Abstract
Purpose
Childhood bone and joint infection (BJI) is a potentially severe disease that may have permanent sequelae, including growth impairment and limb deformity. It has been characterised in the literature with a focus on Western epidemiology; there are currently no reports detailing global epidemiology and bacteriology. This omits key data from determining temporal trends, appropriate antibiotic therapy, and resource allocation. This review aims to identify studies that characterise the incidence of childhood bone and joint infection or provide detailed bacteriology within their region.
Methods
A systematic review of the literature was performed from 01/01/1980 to 31/12/2020. Data has been analysed to give incidence of disease per 100,000 children, primary pathogen by country where available, and risk ratio (RR) for disease by ethnicity. This is applicable for areas that experience race-related inequitable burden of disease.
Results
Forty-four articles met the inclusion area; of these, seven were population-wide studies, primarily from Europe or the United States, and the remainder were cohort studies. Incidence could be derived from 26 studies compromising over 34, 000 children. Information on bacteriology was available from 39 publications (10, 957 cases). Methicillin-sensitive Staphylococcus aureus is the most common pathogen in the West. Recently, disease secondary to Kingella kingae and methicillin-resistant S. aureus has increased. Salmonella remains a dominant pathogen in African regions. Increased risk of disease is observed in Aboriginal, New Zealand Māori, Pacific, Indigenous Fijian, and Bedouin children.
Conclusion
The current state of the literature detailing incidence of childhood BJI focuses on disease patterns from the West. There is a paucity of high-quality publications in the developing world. Despite these limitations, global trends in burden of disease show race-related inequitable risk of BJI. Temporal and regional variation in bacteriology can be demonstrated.
Level of evidence: III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Childhood BJI compromises a range of osteoarticular infections including infection and inflammation of bone, infection of the synovial space, and destruction of adjacent tissues. These infections can be potentially life- or limb-threatening, even when recognised and treated appropriately. Timely diagnosis and intervention is therefore vital to minimise associated morbidity [1]. Multiple authors report on the incidence of bone and joint infection (BJI) in children, acknowledging a substantial difference between industrialised countries and the developing world [2, 3]. Comparison between publications is hindered by a heterogenous definition of “childhood infection”: upper age limits vary between 13 and 19 years and some studies report on specifically septic arthritis (SA) or acute haematogenous osteomyelitis (AHO) rather than combined BJI.
It is well recognised that developing and non-Western regions suffer higher rates of childhood BJI [4]. This has previously been attributed to genetic susceptibility, local pathogens, and variation in humidity [5]. There has yet to be a systematic review fully examining patterns of disease outside the West for both SA and AHO [6]. Developing countries face unique challenges in healthcare delivery and lack of resource is linked to sub-optimal health outcomes. Knowledge of these issues is currently limited to retrospective studies or small case series. Progressive data collation is vital to improving health outcomes.
Results from the literature search have been used to identify research regarding patterns in childhood BJI in both Western and non-Western healthcare systems. The goal was to answer the following questions:
-
(1)
What is currently known about the incidence of childhood BJI in Western and non-Western countries?
-
(2)
How does this vary by ethnicity?
-
(3)
What are the primary pathogens in these regions?
-
(4)
What are the rates of surgical management and outcomes for these centres?
Materials and methods
Search strategy and criteria
The review process was conducted according to the preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. A computer-based literature search was used to identify all studies relating to childhood BJI. Search databases used were MEDLINE (Medical Literature Analysis and Retrieval System Online), CINAHL (Cumulative Index to Nursing and Allied Health Literature, Ipswich, Massachusetts), and Cochrane Library up to 31 December 2020 with date restriction to 1980. Google scholar search engine was also used to avoid missing unpublished or recently released contemporary works. The medical subject heading (MeSH) keywords for search were p(a)ediatric, ‘osteomyelitis’, ‘septic arthritis’, ‘antibiotics’, ‘surgery’, ‘bone and joint infection’, and ‘drainage’. To focus the search to include indigenous populations, ‘ethnicity’ and ‘indigenous’ were also included in a subsequent search.
Selection criteria
Two individuals reviewed the articles to determine whether inclusion criteria were satisfied. When disagreement occurred, a third, independent reviewer was contacted to make a final decision. The following criteria were applied for article inclusion to ensure that primarily epidemiological studies were included and that the specific questions for this systematic review could be addressed. First, only original research studies in peer-reviewed journals of the English language (or suitable translation) were allowed, excluding all review articles. The subjects were required to be 19 years of age or younger, and the case series must include a minimum of 20 patients. No papers reporting on chronic/subacute osteomyelitis, reactive arthritis, Tuberculous or Lyme disease, or surgical-site infection were included. Papers reporting only on specific pathogens were excluded (e.g. a publication detailing Salmonella cases in Nigeria [7]) as well as any case series focussed on specific anatomic sites (e.g., a series on calcaneal AHO [8]).
Assessment of study quality
The quality of studies was assessed but did not determine inclusion/exclusion criteria. Given the relative lack of data collection in non-Western regions, strict publication quality exclusion would necessarily create a selection bias against these areas. Knowledge of disease patterns in socioeconomically deprived areas is of vital interest. For this reason, all studies that met inclusion criteria and were above level of evidence V were considered eligible [9].
Assessment of heterogeneity
We assessed studies for homogeneity to allow for meta-analysis. There were discrepancies in age range and some publications primarily considered either AHO or SA. This is laid out in Table 1. Given high levels of heterogeneity across most criteria and general level of evidence, it was deemed more appropriate to create a descriptive review with comparisons of absolute outcomes (such as incidence/100,000).
Data synthesis
One reviewer obtained information from the included studies. After extracting the data, a spreadsheet was used to separate incidence and study characteristics by region (Table 1), bacteriology (Table 2), and risk ratio by ethnicity (Table 3). This is relevant to centres where indigenous and non-indigenous populations live in a single centre yet experience inequitable disease burden.
Data analysis
The frequency of disease for each region was expressed as incidence per 100,000 whenever possible (Table 1). The assessment of bacteriology included the percentage of positive cultures, primary and secondary pathogens, and percentage of MRSA. Long-term outcomes and mortality rates, if available, were analysed for each paper. Long-term outcomes were described as a ‘complication rate’, to cover all orthopaedic sequelae of disease, or identified specifically if possible, such as rates of leg length discrepancy (LLD) and recurrence of infection. Significant risk of bias for each study is due to incomplete outcome data or selective reporting; outcome data or lack thereof have been detailed for each publication in Table 4.
Results
The literature search returned 1693 articles (Fig. 1). Titles and abstracts were checked using inclusion and exclusion criteria and duplicates removed. After abstract screening, 1495 reports were removed. The remaining 143 articles were read and a further 38 analysed from references (176 manuscripts assessed in total). After in-depth analysis of each and applying exclusion criteria, 45 publications were deemed suitable. The most common reason for exclusion was failure to present epidemiological information (n = 92) or focus on a specific pathogen or anatomic location (n = 39).
Study designs and content
All of the included studies had classification of level of evidence via The Journal of Bone & Joint Surgery guidelines; this is presented in Table 1 [9]. Eight publications were nationwide prevalence or incidence studies [10,11,12,13,14,15,16,17]. Incidence data could be extracted from 26 publications. Detailed bacteriology information was available in 39 publications (Table 2). After data were analysed, a risk ratio for specific ethnic background could be calculated from nine studies (Table 3).
Incidence reporting
The combined cohorts allowing incidence reporting summarise more than 35,000 cases of childhood BJI. Twelve papers were found reporting rates of childhood BJI in Europe and the UK [10,11,12,13,14, 18,19,20,21,22,23,24]. Incidence varied between 0.4 and 32.7 cases per 100,000 with significant variation between countries and conflicting reports on temporal incidence.
The earliest study included was Gillespie et al., whose 1985 report examined national hospital discharge data for Scotland, England and Wales, New Zealand and Australia between 1965 and 1980 focussing on acute haematogenous osteomyelitis (AHO) [25]. The highest annual incidence for England was among males aged 10–14; this was 21/100,000.
Publications suggesting a temporal increased incidence of AHO include a report between 1970 and 1987 in Denmark, in which cases rose from 3.3/100,000 to 5.8/100,000. In a similar fashion, Malcius et al. show an increase from 11.5 to 14.3/100,000 in cases of AHO in Lithuania between 1982 and 2003 [20]. In contrast, conflicting pattern emerges over time in Scotland, where Blyth et al. report a decline of 0.185 cases per 100,000 over a 28-year period [19].
Some regions did not report any variation. Population-based studies have provided a useful picture of rates of AHO and SA in France between 2008 and 2013, in which incidence remained unchanged at 22/100,000 [13, 14]. Of the European region, Switzerland appears to have the greatest burden of disease. Several publications report incidence of childhood BJI between 18.3 and 32.7/100,000 over a 20-year period. No temporal decline in incidence was identified [23, 24].
There are three included publications from the US; nationwide studies by Okubo et al. demonstrate the only analysis of BJI where incidence is reported by ethnicity [15, 17, 26]. The authors analyse patients with AHO and SA under 20 years of age in three separate years: 2006, 2009, and 2012. African American children had higher hospitalisation rates in all timeframes. Socioeconomic status was linked to hospitalisation rates which were generally lower than in Europe, ranging from 1.34 to 1.66/100,000.
In 2008, Gafur et al. examined epidemiology of AHO and SA in Texas comparing rates in 1982 to data from 2002 to 2004 [26]. Annualised incidence of AHO increased 2.8 times, whereas SA remained stable. The authors propose that differences in reported rates of BJI may be a result of improved recognition of BJI via the increased use of magnetic resonance imaging (MRI) [27].
In Australasia and the Pacific, rates of infection are far higher [10, 28,29,30,31,32,33]. Some indigenous and ethnic groups are disproportionately affected. Gillespie et al. separate rates of AHO by ethnicity, showing rates up to 196/100,000 in aboriginal Australian children [25]. They perform a similar analysis for New Zealand Māori and Pacific for whom the highest reported rate is 110/100,000. In contrast, NZ European children in the same geographic region have a maximum incidence of 41/100,000.
Later reports found lower annual incidence of disease but a similar ethnic disparity. The difference appears to be greater for AHO rather than SA. Brischetto et al. looked at cases in Australia in 2010–2013 finding incidence of 31/100,000 overall but 90/100,000 in aboriginal children [30]. Within the Pacific region, Munshi et al. looked at rates of OM in Fijian children, finding greater burden of disease among indigenous communities [31].
Publications on patterns of disease in Africa suffer resource constraint whereby annualised incidence rates are rarely available. Only Lavy et al. provide a reflection of SA incidence for children in Malawi, of up to 20/100,000 in 2002 but using an extremely small cohort of 23 cases [5]. There is also a paucity of information for Asia and the Middle East [34,35,36]. Cambodian children appear to have an incidence of BJI up to 13.8/100,000 [34]. In southern Israel, the only publication found to reflect incidence rates is Cohen et al. This paper examines the Bedouin population separately, finding that they experience more AHO than children of other heritage and lifestyle (7.3 vs. 5.6/100,000) [36].
Incidence of disease by ethnicity
Table 3 outlines incidence rates per 100,000/year between different ethnic groups derived from eight papers. Whilst other publications may have reported increased hospital attendance among specific ethnic groups, an incidence calculation for the wider population was rarely performed. Using the figures available, the risk ratio for developing disease by ethnicity has been presented. The greatest disparity in risk appears to be for aboriginal children who are up to 10 times more likely to develop AHO [25]. There is also an increased risk for SA in this population [30].
Of note, a temporal variability in risk for those of African American ethnicity can be observed in the paper by Okubo et al. Between 2006 and 2012, the nationwide incidence of AHO appeared to be rising in the US [17]. Furthermore, relative risk for developing SA among African American children increased from 1.15 to 1.23 [15].
Bacteriology
There were 39 publications meeting criteria that reported on primary and secondary pathogen by region; this gave a total of 10,097 cases. In the UK and Europe, Staphylococcus aureus is overwhelmingly recognised as the primary pathogen, and is usually methicillin-sensitive (MSSA) [11,12,13,14, 18, 19, 21,22,23,24, 37, 38]. It is implicated in between 21 and 81% of cases (Table 2). Secondary pathogens are frequently Streptococcus pneumoniae or Streptococcus pyogenes. As the publications are laid out from earliest to most recent, Kingella kingae is not observed as a primary or secondary pathogen until 2017 in Switzerland [24]. The other trend made visible in this analysis is the disappearance of Haemophilus influenzae type-b. It was responsible for 29% of identified microbiology in Denmark between 1978 and 1987; since then, it has not emerged as a responsible primary or secondary pathogen [39]. Methicillin-resistant S. aureus (MRSA) is noted in nationwide prevalence studies in France to be responsible for 8% of BJI; elsewhere in Europe and the UK, it is either absent or not identified [14].
In the US, MRSA is responsible for up to 43% of childhood BJI [26, 40, 41]. The proportion of disease caused by MRSA has increased since the 1990s from < 10% in some cohort studies [40]. MSSA remains the dominant pathogen in up to 76% of cases [41]. Little is known about the distribution of pathogens across ethnicities, although a cohort study of S. aureus positive AHO in Hawaii found indigenous Hawaiian children were overrepresented [41].
MSSA was the primary pathogen identified in all publications from Australasia and the Pacific [28,29,30,31,32,33, 42, 43]. Secondary pathogens were usually streptococcal in nature. Compared to the US, there are far fewer infections reported secondary to MRSA. In all but one publication, MRSA was either absent or in less than 10% of positive cultures [33, 42]. The exception to this finding is a review of BJI in Australia from 2010 to 2013 by Brischetto et al., in primarily indigenous children from Northern Australia MRSA was confirmed in 40% of samples and relapse rates were relatively high (15%) [30].
African studies have identified more atypical pathogens [5, 44,45,46,47,48,49]. In two cohorts from Malawi, Salmonella was the primary cultured organism [5, 7, 44]. Secondary organisms were frequently gram negative, such as Escherichia coli [48, 50]. MRSA was identified in 1% of isolates in a cohort from Tanzania; aside from this, there were no reported cases of MRSA-associated childhood BJI [47].
MRSA was found to cause a higher proportion of BJI in papers from Japan (29%) and Thailand (17.5%) [51, 52]. Staphylococcal species remained the most common pathogens across studies in Asia and South America [34, 51,52,53,54,55,56]. Only two publications from the Middle East focussed on childhood AHO [36, 57]. Interestingly, the pathogenicity was found to change before and after the Gulf conflict in a comparative study by Mousa et al. The cohort from 1983 to 1989 had primarily cases of S. aureus and H. influenzae; a subsequent group of children analysed between 1992 and 1997 had a reduced rates of S. aureus and emergence of Klebsiella sp. The authors propose that this difference was caused by poverty, working children, and malnutrition [57].
Management and outcomes
Surgical management is more frequent in papers including cases of SA (Table 4). Operative rates in Europe and the US range from 16 to 66% [18], 58. Efforts have been made to identify which cases of BJI are likely to require multiple surgeries and have a stormier clinical course; Gafur et al. provided a link between pathogen and clinical picture, suggesting operative rates are higher in patients with MRSA, delayed presentation and diffuse disease [26]. In regions where Panton–Valentine Leukocidin (PVL) is identified by molecular typing, this virulence factor is associated with worse disease and higher operative rate [28].
Reported surgical management can be much higher outside the US and Europe. Operative rates in Australasia are between 34 and 84% [42]. The highest operative rate identified was in a cohort from Australia, 52 children with SA of which many were indigenous Aboriginal [43].
In the African region, high intervention rates (75–80%) were required for cohorts of both SA and AHO; in some publications, this was attributed to delayed access to healthcare and worse presentation of disease [47].
Only 25 publications considering global epidemiology comment on relapse and/or long-term sequelae. Across Western regions, the mortality rates for childhood BJI remain lower than 1% [26, 41]. Primary concerns are relapse of infection, chronic disease, and permanent limb deformity. In Europe and the UK, the highest reported rate of relapse following treatment is 4% [18]. Limb shortening is reported at 1.6% [58].
Contrasting this, US relapse rates are higher, up to 6% for all cases and 13% for MRSA-associated BJI in Hawaii [40, 41].
Detailed information about sequelae in paediatric hip and knee infection is available in Hoswell et al.’s 20-year review of outcomes in Australia [43]. The authors looked at Oxford hip and Oxford knee scores in 52 children who had treatment for SA, finding that up to 42% had mild to moderate impairment in limb function.
Generally worse outcomes are experienced by children in developing countries. Mortalities in reports from Africa are as high as 15% for cases of BJI with Salmonella [5]. Limb deformity and permanent growth arrest were found in 14.5% of cases of AHO in Namibia [45]. In Cambodian children with BJI studied between 2007 and 2011, 46% experienced disease complications and relapse rates were 25% [34].
Frustratingly, many of the complications and growth issues that stem from childhood BJI are unlikely to be identified in these regions. Loss to follow-up is generally not reported. In publications that track cases beyond initial hospital stay, 4–60% of children are not brought to planned outpatient appointments [59].
Discussion
The purpose of this review was to describe the global incidence and bacteriology of childhood BJI, with consideration of the different disease patterns between regions and ethnic groups. This is currently the most extensive examination of data with inclusion of non-Western regions. We found higher rates of disease in Australasia, Africa, and parts of Asia with the highest overall incidence among Australian aboriginal children. Although methicillin-sensitive S. aureus is the most common pathogen, attention is drawn to the emergence of K. kingae and MRSA. K. kingae emerged as a significant pathogen in 2017; polymerase chain reaction (PCR) testing was not widely available prior to this and still remains inaccessible for some centres. Molecular typing has also allowed identification of Panton–Valentine Leukocidin (PVL), a virulence factor associated with more severe illness. Disappearance of Haemophilus influenzae type-b is likely due to the introduction of widespread vaccination for developed regions. Salmonella remains an important pathogen in African regions and this is possibly in association with sickle cell disease.
Development of BJI appears to be strongly influenced by socioeconomic, pathogen, and host factors. Early publications by Lavy et al. considering the development of septic arthritis in Africa hypothesised the increased incidence of disease was related to malnutrition, salmonella bacteraemia, and trauma [5]. Salmonella bacteraemia is highly prevalent in sub-Saharan Africa in conjunction with anaemia and malaria [5]. A theory of traumatic septic arthritis development was supported by Molyneux et al., who suggested children under 12 months were predominantly swaddled sustaining minor trauma being swung onto the mother’s back [44].
Stoesser et al. reviewed childhood BJI in Cambodia 2007–2011 and attributed high incidence of disease to childhood malnutrition, poverty, and poor vaccine coverage given that 6% of children had H. influenzae identified [34].
Despite research acknowledging excessive burden of disease in non-Western regions, rigorous statistical analysis for cause is rarely available. A population study in South Korea from Kim et al. found a higher incidence of BJI compared to Western countries. The authors provided a useful multivariate analysis looking for epidemiologic factors associated with surgical need; they report that rural residence, female gender, and older age were all associated with increased hospitalisation [35].
Repeated studies confirm an extremely high risk of disease within Australian Aboriginal, New Zealand Māori, and Pacific ethnicities. Reasons for this are not fully understood. Despite residing in generally well-resourced regions, these communities experience poorer health outcomes driven by inequitable access to healthcare and economic disparity. Socioeconomic factors in New Zealand were explored by Hunter and Baker looking specifically at deprivation index and distance from tertiary care [32]. A higher deprivation index was associated with development of septic arthritis, and the majority of NZ Māori and Pacific patients were in the most deprived deciles. Some of these patients also experience more skin and soft tissue infection (SSTI) [60]. Brischetto et al.’s cohort study from northern Australia highlighted the endemic nature of impetigo among Australian indigenous children (up to 70%) [30]. This paper suggests haematogenous seeding from skin sores as pathogenesis of disease. Although genetic predisposition to infection has been hypothesised as a reason for worse disease burden, there is to date no analysis showing a relationship between genetic makeup and development of BJI for indigenous communities.
It is unclear whether higher disease prevalence is associated with pathogen type. Regions with greater prevalence of childhood BJI, such as Australian and New Zealand indigenous communities, have S. aureus as the primary pathogen [30, 32]. In contrast, MRSA causes significant disease in parts of the US but is almost absent from cases of BJI in New Zealand [17, 32]. Regions with severe disease in the South Pacific also see high rates of the S. aureus PVL virulence factor [28, 61]. Further investigation into regional S. aureus virulence factors may shed light on the disparate burden of disease experienced by these communities.
Weaknesses of this systematic review include study heterogeneity and limited outcome reporting. Limitations for outcome reporting in developing countries reduced the quality of publications. This reflects socioeconomic barriers to data collection and patient follow-up. Prohibitive cost reduces healthcare delivery for many of these centres, such as the lack of modern culture techniques and PCR preventing identification of pathogens. Rigorous exclusion of these publications creates selection bias where only disease patterns from the West are routinely analysed.
Conclusion
Literature detailing incidence of childhood BJI is disproportionately focussed on Western disease patterns. There is a paucity of high-quality publications in the developing world. Despite these limitations, global trends in burden of disease show race-related inequitable risk of BJI. The temporal and regional variation in bacteriology can be demonstrated. K. kingae and MRSA are of increasing importance across multiple studies.
References
Iliadis AD, Ramachandran M. Paediatric bone and joint infection. EFORT Open Rev. 2017. https://doi.org/10.1302/2058-5241.2.160027.
Gigante A, Coppa V, Marinelli M, Giampaolini N, Falcioni D, Specchia N. Acute osteomyelitis and septic arthritis in children: a systematic review of systematic reviews. Eur Rev Med Pharmacol Sci. 2019;23:145–58. https://doi.org/10.26355/eurrev_201904_17484.
Kang SN, Sanghera T, Mangwani J, Paterson JMH, Ramachandran M. The management of septic arthritis in children: systematic review of the English language literature. J Bone Jt Surg Ser B. 2009;91:1127–33. https://doi.org/10.1302/0301-620X.91B9.22530.
Dartnell J, Ramachandran M, Katchburian M. Haematogenous acute and subacute paediatric osteomyelitis: a systematic review of the literature. J Bone Joint Surg Br. 2012;94B:584–95. https://doi.org/10.1302/0301-620X.94B5.28523.
Lavy CBD. The clinical features and surgical treatment of acute septic arthritis in Malawian children. PQDT Glob. 2006. https://doi.org/10.1542/peds.2005-0566.
Tanwar YS, Jaiswal A, Singh S, Arya RK, Lal H. Acute pediatric septic arthritis: a systematic review of literature and current controversies. Polish Orthop Traumatol. 2014;79:23–9.
Graham SM, Molyneux EM, Walsh AL, Cheesbrough JS, Molyneux ME, Hart CA. Nontyphoidal Salmonella infections of children in tropical Africa. Pediatr Infect Dis J. 2000;19:1189–96. https://doi.org/10.1097/00006454-200012000-00016.
Pääkkönen M, Kallio MJT, Peltola H, Kallio PE. Antibiotic treatment and surgery for acute hematogenous calcaneal osteomyelitis of childhood. J Foot Ankle Surg. 2015. https://doi.org/10.1053/j.jfas.2015.01.006.
Marx RG, Wilson SM, Swiontkowski MF. Updating the assignment of levels of evidence. J Bone Jt Surg - Am. 2015;97:1–3. https://doi.org/10.2106/JBJS.N.01112.
Gillespie WJ. The epidemiology of acute haematogenous osteomyelitis of childhood. Int J Epidemiol. 1985;14:600–6. https://doi.org/10.1093/ije/14.4.600.
Dahl LB, Høyland A-L, Dramsdahl H, Kaaresen PI. Acute Osteomyelitis in Children: A Population-based Retrospective Study 1965 to 1994. Scand J Infect Dis. 1998;30:573–7. https://doi.org/10.1080/00365549850161124.
Riise ØR, Kirkhus E, Handeland KS, Flatø B, Reiseter T, Cvancarova M, et al. Childhood osteomyelitis-incidence and differentiation from other acute onset musculoskeletal features in a population-based study. BMC Pediatr. 2008;8:45. https://doi.org/10.1186/1471-2431-8-45.
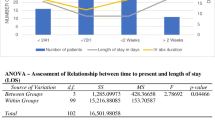
Laurent E, Petit L, Maakaroun-Vermesse Z, Bernard L, Odent T, Grammatico-Guillon L. National epidemiological study reveals longer paediatric bone and joint infection stays for infants and in general hospitals. Acta Paediatr. 2018;107:1270–5. https://doi.org/10.1111/apa.13909.
Grammatico-Guillon L, Maakaroun Vermesse Z, Baron S, Gettner S, Rusch E, Bernard L. Paediatric bone and joint infections are more common in boys and toddlers: a national epidemiology study. Acta Paediatr. 2013;102:e120–5. https://doi.org/10.1111/apa.12115.
Okubo Y, Nochioka K, Marcia T. Nationwide survey of pediatric septic arthritis in the United States. J Orthop. 2017. https://doi.org/10.1016/j.jor.2017.06.004.
Kim J, Lee MU, Kim T-H. Nationwide epidemiologic study for pediatric osteomyelitis and septic arthritis in South Korea. Medicine (Baltimore). 2019;98: e15355. https://doi.org/10.1097/MD.0000000000015355.
Okubo Y, Nochioka K, Testa M. Nationwide survey of pediatric acute osteomyelitis in the USA. J Pediatr Orthop B. 2017. https://doi.org/10.1097/BPB.0000000000000441.
Christiansen P, Frederiksen B, Glazowski J, Scavenius M, Knudsen FU. Epidemiologic, bacteriologic, and long-term follow-up data of children with acute hematogenous osteomyelitis and septic arthritis: a ten-year review. J Pediatr Orthop B. 1999. https://doi.org/10.1097/01202412-199910000-00014.
Blyth MJG, Kincaid R, Craigen MAC, Bennet GC. The changing epidemiology of acute and subacute haematogenous osteomyelitis in children. J Bone Jt Surg Ser B. 2001;83:99–102. https://doi.org/10.1302/0301-620X.83B1.10699.
Malcius D, Trumpulyte G, Barauskas V, Kilda A. Two decades of acute hematogenous osteomyelitis in children: are there any changes? Pediatr Surg Int. 2005;21:356–9. https://doi.org/10.1007/s00383-005-1432-7.
Shivarathre D, George H, Kaimal N, James L. Epidemiology of acute haematogenous osteomyelitis in children—a single unit’s experience over three different time-periods. Acta Orthop Belg. 2009;75(1):81–6.
Mitha A, Boutry N, Nectoux E, Petyt C, Lagrée M, Happiette L, et al. Community-acquired bone and joint infections in children: a 1-year prospective epidemiological study. Arch Dis Child. 2015. https://doi.org/10.1136/archdischild-2013-305860.
Juchler C, Spyropoulou V, Wagner N, Merlini L, Dhouib A, Manzano S, et al. The contemporary bacteriologic epidemiology of osteoarticular infections in children in Switzerland. J Pediatr. 2018. https://doi.org/10.1016/j.jpeds.2017.11.025.
Samara E, Spyropoulou V, Tabard-Fougère A, Merlini L, Valaikaite R, Dhouib A, et al. Kingella kingae and osteoarticular infections. Pediatrics. 2019;144: e20191509. https://doi.org/10.1542/peds.2019-1509.
Gillespie WJ, Mayo KM. The managment of acute haematogenous osteomyelitis in the antibiotic era. A study of the outcome. J Bone Jt Surg Ser B. 1981;63B:126–31. https://doi.org/10.1302/0301-620x.63b1.7009619.
Gafur OA, Copley LAB, Hollmig ST, Browne RH, Thornton LA, Crawford SE. The impact of the current epidemiology of pediatric musculoskeletal infection on evaluation and treatment guidelines. J Pediatr Orthop. 2008;28:777–85. https://doi.org/10.1097/BPO.0b013e318186eb4b.
Lee YJ, Sadigh S, Mankad K, Kapse N, Rajeswaran G. The imaging of osteomyelitis. Quant Imaging Med Surg. 2016;6:184–98. https://doi.org/10.21037/qims.2016.04.01.
Labbé JL, Peres O, Leclair O, Goulon R, Scemama P, Jourdel F, et al. Acute osteomyelitis in children: the pathogenesis revisited? Orthop Traumatol Surg Res. 2010;96:268–75. https://doi.org/10.1016/j.otsr.2009.12.012.
Street M, Puna R, Huang M, Crawford H. Pediatric acute hematogenous osteomyelitis. J Pediatr Orthop. 2015;35:634. https://doi.org/10.1097/BPO.0000000000000332.
Brischetto A, Leung G, Marshall CS, Bowen AC. A Retrospective case-series of children with bone and joint infection from northern Australia. Medicine (USA). 2016;95: e2885. https://doi.org/10.1097/MD.0000000000002885.
Munshi B, MacFater W, Hill AG, McCaig EH. Paediatric osteomyelitis in Fiji. World J Surg. 2018. https://doi.org/10.1007/s00268-018-4743-2.
Hunter S, Baker JF. Ten-year retrospective review of paediatric septic arthritis in a New Zealand centre. Int Orthop. 2021. https://doi.org/10.1007/s00264-020-04611-z.
Rossaak M, Pitto RP. Osteomyelitis in Polynesian children. Int Orthop. 2005. https://doi.org/10.1007/s00264-004-0597-3.
Stoesser N, Pocock J, Moore CE, Soeng S, Hor PC, Sar P, et al. The epidemiology of pediatric bone and joint infections in cambodia, 2007–11. J Trop Pediatr. 2013. https://doi.org/10.1093/tropej/fms044.
Kim J, Lee MU, Kim TH. Nationwide epidemiologic study for pediatric osteomyelitis and septic arthritis in South Korea: A cross-sectional study of national health insurance review and assessment service. Medicine (Baltimore). 2019;98: e15355. https://doi.org/10.1097/MD.0000000000015355.
Cohen E, Lifshitz K, Fruchtman Y, Eidelman M, Leibovitz E. Current data on acute haematogenous osteomyelitis in children in Southern Israel: epidemiology, microbiology, clinics and therapeutic consequences. Int Orthop. 2016. https://doi.org/10.1007/s00264-016-3211-6.
Rasmont Q, Yombi JC, Van Der Linden D, Docquier PL. Osteoarticular infections in Belgian children: A survey of clinical, biological, radiological and microbiological data. Acta Orthop Belg. 2008;74:374–85.
Chiappini E, Krzysztofiak A, Bozzola E, Gabiano C, Esposito S, Lo Vecchio A, et al. Risk factors associated with complications/sequelae of acute and subacute haematogenous osteomyelitis: an Italian multicenter study. Expert Rev Anti Infect Ther. 2018;16:351–8. https://doi.org/10.1080/14787210.2018.1453357.
Refakis CA, Arkader A, Baldwin KD, Spiegel DA, Sankar WN. Predicting periarticular infection in children with septic arthritis of the hip: regionally derived criteria may not apply to all populations. J Pediatr Orthop. 2019;39:268–74. https://doi.org/10.1097/BPO.0000000000000934.
Saavedra-Lozano J, Mejías A, Ahmad N, Peromingo E, Ardura MI, Guillen S, et al. Changing trends in acute osteomyelitis in children: Impact of methicillin-resistant Staphylococcus aureus infections. J Pediatr Orthop. 2008;28:569–75. https://doi.org/10.1097/BPO.0b013e31817bb816.
Erdem G, Salazar R, Kimata C, Simasathien T, Len KA, Bergert L, et al. Staphylococcus aureus osteomyelitis in Hawaii. Clin Pediatr (Phila). 2010. https://doi.org/10.1177/0009922809352805.
Goergens ED, McEvoy A, Watson M, Barrett IR. Acute osteomyelitis and septic arthritis in children. J Paediatr Child Health. 2005;41:59–62. https://doi.org/10.1111/j.1440-1754.2005.00538.x.
Hoswell RL, Johns BP, Loewenthal MR, Dewar DC. Outcomes of paediatric septic arthritis of the hip and knee at 1–20 years in an Australian urban centre. ANZ J Surg. 2019. https://doi.org/10.1111/ans.15139.
Molyneux E, French G. Salmonella joint infection in Malawian children. J Infect. 1982;4:131–8. https://doi.org/10.1016/S0163-4453(82)93701-X.
Lauschke EHM, Frey CT. Hematogenous osteomyelitis in infants and children in the Northwestern region of Namibia. Management and two-year results. J Bone Jt Surg A. 1994;76:502–10. https://doi.org/10.2106/00004623-199404000-00004.
Visser H. Paediatric septic arthritis in tertiary setting. 2010;92. Available from http://www.scielo.org.za/pdf/saoj/v9n2/v9n2a14.pdf
Ali AM, Maya E, Lakhoo K. Challenges in managing paediatric osteomyelitis in the developing world: analysis of cases presenting to a tertiary referral centre in Tanzania. African J Paediatr Surg. 2014. https://doi.org/10.4103/0189-6725.143136.
Mue D, Salihu M, Awonusi F, Yongu W, Kortor J, Elachi I. The epidemiology and outcome of acute septic arthritis: a hospital based study. J West African Coll Surg. 2013;36:40–52.
Emeagui NK, Obu GO, Opara HIO, Emeagui OD, Ajaegbu OC, Esievoadje SE, et al. Paediatric osteomyelitis in a tertiary hospital in South-South Nigeria clinical experience at federal medical centre Asaba. J Adv Med Med Res. 2020;32:57–64. https://doi.org/10.9734/jammr/2020/v32i2130694.
Omoke N, Obasi A. Childhood pyogenic septic arthritis as seen in a teaching hospital South East Nigeria. Niger J Surg. 2017;23:26. https://doi.org/10.4103/1117-6806.199968.
Sukswai P, Kovitvanitcha D, Thumkunanon V, Chotpitayasunondh T, Sangtawesin V, Jeerathanyasakun Y. Acute hematogenous osteomyelitis and septic arthritis in children: clinical characteristics and outcomes study. J Med Assoc Thai. 2011;94:S209–16.
Yamagishi Y, Togawa M, Shiomi M. Septic arthritis and acute hematogenous osteomyelitis in childhood at a tertiary hospital in Japan. Pediatr Int. 2009;51:371–6. https://doi.org/10.1111/j.1442-200X.2008.02740.x.
Kini AR, Shetty V, Kumar AM, Shetty SM, Shetty A. Community-associated, methicillin-susceptible, and methicillin-resistant Staphylococcus aureus bone and joint infections in children: experience from India. J Pediatr Orthop B. 2013;22:158–66. https://doi.org/10.1097/BPB.0b013e32835c530a.
Yadav S, Dhillon MS, Aggrawal S, Tripathy SK. Microorganisms and their sensitivity pattern in septic arthritis of north Indian children: a prospective study from tertiary care level hospital. ISRN Orthop. 2013. https://doi.org/10.1155/2013/583013.
Chou ACC, Mahadev A. Acute bacterial osteomyelitis in children. J Orthop Surg. 2016;24:250–2. https://doi.org/10.1177/1602400225.
Motwani G, Mehta R, Aroojis A, Vaidya S. Current trends of microorganisms and their sensitivity pattern in paediatric septic arthritis: a prospective study from tertiary care level hospital. J Clin Orthop Trauma. 2017;8:89–92. https://doi.org/10.1016/j.jcot.2016.09.001.
Mousa HAL, Abaid MG. Acute haematogenous osteomyelitis: Microbial conversion and unusual age presentation. East Mediterr Heal J. 2000;6:89–92.
Chiappini E, Camposampiero C, Lazzeri S, Indolfi G, De Martino M, Galli L. Epidemiology and management of acute haematogenous osteomyelitis in a tertiary paediatric center. Int J Environ Res Public Health. 2017;14:477. https://doi.org/10.3390/ijerph14050477.
Osei L, El Houmami N, Minodier P, Sika A, Basset T, Seligmann H, et al. Paediatric bone and joint infections in French Guiana: a 6 year retrospective review. J Trop Pediatr. 2017;63:380–8. https://doi.org/10.1093/tropej/fmw102.
Williamson DA, Ritchie SR, Roberts SA, Coombs GW, Thomas MG, Hannaford O, et al. Clinical and molecular epidemiology of community-onset invasive Staphylococcus aureus infection in New Zealand children. Epidemiol Infect. 2014;142:1713–21.
Bocchini CE, Hulten KG, Mason EO, Gonzalez BE, Hammerman WA, Kaplan SL. Panton-Valentine leukocidin genes are associated with enhanced inflammatory response and local disease in acute hematogenous Staphylococcus aureus osteomyelitis in children. Pediatrics. 2006. https://doi.org/10.1542/peds.2005-0566.
Funding
The authors did not receive support from any organization for the submitted work. No funding was received to assist with the preparation of this manuscript. No funding was received for conducting this study. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no potential conflicts of interest identified in the creation of this systematic review.
Rights and permissions
About this article
Cite this article
Hunter, S., Chan, H. & Baker, J.F. Global epidemiology of childhood bone and joint infection: a systematic review. Infection 50, 329–341 (2022). https://doi.org/10.1007/s15010-021-01741-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-021-01741-3