 13].
Cluster-Wise Spatial Distribution of Stunting among Indian Children
Figure 3 illustrates the geographical distribution of childhood stunting in India based on clusters. Each cluster represented a fixed number of 22–24 households. Each point on the map represents a cluster defined by the stunting incidence in that specific zone. The green color on the map represents clusters with a lower proportion of childhood stunting, ranging from 0 to 12%. Conversely, the red color on the map indicates areas or clusters with a higher proportion of childhood stunting, ranging from 61 to 100%.
The presented data in Fig. 4 indicate that childhood stunting is not distributed randomly in nearby regions of India. The panels on the right side of the figure showed a clustered pattern (Global Moran’s I value: 0.083), which indicated that similar levels of childhood stunting were clustered together in specific geographical areas in India.
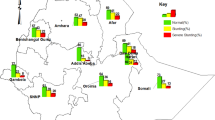
Figure 5 depicts the hot and cold spot areas for stunting in India. The red color indicated significant hot spot areas, and the blue color showed the cold spot areas of childhood stunting. In India, Meghalaya, Bihar, Uttar Pradesh, Jharkhand, Assam, Gujarat, Odisha, Madhya Pradesh, Rajasthan, Chhattisgarh, Karnataka, Andhra Pradesh, and Telangana were the significant hotspot areas for childhood stunting. In India, most of the Northern states (Punjab, Haryana, Chandigarh, Uttarakhand, and Jammu and Kashmir), and some regions of the Southern states (Kerala, Tamil Nadu, and Puducherry) and North-Eastern states (Sikkim, Arunachal Pradesh, and Manipur) were the significant cold spot areas for childhood stunting.
Determinants of Childhood Stunting in India
From Table 1, according to the results obtained from the individual-level factors (Model I), children aged between 12 and 23 months, male children, households with three under-five children, fifth or sixth birth order, underweight mothers, mothers who lacked schooling, larger families, poor sanitation facilities, and poorest families had a higher chance of experiencing stunting. Similarly, from Model II, infants in rural areas and clusters in the central region of India had higher odds of experiencing stunting. The results of Model III revealed that both individual and contextual level factors contributed to childhood stunting in India. Children aged 12–23 months were more prone to stunting than the age group of 0–11 months children [AOR: 2.32; 95% CI: 2.25, 2.40]. When compared to boys, girls were less likely to experience stunting [AOR: 0.92; 95% CI: 0.89, 0.94]. When compared to the households having single under five children, households with three children under five years had a higher probability of experiencing stunting [AOR: 1.28; 95% CI: 1.24, 1.33]. Children with a 5–6 birth order had higher chances of experiencing stunting than children with a 1–2 birth order [AOR: 1.23; 95% CI: 1.16, 1.29]. Children of mothers aged 35–49 years had lower chances of being affected by stunting than children of mothers aged 20–34 years [AOR: 0.90; 95% CI: 0.84, 0.96]. Whereas children with mothers aged < 20 years had a greater likelihood of getting stunted than children of mothers aged 20–34 years [AOR: 1.11; 95% CI: 1.07, 1.15]. Stunting was greater for the offspring of underweight mothers compared to the offspring of normal-weight mothers [AOR: 1.31; 95% CI: 1.28, 1.35]. Mothers with no education were more chances to have stunted children compared to educated mothers [AOR: 1.62; 95% CI: 1.55, 1.69]. Children from larger family sizes had higher odds of stunting than children from smaller family sizes [AOR: 1.06; 95% CI: 1.02, 1.11]. Children from unimproved sanitation facilities were more prone to get stunted than children from improved sanitation facilities [AOR: 1.11; 95% CI: 1.08, 1.14]. Children from the poorest families had higher chances of getting stunted than children from the richest families [AOR:2.14; 95% CI: 2.03, 2.26]. Rural children had lower chances of getting stunted than urban children [AOR: 0.96; 95% CI: 0.92, 0.99]. Children residing in the western region [AOR: 1.22; 95% CI: 1.15, 1.28] and central region [AOR: 1.12; 95% CI: 1.07, 1.17] had more chances of being stunted.
Results of Random Effects
The likelihood of childhood stunting in India varied significantly across the clustering of PSUs, as illustrated by Model 0 [σ2 = 0.57; 95% CI: 0.55–0.59]. Model 0 showed that 14.80% of the variability in childhood stunting among Indian children may be attributable to the differences in ICC, which is equal to 0.148. The inter-cluster variation dropped to 13.2% (0.132) in Model I, 13.8% in Model II, and 13% in Model III, respectively. After doing a multilevel analysis, we determined that Model III was the most appropriate choice out of all the models (Table 1).
Discussion
Stunting is a complex issue in India that has deep-seated health, social, and economic causes. The problem of stunting is a clear indicator of chronic undernutrition and has long-term impacts on both individuals and society. For a country as large and diverse as India, identifying the hot-spot areas with the highest stunting prevalence among children is of utmost importance. This information is critical to effectively addressing the multifaceted issue of childhood stunting. Hence, this study examined the spatial distribution and identified the predictors of stunting in Indian children using NFHS-5 data, 2019–21. Spatial autocorrelation analysis showed that similar levels of childhood stunting were clustered together in specific geographical areas in India. In light of these results, interventions aimed at mitigating childhood stunting would be most efficacious when tailored to particular regions of India. By identifying the areas with the highest and lowest prevalence of stunting, we can focus our efforts and resources to help combat this issue. Hence, the current study has identified the hotspots and cold spots for childhood stunting in India.
Infants aged 12–23 months had more odds of getting stunted in India. Boys were more liable to experience stunting than girls. The possible reasons for gender disparities in child-feeding practices may be due to gender dynamics and preferential feeding practices [2, 3, 32]. Therefore, it is imperative to take decisive action to address this issue and prioritize interventions that ensure boys receive the essential nutrition for their optimal growth. Households with more under-five children (three) had more chances of facing stunting than households with a single child in the same age group. This information aligns with similar findings reported in the literature [28, 34]. Having multiple children in the same household can increase the pressure on caregivers to distribute food. Further, children with a birth order of 5–6 have more chances to experience stunted growth than those with a 1–2 birth order, as reported in previous studies [16, 19]. Additionally, kids whose mothers were < 20 years old were more inclined toward stunting than those mothers 20 and 34 years old. Young mothers who come from low-income families or have low economic backgrounds and have dropped out of school may lack the knowledge to care for their children properly. Children born to mothers 35–49 years old have a lower likelihood of experiencing stunted growth compared to those born to mothers 20–34 years old. This suggests a correlation between maternal age and child development, with advanced maternal age potentially providing benefits for child growth and health [9, 35]. Specifically, underweight mothers were realized to have a greater likelihood of bearing children with stunted growth than mothers who had a normal BMI. Research conducted in the past has revealed a significant correlation between the mother’s BMI and the growth of their offspring [4, 24]. Stunting could be due to biological factors such as intrauterine growth restriction, insufficient breast milk production, or food insecurity. Kids innate to uneducated or less educated mothers were more susceptible to experiencing stunted growth than those innate to highly educated mothers. Educated mothers know proper childcare practices, engage in healthy actions during gravidity and lactation, exhibit better health-seeking behavior, be financially stable, and practice appropriate child feeding [5, 23]. Children who grew up in households with a larger size of 6 or more members faced a higher risk of stunting. In households with a greater number of family members, there may be a reduced amount of food available for each individual, even when compared to households with fewer members but the same level of economic power. Moreover, children who lack access to improved sanitation facilities were 1.11 times more prone to experiencing stunted growth due to inadequate hygiene and sanitation practices. These practices are often products of poverty, lack of infrastructure, deep-rooted societal beliefs and norms, cultural traditions, and insufficient awareness [1]. Kids from the poorest family backgrounds were more prone to stunting than those from the wealthiest family backgrounds [2, 4, 17, 29]. The poorest families are at risk of stunting due to insufficient food, inadequate access to primary healthcare, and heightened infection susceptibility. Urban children had a higher chance of being stunted in India. This outcome aligns with the results of a past study [22]. Extensive research suggests that urban–rural child nutrition disparities stem from wealth, maternal education, and health service access. The study has revealed significant regional disparities in stunting among children across different regions in India. These disparities in childhood stunting can be attributed to variations in maternal education, economic prosperity, hygiene practices, health service access, and child-rearing practices [12].
Conclusions
India is currently grappling with a serious issue of stunted growth among children, and immediate action is required to tackle this public health crisis. Although the prevalence has decreased marginally among children, the situation remains alarming. Stunting is not evenly spread across the country and is concentrated in certain regions of India, with varying degrees of prevalence. In India, the hot spot areas for childhood stunting were Meghalaya, Jharkhand, Bihar, Uttar Pradesh, Assam, Gujarat, Odisha, Madhya Pradesh, Rajasthan, Karnataka, Chhattisgarh, Andhra Pradesh, and Telangana. To address this problem effectively, it is crucial to develop targeted interventions and strategies that cater to the high-risk populations in these areas. By prioritizing and investing in these hot spot areas, we can create a healthier and more prosperous future for our children. From multilevel logistic regression analysis, the age and gender of the child, the number of under-five children, birth order, maternal BMI, mother’s education, mother’s age at first birth, family size, type of sanitation facility, household wealth index, place of residence, and region were identified as significant predictors of stunting. Stunting prevalence was greater among male children aged 12–59 months in India, especially those born to young, underweight, uneducated mothers, households with poor sanitation facilities, larger family sizes, and the poorest wealth index. These significant predictors were crucial to consider and tackle effectively the issue of stunting in India. The study strongly supports the need for more effective implementation of nutritional interventional policies in India addressing maternal education, basic sanitation facilities, family size reduction, and improvement of socioeconomic conditions in the poorest households.
Future research could investigate the impact of existing nutritional intervention programs and policies in India that specifically address the nutritional outcomes of women and children. It also needs to investigate how advancements and interventions in agriculture can bolster the nation’s food security and nutrition.
Data Availability
The manuscript, code book, and analytic code contain data that will be made available upon reasonable request. The data are stored in a public, open-access repository. MEASURE DHS provided the relevant data, which can be obtained from the DHS Program (https://dhsprogram.com/data/dataset_admin/index.cfm).
References
Aguayo VM, Menon P (2016) Stop stunting: improving child feeding, women’s nutrition and household sanitation in South Asia. Matern Child Nutr 12:3–11. https://doi.org/10.1111/mcn.12283
Akombi BJ, Agho KE, Hall JJ, Merom D, Astell-Burt T, Renzaho AMN (2017) Stunting and severe stunting among children under-5 years in Nigeria: a multilevel analysis. BMC Pediatr 17:15. https://doi.org/10.1186/s12887-016-0770-z
Ali MS, Alemu TG, Techane MA et al (2022) Spatial variation and determinants of underweight among children under 5 years of age in Ethiopia: a multilevel and spatial analysis based on data from the 2019 Ethiopian demographic and health survey. Nutrition 102:111743. https://doi.org/10.1016/j.nut.2022.111743
Ali Z, Saaka M, Adams A-G, Kamwininaang SK, Abizari A-R (2017) The effect of maternal and child factors on stunting, wasting and underweight among preschool children in Northern Ghana. BMC Nutr 3:31. https://doi.org/10.1186/s40795-017-0154-2
Amaha ND, Woldeamanuel BT (2021) Maternal factors associated with moderate and severe stunting in Ethiopian children: analysis of some environmental factors based on 2016 demographic health survey. Nutr J 20:18. https://doi.org/10.1186/s12937-021-00677-6
Amegbor PM, Zhang Z, Dalgaard R, Sabel CE (2020) Multilevel and spatial analyses of childhood malnutrition in Uganda: examining individual and contextual factors. Sci Rep 10:20019. https://doi.org/10.1038/s41598-020-76856-y
Amir-Ud-Din R, Fawad S, Naz L, Zafar S, Kumar R, Pongpanich S (2022) Nutritional inequalities among under-five children: a geospatial analysis of hotspots and cold spots in 73 low- and middle-income countries. Int J Equity Health 21:135. https://doi.org/10.1186/s12939-022-01733-1
Assaf S, Juan C (2020) Stunting and anemia in children from urban poor environments in 28 low and middle-income countries: a meta-analysis of demographic and health survey data. Nutrients 12:3539. https://doi.org/10.3390/nu12113539
Astuti FD, Azka A, Rokhmayanti R (2022) Maternal age correlation of stunting in children: systematics review. J Matern Child Health 7:479–448. https://doi.org/10.26911/thejmch.2022.07.04.11
Ayele MA, Fenta HM, Zike DT, Tesfaw LM (2023) Spatial distribution and trends of anemia among pregnant women in Ethiopia: EDHS 2005–2016. Front Public Health. https://doi.org/10.3389/fpubh.2023.1089383
Baker P, Hawkes C, Wingrove K, Demaio AR, Parkhurst J, Thow AM, Walls H (2018) What drives political commitment for nutrition? A review and framework synthesis to inform the United Nations Decade of Action on Nutrition. BMJ Glob Health 3:e000485. https://doi.org/10.1136/bmjgh-2017-000485
Banerjee K, Dwivedi LK (2020) Disparity in childhood stunting in India: Relative importance of community-level nutrition and sanitary practices. PLoS ONE 15:e0238364. https://doi.org/10.1371/journal.pone.0238364
Bloem MW, de Pee S, Le Hop T, Khan NC, Laillou A, Minarto M-P, Soekarjo D, Soekirman SJA, Theary C, Wasantwisut E (2013) Key strategies to further reduce stunting in Southeast Asia: lessons from the ASEAN countries workshop. Food Nutr Bull 34:S8–S16. https://doi.org/10.1177/15648265130342S103
Crookston BT, Dearden KA, Alder SC, Porucznik CA, Stanford JB, Merrill RM, Dickerson TT, Penny ME (2011) Impact of early and concurrent stunting on cognition. Matern Child Nutr 7:397–409. https://doi.org/10.1111/j.1740-8709.2010.00255.x
Defar A, B. Okwaraji Y, Tigabu Z, Persson LÅ, Alemu K, (2023) Spatial distribution of common childhood illnesses, healthcare utilisation and associated factors in Ethiopia: evidence from 2016 Ethiopian demographic and health survey. PLoS ONE 18:e0281606. https://doi.org/10.1371/journal.pone.0281606
Dhingra S, Pingali PL (2021) Effects of short birth spacing on birth-order differences in child stunting: Evidence from India. Proc Nat Acad Sci. https://doi.org/10.1073/pnas.2017834118
Haile D, Azage M, Mola T, Rainey R (2016) Exploring spatial variations and factors associated with childhood stunting in Ethiopia: spatial and multilevel analysis. BMC Pediatr 16:49. https://doi.org/10.1186/s12887-016-0587-9
Jain A, Wang W, James KS, Sarwal R, Kim R, Subramanian SV (2022) Small area variations in dietary diversity among children in India: a multilevel analysis of 6–23-month-old children. Front Nutr. https://doi.org/10.3389/fnut.2021.791509
Jayachandran S, Pande R (2017) Why are Indian children so short? The role of birth order and son preference. Am Econ Rev 107:2600–2629. https://doi.org/10.1257/aer.20151282
Kassie Tesema A, Liyew AM, Alem AZ, Yeshaw Y, Tesema GA, Teshale AB (2021) Spatial distribution and determinants of undernutrition among reproductive age women of Ethiopia: a multilevel analysis. PLoS ONE 16:e0257664. https://doi.org/10.1371/journal.pone.0257664
Mamun S, Mascie-Taylor CGN (2019) Double Burden of malnutrition (DBM) and anaemia under the same roof: a Bangladesh perspective. Med Sci 7:20. https://doi.org/10.3390/medsci7020020
Mberu BU, Haregu TN, Kyobutungi C, Ezeh AC (2016) Health and health-related indicators in slum, rural, and urban communities: a comparative analysis. Glob Health Action 9:33163. https://doi.org/10.3402/gha.v9.33163
Musbah E, Worku A (2016) Influence of maternal education on child stunting in SNNPR, Ethiopia. Central Afr J Public Health 2:71–82. https://doi.org/10.11648/j.cajph.20160202.15
Paul P, Saha R (2022) Is maternal autonomy associated with child nutritional status? Evidence from a cross-sectional study in India. PLoS ONE 17:e0268126. https://doi.org/10.1371/journal.pone.0268126
Pravana NK, Piryani S, Chaurasiya SP, Kawan R, Thapa RK, Shrestha S (2017) Determinants of severe acute malnutrition among children under 5 years of age in Nepal: a community-based case–control study. BMJ Open 7:e017084. https://doi.org/10.1136/bmjopen-2017-017084
Prendergast AJ, Humphrey JH (2014) The stunting syndrome in developing countries. Paediatr Int Child Health 34:250–265. https://doi.org/10.1179/2046905514Y.0000000158
Prusty RK, Bairwa M, Anwar F, Mishra VK, Patel KK, Mangal DK (2022) Socio-biomedical predictors of child nutrition in India: an ecological analysis from a nationally representative demographic and health survey, 2015–2016. J Health Popul Nutr 41:1. https://doi.org/10.1186/s41043-021-00273-8
Quamme SH, Iversen PO (2022) Prevalence of child stunting in Sub-Saharan Africa and its risk factors. Clin Nutr Open Sci 42:49–61. https://doi.org/10.1016/j.nutos.2022.01.009
Seboka BT, Alene TD, Ngusie HS, Hailegebreal S, Yehualashet DE, Gilano G, Ahmed MH, Kabthymer RH, Kanno GG, Tesfa GA (2021) Spatial variations and determinants of acute malnutrition among under-five children in Ethiopia: evidence from 2019 Ethiopian demographic health survey. Ann Glob Health 87:114. https://doi.org/10.5334/aogh.3500
Seboka BT, Hailegebreal S, Yehualashet DE, Kabthymer RH, Negas B, Kanno GG, Tesfa GA, Yasmin F (2022) Methods used in the spatial analysis of diarrhea. Med Case Rep Stud Protoc 3:e0228. https://doi.org/10.1097/MD9.0000000000000228
Swaminathan S, Hemalatha R, Pandey A et al (2019) The burden of child and maternal malnutrition and trends in its indicators in the states of India: the Global Burden of Disease Study 1990–2017. Lancet Child Adolesc Health 3:855–870. https://doi.org/10.1016/S2352-4642(19)30273-1
Thurstans S, Opondo C, Seal A, Wells J, Khara T, Dolan C, Briend A, Myatt M, Garenne M, Sear R, Kerac M (2020) Boys are more likely to be undernourished than girls: a systematic review and meta-analysis of sex differences in undernutrition. BMJ Glob Health 5:e004030. https://doi.org/10.1136/bmjgh-2020-004030
Varghese JS, Stein AD (2019) Malnutrition among women and children in India: limited evidence of clustering of underweight, anemia, overweight, and stunting within individuals and households at both state and district levels. Am J Clin Nutr 109:1207–1215. https://doi.org/10.1093/ajcn/nqy374
Wali N, Agho KE, Renzaho AMN (2020) Factors associated with stunting among children under 5 years in five South Asian countries (2014–2018): analysis of demographic health surveys. Nutrients 12:3875. https://doi.org/10.3390/nu12123875
Wemakor A, Garti H, Azongo T, Garti H, Atosona A (2018) Young maternal age is a risk factor for child undernutrition in Tamale Metropolis. Ghana BMC Res Notes 11:877. https://doi.org/10.1186/s13104-018-3980-7
Yourkavitch J, Burgert-Brucker C, Assaf S, Delgado S (2018) Using geographical analysis to identify child health inequality in sub-Saharan Africa. PLoS ONE 13:e0201870. https://doi.org/10.1371/journal.pone.0201870
Acknowledgements
I am grateful to the Postgraduate School of IARI for their invaluable support and expertise, which guided me throughout my academic journey and helped me complete my research work successfully.
Funding
The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Contributions
Conceptualization was contributed by Alka Singh and Praveen Koovalamkadu Velayudhan; methodology was contributed by Venkata Naga Sindhuja Padigapati, Alka Singh, and Selvaprakash Ramalingam; formal analysis and investigation were contributed by Venkata Naga Sindhuja Padigapati, Alka Singh, and Selvaprakash Ramalingam; writing—original draft preparation, was contributed by Venkata Naga Sindhuja Padigapati; resources were contributed by Praveen Koovalamkadu Velayudhan and Anbukkani Perumal; supervision was contributed by Alka Singh, Praveen Koovalamkadu Velayudhan, and Anbukkani Perumal.
Corresponding author
Ethics declarations
Conflict of interest
The authors hereby state that they do not have any conflicts of interest.
Ethical Approval and Consent to Participate
Since the data used in this study are publicly available and does not contain personal information such as individual names or household addresses, ethics approval was not necessary. For information on DHS data ethical standards, visit the DHS website (https://dhsprogram.com/).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Padigapati, V.N.S., Singh, A., Velayudhan, P.K. et al. Examining the Prevalence and Predictors of Stunting in Indian Children: A Spatial and Multilevel Analysis Approach. Agric Res (2024). https://doi.org/10.1007/s40003-024-00757-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40003-024-00757-z