Abstract
Purpose
In this multicentre, retrospective, matched cohort study we aimed to evaluate the outcomes of neutropenic fever cases that were treated with daptomycin or a glycopeptide (vancomycin or teicoplanin).
Methods
Data and outcomes of adult (aged > 18-years old) patients with neutropenic fever [(1) without clinical and radiological evidence of pneumonia, (2) who were treated with daptomycin or a glycopeptide (teicoplanin or vancomycin) for any reason and for at least 72 h] were extracted from the hospital databases. Matching was performed with all of the three following criteria: (1) underlying disease, (2) reason for starting daptomycin or glycopeptide (microbiologic evidence vs. microbiologic evidence, clinical infection vs. clinical infection and empirical therapy vs. empirical therapy) and (3) neutropenic status.
Results
Overall 128 patients [(69/123) (56.1%) in the daptomycin cohort (D) and 59/123 (48%) in the glycopeptide cohort (G)] had a resolution of fever at the end of 72 h antibiotic treatment (p = 0.25). There was no significant difference in cured, improved and (cured + improved) rates between (D) and (G) cohorts as well as fever of unknown origin cases or microbiologically confirmed infections or clinically defined infections subgroups (p > 0.05). There was also no significant difference (p > 0.05), in terms of persistent response in the (D) versus (G) cohorts,
Conclusions
These findings suggest that although not better, daptomycin efficacy is comparable to vancomycin if used as empiric therapy in the treatment of adult febrile neutropenia. We conclude that daptomycin may be used at least as a salvage therapy alternative to glycopeptides in the treatment of adult febrile neutropenia cases. A large, randomized-controlled trial may further consolidate the evidence related to this question.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In spite of developments in medical care and antimicrobial therapy, neutropenic fever is still associated with significant morbidity and mortality if not treated quickly and appropriately [1,2,3,4,5,6,7,8]. Empirical treatment with anti-pseudomonal betalactams is the mainstay of clinical management [2]. However, anti-pseudomonal beta-lactam may be used in combination with a glycopeptide (vancomycin or teicoplanin) or linezolid in established indications (e.g. hemodynamic instability, suspected catheter-related infection, pneumonia, skin and soft tissue infection or unresponsive persistent fever) [1, 3]. Despite the use of broad-spectrum anti-pseudomonal (meropenem, piperacillin/tazobactam, etc.), anti-staphylococcal antibacterial agents (vancomycin or teicoplanin) or antifungals, fever may still persist and febrile neutropenia episodes may still result in mortality [5,6,7,8].
Daptomycin is highly effective against gram-positive multidrug-resistant bacteria such as methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant enterococci (VRE) [9, 10]. In 2003, daptomycin was granted FDA-approval for the treatment of complicated skin and soft tissue infections caused by gram-positive organisms, including vancomycin-susceptible Enterococcus faecalis. In 2006, daptomycin received approval for S. aureus bacteraemia and right-sided infective endocarditis. It was also approved by the European regulatory agency for the same clinical indications in 2006 [11]. Despite these indications and lack of data in neutropenic patients, daptomycin is used in off-label indications such as meningitis, osteomyelitis and febrile neutropenia [7, 8, 12,13,14]. However, the published research regarding daptomycin for the treatment of febrile neutropenia is quite limited [7, 8, 14]. The purpose of this multicentre, retrospective, matched cohort study was to compare the outcomes of patients who received daptomycin or a glycopeptide (vancomycin or teicoplanin) as part of a combination regimen for the management of febrile neutropenia.
Methods
This study gathered data from 14 centres from ten cities (Izmir, Trabzon, Malatya, Ankara, Adana, Antalya, Mersin, Denizli, Istanbul, Eskisehir) located in six geographic regions of Turkey.
Patients
Neutropenic fever was defined as an absolute neutrophil count < 500 mm3 or a count < 1000 mm3 but expected to fall to < 500 mm3 within 48 h and a single measurement of temperature > 38.3 or 38.0 °C on two or more occasions within 12 h. Risk evaluation was made according to the criteria of the Multinational Association for Supportive Care in Cancer (MASCC) and patients with ≥ 21 risk index were considered to be low-risk cases [5, 6].
Patients were included if they were (1) > 18-years old, (2) had neutropenic fever fulfilling above criteria, (3) did not have pneumonia (excluded by clinical and radiological findings), and (4) were started on daptomycin or a glycopeptide (teicoplanin or vancomycin) for any reason and received it for at least 72 h between 1st January 2010 until 31st May 2016. Relevant data were analysed retrospectively by chart review and hospital databases.
Matching criteria
Matching was performed with all of the three following criteria: (1) underlying disease (solid organ malignancy vs. solid organ malignancy etc.), (2) reason for starting daptomycin or a glycopeptide (microbiologic evidence vs. microbiologic evidence, clinical infection vs. clinical infection and empirical therapy vs. empirical therapy) and (3) neutropenic status [severe neutropenia (< 100 neutrophils/mm3) vs. severe neutropenia].
Clinical and laboratory evaluation
Standard follow-up of neutropenic fever in the study centres was as follows. Before the start of antibiotic therapy, a complete medical history and physical examination were performed. Complete blood cell and differential counts, routine biochemistry, at least two sets of blood cultures (from two different peripheral veins and all lumens of the central venous catheter) and a chest X-ray were obtained before starting antibiotic treatment. In case of suspected pneumonia or urinary tract infection, urine and sputum cultures were performed. Cultures of other sites of infection were performed as clinically indicated. Microbiological sampling was repeated during therapy if fever persisted to isolate the causative pathogen and to document the eradication of the isolated pathogen. In case of persistent fever, chest X-ray and computerized tomography or abdominal ultrasonography were obtained. Complete blood cell counts, coagulation, biochemistry parameters and urine analysis were performed at least once a week [3, 5, 6].
Bacteriological isolates were identified by standard techniques. Antimicrobial susceptibility testing of the isolates was performed with the VITEK 2 system (bio Merieux, La Balme-les-Grottes, France) in nine centers and BD Phoenix (BD Diagnostic Systems, Sparks, MD) in two centres. Results were interpreted according to the CLSI criteria [15]. Vancomycin or teicoplanin or daptomycin Etest (bio Merieux, La Balme-les-Grottes, France) was used when automated system resulted as “non susceptible”.
Classification of febrile episodes
Microbiologically documented infection (MDI) was defined as the isolation of microorganisms from any clinical sample including blood, urine, or sputum. Coagulase-negative staphylococcal bacteraemia was defined as two positive and identical (in terms of species identification and antibiotic susceptibility tests) results of two independent blood cultures. Clinically documented infection (CDI) was considered when there was a focus of infection on physical examination without microbiological documentation. Fever of unknown origin (FUO) was considered when there was no clinical or microbiological evidence of infection in a febrile episode [5, 6].
Antibiotic regimens
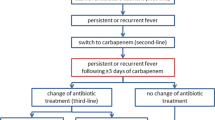
Patients who received daptomycin received it as 6–8 mg/kg q24h and vancomycin as 500 mg q6h and teicoplanin as 400 mg q12h. Each antimicrobial agent was infused intravenously over 60 min. Concomitant gram-negative agents’ dosages were as follows: meropenem 1 gr q8h, imipenem 500 mg q6h, piperacillin/tazobactam 4.5 gr q6h, cefepime and cefoperazone/sulbactam 2 gr q8h. Treatment was switched to oral amoxicillin/clavunalate 875/125 mg q 12h + ciprofloxacin 500 mg q 12 h, in patients with apyrexia (body temperature < 38 °C) continued for > 72 h and whose neutropenia resolved.
Evaluation of response definitions
Cure was defined as a persistent response in clinical signs (including fever and symptoms); no indication of additional antibiotic therapy and/or negative culture reported at the end of the therapy [7].
Improved Partial resolution of clinical signs and symptoms and/or additional antibiotic therapy warranted at the end of therapy [7].
Failure Inadequate response to therapy evident by worsening or new/recurrent signs and symptoms, fever still persisting after 72–96 h prompting modification of the initial therapy, need for a change in antibiotic therapy or a positive culture reported at the end of therapy or mortality due to any reason [7].
Non-evaluable Unable to determine response due to insufficient information [7].
The term end of treatment clinical success was used to describe patients with an outcome of cure or improved [7]. Infection-related mortality referred to death resulting from a documented or presumed infection during the neutropenic episode and daptomycin or glycopeptide treatment. Microbiological success was defined as clearance of the infecting bacteria on the test of cure cultures. All-cause mortality referred to death resulting from a documented or presumed infection or a defined or unidentified reason during the treatment and a 30-day follow-up period. Secondary efficacy outcome was defined as the maintenance of success (without any relapse and mortality) through 1 month following completion of daptomycin or glycopeptide including therapy.
Ethical approval
The local Institutional Review Board approved the study.
Statistical analysis
The objective of this study was to compare the clinical success rates of the daptomycin and glycopeptide cohorts. All analyses were performed using SPSS version 18.0 (Chicago, IL, USA). The significance of the difference between groups was evaluated by χ2 test and t test as indicated. The significance level was accepted as p < 0.05.
Results
Characteristics of the study population
A total of 246 patients, 123 patients each in the daptomycin (D) and glycopeptide groups (G), fulfilled the criteria to be included in the study. If one patient had more than one episode, data of the first episode was included in the study. Table 1 shows the clinical characteristics of patients in the two treatment cohorts. Overall, 4.9% (12/246) of the patients had solid tumours and 95.1% (234/246) had hematologic malignancies in both cohorts (Table 1, p > 0.05). Age, gender, comorbidities, hypotensive state, being on a vasopressor agent, severe neutropenia, central venous catheter, low-risk neutropenic fever (MASCC risk index was ≥ 21), ICU hospitalization, mechanical ventilation and administration of levofloxacin prophylaxis were similar in both treatment groups (Table 1).
Type of infection and distribution of microorganisms
Approximately 41% (101/246) of the febrile neutropenia episodes were considered to be FUO whereas 29.2% (72/246) were CDI and 29.6% (73/246) were MDI episodes (Table 2). There was no statistically significant difference between (D) and (G) cohorts in terms of infection types (p > 0.05). During the neutropenic fever episodes, causative microorganisms were isolated from 73 cases; 69 from blood, two from urine and two soft tissue biopsy cultures. The most common isolates were coagulase-negative staphylococci (n = 45), S. aureus (n = 14) and E. faecalis (n = 7) (Table 2). When blood culture results were evaluated, there were 11 methicillin-resistant S. aureus and 35 methicillin-resistant S. epidermidis. There was no significant difference in terms of etiologic agents between (D) and (G) cohorts (Table 2, p > 0.05).
Treatment
In the (D) cohort, 92 cases received daptomycin including regimens as primary treatment (mostly due to lack of glycopeptides in the hospital pharmacies-this lack was not due to unavailability of the drugs in Turkey but due to payment problems of the hospital pharmacies/administrations). A total of 31 cases had received other antibacterial therapy (27 a glycopeptide, three linezolid and one both a glycopeptide and linezolid, for 8 ± 7.2 days, all switched to daptomycin due to clinical failure) before receiving regimens including daptomycin. All patients received the glycopeptides as primary treatment in the (G) cohort.
In (D) cohort, daptomycin dosage was 6–8 mg/kg in all cases. 43 cases received daptomycin due to MDI (all susceptible to daptomycin, susceptibility result of five cases in (D) cohort needed confirmation by Etest), whereas the remaining cases received it for empirical treatment of fever or fever + hypotension or septic shock (defined as febrile neutropenia + hypotension + being on vasopressor) or CDI (Tables 1, 2).
In the (G) cohort, 800 mg of teicoplanin was given as an initial dose, followed by a maintenance dose of 400 mg twice a day whereas vancomycin was given at a dose of 1000 mg twice a day. In 30 cases, glycopeptides were given due to MDI (all susceptible to glycopeptide - susceptibility result of five cases (G) cohort needed confirmation by Etest), while in the remaining cases it was started empirically for the treatment of fever or fever + hypotension or fever + septic shock or CDI (Tables 1, 2).
No additional therapy was used after daptomycin in 90 patients, whereas 33 patients received further oral therapy (further/additional oral cotrimoxazole, tetracyclines, levofloxacin, etc.). No additional therapy was used after glycopeptides in 83 patients, while 40 patients received further oral therapy (p > 0.05).
Clinical response and following antibiotic modification
Overall 128 (69/123, 56% in D and 59/123, 48% in G cohorts, p = 0.25) had resolution of fever at the end of 72 h treatment. In terms of overall clinical response, there was no significant difference in cured, improved, cured + improved rates between (D) and (G) cohorts (Table 3). Furthermore, no significant difference was observed in low risk, high risk, hypotensive, cases in ICU, empirically started cases, CDI, MDI subgroups (Supplemantal file-Table 1). Mean duration of treatment was 12.4 ± 5.5 days in the (D) group and 10.8 ± 4.7 days in the (G) group (p > 0.05). When we evaluated the persistent response in the FUO cases as a separated group in (D) vs. (G) cohorts, there was also no significant difference (28/44, 63.6% in D group vs. 28/57, 49.1% in G group, p = 0.16). Overall end of treatment cure rates were also similar in the empirical therapy (28/44, 63.6% vs. 28/57, 49.1%, p = 0.16) and CDI (23/36, 63.8% vs. 21/36, 58.3%, p = 0.80) and MDI cases (33/43, 76.7% vs. 23/30, 76.7%, p = 1) in (D) vs. (G) cohorts. The need for antibacterial and/or antifungal treatment modification was similar in both treatment groups (Table 4).
Overall 95 cases (52/123, 42.3% in D and 43/123, 35% in G cohorts, p = 0.58) that had a resolution of fever after 72 h of treatment had a successful outcome without any modification and achieved a 30-day post-treatment survival.
Mortality
All-cause mortality during the treatment and 30-day follow-up period were not different between (D) and (G) cohorts (17/123, 13.8% and 21/123, 17.1% vs. 17/123, 13.8% and 20/123, 16.3%, respectively, p > 0.05). In the septic shock subgroup, 15 of 23 cases (8/18, 44.4% vs. 7/8, 87.5%, p = 0.08) died due to septic shock. Overall mortality rates were similar in males (D: 13/74 vs. G: 14/80, p = 1) vs. females (D: 8/49 vs. G: 6/43, p = 0.78), cases with severe neutropenia vs. others (D: 15/65 vs. G: 10/62, p = 0.37) and in cases receiving levofloxacin prophylaxis vs. others (D: 2/10 vs. G: 4/14, p = 1).
Adverse effects
There was no severe adverse effect requiring antibiotic cessation in (D) cohort whereas glycopeptides were stopped due to nephrotoxicity (n = 2) and rash (n = 2) in four cases (p = 0.12). In (D) cohort, there were phlebitis (n = 1), myalgia (n = 1) and mild rash (n = 1) that did not require a change in therapy. There was one episode of diarrhoea in (G) cohort, which did not require antibiotic cessation.
Discussion
Vancomycin and teicoplanin have been the two glycopeptides, used as the principal antibacterial agents for the treatment of gram-positive multidrug-resistant bacterial infections including MRSA and MRCNS since the 1960s and 1980s [16,17,18,19,20,21,22,23,24]. Both agents were evaluated for the initial empirical treatment of fever, treatment of persistent fever and known MRSA and MRCNS infections in the neutropenic host [3, 17, 22]. Most recent IDSA and the Infectious Diseases Working Party of the German Society of Haematology and Medical Oncology guidelines suggest glycopeptides in restricted indications [3, 22]. Accordingly, vancomycin (or other agents active against aerobic gram-positive cocci) is not recommended as a standard part of the initial antibiotic regimen for fever and neutropenia (A–I). These agents should be considered for specific clinical indications, including suspected catheter-related infection, skin or soft-tissue infection, radiologically confirmed pneumonia, colonization with MDR gram-positive bacteria such as MRSA and VRE or sepsis with hemodynamic instability [3].
44 cases in (D) cohort and 57 in (G) cohort, patients received daptomycin or glycopeptides for empirical therapy (fever or fever + hypotension/septic shock) of febrile neutropenia episode. However, fever alone [26 in (D) cohort and 50 in (g) cohort] is not a guideline recommended indication [1, 3, 22]. These cases were mostly in five study settings, which had a dominance of gram-positive bacterial infection in the aetiology and had added Gram-positive oriented antibiotics to the empirical therapy regimens on the third day of persisting fever.
Daptomycin, tigecycline and linezolid are the major alternative agents available in Turkey for the management of MDR gram-positive bacteria. Although there are clinical studies related to linezolid in neutropenic host, it has the disadvantages of being both bacteriostatic and haematologically toxic [20, 25]. Tigecycline has the advantage of covering susceptible Acinetobacter spp. infections (very common in Turkey) concomitant with the disadvantage of being bacteriostatic and being ineffective against Pseudomonas [25]. In clinical practice, daptomycin is an important alternative antibacterial agent for the treatment of MDR gram-positive bacterial infections especially those caused by S. aureus with glycopeptide MIC > 1 mg/l and vancomycin-resistant enterococci [17]. Data regarding daptomycin in the neutropenic host are scarce. Bubalo et al. [14] evaluated daptomycin in 30 febrile neutropenia cases with persistent fever after 72 h of initial antibacterial therapy. Clinically, 87% of patients improved on daptomycin in combination with gram-negative coverage, and 73% achieved a successful outcome. Rolston et al. [7] analysed the efficacy of daptomycin in neutropenic patients with documented gram-positive infections in a retrospective observational registry study [The Cubicin® Outcome Registry and Experience (CORE®)]. They reported an overall 85% clinical success (definition was similar to our study) in 186 cases. Keil et al. [24] analysed the neutropenic subgroup from the European registry study database (< 1000 cells/mm3; n = 446 cases). The overall clinical success rate (cured + improved) associated with daptomycin was 77.1%. The success rate in uncomplicated skin and soft tissue infections was 73.1% (n = 19). The clinical success rates by infecting pathogen were relatively high for coagulase negative staphylococci (85.6%; n = 95) and S. aureus (77.1%; n = 39). In the presented study, overall cured + improved rates were 20/21 (95%), 3/5 (60%) and 19/19 (100%) in skin and soft tissue infection, MRSA bacteraemia and MRCNS bacteraemia subgroups (main guideline recommended indications [1, 3, 22]), respectively. When compared with results of Keil et al, our success rates for skin and soft tissue infections were a little higher. MRCNS or MRSA bacteraemia results were not clear in both studies [17, 24]. However, our cured + improved rate (76.7%) in any kind of MDI was compatible with the results of Rolston et al. [7] (ranging between 81% for VRE and 94% for CNS) and Keil et al. (ranging between 71.4% for enterococci and 85.6% for CNS) [24]. Furthermore, similar to these previously published outcomes (73–85%) [7, 14, 24], our overall cured + improved rate was 86.2% in the (D) cohort.
The mean duration of daptomycin treatment in the presented study (12.4 ± 5.5 days) was similar to previous studies (ranging between 8 and 14 days) [7, 8, 24]. In the previously reported studies, severe adverse events related to daptomycin were reported to range between 1.6 and 6% [7, 8, 24]. Similar to these studies, 3.3% cases had severe adverse effects requiring drug cessation in (D) cohort in the presented study.
In the (D) cohort, 92 cases received daptomycin including regimens as primary treatment. The reason for primary treatment may be a temporary and intermittent lack of glycopeptides in hospital pharmacies due to hospital budget problems during the study period. In Turkey, > 95% of the population’s health care services is reimbursed by the Turkish Republic Social Security Institution, which is funded by the government. However, the Turkish government has not made any increase in the payment for healthcare services to the hospitals since 2009. Thus, hospitals are under pressure of the need to balance their increasingly restricted budgets, and this, commonly leads to intermittent shortage of several drugs (due to economical or payment problems of hospital administrations) including antibiotics such as glycopeptides [26, 27].
Our study has several limitations. Although it was a multicentre study, this was a retrospective matched cohort study. Despite the fact that baseline characteristics of the (D) and (G) cohorts were similar, this was not a randomized-controlled study. Hence, although we tried to overcome selection bias by matching by three criteria, we still cannot exclude a selection bias. Although recommended in guidelines [22], therapeutic drug monitoring was not performed in any of the cases. Since this was a retrospective cohort study, there was not an opportunity to measure time to culture negativity. In addition, we could not analyse infection-related mortality; instead, we used 1-month survival as all-cause mortality data. In any combination therapy case, positive response was not only due to daptomycin or glycopeptides but also other antibiotics used concomitantly. However, this would be a disadvantage of any study evaluating glycopeptides or daptomycin in febrile neutropenia. Daptomycin was used in combination with other drugs and often as salvage therapy. Hence, the real comparison between daptomycin and glycopeptides in 1st line treatment could not be performed. Daptomycin or glycopeptide dosages were not adjusted according to patient weight. For this reason, it could not be possible to compare the results of 6 mg/kg vs. 8 mg/kg or any other dosage in (D) cohort. Some of the cases received glycopeptides or daptomycin in not guideline recommended indications [1, 3, 22]. Despite these disadvantages, to our knowledge, these are the largest cohorts comparing daptomycin with glycopeptides in adult febrile neutropenia.
These findings suggest that although not better, daptomycin efficacy is comparable to vancomycin. We conclude that daptomycin may be used at least as a salvage therapy alternative to glycopeptides in the treatment of adult febrile neutropenia cases. A large, randomized-controlled trial may further consolidate the findings of the present study.
References
Febrile Neutropenia Study Group. Guidelines for diagnosis and treatment of neutropenic patients. Flora. 2004;9:5–28.
Alp S, Akova M. Management of febrile neutropenia in the era of bacterial resistance. Ther Adv Infect Dis. 2013;1:37–43.
Freifeld AG, Bow EJ, Sepkowitz KA, et al. Infectious Diseases Society of America. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2011;52:427–31.
Ozden M, Denk A, Demirdag K, et al. Investigation of febrile neutropenic cases and risk factors. Mediterr J Infect Microb Antimicrob. 2013;2:3.
Oztoprak N, Piskin N, Aydemir H, et al. Piperacillin-tazobactam versus carbapenem therapy with and without amikacin as empirical treatment of febrile neutropenia in cancer patients: results of an open randomized trial at a university hospital. Jpn J Clin Oncol. 2010;40:761–7.
Sipahi OR, Arda B, Nazli-Zeka A, et al. Piperacillin/tazobactam vs. cefoperazone/sulbactam in adult low-risk febrile neutropenia cases. Int J Clin Pract. 2014;68:230–5.
Rolston KV, Besece D, Lamp KC, et al. Daptomycin use in neutropenic patients with documented gram-positive infections. Support Care Cancer. 2014;22:7–14.
Chaftari AM, Hachem R, Mulanovich V, et al. Efficacy and safety of daptomycin in the treatment of Gram-positive catheter-related bloodstream infections in cancer patients. Int J Antimicrob Agents. 2010;36:182–6.
Aktaş G, Derbentli S. In vitro activity of daptomycin against VRE and MRSA strains. Mikrobiyol Bul. 2014;48:123–8.
Fowler VG Jr, Boucher HW, Corey GR, et al. Daptomycin versus standard therapy for bacteremia and endocarditis caused by Staphylococcus aureus. N Engl J Med. 2006;355:653–65.
Tran TT, Munita JM, Arias CA. Mechanisms of drug resistance: daptomycin resistance. Ann N Y Acad Sci. 2015 Sep;1354:32–53.
Sipahi OR, Bardak-Ozcem S, Turhan T, et al. Vancomycin versus linezolid in the treatment of methicillin- resistant Staphylococcus aureus meningitis. Surg Infect (Larchmt). 2013;14:357–62.
Candevir-Ulu A, Kurtaran B, İnal AS, et al. Daptomycin experience between years 2009–2013: review of 139 cases. Mediterr J Infect Microb Antimicrob. 2014;3:23.
Bubalo JS, Kullar R, Maziarz RT. A pilot study of the efficacy and safety of empiric daptomycin therapy in oncology patients with fever and severe neutropenia. Ther Adv Infect Dis. 2013;1:183–90.
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing: twenty-third informational supplement M100-S23. Wayne: CLSI; 2013.
Molina KC, Huang V. Resistance to non-glycopeptide agents in serious Staphylococcus aureus infections. Curr Infect Dis Rep. 2016;18:47.
Vardakas KZ, Mavros MN, Roussos N, et al. Meta-analysis of randomized controlled trials of vancomycin for the treatment of patients with gram-positive infections: focus on the study design. Mayo Clin Proc. 2012;87:349–63.
Moise PA, Sakoulas G, Forrest A, et al. Vancomycin in vitro bactericidal activity and its relationship to efficacy in clearance of methicillin-resistant Staphylococcus aureus bacteremia. Antimicrob Agents Chemother. 2007;51:2582–6.
Gould IM. Treatment of bacteraemia: meticillin-resistant Staphylococcus aureus (MRSA) to vancomycin-resistant S. aureus (VRSA). Int J Antimicrob Agents. 2013;42:17–21.
Jaksic B, Martinelli G, Perez-Oteyza J, et al. Efficacy and safety of linezolid compared with vancomycin in a randomized, double-blind study of febrile neutropenic patients with cancer. Clin Infect Dis. 2006;42:597–607.
Murray KP, Zhao JJ, Davis SL, et al. Early use of daptomycin versus vancomycin for methicillin-resistant Staphylococcus aureus bacteremia with vancomycin minimum inhibitory concentration> 1 mg/L: a matched cohort study. Clin Infect Dis. 2013;56:1562–9.
Heinz WJ, Buchheidt D, Christopeit M, et al. Diagnosis and empirical treatment of fever of unknown origin (FUO) in adult neutropenic patients: guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Medical Oncology (DGHO). Ann Hematol. 2017;96:1775–92.
Chong PP, van Duin D, Bangdiwala A, et al. Vancomycin-resistant enterococcal bloodstream infections in hematopoietic stem cell transplant recipients and patients with hematologic malignancies: impact of daptomycin MICs of 3 to 4 mg/L. Clin Ther. 2016;38:2468–76.
Keil F, Daikos GL, Skoutelis A, Dominguez JI, Pathan R, Hamed K. Daptomycin for gram-positive infections in patients with neutropenia: clinical experience from a european outcomes registry. Adv Ther. 2015;32:715–26. https://doi.org/10.1007/s12325-015-0231-3.
Sipahi OR. Economics of antibiotic resistance. Expert Rev Anti Infect Ther. 2008;6:523–39.
Üniversite hastaneleri borç batağında. University hospitals are in debt swamp. https://www.cnnturk.com/ekonomi/universite-hastaneleri-borc-bataginda. Accessed 21st October 2018.
Bülüç F, Ozkan O, Agirbas İ. Evaluation of financial performance of university hospitals by ratio analysis method. Bus Manag Stud Int J. 2017;5:268-281.
Acknowledgements
Authors thank ESCMID Study Group for Infections in Compromised Hosts (Esgich). This research did not receive any specific grant from any party. Authors also thank Anthony Patterson, PhD (Assistant Professor in English Language and Literature in Celal Bayar University) and Emine Sevim Kocakız (English Teacher) for English proofreading.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
ORS, SU, BA, HP and MT received speaker’s honorarium from MSD.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sipahi, O.R., Kahraman, H., Erdem, H.A. et al. Daptomycin vs. glycopeptides in the treatment of febrile neutropenia: results of the Izmir matched cohort study. Infection 47, 259–266 (2019). https://doi.org/10.1007/s15010-018-1256-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-018-1256-8