Abstract
Background
Introduced in 2013–2014, the second- and third-wave directly acting antivirals (DAAs) have strongly enhanced the efficacy and tolerability of anti-HCV treatment, with a sustained virological response (SVR) in 90–95% of cases treated. The aim of this paper was to focus on the type and prevalence of viral strains with a reduced sensitivity to DAAs and on treatment choices for DAA-experienced patients.
Methods
The Medline was searched for “HCV infection”, “HCV treatment”, “Directly acting antivirals”,“HCV resistance”.
Results
Most patients who did not achieve an SVR have been found to be infected with HCV mutant strains with a reduced susceptibility to these drugs. These mutants occur frequently in the NS5A region, with a moderate frequency in the NS3/4A regions and rarely in the NS5B region. Treatment-induced mutants resistant to NS5A DAAs persist for years after treatment discontinuation, whereas those resistant to the NS3 DAAs have a shorter duration.
Conclusions
Patients who have failed HCV treatment with DAA agents have several re-treatment options, but re-treatment selection may be intricate and resistance testing is recommended to optimize this choice. It is, therefore, important to bear in mind that the correct determination of HCV genotype and subtype and the identification of RASs are essential elements for choosing the optimal re-treatment. It is supposed that it is useful to give readers some other suggestions regarding therapeutic reprocessing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatitis C virus (HCV) causes a symptomless acute hepatitis that progresses to chronicity in nearly 70% of cases. HCV-related chronic hepatitis is characterized by a long-term persistence of liver necro-inflammation and fibrosis, leading to liver cirrhosis in nearly 20% of the cases in 20 years; furthermore, HCV-cirrhotic patients develop hepatocellular carcinoma (HCC) with a 3–4% yearly rate [1, 2]. Several factors may speed this progression, such as old age at the time of infection, a concomitant metabolic disorder, an impaired host immune response, alcohol abuse and coinfection with HBV or HIV [2,3,4].
Up to 3% of the world’s population live with HCV infection [5, 6], with more than 300,000 deaths and 3–4 million new cases per year [5,6,7]. A high prevalence (> 3.5%) of subjects with the antibody to HCV (anti-HCV) have been reported in some countries in Eastern Asia, Africa and Middle East regions [8], whereas lower values have been observed in Western countries, from 1.8% in the USA to 0.6% in Germany.
Currently, intravenous drug use, exposure to medical procedures (e.g., surgery, dialysis, dental treatment) and unsafe sex (e.g., sex with multiple partners, anal sex, sex with trauma, sex in the presence of genital lesions) are factors associated with a high risk of acquiring HCV infection [9,10,11,12,13]. Vertical transmission to newborn babies accounts only for 5% of the cases (from 5.8 to 10.8% if mothers are coinfected with HIV) [14]. Needlestick injury occurs frequently in health care workers, but its epidemiologic role is limited [15].
HCV virology
HCV is a positive sense, single-stranded RNA virus of the Flaviviridae family, with a genome of 9.6 kb containing a single open reading frame (ORF) flanked by 5-and 3-untranslated regions [16].
The ORF codes for a single polyprotein of approximately 3000 residues, cleaved into four structural proteins (core, E1, E2 and P7) and seven non-structural (NS) genes by cellular and viral proteases. Three NS genes, targeted by the directly acting antivirals (DAA) in clinical practice, play an essential role for viral replication [17]: NS3, NS5A and NS5B.
The NS3 is dedicated to the cleavage at the NS2/NS3 site, which occurs rapidly by a conformation-dependent autocatalytic mechanism [18]. The NS5A is a membrane-associated phosphoprotein of unknown structure and function, found in a basally phosphorylated form of 56 kDa and in a hyper phosphorylated form of 58 kDa. The function of NS5A in the HCV replication cycle is unknown, but adaptive mutations cluster in the central region of NS5A in the replicon system [19], suggesting its involvement in viral replication, either directly and/or by interaction with cellular proteins and pathways. This, together with the modulation of NS5A hyper-phosphorylation by the nonstructural proteins 3, 4A, and 4B [20] supports the view that NS5A is an essential component of the HCV replication complex [21]. NS5B is an RNA-dependent RNA polymerase, structurally organized in a characteristic “right hand motif” containing palm and thumb domains. The error-prone nature of the HCV NS5B polymerase and the accumulation of mutations in a small hyper-variable region in the envelope-encoding genes generate a high level of variability. This variability translates into the existence of seven major HCV genotypes (with 30–35% variation at the nucleotide level), 67 subtypes (with less than 15% difference at the nucleotide level) each composed of a myriad of viral quasi-species, and nine recombinant forms (e.g., the most frequently reported genotype 2 k/1b, which has multiple isolates) [22]. Each genotype exhibits a different degree of variability: 7 subtypes in genotype 1, 11 in genotype 2, 6 in genotype 3, 17 in genotype 4, 24 in genotype 6 and only 1 in genotypes 5 and 7 [23]. There are several consequences related to this enormous viral heterogeneity, such as the possibility of re-infections with a different viral strain because of the limited cross-antigenicity, the emergence of immune-escape mutants accounting for the high rate of patients who progress to chronicity, the genotype- and subtype-specific response to treatments and the spontaneous or drug-induced selection of viral-resistant strains.
Treatment of chronic HCV infection
For more than a decade and until 2013, the combination of pegylated interferon-alpha (peg-IFN) and ribavirin (RBV) was the treatment of choice for HCV infection. This combination therapy provided a sustained clearance of circulating HCV (sustained viral response—SVR) in half of the patients infected with HCV genotype 1, in about 70% of those with genotype 2 and in about 60% of those with HCV genotype 3. Besides an insufficient response rate, this combination therapy was poorly tolerated and produced serious adverse reactions [24,25,26,27,28,29,30].
Treatment of HCV infection has been revolutionized by the recent availability of the well-tolerated, potent directly acting antivirals (DAAs), which, used in combination, allow excellent chances for an HCV clearance, prevention of disease progression and reduction of both liver-related and overall mortality [31,32,33,34]. Several IFN-free DAA regimens allow up to 95% HCV clearance after a 12-week treatment [34, 35] in DAA-naïve patients: different treatment schedules have been recommended, depending on the HCV genotype and subtype and on the presence or absence of cirrhosis (Table 1).
Around 5% of patients fail to eradicate HCV infection, mostly due to the presence of cirrhosis, HCV genotype 3 or resistance-associated substitutions (RASs). The high error rate of the HCV polymerase and the fast virion production result in a mixture of naïve viral genetic populations, termed quasi-species, existing even before treatment. In an Italian study, a pre-treatment presence of NS5A RASs was detected in 14 (23.0%) of 61 patients with HCV genotype 1b and in 3 (4.9%) of the 61 with HCV genotype 1a; the pangenotypic RAS Y93H was detected in 1 (1.6%) patient with genotype 1a and in 4 (6.6%) with genotype 1b [36].
RAS distribution in the three HCV regions targeted by DAAs
The detection of RASs may be made by population sequencing or next-generation sequencing (NGS). Population sequencing can detect only variants representing > 15–20% of the quasi-species, NGS can reach those with a 0.1–1% prevalence. Although NGS has a better sensitivity, it is noted that a 15% cutoff for minor variant frequency better predicts DAA-treatment failure and that drug-specific RASs identified at a lower frequency do not reduce SVR rates with currently available DAA regimens [37,38,39,40,41].
The emergence of RASs, the main cause of failure to DAA therapy, depends on the HCV genotype and the DAA used (Tables 2, 3, 4).
NS3/4A protease inhibitors and corresponding RASs (Table 2)
The first-generation PIs boceprevir and telaprevir act only against HCV genotype 1, have a low genetic barrier to resistance and considerable cross-resistances involving amino acids at positions V36, T54, R155 and A156. Instead, the second- and third-generation PIs (simeprevir, asunaprevir, paritaprevir, grazoprevir, vaniprevir, glecaprevir, danoprevir, voxilaprevir, sovaprevir and vedroprevir) have a higher genetic barrier and an enhanced antiviral activity against the different HCV genotypes (GT) [42].
Among patients with HCV GT 1, the NS3/4A mutations are detected more frequently in those with GT 1a than in those with GT 1b [43].
Boceprevir is used to treat patients with GT 1 HCV infection. The resistance mutations most frequently selected by boceprevir are V36M, T54S and R155K in GT1a-infected patients and T54A/S, V55A, A156S and V170A in those infected with GT1b [44].
Telaprevir is used to treat GT1 HCV infection; the most frequent resistance mutations selected by this drug are V36M and R155K in GT1a-infected patients and V36A, T54A and A156S in the GT1b-infected [45].
Simeprevir (SIM), a drug approved to treat HCV GT1 infection, most frequently selects R155K and D168E/V resistance mutations in GT1a-infected patients and Q80R and D168E/V in the GT1b-infected. The presence of the Q80K polymorphism substantially reduces the rate of SVR in GT 1a patients with cirrhosis, an effect not observed in those without cirrhosis; in patients with Q80K at baseline who did not achieve an SVR, an additional resistance-associated substitution (mainly R155K) may be selected during treatment failure [46].
Asunaprevir is used to treat GT1 and GT4 HCV infections. The most frequent resistance mutations selected by asunaprevir are R155K and D168E in GT1a-infected patients and D168E/V/Y in GT1b-infected patients [47, 48].
Paritaprevir, a drug approved to treat GT1 and GT4 HCV infection, may select D168A/V/Y in GT1a-infected patients, Y56H and D168V in the GT1-infected and D168V in the GT4-infected [49].
Grazoprevir is used to treat HCV GT1 infection; the most frequent resistance mutations selected by this drug are Q80K and D168A in GT1a-infected patients and T54S and V170I in the GT1b-infected [50].
Vaniprevir has been developed to treat GT1 HCV infection. The most frequent resistance mutations selected by this drug are R155K and D168T/V/Y in GT1a-infected patients and D168H/T/V in the GT1b-infected [51, 52].
Glecaprevir has a pangenotypic activity; the most frequent resistance mutations selected are V36M and D168A in GT1a-infected patients and Y56H and D/Q168K/R in the GT1b-infected [53, 54].
Voxilaprevir (VOX) has a wide pangenotypic activity. The most frequent resistance mutations selected by this drug are R155W and A156T/V in GT1a-infected patients, A156V in the GT1b-infected and R155G in the GT3-infected [55].
NS5A inhibitors and corresponding RASs (Table 3)
The NS5A inhibitors are characterized by a broad genotypic coverage and by a relatively low barrier to resistance. The NS5A mutations may be detected as natural baseline polymorphisms, and in this case the degree of resistance may have clinical relevance, as occurs for Y93H.
Daclatasvir has a pangenotypic activity and may select M28T, Q30E/H/R, L31M, H58D in GT1a-infected patients, L31M/V and Y93H in the GT1b-infected, M28I, Q30K and Y93H in those with GT3 infection and Q30H/S in those with GT4 infection [56,57,58].
Ledipasvir (LDV) is an NS5A inhibitor used to treat GT1 HCV infection. The most frequent resistance mutations selected by ledipasvir are Q30E/R, L31M and Y93C/H/N in the GT1a-infected and Y93H in the GT1b-infected [59, 60].
Ombitasvir has a pangenotypic activity and most frequently selects M28T and Q30R resistance mutations in GT1a-infected patients, Y93H in GT1b-infected and L28V in the GT4-infected [61].
Elbasvir is an NS5A inhibitor with pangenotypic activity that most frequently selects the resistance mutations M28T, Q30R, L31V and Y93H in GT1a-infected patients, L31V and Y93H in GT1b-infected patients and A30K, L31F and Y93H in those with GT3 infection [62].
Velpatasvir (VEL) is an NS5A inhibitor with pangenotypic activity. The most frequent resistance mutations selected by this drug are M28T, Q30R/H, L31M/V and Y93H/C/N in GT1a-infected patients, Q30R, L31M/V and Y93H/C/N in the GT1b-infected, L31I/M/V and Y93H in patients with GT2 infection and E92K and Y93H in the GT3-infected [63, 64].
Pibrentasvir is an NS5A inhibitor with pangenotypic activity. The most frequent resistance mutations selected by this drug are M/L/F28G, Q30R, L31M and Y93H in GT1a-infected patients and K24F, M/L/F28K, Q30K, L31F/I and Y93H in the GT3-infected [49, 65].
NS5B inhibitors and corresponding RASs (Table 4)
Given their different mechanisms and sites of interaction, no cross-resistance exists across nucleotide and non-nucleoside polymerase inhibitors.
Sofosbuvir (SOF) is a nucleoside NS5B polymerase inhibitor with pangenotypic activity whose most frequent resistance mutations are L159F and C316N in GT1a-infected patients, S282G/T and C316N/H/F in the GT1b-infected, L159F and S282T in those with GT2 infection, L159F and V321A in the GT3-infected and E237G, S282T and V321A in those with GT4 infection [69,70,71].
Dasabuvir has been developed to treat HCV GT1 infection; the most frequent resistance mutations selected by this drug are M414T and S556G in GT1a-infected patients and S556G in the GT1b-infected [72].
Therapeutic options for patients who failed a DAA regimen
Despite the excellent efficacy shown by the licensed DAA-based regimens, virological failures occur in around 5–10% of patients treated, mostly associated with RASs selected by the drugs used [73,74,75,76,77,78,79,80]. An example of this is shown by the data from an Italian study where 139 (3.6%) patients out of the 3,830 DAA-treated for advanced fibrosis (F3) or cirrhosis did not achieve an SVR. The failure rate was 7.6% for patients treated with a suboptimal, i.e., no longer recommended (sofosbuvir + ribavirin or simeprevir + sofosbuvir ± ribavirin) and 1.4% for those treated with a combination of sofosbuvir/daclatasvir, sofosbuvir/ledipasvir or other effective DAA treatments. Of these 139, 72 patients were re-treated with a second DAA regimen (38 with sofosbuvir + daclatasvir, 27 with sofosbuvir + ledipasvir, and 7 with other DAAs ± ribavirin), with an SVR12 in 96% of cases [81].
As regards RASs and the therapeutic options for re-treatment, it is useful to remember that the NS5A inhibitors have a low barrier to resistance and that the variants they select frequently confer cross-resistance across the drug class [87, 88], persist longer than those selected by NS3 and NS5B inhibitors [89,90,96,92,93] and represent a challenge for DAA-based therapy [50, 83,84,85].
The HCV resistance test may identify the clinically relevant RASs, but current guidelines do not offer a clear indication to their use. In fact, the American Association for the Study of the Liver recommends a resistance test for RASs only for patients who failed a DAA regimen including an NS5A inhibitor and, in positive cases, to test also for NS3 RASs, whereas a panel of Italian experts proposed resistance testing for all three genes (NS3, NS5A and NS5B) [86]. In our view, the analysis of the presence of RASs in all three HCV regions is needed to choose the best re-treatment option in patients with DAA failure. In truth, only fragmentary data come from limited clinical trials and real-life studies and currently re-treatment approaches should be based on expert opinions. We must also point out that the AASLD recommends deferring re-treatment unless it is an urgent priority.
Hezode et al. described 16 patients who had failed an NS5A-based treatment with daclatasvir plus pegylated interferon (Peg-IFN) and ribavirin (RBV), with or without asunaprevir; all 16 patients were re-treated with SOF plus SIM for 12 weeks and an SVR12 was achieved by 14 of them [87].
Feld et al. in the ASTRAL 1 TRIAL evaluated treatment-naive or treatment-experienced patients infected with HCV genotype 1, 2, 4, 5, or 6 treated with SOF/velpatasvir for 12 weeks. In this study, all 48 participants with a previous failure to a protease inhibitor plus peginterferon/ribavirin achieved an SVR12 [64]; similar results were obtained for 27 patients in a prior phase 2 open-label trial [88].
Afdhal et al. evaluated the safety and efficacy of the combination LDV/SOV in genotype 1-infected patients who had failed a prior treatment with an HCV protease inhibitor (telaprevir or boceprevir) plus peginterferon/ribavirin; a 94 and 98% SVR12 rate was obtained, respectively, with a 12- or 24-week LDV/SOF regimen. The presence of cirrhosis and/or a baseline NS5A RAS were the major reasons for relapse in the 12-week re-treatment arm [60].
Reddy et al. [89] performed a post hoc integrated safety and efficacy analysis of the LDV/SOF combination on seven trials with 240 cirrhotic patients, naïve or experienced for a combination regimen including a first-generation PI. Overall, a 96% SVR12 rate was observed; this rate was significantly lower (90%) in patients re-treated for 12 weeks, suggesting that the extension of treatment to 24 weeks or the addition of RBV might have been beneficial in this subset of patients; in the same study, the addition of ribavirin significantly improved the rate of SVR in patients with a baseline NS5A resistance re-treated with LDV/SOF for 12 (from 88 to 94%) or 24 weeks (from 85 to 100%).
The POLARIS-4 trial evaluated the efficacy of the combination SOF/VEL/VOX in re-treating GT1-4 patients who had failed a prior non-NS5A DAA regimen; patients exposed only to an NS3/4A inhibitor were not included. Among patients with a prior DAA failure, 69% had been exposed to SOF plus RBV with or without peg-IFN and 11% to SOF plus SMV. Patients re-treated with SOF/VEL/VOX for 12 weeks showed a higher SVR12 rate (98%) than those in the SOF/VEL arm (90%) [90].
The placebo-control phase 3 POLARIS-1 trial evaluated the efficacy of a 12-week course of SOF/VEL/VOX combination in patients with HCV GT 1–6 infection who had failed a previous DAA regimen containing an NS5A inhibitor. The SVR rate was 96% in patients infected with genotype 1a, 100% in those infected with genotype 1b, 100% with genotype 2, 95% with genotype 3, 91% with genotype 4 and 100% with HCV genotype 6; the only patient infected with HCV genotype 5 achieved an SVR. Overall, the SVR rate was 93% in patients with cirrhosis and 99% in those without.
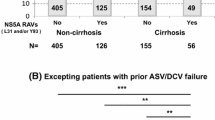
The MAGELLAN-1 Part 2 randomized, open-label, phase 3 study evaluated the efficacy and safety of the combination glecaprevir/pibrentasvir (G/P) in patients with chronic HCV infection who experienced a virological failure to an NS3/4A protease- and/or an NS5A inhibitor-containing therapy. Patients with compensated liver disease, with or without cirrhosis, and HCV genotype 1, 4, 5, or 6 were 1:1 randomized to receive 12 or 16 weeks G/P treatment. An SVR was achieved by 89% (39 of 44) and 91% (43 of 47) of patients who, respectively, received 12 or 16 weeks G/P treatment; a virological relapse occurred in 9% (4 of 44) of patients treated for 12 weeks and in none of those treated for 16 weeks [101,102,103].
A study from de Lédinghen reported an SVR12 in 25 of 26 patients with HCV genotype 1 or 4 re-treated with SOF/grazoprevir/elbasvir + ribavirin for 16 or 24 weeks after they had developed a RAS at a prior failure to an NS5A- or NS3-inhibitor-based regimen [94].
Conclusions
Most patients who have failed an HCV treatment with DAA agents have several re-treatment options, but re-treatment selection may be intricate and resistance testing is recommended to optimize this choice. Before resistance testing is performed, it is useful to make sure that the classification of HCV genotype and subtype has been made with a reliably sensitive test; in case of doubt, the repetition of the test is indicated. In fact, Di Maio et al. reported that HCV genotype had been misclassified in 6 (3.0%) of 197 patients who failed DAA treatment [95]. Similarly, Starace et al. [79] found HCV genotype misclassification in 13 (14.9%) of 87 patients who had failed a DAA regimen. It is therefore important to bear in mind that the correct determination of HCV genotype and subtype and the identification of RASs are essential elements for choosing the optimal re-treatment.
We think it is useful to give readers some other suggestions regarding therapeutic reprocessing (Figs. 1, 2, 3, 4):
-
in patients with HCV genotype 1a, the RASs in position 93, 30 and 31 have a high fold-change in resistance compared to the wild-type replicon for all NS5A inhibitors. In the absence of these RASs we can use sofosbuvir + velpatasvir + ribavirin, or pibrentasvir + glecaprevir or an unconventional combination (paritaprevir–ritonavir/ombitasvir/dasabuvir + sofosbuvir or elbasvir + grazoprevir + sofosbuvir), while, in the presence of these RASs, re-treatment with sofosbuvir + velpatasvir + voxilaprevir is the only available option (Fig. 1);
-
in patients with HCV genotype 1b or 2, sofosbuvir + velpatasvir + ribavirin is the best re-treatment DAA option regardless of the presence or absence of NS5A RASs; in fact, the RASs in NS5A show a low fold-change in resistance compared to the wild-type replicon for new NS5A inhibitors (Figs. 2, 3);
-
in patients with HCV genotype 3, Y93H has a very high fold-change in resistance compared to the wild-type replicon for all NS5A inhibitors; therefore, in the absence of Y93H we can use sofosbuvir + velpatasvir + ribavirin or pibrentasvir + glecaprevir, whereas sofosbuvir + velpatasvir + voxilaprevir is the only re-treatment option available for those showing Y93H (Fig. 4);
-
few data are currently available for patients with HCV genotypes 4–6 with DAA failure and consequently it is preferable not to give indications for reprocessing these patients.
References
Poynard T, Ratziu V, Benmanov Y, Di Martino V, Bedossa P, Opolon P. Fibrosis in patients with chronic hepatitis C: detection and significance. Semin Liver Dis. 2000;20:47–55.
Poynard T, Bedossa P, Opolon P. Natural history of liver fibrosis progression in patients with chronic hepatitis C. Lancet. 1997;349:825–32.
Alter HJ, Seeff LB. Recovery, persistence, and sequelae in hepatitis C virus infection: a perspective on long-term outcome. Semin Liver Dis. 2000;20:17–35.
Coppola N, Zampino R, Bellini G, Macera M, Marrone A, Pisaturo M, Boemio A, Nobili B, Pasquale G, Maione S, Adinolfi LE, Perrone L, Sagnelli E, Miraglia Del Giudice E, Rossi F. Association between a polymorphism in cannabinoid receptor 2 and severe necroinflammation in patients with chronic hepatitis C. Clin Gastroenterol Hepatol. 2014;12:334–40. https://doi.org/10.1016/j.cgh.2013.05.008.
Shepard CW, Finelli L, Alter MJ. Global epidemiology of hepatitis C virus infection. Lancet Infect Dis. 2005;5:558–67.
Lauer GM, Walker BD. Hepatitis C virus infection. N Engl J Med. 2001;345:41–52.
Zaltron S, Spinetti A, Biasi L, Baiguera C, Castelli F. Chronic HCV infection: epidemiological and clinical relevance. BMC Infect Dis. 2012;12:S2. https://doi.org/10.1186/1471-2334-12-S2-S2.
Mohd Hanafiah K, Groeger J, Flaxman AD, Wiersma ST. Global epidemiology of hepatitis C virus infection: new estimates of age-specific antibody to HCV seroprevalence. Hepatology. 2013;57:1333–42. https://doi.org/10.1002/hep.26141.
Centers for Disease Control and Prevention. Surveillance for acute viral hepatitis United States. 56th ed. Atlanta: Centers for Disease Control and Prevention; 2005. p. 1–24.
Santantonio T, Medda E, Ferrari C, Fabris P, Cariti G, Massari M, Babudieri S, Toti M, Francavilla R, Ancarani F, Antonucci G, Scotto G, Di Marco V, Pastore G, Stroffolini T. Risk factors and outcome among a large patient cohort with community-acquired acute hepatitis C in Italy. Clin Infect Dis. 2006;43:1154–9. https://doi.org/10.1086/507640.
Corey KE, Ross AS, Wurcel A, Schulze Zur Wiesch J, Kim AY, Lauer GM, Chung RT. Outcomes and treatment of acute hepatitis C virus infection in a United States population. Clin Gastroenterol Hepatol. 2006;4:1278–82. https://doi.org/10.1016/j.cgh.2006.06.026.
Esteban JI, Sauleda S, Quer J. The changing epidemiology of hepatitis C virus infection in Europe. J Hepatol. 2008;48:148–62.
Martinez-Bauer E, Forns X, Armelles M, Planas R, Solà R, Vergara M, Fàbregas S, Vega R, Salmerón J, Diago M, Sánchez-Tapias JM, Bruguera M, Spanish Acute HCV Study Group. Hospital admission is a relevant source of hepatitis C virus acquisition in Spain. J Hepatol. 2008;48:20–7. https://doi.org/10.1016/j.jhep.2007.07.031.
Benova L, Mohamoud YA, Calvert C, Abu-Raddad LJ. Vertical transmission of hepatitis C virus: systematic review and meta-analysis. Clin Infect Dis. 2014;59:765–73. https://doi.org/10.1093/cid/ciu447.
Kiyosawa K, Sodeyama T, Tanaka E, Nakano Y, Furuta S, Nishioka K, Purcell RH, Alter HJ. Hepatitis C in hospital employees with needlestick injuries. Ann Intern Med. 1991;115:367–9.
Choo QL, Kuo G, Weiner AJ, Overby LR, Bradley DW, Houghton M. Houghton Isolation of a cDNA clone derived from a blood-borne non-A, non-B viral-hepatitis genome. Science. 1989;244:359–62.
Ruta S, Cernescu C. Injecting drug use: a vector for the introduction of new hepatitis C virus genotypes. World J Gastroenterol. 2015;21:10811–23. https://doi.org/10.3748/wjg.v21.i38.10811.
Hijikata M, Mizushima H, Akagi T, Mori S, Kakiuchi N, Kato N, Tanaka T, Kimura K, Shimotohno K. Two distinct proteinase activities required for the processing of a putative nonstructural precursor protein of hepatitis C virus. J Virol. 1993;67:4665–75.
Bartenschlager R. Hepatitis C virus replicons: potential role for drug development. Nat Rev Drug Discov. 2002;1:911–6. https://doi.org/10.1038/nrd942.
Koch JO, Bartenschlager R. Modulation of hepatitis C virus NS5A hyperphosphorylation by nonstructural proteins NS3, NS4A, and NS4B. J Virol. 1999;73:7138–46.
Hanoulle X, Verdegem D, Badillo A, Wieruszeski JM, Penin F, Lippens G. Domain 3 of non-structural protein 5A from hepatitis C virus is natively unfolded. Biochem Biophys Res Commun. 2009;381:634–8.
Smith DB, Bukh J, Kuiken C, Muerhoff AS, Rice CM, Stapleton JT, Simmonds P. Expanded classification of hepatitis C virus into 7 genotypes and 67 subtypes: updated criteria and genotype assignment web resource. Hepatology. 2014;59:318–27.
Gower E, Estes C, Blach S, Razavi-Shearer K, Razavi H. Global epidemiology and genotype distribution of the hepatitis C virus infection. J Hepatol. 2014;61:45–57.
Ghany MG, Strader DB, Thomas DL, Seeff LB, American Association for the Study of Liver Diseases. Diagnosis, management, and treatment of hepatitis C: an update. Hepatology. 2009;49:1335–74. https://doi.org/10.1002/hep.22759.
Coppola N, Martini S, Pisaturo M, Sagnelli C, Filippini P, Sagnelli E. Treatment of chronic hepatitis C in patients with HIV/HCV coinfection. World J Virol. 2015;4:1–12. https://doi.org/10.5501/wjv.v4.i1.1 (review).
Coppola N, Pisaturo M, Zampino R, Macera M, Sagnelli C, Sagnelli E. Hepatitis C virus markers in infection by hepatitis C virus: in the era of directly acting antivirals. World J Gastroenterol. 2015;21:10749–59. https://doi.org/10.3748/wjg.v21.i38.10749.
Coppola N, Pisaturo M, Tonziello G, Sagnelli C, Sagnelli E, Angelillo IF. Efficacy of pegylated interferon α-2a and α-2b in patients with genotype 1 chronic hepatitis C: a meta-analysis. BMC Infect Dis. 2012;12:357. https://doi.org/10.1186/1471-2334-12-357.
Coppola N, Pisaturo M, Sagnelli C, Sagnelli E, Angelillo IF. Peg-interferon plus ribavirin with or without boceprevir or telaprevir for HCV genotype 1: a meta-analysis on the role of response predictors. PLoS One. 2014;9:e94542. https://doi.org/10.1371/journal.pone.0094542 (eCollection 2014).
Italian Association for the Study of the Liver; Italian Society of Infectious, Tropical Diseases; Italian Society for the Study of Sexually Transmitted Diseases. Practice guidelines for the treatment of hepatitis C: recommendations from an AISF/SIMIT/SIMAST Expert Opinion Meeting. Dig Liver Dis. 2010;42:81–91. https://doi.org/10.1016/j.dld.2009.08.001.
European Association of the Study of the Liver. European Association of the Study of the Liver hepatitis C virus clinical practice guidelines. Liver Int. 2011;32(Suppl 1):2–8. https://doi.org/10.1111/j.1478-3231.2011.02703.x.
van der Meer AJ, Veldt BJ, Feld JJ, Wedemeyer H, Dufour JF, Lammert F, Duarte-Rojo A, Heathcote EJ, Manns MP, Kuske L, Zeuzem S, Hofmann WP, de Knegt RJ, Hansen BE, Janssen HL. Association between sustained virological response and all-cause mortality among patients with chronic hepatitis C and advanced hepatic fibrosis. JAMA. 2012;308:2584–93.
Deterding K, Hoener zu Siederdissen C, Port K, Solbach P, Sollik L, Kirschner J, Mix C, Cornberg J, Worzala D, Mix H, Manns MP, Cornberg M, Wedemeyer H. Improvement of liver function parameters in advanced HCV associated liver cirrhosis by IFN-free antiviral therapies. Aliment Pharmacol Ther. 2015;42:889–901.
AASLD-IDSA HCV Guidance. Recommendations for testing, managing, and treating hepatitis C. https://www.hcvguidelines.org. Accessed 1 June 2018.
EASL Recommendations on Treatment of Hepatitis C. Hepatitis C guidance: AASLD-IDSA recommendations for testing, managing, and treating hepatitis C. J Hepatol 2017. 2016;66:153–94.
Coppola N, De Pascalis S, Messina V, Di Caprio G, Martini S, de Stefano G, Starace M, Stornaiuolo G, Stanzione M, Ascione T, Minichini C, Sangiovanni V, Zampino R, Calò F, Rinaldi L, Persico M, Federico A, Buonomo AR, Borgia G, Gaeta GB, Filippini P, Gentile I. ITPase activity modulates the severity of anaemia in HCV-related cirrhosis treated with ribavirin-containing interferon-free regimens. Antivirus Ther. 2017;22:551–8. https://doi.org/10.3851/IMP3134.
Caudai C, Materazzi A, Saladini F, Di Giambenedetto S, Torti C, Ricciardi B, Rossetti B, Almi P, De Luca A, Zazzi M. Natural NS5A inhibitor resistance associated substitutions in hepatitis C virus genotype 1 infected patients from Italy. Clin Microbiol Infect. 2017. https://doi.org/10.1016/j.cmi.2017.08.003.
Zeuzem S, Mizokami M, Pianko S, Mangia A, Han KH, Martin R, et al. NS5A resistance-associated substitutions inpatients with genotype 1 hepatitis C virus: prevalence and effect on treatment outcome. J Hepatol. 2017;66:910–918.
AASLD-IDSA. 2018. Recommendations for testing, managing, and treating hepatitis C. http://www.hcvguidelines.org. Accessed 24 Oct 2017.
Sorbo MC, Cento V, Di Maio VC, Howe AYM, Garcia F, Perno CF, Ceccherini-Silberstein F. Hepatitis C virus drug resistance associated substitutions and their clinical relevance: update 2018. Drug Resist Update. 2018;37:17–39. https://doi.org/10.1016/j.drup.2018.01.004 (Epub 2018 Feb 21. Review. Erratum in: Drug Resist Update).
Wei B, Kang J, Kibukawa M, Chen L, Qiu P, Lahser F, Marton M, Levitan D. Development and validation of a template-independent next-generation sequencing assay for detecting low-level resistance-associated variants of hepatitis C virus. J Mol Diagn. 2016;18(5):643–656. https://doi.org/10.1016/j.jmoldx.2016.04.001. (Epub 2016 Jul 7).
Wang W, Ren Y, Lu Y, Xu Y, Crosby SD, Di Bisceglie AM, Fan X. Template-dependent multiple displacement amplification for profiling human circulating RNA. Biotechniques. 2017;63(1):21–27. https://doi.org/10.2144/000114566.
Paolucci S, Fiorina L, Piralla A, Gulminetti R, Stefano Novati S, Giorgio Barbarini G, Paolo Sacchi P, Mrta Gatti M, Luca Dossena L, Baldanti F. Naturally occurring mutations to HCV protease inhibitors in treatment-naive patients. Virol J. 2012;9:245. https://doi.org/10.1186/1743-422X-9-245.
Costantino A, Spada E, Equestre M, Bruni R, Tritarelli E, Coppola N, Sagnelli C, Sagnelli E, Ciccaglione AR. Naturally occurring mutations associated with resistance to HCV NS5B polymerase and NS3 protease inhibitors in treatment-naive patients with chronic hepatitis C. Virol J. 2015;12:186. https://doi.org/10.1186/s12985-015-0414-1.
Sarrazin C, Zeuzem S. Resistance to direct antiviral agents in patients with hepatitis C virus infection. Gastroenterology. 2010;138:447–62. https://doi.org/10.1053/j.gastro.2009.11.055.
Sullivan JC, De Meyer S, Bartels DJ, Dierynck I, Zhang EZ, Spanks J, Tigges AM, Ghys A, Dorrian J, Adda N, Martin EC, Beumont M, Jacobson IM, Sherman KE, Zeuzem S, Picchio G, Kieffer TL. Evolution of treatment-emergent resistant variants in telaprevir phase 3 clinical trials. Clin Infect Dis. 2013;57:221–9. https://doi.org/10.1093/cid/cit226.
US Food and Drug Administration. Simeprevir product insert. 2013. http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/205123s001lbl.pdf. Accessed 24 May 2018.
McPhee F, Friborg J, Levine S, Chen C, Falk P, Yu F, Hernandez D, Lee MS, Chaniewski S, Sheaffer AK, Pasquinelli C. Resistance analysis of the hepatitis C virus NS3 protease inhibitor asunaprevir. Antimicrob Agents Chemother. 2012;56:3670–81. https://doi.org/10.1128/AAC.00308-12.
Everson GT, Sims KD, Rodriguez-Torres M, Hézode C, Lawitz E, Bourlière M, Loustaud-Ratti V, Rustgi V, Schwartz H, Tatum H, Marcellin P, Pol S, Thuluvath PJ, Eley T, Wang X, Huang SP, McPhee F, Wind-Rotolo M, Chung E, Pasquinelli C, Grasela DM, Gardiner DF. Efficacy of an interferon- and ribavirin-free regimen of daclatasvir, asunaprevir, and BMS-791325 in treatment-naive patients with HCV genotype 1 infection. Gastroenterology. 2014;146:420–9. https://doi.org/10.1053/j.gastro.2013.10.057.
Zeuzem Jacobson IM, Baykal T, Marinho RT, Poordad F, Bourlière M, Sulkowski MS, Wedemeyer H, Tam E, Desmond P, Jensen DM, Di Bisceglie AM, Varunok P, Hassanein T, Xiong J, Pilot-Matias T, DaSilva-Tillmann B, Larsen L, Podsadecki T, Bernstein B. Retreatment of HCV with ABT-450/r-ombitasvir and dasabuvir with ribavirin. N Engl J Med. 2014;370:1604–14. https://doi.org/10.1056/NEJMoa1401561.
Zeuzem S, Ghalib R, Reddy KR, Pockros PJ, Ben Ari Z, Zhao Y, Brown DD, Wan S, DiNubile MJ, Nguyen BY, Robertson MN, Wahl J, Barr E, Butterton JR. Grazoprevir-elbasvir combination therapy for treatment-naive cirrhotic and noncirrhotic patients with chronic hepatitis C virus genotype 1, 4, or 6 infection: a randomized trial. Ann Intern Med. 2015;163:1–13. https://doi.org/10.7326/M15-0785.
Barnard RJ, McHale CM, Newhard W, Cheney CA, Graham DJ, Himmelberger AL, Strizki J, Hwang PM, Rivera AA, Reeves JD, Nickle D, Dinubile MJ, Hazuda DJ, Mobashery N. Emergence of resistance-associated variants after failed triple therapy with vaniprevir in treatment- experienced non-cirrhotic patients with hepatitis C-genotype 1 infection: a population and clonal analysis. Virology. 2013;443:278–84. https://doi.org/10.1016/j.virol.2013.05.013.
Lawitz E, Sulkowski M, Jacobson I, Kraft WK, Maliakkal B, Al-Ibrahim M, Gordon SC, Kwo P, Rockstroh JK, Panorchan P, Miller M, Caro L, Barnard R, Hwang PM, Gress J, Quirk E, Mobashery N. Characterization of vaniprevir, a hepatitis C virus NS3/4A protease inhibitor, in patients with HCV genotype 1 infection: safety, antiviral activity, resistance, and pharmacokinetics. Antivir Res. 2013;99:214–20. https://doi.org/10.1016/j.antiviral.2013.05.015.
Poordad F. High efficacy of ABT-493 and ABT-530 in HCV genotype- 1 infected patients who have failed direct-acting antiviral-containing regimens: the MAGELLAN-I study [Abstract SAT-157]. In: The International Liver CongressTM EASL—European Association for the Study of the Liver. Barcelona, Spain. Journal of Hepatology; 2016. p. S768.
Ng T. Analysis of HCV Genotype 2 and 3 variants in patients treated with combination therapy of next generation HCV direct-acting antiviral agents ABT-493 and ABT-530 [Abstract THU-240]. In: The International liver congress TMEASL—European Association for the Study of the Liver. Barcelona. Journal of Hepatology; 2016. p. S409.
Lawitz E, Yang JC, Stamm LM, Taylor JG, Cheng G, Brainard DM, Miller MD, Mo H, Dvory-Sobol H. Characterization of HCV resistance from a 3-day monotherapy study of voxilaprevir, a novel pangenotypic NS3/4A protease inhibitor. Antivir Ther. 2017. https://doi.org/10.3851/IMP3202.
Dore GJ, Lawitz E, Hézode C, Shafran SD, Ramji A, Tatum HA, Taliani G, Tran A, Brunetto MR, Zaltron S, Strasser SI, Weis N, Ghesquiere W, Lee SS, Larrey D, Pol S, Harley H, George J, Fung SK, de Lédinghen V, Hagens P, McPhee F, Hernandez D, Cohen D, Cooney E, Noviello S, Hughes EA. Daclatasvir plus peginterferon and ribavirin is non-inferior to peginterferon and ribavirin alone, and reduces duration of treatment for HCV genotype 2 or 3 infection. Gastroenterology 2015;148:355–66.e1. https://doi.org/10.1053/j.gastro.2014.10.007.
Jensen D, Sherman KE, Hézode C, Pol S, Zeuzem S, de Ledinghen V, Tran A, Elkhashab M, Younes ZH, Kugelmas M, Mauss S, Everson G, Luketic V, Vierling J, Serfaty L, Brunetto M, Heo J, Bernstein D, McPhee F, Hennicken D, Mendez P, Hughes E, Noviello S, HALLMARK-QUAD Study Team. Daclatasvir and asunaprevir plus peginterferon alfa and ribavirin in HCV genotype 1 or 4 non-responders. J Hepatol. 2015;63:30–7. https://doi.org/10.1016/j.jhep.2015.02.018.
Nelson DR, Cooper JN, Lalezari JP, Lawitz E, Pockros PJ, Gitlin N, Freilich BF, Younes ZH, Harlan W, Ghalib R, Oguchi G, Thuluvath PJ, Ortiz-Lasanta G, Rabinovitz M, Bernstein D, Bennett M, Hawkins T, Ravendhran N, Sheikh AM, Varunok P, Kowdley KV, Hennicken D, McPhee F, Rana K, Hughes EA. ALLY-3 Study Team. All-oral 12-week treatment with daclatasvir plus sofosbuvir in patients with hepatitis C virus genotype 3 infection: ALLY-3 phase III study. Hepatology. 2015;61:1127–35. https://doi.org/10.1002/hep.27726.
Lawitz EJ, Gruener D, Hill JM, Marbury T, Moorehead L, Mathias A, Cheng G, Link JO, Wong KA, Mo H, McHutchison JG, Brainard DM. A phase 1, randomized, placebo-controlled, 3-day, dose-ranging study of GS-5885, an NS5A inhibitor, in patients with genotype 1 hepatitis C. J Hepatol. 2012;57:24–31. https://doi.org/10.1016/j.jhep.2011.12.029.
Afdhal NH, Zeuzem S, Kwo P, Chojkier M, Gitlin N, Puoti M, Romero-Gomez M, Zarski JP, Agarwal K, Buggisch P, Foster GR, Bräu N, Buti M, Jacobson IM, Subramanian GM, Ding X, Mo H, Yang JC, Pang PS, Symonds WT, McHutchison JG, Muir AJ, Mangia A, Marcellin P, ION-1 Investigators. Ledipasvir and sofosbuvir for untreated HCV genotype 1 infection. N Engl J Med. 2014;370:1889–98. https://doi.org/10.1056/NEJMoa1402454.
Krishnan P, Beyer J, Mistry N, Koev G, Reisch T, DeGoey D, Kati W, Campbell A, Williams L, Xie W, Setze C, Molla A, Collins C, Pilot-Matias T. In vitro and in vivo antiviral activity and resistance profile of ombitasvir, an inhibitor of hepatitis C virus NS5A. Antimicrob Agents Chemother. 2015;59:979–87. https://doi.org/10.1128/AAC.04226-14.
Liu R, Curry S, McMonagle P, Yeh WW, Ludmerer SW, Jumes PA, Marshall WL, Kong S, Ingravallo P, Black S, Pak I, DiNubile MJ, Howe AY. Susceptibilities of genotype 1a, 1b, and 3 hepatitis C virus variants to the NS5A inhibitor elbasvir. Antimicrob Agents Chemother. 2015;59:6922–29. https://doi.org/10.1128/AAC.01390-15.
Lawitz EJ, Dvory-Sobol H, Doehle BP, Worth AS, McNally J, Brainard DM, Link JO, Miller M, Mo H. Clinical resistance to velpatasvir (GS-5816), a novel pan-genotypic inhibitor of the hepatitis C virus NS5A protein. Antimicrob Agents Chemother. 2016;60:5368–78. https://doi.org/10.1128/AAC.00763-16.
Feld JJ, Jacobson IM, Hézode C, Asselah T, Ruane PJ, Gruener N, Abergel A, Mangia A, Lai CL, Chan HL, Mazzotta F, Moreno C, Yoshida E, Shafran SD, Towner WJ, Tran TT, McNally J, Osinusi A, Svarovskaia E, Zhu Y, Brainard DM, McHutchison JG, Agarwal K, Zeuzem S, ASTRAL-1 Investigators. Sofosbuvir and velpatasvir for HCV genotype 1, 2, 4, 5, and 6 infection. N Engl J Med. 2015;373:2599–607. https://doi.org/10.1056/NEJMoa1512610.
Poordad F, Landis CS, Asatryan A, Jackson DF 3rd, Ng TI, Fu B, Lin CW, Yao B, Kort J. High antiviral activity of NS5A inhibitor ABT-530 with paritaprevir/ritonavir and ribavirin against hepatitis C virus genotype 3 infection. Liver Int. 2016;36:1125–32. https://doi.org/10.1111/liv.13067.
Wilfret DA, Walker J, Adkison KK, Jones LA, Lou Y, Gan J, Castellino S, Moseley CL, Horton J, de Serres M, Culp A, Goljer I, Spreen W. Safety, tolerability, pharmacokinetics, and antiviral activity of GSK2336805, an inhibitor of hepatitis C virus (HCV) NS5A, in healthy subjects and subjects chronically infected with HCV genotype 1. Antimicrob Agents Chemother. 2013;57:5037–44. https://doi.org/10.1128/AAC.00910-13.
Muir A, Hill J. ACH-3102 A, Second Generation NS5A, Inhibitor, Demonstrates potent antiviral activity in patients with genotype 1A HCV infection despite the presence of baseline NS5A-resistant variants [Abstract 876]. In: The international liver congress TMEASL—European association for the study of the liver; 2013. The Netherlands, Amsterdam: J Hepatol; 2013. p. S360.
Heinrich B. Persistence of resistance-associated variants in hepatitis C virus (HCV) genotypes 1–4 infected subjects following 3-day samatasvir monotherapy. In: International workshop on antiviral drug resistance—meeting the global: antiviral therapy; 2014.
Gane EJ. Nucleotide polymerase inhibitor sofosbuvir plus ribavirin for hepatitis C. N Engl J Med. 2013;368:34–44.
Svarovskaia ES, Gane E, Dvory-Sobol H, Martin R, Doehle B, Hedskog C, Jacobson IM, Nelson DR, Lawitz E, Brainard DM, McHutchison JG, Miller MD, Mo H. L159F and V321A sofosbuvir-associated hepatitis C Virus NS5B substitutions. J Infect Dis. 2016;213:1240-7. https://doi.org/10.1093/infdis/jiv564.
Donaldson EF, Harrington PR, O’Rear JJ, Naeger LK. Clinical evidence and bioinformatics characterization of potential hepatitis C virus resistance pathways for sofosbuvir. Hepatology. 2014;61:56–65
Feld JJ, Kowdley KV, Coakley E, Sigal S, Nelson DR, Crawford D, Weiland O, Aguilar H, Xiong J, Pilot-Matias T, DaSilva-Tillmann B, Larsen L, Podsadecki T, Bernstein B. Treatment of HCV with ABT-450/r-ombitasvir and dasabuvir with ribavirin. N Engl J Med. 2014;370:1594–603. https://doi.org/10.1056/NEJMoa1315722.
Leroy V, Angus P, Bronowicki JP, Hezode C, Pianko S, Pol S, Stuart K, Tse E, McPhee F, Bhore R, Jimenez-Exposito MJ, Thompson AJ. Daclatasvir, sofosbuvir, and ribavirin for hepatitis C virus genotype 3 and advanced liver disease: a randomized phase III study (ALLY-3+). Hepatology. 2016;63:1430–41. https://doi.org/10.1002/hep.28473.
Krishnan P, Tripathi R, Schnell G, Reisch T, Beyer J, Irvin M, Xie W, Larsen L, Cohen D, Podsadecki T, Pilot-Matias T, Collins C. Resistance analysis of baseline and treatment-emergent variants in hepatitis C virus genotype 1 in the AVIATOR study with paritaprevir-ritonavir, ombitasvir, and dasabuvir. Antimicrob Agents Chemother. 2015;59:5445–54. https://doi.org/10.1128/AAC.00998-15.
Kwo P, Gitlin N, Nahass R, Bernstein D, Etzkorn K, Rojter S, Schiff E, Davis M, Ruane P, Younes Z, Kalmeijer R, Sinha R, Peeters M, Lenz O, Fevery B, De La Rosa G, Scott J. Witek J.Simeprevir plus sofosbuvir (12 and 8 weeks) in HCV genotype 1-infected patients without cirrhosis: OPTIMIST-1, a phase 3. Randomized study. Hepatology. 2016;64:370–80. https://doi.org/10.1002/hep.28467.
Lawitz E, Matusow G, DeJesus E, Yoshida EM, Felizarta F, Ghalib R, Godofsky E, Herring RW, Poleynard G, Sheikh A, Tobias H, Kugelmas M, Kalmeijer R, Peeters M, Lenz O, Fevery B, De La Rosa G, Scott J, Sinha R, Witek J. Simeprevir plus sofosbuvir in patients with chronic hepatitis C virus genotype 1 infection and cirrhosis: a phase 3 study (OPTIMIST-2). Hepatology. 2015;64:360–9. https://doi.org/10.1002/hep.28422.
Poordad F, Schiff ER, Vierling JM, Landis C, Fontana RJ, Yang R, McPhee F, Hughes EA, Noviello S, Swenson ES. Daclatasvir with sofosbuvir and ribavirin for hepatitis C virus infection with advanced cirrhosis or post-liver transplantation recurrence. Hepatology. 2016;63:1493–505. https://doi.org/10.1002/hep.28446.
Pawlotsky JM. Hepatitis C Virus resistance to direct-acting antiviral drugs in interferon-free regimens. Gastroenterology. 2016;151:70–86.
Starace M, Minichini C, De Pascalis S, Macera M, Occhiello L, Messina V, Sangiovanni V, Adinolfi LE, Claar E, Precone D, Stornaiuolo G, Stanzione M, Ascione T, Caroprese M, Zampino R, Parrilli G, Gentile I, Brancaccio G, Iovinella V, Martini S, Masarone M, Fontanella L, Masiello A, Sagnelli E, Punzi R, Salomone Megna A, Santoro R, Gaeta GB, Coppola N. Virological patterns of HCV patients with failure to interferon-free regimens. J Med Virol. 2018. https://doi.org/10.1002/jmv.25022.
Coppola N, Minichini C, Starace M, Sagnelli C, Sagnelli E. Clinical impact of the hepatitis C virus mutations in the era of directly acting antivirals. J Med Virol. 2016;88:1659–71. https://doi.org/10.1002/jmv.24527.
Loreta LA, Gaeta GB, Brunetto MR, Di Leo A, Iannone A, Santantonio TA, Giammario A, Raimondo G, Filomia R, Coppola C, Amoruso DC, Blanc P, Del Pin B, Chemello L, Cavalletto L, Morisco F, Donnarumma L, Rumi MG, Gasbarrini A, Siciliano M, Massari M, Corsini R, Coco B, Madonia S, Cannizzaro M, Zignego AL, Monti M, Russo FP, Zanetto A, Persico M, Masarone M, Villa E, Bernabucci V, Taliani G, Biliotti E, Chessa L, Pasetto MC, Andreone P, Margotti M, Brancaccio G, Ieluzzi D, Borgia G, Zappulo E, Calvaruso V, Petta S, Falzano L, Quaranta MG, Weimer LE, Rosato S, Vella S, Giannini EG. Incidence of DAA failure and the clinical impact of retreatment in real-life patients treated in the advanced stage of liver disease: interim evaluations from the PITER network. PLoS One. 2017;12:e0185728. https://doi.org/10.1371/journal.pone.0185728.
Yoshimi S, Imamura M, Murakami E, Hiraga N, Tsuge M, Kawakami Y, Aikata H, Abe H, Hayes CN, Sasaki T, Ochi H, Chayama K. Long term persistence of NS5A inhibitor-resistant hepatitis C virus in patients who failed daclatasvir and asunaprevir therapy. J Med Virol. 2015;87:1913–20. https://doi.org/10.1002/jmv.24255.
Lawitz E, Flamm S, Yang JC, Shyam K, Pfeiffer RM. Retreatment of patients who failed 8 or 12 weeks of ledipasvir/sofosbuvir- based regimens with ledipasvir/sofosbuvir for 24 weeks. J Hepatol. 2015;62:S192.
Gane EJ, Shiffman ML, Etzkorn K, Morelli G, Stedman C, Davis MN, Hinestrosa F. Sofosbuvir/velpatasvir in combination with ribavirin for 24 weeks is effective retreatment for patients who failed prior NS5A- containing DAA regimens: results of the retreatment study. J Hepatol. 2016;64:147.
Sarrazin C, Dvory-Sobol H, Svarovskaia ES, Doehle BP, Pang PS, Chuang SM, Ma J, Ding X, Afdhal NH, Kowdley KV, Gane EJ, Lawitz E, Brainard DM, McHutchison JG, Miller MD, Mo H. Prevalence of resistance- associated substitutions in HCV NS5A, NS5B, or NS3 and outcomes of treatment with ledipasvir and sofosbuvir. Gastroenterology. 2016;151:501–12. https://doi.org/10.1053/j.gastro.2016.06.002.
Craxi A, Perno CF, Vigano M, Ceccherini-Silberstein F, Petta S. From current status to optimization of HCV treatment: recommendations from an expert panel. Dig Liver Dis. 2016;48:995–1005.
Hézode C, Chevaliez S, Scoazec G, Soulier A, Varaut A, Bouvier-Alias M, Ruiz I, Roudot-Thoraval F, Mallat A, Féray C, Pawlotsky JM. Retreatment with sofosbuvir and simeprevir of patients with hepatitis C virus genotype 1 or 4 who previously failed a daclatasvir-containing regimen. Hepatology. 2016;63:1809–16. https://doi.org/10.1002/hep.28491.
Pianko S, Flamm SL, Shiffman ML, Kumar S, Strasser SI, Dore GJ, McNally J, Brainard DM, Han L, Doehle B, Mogalian E, McHutchison JG, Rabinovitz M, Towner WJ, Gane EJ, Stedman CA, Reddy KR, Roberts SK. Sofosbuvir plus velpatasvir combination therapy for treatment-experienced patients with genotype 1 or 3 hepatitis C virus infection: a randomized trial. Ann Intern Med. 2015;163:809–17. https://doi.org/10.7326/M15-1014.
Reddy KR, Bourlière M, Sulkowski M, Omata M, Zeuzem S, Feld JJ, Lawitz E, Marcellin P, Welzel TM, Hyland R, Ding X, Yang J, Knox S, Pang P, Dvory-Sobol H, Subramanian GM, Symonds W, McHutchison JG, Mangia A, Gane E, Mizokami M, Pol S, Afdhal N. Ledipasvir and sofosbuvir in patients with genotype 1 hepatitis C virus infection and compensated cirrhosis: an integrated safety and efficacy analysis. Hepatology. 2015;62:79–86. https://doi.org/10.1002/hep.27826.
Bourliere M, Gordon SC, Flamm SL, Cooper CL, Ramji A, Tong M, Ravendhran N, Vierling JM, Tran TT, Pianko S, Bansal MB, de Lédinghen V, Hyland RH, Stamm LM, Dvory-Sobol H, Svarovskaia E, Zhang J, Huang KC, Subramanian GM, Brainard DM, McHutchison JG, Verna EC, Buggisch P, Landis CS, Younes ZH, Curry MP, Strasser SI, Schiff ER, Reddy KR, Manns MP, Kowdley KV, Zeuzem S, POLARIS-1 and POLARIS-4 Investigators. Sofosbuvir, velpatasvir, and voxilaprevir for previously treated HCV infection. N Engl J Med. 2017;376:2134–46. https://doi.org/10.1056/NEJMoa1613512.
Poordad F, Pol S, Asatryan A, Buti M, Shaw D, Hézode C, Felizarta F, Reindollar RW, Gordon SC, Pianko S, Fried MW, Bernstein DE, Gallant J, Lin CW, Lei Y, Ng TI, Krishnan P, Kopecky-Bromberg S, Kort J, Mensa FJ. Glecaprevir/pibrentasvir in patients with hepatitis C virus genotype 1 or 4 and past direct-acting antiviral treatment failure. Hepatology. 2017. https://doi.org/10.1002/hep.29671.
Poordad F, Felizarta F, Asatryan A, Sulkowski MS, Reindollar RW, Landis CS, Landis CS, Gordon SC, Flamm SL, Fried MW, Bernstein DE, Lin CW, Liu R, Lovell SS, Ng TI, Kort J, Mensa FJ. Glecaprevir and pibrentasvir for 12 weeks for hepatitis C virus genotype 1 infection and prior direct-acting antiviral treatment. Hepatology. 2017;66:389–97. https://doi.org/10.1002/hep.29081.
Poordad F, Pol S, Asatryan A, Buti M, Shaw DR, Hezode C, Felizarta F, Reindollar RW, Gordon SC, Pianko S, Fried MW, Bernstein DE, Gallant J, Lin CW, Lei Y, Ng TI, Krishnan P, Kopecky-Bromberg S, Kort J, Mensa FJ. Glecapreir and pibrentasvir for 12 or 16 weeks in patients with chronic HCV genotype 1 or 4 and prior direct-acting antiviral treatment failure. Gastroenterology. 2017;152:1057. https://doi.org/10.1002/hep.29671.
de Lédinghen V, Laforest C, Hézode C, Pol S, Renault A, Alric L, Larrey D, Métivier S, Tran A, Jézéquel C, Samuel D, Zoulim F, Tual C, Pailhé A, Gibowski S, Bourlière M, Bellissant E, Pawlotsky JM. Retreatment with sofosbuvir plus grazoprevir/elbasvir plus ribavirin of patients with hepatitis C virus genotype 1 or 4 who previously failed a NS5A or NS3-containing regimen. ANRS HC34 REVENGE. Clin Infect Dis. 2017. https://doi.org/10.1093/cid/cix916.
Di Maio VC, Cento V, Lenci I, Aragri M, Rossi P, Barbaliscia S, Melis M, Verucchi G, Magni CF, Teti E, Bertoli A, Antonucci F, Bellocchi MC, Micheli V, Masetti C, Landonio S, Francioso S, Santopaolo F, Pellicelli AM, Calvaruso V, Gianserra L, Siciliano M, Romagnoli D, Cozzolongo R, Grieco A, Vecchiet J, Morisco F, Merli M, Brancaccio G, Di Biagio A, Loggi E, Mastroianni CM, Pace Palitti V, Tarquini P, Puoti M, Taliani G, Sarmati L, Picciotto A, Vullo V, Caporaso N, Paoloni M, Pasquazzi C, Rizzardini G, Parruti G, Craxì A, Babudieri S, Andreoni M, Angelico M, Perno CF, Ceccherini-Silberstein F, HCV Italian Resistance Network Study Group. Multiclass HCV resistance to direct-acting antiviral failure in real-life patients advocates for tailored second-line therapies. Liver Int. 2017;37:514–28. https://doi.org/10.1111/liv.13327.
Salerno F, Borzio M, Pedicino C, Simonetti R, Rossini A, Boccia S, Cacciola I, Burroughs AK, Manini MA, La Mura V, Angeli P, Bernardi M, Dalla Gasperina D, Dionigi E, Dibenedetto C, Arghittu M, AISF Investigators. The impact of infection by multidrug-resistant agents in patients with cirrhosis. A multicenter prospective study. Liver Int. 2017;37:71–9. https://doi.org/10.1111/liv.13195.
Manns M, Pol S, Jacobson IM, Marcellin P, Gordon SC, Peng CY, Chang TT, Everson GT, Heo J, Gerken G, Yoffe B, Towner WJ, Bourliere M, Metivier S, Chu CJ, Sievert W, Bronowicki JP, Thabut D, Lee YJ, Kao JH, McPhee F, Kopit J, Mendez P, Linaberry M, Hughes E, Noviello S, HALLMARK-DUAL Study Team. All-oral daclatasvir plus asunaprevir for hepatitis C virus genotype 1b: a multinational, phase 3, multicohort study. Lancet. 2014;384:1597–605.
Kumad H, Suzuki Y, Ikeda K, Toyota J, Karino Y, Chayama K, Kawakami Y, Ido A, Yamamoto K, Takaguchi K, Izumi N, Koike K, Takehara T, Kawada N, Sata M, Miyagoshi H, Eley T, McPhee F, Damokosh A, Ishikawa H, Hughes E. Daclatasvir plus asunaprevir for chronic HCV genotype 1b infection. Hepatology. 2014;59:2083–91. https://doi.org/10.1002/hep.27113.
Fevery B, Thys K, Van Eygen V, Verbinnen T, Van Rossem E, Buelens A, Aerssens J, Witek J, Picchio G, De Meyer S, Lenz O. Pre-existence and persistence of resistant minority hepatitis C virus variants in genotype 1-infected patients treated with simeprevir/peginterferon/ribavirin. Open Forum Infect Dis. 2016;3:ofw052. https://doi.org/10.1093/ofid/ofw052.
Jiang M, Mani N, Lin C, Ardzinski A, Nelson M, Reagan D, Bartels D, Zhou Y, Nicolas O, Rao BG, Müh U, Hanzelka B, Tigges A, Rijnbrand R, Kieffer TL. In vitro phenotypic characterization of hepatitis C virus NS3 protease variants observed in clinical studies of telaprevir. Antimicrob Agents Chemother. 2013;57:6236–45. https://doi.org/10.1128/AAC.01578-13.
Lagace L, White PW, Bousquet C, Dansereau N, Dô F, Llinas-Brunet M, Marquis M, Massariol MJ, Maurice R, Spickler C, Thibeault D, Triki I, Zhao S, Kukolj G. In vitro resistance profile of the hepatitis C virus NS3 protease inhibitor BI 201335. Antimicrob Agents Chemother. 2012;56:569–72. https://doi.org/10.1128/AAC.05166-11.
Fridell RA, Qiu D, Valera L, Wang C, Rose RE, Gao M. Distinct functions of NS5A in hepatitis C virus RNA replication uncovered by studies with the NS5A inhibitor BMS-790052. J Virol. 2011;85:7312–20.
Verbinnen T, Fevery B, Vijgen L, Jacobs T, De Meyer S, Lenz O. In vitro activity of simeprevir against hepatitis C virus genotype 1 clinical isolates and its correlation with NS3 sequence and site-directed mutants. Antimicrob Agents Chemother. 2015;59:7548–57.
Lontok E, Harrington P, Howe A, Kieffer T, Lennerstrand J, Lenz O, McPhee F, Mo H, Parkin N, Pilot-Matias T, Miller V. Hepatitis C virus drug resistance-associated substitutions: state of the art summary. Hepatology. 2015;62:1623–32. https://doi.org/10.1002/hep.27934.
Krishnan P, Schnell G, Tripathi R, Beyer J, Reisch T, Zhang X, Setze C, Rodrigues L Jr, Burroughs M, Redman R, Chayama K, Kumada H, Collins C, Pilot-Matias T. Analysis of hepatitis C virus genotype 1b resistance variants in Japanese patients treated with paritaprevir-ritonavir and ombitasvir. Antimicrob Agents Chemother. 2016;60:1106–13. https://doi.org/10.1128/AAC.02606-15.
Pilot-Matias T, Tripathi R, Cohen D, Gaultier I, Dekhtyar T, Lu L, Reisch T, Irvin M, Hopkins T, Pithawalla R, Middleton T, Ng T, McDaniel K, Or YS, Menon R, Kempf D, Molla A, Collins C. In vitro and in vivo antiviral activity and resistance profile of the hepatitis C virus NS3/4A protease inhibitor ABT-450. Antimicrob Agents Chemother. 2015;59:988–97. https://doi.org/10.1128/AAC.04227-14.
Ludmerer SW, Hirano T, Black S, Howe AY, Chang W, Takase A, Nakamura K, Tanaka Y, Kumada H, Hayashi N, Nickle D. HCV evolutionary genetics of SVR versus virologic failure assessed from the vaniprevir phase III registration trials. Antivir Res. 2016;130:118–29. https://doi.org/10.1016/j.antiviral.2016.03.004.
Poordad F, Gordon SC, Asatryan A, et al. High efficacy of ABT-493 and ABT-530 in HCV genotype-1 infected patients who have failed direct-acting antiviral-containing regimens: the MAGELLAN-I 19 study [Abstract SAT-157]. In: The international liver congress™ EASL—European association for the study of the liver. Barcelona, Spain: Journal of Hepatology; 2016. p. S768.
Gane EJ, Schwabe C, Hyland RH, et al. Efficacy of the combination of sofosbuvir, velpatasvir, and the NS3/4A protease inhibitor GS-9857 in treatment-naive or previously treated patients with HCV genotype 1 or 3 infections. Gastroenterology. 2016;151:448–456
Lawitz E, Dvory-Sobol H, Yang JC, et al. Characterization of HCV resistance from a 3-day monotherapy study of GS-9857, a novel pangenotypic NS3/4A protease inhibitor [Abstract 718]. American Association for the Study of Liver Diseases (AASLD), vol. 62 San Francisco: Hepatology; 2015. p. 119A.
Bartolini B, Selleri M, Garbuglia AR, Giombini E, Taibi C, Lionetti R, D’Offizi G, Capobianchi MR. HCV NS3 quasispecies in liver and plasma and dynamics of telaprevir resistant variants in breakthrough patients assessed by UDPS: a case study. J Clin Virol. 2015;72:60–5.
Beloukas A, King S, Childs K, Papadimitropoulos A, Hopkins M, Atkins M, Agarwal K, Nelson M, Geretti AM. Detection of the NS3 Q80K polymorphism by Sanger and deep sequencing in hepatitis C virus genotype 1a strains in the UK. Clin Microbiol Infect. 2015;21:1033–339.
Boglione L, De Nicolo A, Cardellino CS, Ruggiero T, Ghisetti V, Cariti G, Di Perri G, D’Avolio A. Relationship between the early boceprevir-S isomer plasma concentrations and the onset of breakthrough during HCV genotype 1 triple therapy. Clin Microbiol Infect. 2015;21:205.e1.
Liverton NJ, Carroll SS, Dimuzio J, et al. MK-7009, a potent and selective inhibitor of hepatitis C virus NS3/4A protease. Antimicrob Agents Chemother. 2010;54:305–11.
Verbinnen T, Van Marck H, Vandenbroucke I, et al. Tracking the evolution of multiple in vitro hepatitis C virus replicon variants under protease inhibitor selection pressure by 454 deep sequencing. J Virol. 2010;84:11124–33.
Larrat S, Vallet S, David-Tchouda S, Caporossi A, Margier J, Ramiere C, Scholtes C, Ha€ım-Boukobza S, Roque-Afonso AM, Besse B, Andre-Garnier E, Mohamed S, Halfon P, Pivert A, LeGuillou-Guillemette H, Abravanel F, Guivarch M, Mackiewicz V, Lada O, Mourez T, Plantier JC, Baazia Y, Alain S, Hantz S, Thibault V, Gaudy-Graffin C, Bouvet D, Mirand A, Henquell C, Gozlan J, Lagathu G, Pronier C, Velay A, Schvoerer E, Trimoulet P, Fleury H, Bouvier-Alias M, Brochot E, Duverlie G, Maylin S, Gouriou S, Pawlotsky JM, Morand P. Naturally occurring resistance-associated variants of hepatitis C virus protease inhibitors in poor responders to pegylated interferon-ribavirin. J Clin Microbiol. 2015;53:2195–202.
Susser S, Dietz J, Vermehren J, et al. European RAVs database: frequency and characteristics of RAVs in treatment-naive and DAA-experienced patients [Abstract PS007]. In: Abstracts of the international liver congress™ 2016, EASL—European Association for the Study of the Liver. Barcelona, Spain: Journal of Hepatology; 2016. p. S139.
Kumada H, Chayama K, Rodrigues L Jr, Suzuki F, Ikeda K, Toyoda H, Sato K, Karino Y, Matsuzaki Y, Kioka K, Setze C, Pilot-Matias T, Patwardhan M, Vilchez RA, Burroughs M, Redman R. Randomized phase 3 trial of ombitasvir/paritaprevir/ritonavir for hepatitis C virus genotype 1b-infected Japanese patients with or without cirrhosis. Hepatology. 2015;62:1037–46. https://doi.org/10.1002/hep.27972.
Schnell G, Tripathi R, Beyer J, et al. Hepatitis C virus genotype 4 resistance and subtype demographic characterization of patients treated with ombitasvir plus paritaprevir/ritonavir. Antimicrob Agents Chemother. 2015;59:6807–15.
Iio E, Shimada N, Abe H, et al. Efficacy of daclatasvir/asunaprevir according to resistance-associated variants in chronic hepatitis C with genotype 1. J Gastroenterol. 2016. https://doi.org/10.1007/s00535-016-1225-x (Epub 2016 May 28).
McPhee F, Hernandez D, Yu F, et al. Resistance analysis of hepatitis C virus genotype 1 prior treatment null responders receiving daclatasvir and asunaprevir. Hepatology. 2013;58:902–11. https://doi.org/10.1002/hep.26388 (Epub 2013 Jul 16).
Lenz O, Verbinnen T, Fevery B, et al. Virology analyses of HCV isolates from genotype 1-infected patients treated with simeprevir plus peginterferon/ribavirin in phase IIb/III studies. J Hepatol. 2015;62:1008–14.
Ruggiero T, Proietti A, Boglione L, Milia MG, Allice T, Burdino E, Orofino G, Bonora S, Di Perri G, Ghisetti V. Predominance of hepatitis C virus Q80K among NS3 baseline-resistance associated amino acid variants in direct-antiviral-agent-naïve patients with chronic hepatitis: single-centre experience. Arch Virol. 2015;160:2881–5.
Dietz J, Susser S, Vermehren J, Peiffer KH, Grammatikos G, Berger A, Ferenci P, Buti M, Müllhaupt B, Hunyady B, Hinrichsen H, Mauss S, Petersen J, Buggisch P, Felten G, Hüppe D, Knecht G, Lutz T, Schott E, Berg C, Spengler U, von Hahn T, Berg T, Zeuzem S, Sarrazin C, European HCV Resistance Study Group. Patterns of resistance-associated substitutions in patients with chronic HCV infection following treatment with direct-acting antivirals. Gastroenterology. 2017. https://doi.org/10.1053/j.gastro.2017.11.007.
Taylor JG, Appleby T, Barauskas O, et al. Preclinical profile of the pan-genotypic HCV NS3/4A protease inhibitor GS-9857 [Abstract P0899]. In: EASL—the international liver congress 2015 50th annual Meeting of the European association for the Study of the Liver. Vienna, Austria: Journal of Hepatology; 2015. p. S681.
Kattakuzhy S, Wilson E, Sidharthan S, et al. Moderate sustained virologic response rates with 6-week combination directly acting anti-hepatitis C virus therapy in patients with advanced liver disease. Clin Infect Dis. 2016;62:440–7.
Lim SR, Qin X, Susser S, Nicholas JB, Lange C, Herrmann E, Hong J, Arfsten A, Hooi L, Bradford W, Nájera I, Smith P, Zeuzem S, Kossen K, Sarrazin C, Seiwert SD. Virologic escape during danoprevir (ITMN-191/RG7227) monotherapy is hepatitis C virus subtype dependent and associated with R155K substitution. Antimicrob Agents Chemother. 2012;56:271–79. https://doi.org/10.1128/AAC.05636-11.
Romano KP, Ali A, Aydin C, Soumana D, Ozen A, Deveau LM, Silver C, Cao H, Newton A, Petropoulos CJ, Huang W, Schiffer CA. The molecular basis of drug resistance against hepatitis C virus NS3/4A protease inhibitors. PLoS Pathog. 2012;8:e1002832. https://doi.org/10.1371/journal.ppat.1002832.
Serre SB, Jensen SB, Ghanem L, Humes DG, Ramirez S, Li YP, Krarup H, Bukh J, Gottwein JM. Hepatitis C virus genotype 1 to 6 protease inhibitor escape variants: in vitro selection, fitness, and resistance patterns in the context of the infectious viral life cycle. Antimicrob Agents Chemother. 2016;60:3563–78. https://doi.org/10.1128/AAC.02929-15.
Howe AY, Black S, Curry S, Ludmerer SW, Liu R, Barnard RJ, Newhard W, Hwang PM, Nickle D, Gilbert C, Caro L, DiNubile MJ, Mobashery N. Virologic resistance analysis from a phase 2 study of MK-5172 combined with pegylated interferon/ribavirin in treatment-naive patients with hepatitis C virus genotype 1 infection. Clin Infect Dis. 2014;59:1657–65. https://doi.org/10.1093/cid/ciu696.
Soumana DI, Ali A, Schiffer CA. Structural analysis of asunaprevir resistance in HCV NS3/4A protease. ACS Chem Biol. 2014;9:2485–90.
Jensen SB, Serre SB, Humes DG, Ramirez S, Li YP, Bukh J, Gottwein JM. Substitutions at NS3 residue 155, 156, or 168 of hepatitis C virus genotypes 2 to 6 induce complex patterns of protease inhibitor resistance. Antimicrob Agents Chemother. 2015;59:7426–36. https://doi.org/10.1128/AAC.01953-15.
Black S, Pak I, Ingravallo P, et al. Resistance analysis of virologic failures in hepatitis c genotype 1-infected patients treated with grazoprevir + elbasvir ± ribavirin: the C-WORTHY study [abstract P0891]. In: The international liver congress 2015, 50th annual meeting of the European association for the Study of the Liver (EASL). Vienna, Austria: Journal of Hepatology; 2015. p. S677–S8.
Ng T, Reisch T, Middleton T, et al. ABT-493, a Potent HCV NS3/4A protease inhibitor with broad genotype coverage [abstract 636]. In: 21st conference on retroviruses and opportunistic infections-CROI. Boston; 2014.
Reau N, Nguyen MH, Kowdley KV, et al. Integrated resistance analyses of HCV-infected patients treated with sofosbuvir, velpatasvir and voxilaprevir for 8 and 12 weeks from phase 2 studies [Poster 846. American Association for the Study of Liver Diseases (AASLD). Boston: Hepatology; 2016.
Ali A, Aydin C, Gildemeister R, Romano KP, Cao H, Ozen A, Soumana D, Newton A, Petropoulos CJ, Huang W, Schiffer CA. Evaluating the role of macrocycles in the susceptibility of hepatitis C virus NS3/4A protease inhibitors to drug resistance. ACS Chem Biol. 2013;8:1469–78. https://doi.org/10.1021/cb400100g.
Suzuki Y, Ikeda K, Suzuki F, Toyota J, Karino Y, Chayama K, Kawakami Y, Ishikawa H, Watanabe H, Hu W, Eley T, McPhee F, Hughes E, Kumada H. Dual oral therapy with daclatasvir and asunaprevir for patients with HCV genotype 1b infection and limited treatment options. J Hepatol. 2013;58:655–62. https://doi.org/10.1016/j.jhep.2012.09.037.
Zeuzem S, Foster GR, Wang S, Asatryan A, Gane E, Feld JJ, Asselah T, Bourlière M, Ruane PJ, Wedemeyer H, Pol S, Flisiak R, Poordad F, Chuang WL, Stedman CA, Flamm S, Kwo P, Dore GJ, Sepulveda-Arzola G, Roberts SK, Soto-Malave R, Kaita K, Puoti M, Vierling J, Tam E, Vargas HE, Bruck R, Fuster F, Paik SW, Felizarta F, Kort J, Fu B, Liu R, Ng TI, Pilot-Matias T, Lin CW, Trinh R, Mensa FJ. Glecaprevir-pibrentasvir for 8 or 12 weeks in HCV genotype 1 or 3 infection. N Engl J Med. 2018;378:354–69. https://doi.org/10.1056/NEJMoa1702417.
Gane E, Svarovskaia ES, Hyland RH, et al. Resistance analysis of treatment-naïve and DAA-experienced genotype 1 patients with and without cirrhosis who received short-duration treatment with sofosbuvir/velpatasvir + GS-9857 [abstract 713], Vol. 62. San Francisco: Hepatology: American Association for the Study of Liver Diseases (AASLD); 2015.
Karino Y, Toyota J, Ikeda K, Suzuki F, Chayama K, Kawakami Y, Ishikawa H, Watanabe H, Hernandez D, Yu F, McPhee F, Kumada H. Characterization of virologic escape in hepatitis C virus genotype 1b patients treated with the direct-acting antivirals daclatasvir and asunaprevir. J Hepatol. 2013;58:646–54. https://doi.org/10.1016/j.jhep.2012.11.012.
Wang C, Jia L, O’Boyle DR 2nd, Sun JH, Rigat K, Valera L, Nower P, Huang X, Kienzle B, Roberts S, Gao M, Fridell RA. Comparison of daclatasvir resistance barriers on NS5A from hepatitis C virus genotypes 1 to 6: implications for cross-genotype activity. Antimicrob Agents Chemother. 2014;58:5155–63. https://doi.org/10.1128/AAC.02788-14.
Bilello JP, Lallos LB, McCarville JF, La Colla M, Serra I, Chapron C, Gillum JM, Pierra C, Standring DN, Seifer M. In vitro activity and resistance profile of samatasvir, a novel NS5A replication inhibitor of hepatitis C virus. Antimicrob Agents Chemother. 2014;58:4431–42. https://doi.org/10.1128/AAC.02777-13.
Zhou N, Hernandez D, Ueland J, Yang X, Yu F, Sims K, Yin PD, McPhee F. NS5A sequence heterogeneity and mechanisms of daclatasvir resistance in hepatitis C virus genotype 4 infection. The Journal of infectious diseases. 2016;213:206–15. https://doi.org/10.1093/infdis/jiv379.
Manns M, Samuel D, Gane EJ, Mutimer D, McCaughan G, Buti M, Prieto M, Calleja JL, Peck-Radosavljevic M, Müllhaupt B, Agarwal K, Angus P, Yoshida EM, Colombo M, Rizzetto M, Dvory-Sobol H, Denning J, Arterburn S, Pang PS, Brainard D, McHutchison JG, Dufour JF, Van Vlierberghe H, van Hoek B, Forns X. SOLAR-2 investigators. Ledipasvir and sofosbuvir plus ribavirin in patients with genotype 1 or 4 hepatitis C virus infection and advanced liver disease: a multicentre, open-label, randomised, phase 2 trial. Lancet Infect Dis. 2016;16:685–97. https://doi.org/10.1016/S1473-3099(16)00052-9.
Schnell G, Tripathi R, Beyer J, et al. Combined resistance, demographic, and phylogenetic analysis of HCV genotype 4-infected patients treated with ombitasvir/paritaprevir/r +/- ribavirin in the PEARL-I and AGATE-I studies [Poster 866. In: American Association for the Study of Liver Diseases (AASLD). Boston (MA): Hepatology; 2016. p. 427–176.
Jacobson IM, Liu EA-A. R, et al. Prevalence and impact of baseline NS5A resistance associated variants (RAVs) on the efficacy of elbasvir/grazoprevir (EBR/GZR) against GT1a infection [abstract LB22]. In: American Association for the Study of Liver Diseases (AASLD). San Francisco: Hepatology; 2015.
Peres-da-Silva A, de Almeida A, Lampe E. NS5A inhibitor resistance-associated polymorphisms in Brazilian treatment-naive patients infected with genotype 1 hepatitis C virus. J Antimicrob Chemother. 2015;70:726–30.
Asselah T, Reesink H, Gerstoft J, de Ledinghen V, Pockros PJ, Robertson M, Hwang P, Asante-Appiah E, Wahl J, Nguyen BY, Barr E, Talwani R, Serfaty L. Efficacy of elbasvir and grazoprevir in participants with hepatitis C virus genotype 4 infection: a pooled analysis. Liver Int. 2018. https://doi.org/10.1111/liv.13727.
Hezode C, Colombo M, Spengler U, et al. C-EDGE IBLD: efficacy and safety of elbasvir/grazoprevir in patients with chronic hepatitis c virus infection and inherited blood disorders [Abstract SAT-128]. In: The international liver congress™ EASL—European Association for the Study of the Liver. Barcelona: Journal of Hepatology; 2016. p. S753.
Ferenci P, Bernstein D, Lalezari J, Cohen D, Luo Y, Cooper C, Tam E, Marinho RT, Tsai N, Nyberg A, Box TD, Younes Z, Enayati P, Green S, Baruch Y, Bhandari BR, Caruntu FA, Sepe T, Chulanov V, Janczewska E, Rizzardini G, Gervain J, Planas R, Moreno C, Hassanein T, Xie W, King M, Podsadecki T, Reddy KR, PEARL-III Study; PEARL-IV Study. ABT-450/r-ombitasvir and dasabuvir with or without ribavirin for HCV. N Engl J Med. 2014;370:1983-92. https://doi.org/10.1056/NEJMoa1402338.
Komatsu TE, Boyd S, Sherwat A, Tracy L, Naeger LK, O’Rear JJ, Harrington PR. Regulatory analysis of effects of hepatitis C virus NS5A polymorphisms on efficacy of elbasvir and grazoprevir. Gastroenterology. 2017;152:586–97. https://doi.org/10.1053/j.gastro.2016.10.017.
Rockstroh JK, Nelson M, Katlama C, Lalezari J, Mallolas J, Bloch M, Matthews GV, Saag MS, Zamor PJ, Orkin C, Gress J, Klopfer S, Shaughnessy M, Wahl J, Nguyen BY, Barr E, Platt HL, Robertson MN, Sulkowski M. Efficacy and safety of grazoprevir (MK-5172) and elbasvir (MK-8742) in patients with hepatitis C virus and HIV co-infection (C-EDGE CO-INFECTION): a non-randomised, open-label trial. Lancet HIV. 2015;2:e319–27. https://doi.org/10.1016/S2352-3018(15)00114-9.
Patel D, Zhao Y, Fabrycki J, et al. Achievement of SVR24 despite the presence of HCV variants resistant to first-generation NS5A inhibitors in genotype-1 hepatitis C patients after 8-week therapy of ACH-3102 in combination with sofosbuvir [Abstract P0805]. In: EASL—the international liver congress 2015 50th annual Meeting of the European association for the Study of the Liver. Vienna, Austria: Journal of Hepatology; 2015.
Huang W, Newton A, Frantzell A, et al. Genotypic and phenotypic characterization of clinical HCV NS5A drug resistance [abstract 579]. In: Conference on retroviruses and opportunistic infections (CROI). Boston; 2016.
Lawitz E, Gane E, Pearlman B, Tam E, Ghesquiere W, Guyader D, Alric L, Bronowicki JP, Lester L, Sievert W, Ghalib R, Balart L, Sund F, Lagging M, Dutko F, Shaughnessy M, Hwang P, Howe AY, Wahl J, Robertson M, Barr E, Haber B. Efficacy and safety of 12 weeks versus 18 weeks of treatment with grazoprevir (MK-5172) and elbasvir (MK-8742) with or without ribavirin for hepatitis C virus genotype 1 infection in previously untreated patients with cirrhosis and patients with previous null response with or without cirrhosis (C-WORTHY): a randomised, open-label phase 2 trial. Lancet. 2015;385:1075–86. https://doi.org/10.1016/S0140-6736(14)61795-5.
Wilson EM, Kattakuzhy S, Sidharthan S, Sims Z, Tang L, McLaughlin M, Price A, Nelson A, Silk R, Gross C, Akoth E, Mo H, Subramanian GM, Pang PS, McHutchison JG, Osinusi A, Masur H, Kohli A, Kottilil S. Successful retreatment of chronic HCV genotype-1 infection with ledipasvir and sofosbuvir after initial short course therapy with direct-acting antiviral regimens. Clin Infect Dis. 2016;62:280–8. https://doi.org/10.1093/cid/civ874.
Stirnimann G. Ombitasvir. (ABT-267), a novel NS5A inhibitor for the treatment of hepatitis C. Expert Opin Pharmacother. 2014;15:2609–22.
Walker J, Crosby R, Wang A, Woldu E, Vamathevan J, Voitenleitner C, You S, Remlinger K, Duan M, Kazmierski W, Hamatake R. Preclinical characterization of GSK2336805, a novel inhibitor of hepatitis C virus replication that selects for resistance in NS5A. Antimicrob Agents Chemother. 2014;58:38–47. https://doi.org/10.1128/AAC.01363-13.
Gao M, Nettles RE, Belema M, Snyder LB, Nguyen VN, Fridell RA, Serrano-Wu MH, Langley DR, Sun JH, O’Boyle DR 2nd, Lemm JA, Wang C, Knipe JO, Chien C, Colonno RJ, Grasela DM, Meanwell NA, Hamann LG. Chemical genetics strategy identifies an HCV NS5A inhibitor with a potent clinical effect. Nature. 2010;465:96–100. https://doi.org/10.1038/nature08960.
Fridell RA, Qiu D, Wang C, Valera L, Gao M. Resistance analysis of the hepatitis C virus NS5A inhibitor BMS-790052 in an in vitro replicon system. Antimicrob Agents Chemother. 2010;54:3641–50.
Dvory-Sobol H, Doehle B, Svarovskaia E, et al. The prevalence of HCV NS5A nucleoside and protease inhibitor resistance associated variants and the effects on treatment with ledipasvir/sofosbuvir + RBV in the phase 3 ION study. In: International workshop on antiviral drug resistance Berlin, German; 2014.
Sulkowski M, Krishnan P, Tripathi R, et al Effect of baseline resistance-associated variants on SVR with the 3D regimen plus RBV [abstract 6LB-3113]. In: 23rd annual conference on retroviruses and opportunistic infections, CROI. Boston, Massachusetts; 2016.
Fridell RA, Wang C, Sun JH, O’Boyle DR 2nd, Nower P, Valera L, Qiu D, Roberts S, Huang X, Kienzle B, Bifano M, Nettles RE, Gao M. Genotypic and phenotypic analysis of variants resistant to hepatitis C virus nonstructural protein 5A replication complex inhibitor BMS-790052 in humans: in vitro and in vivo correlations. Hepatology. 2011;54:1924–35. https://doi.org/10.1002/hep.24594.
Curry MP, O’Leary JG, Bzowej N, et al. Sofosbuvir and velpatasvir for HCV in patients with decompensated cirrhosis. N Engl J Med. 2015;373:2618–28.
Sarrazin C, Dvory-Sobol H, Svarovskaia ES, et al. The prevalence and the effect of HCV NS5A resistance-associated variants in patients with compensated cirrhosis treated with ledipasvir/sofosbuvir ± RBV [abstract P0773]. In: The International liver congress 2015, 50th 24 annual Meeting of the European association for the Study of the Liver (EASL). Vienna, Austria: Journal of Hepatology; 2015. p. S620.
Wong KA, Worth A, Martin R, et al. Characterization of Hepatitis C virus resistance from a multiple-dose clinical trial of the novel NS5A inhibitor GS-5885. Antimicrob Agents Chemother. 2013;57:6333–40.
Hezode C, Asselah T, Reddy KR, et al. Ombitasvir plus paritaprevir plus ritonavir with or without ribavirin in treatment-naive and treatment-experienced patients with genotype 4 chronic hepatitis C virus infection (PEARL-I): a randomised, open-label trial. Lancet. 2015;385(9986):2502–9.
Wang C, Jia L, Huang H, Qiu D, Valera L, Huang X, Sun JH, Nower PT, O’Boyle DR 2nd, Gao M, Fridell RA. In vitro activity of BMS-790052 on hepatitis C virus genotype 4 NS5A. Antimicrob Agents Chemother. 2012;56:1588–90. https://doi.org/10.1128/AAC.06169-11.
Wang C, Valera L, Jia L, Kirk MJ, Gao M, Fridell RA. In vitro activity of daclatasvir on hepatitis C virus genotype 3 NS5A. Antimicrob Agents Chemother. 2013;57:611–3.
Zhou N, Han Z, Hartman NS, et al. High sustained virologic response rates in patients infected with HCV genotype 2 with baseline NS5A polymorphisms treated with daclatasvir-based regimens [abstract 234]. In: The international liver congress™ EASL—European Association for the Study of the Liver. Spain: Barcelona; 2016. p. S407.
Hernandez D, Zhou N, Ueland J, Monikowski A, McPhee F. Natural prevalence of NS5A polymorphisms in subjects infected with hepatitis C virus genotype 3 and their effects on the antiviral activity of NS5A inhibitors. J Clin Virol. 2013;57:13–18.
Lahser FC, Bystol K, Curry S, McMonagle P, Xia E, Ingravallo P, Chase R, Liu R, Black T, Hazuda D, Howe AY, Asante-Appiah E. The combination of grazoprevir, a hepatitis C virus (HCV) NS3/4A protease inhibitor, and elbasvir, an HCV NS5A inhibitor, demonstrates a high genetic barrier to resistance in HCV genotype 1a replicons. Antimicrob Agents Chemother. 2016;60:2954–64. https://doi.org/10.1128/AAC.00051-16.
Kowdley KV, Gordon SC, Reddy KR, et al. Ledipasvir and sofosbuvir for 8 or 12 weeks for chronic HCV without cirrhosis. N Engl J Med. 2014;370:1879–88.
Charlton M, Manns M, Dvory-Sobol H, et al. Resistance analyses for ledipasvir/sofosbuvir-containing regimens in patients infected with chronic HCV who have advanced liver disease or are post liver transplant (SOLAR-1 and -2 studies). In: The international liver congress™ 2016. Spain: EASL. Barcelona; 2016.
Lawitz E, Freilich B, Link J, et al. A phase 1, randomized, dose: ranging study of GS-5816, a once-daily NS5A inhibitor, in patients with genotype 1–4 hepatitis C virus. J Viral Hepat. 2015;22:1011–9.
Abergel A, Metivier S, Samuel D, et al. Ledipasvir plus sofosbuvir for 12 weeks in patients with hepatitis C genotype 4 infection. Hepatology. 2016;64:1049–1056.
Xu S, Rajyaguru S, Hebner C, et al. In vitro selection of resistance to sofosbuvir in GT 2a, 2b, 3a, 4a, 5a and 6a replicons [abstract O_01B]. In: International workshop on hepatitis C resistance and new compounds. Cambridge, USA; 2013.
Svarovskaia ES, Dvory-Sobol H, Parkin N, Hebner C, Gontcharova V, Martin R, Ouyang W, Han B, Xu S, Ku K, Chiu S, Gane E, Jacobson IM, Nelson DR, Lawitz E, Wyles DL, Bekele N, Brainard D, Symonds WT, McHutchison JG, Miller MD, Mo H. Infrequent development of resistance in genotype 1–6 hepatitis C virus-infected subjects treated with sofosbuvir in phase 2 and 3 clinical trials. Clin Infect Dis. 2014;59:1666–74. https://doi.org/10.1093/cid/ciu697.
Lemm JA, Liu M, Gentles RG, Ding M, Voss S, Pelosi LA, Wang YK, Rigat KL, Mosure KW, Bender JA, Knipe JO, Colonno R, Meanwell NA, Kadow JF, Santone KS, Roberts SB, Gao M. Preclinical characterization of BMS-791325, an allosteric inhibitor of hepatitis C Virus NS5B polymerase. Antimicrob Agents Chemother. 2014;58:3485–95.
Devogelaere B, Berke JM, Vijgen L, Dehertogh P, Fransen E, Cleiren E, van der Helm L, Nyanguile O, Tahri A, Amssoms K, Lenz O, Cummings MD, Clayton RF, Vendeville S, Raboisson P, Simmen KA, Fanning GC, Lin TI. TMC647055, a potent nonnucleoside hepatitis C virus NS5B polymerase inhibitor with cross-genotypic coverage. Antimicrob Agents Chemother. 2012;56:4676–84. https://doi.org/10.1128/AAC.00245-12.
Poordad F, Hezode C, Trinh R, Kowdley KV, Zeuzem S, Agarwal K, Shiffman ML, Wedemeyer H, Berg T, Yoshida EM, Forns X, Lovell SS, Da Silva-Tillmann B, Collins CA, Campbell AL, Podsadecki T, Bernstein B. ABT-450/r-ombitasvir and dasabuvir with ribavirin for hepatitis C with cirrhosis. N Engl J Med. 2014;370:1973–82. https://doi.org/10.1056/NEJMoa1402869.
Tong X, Le Pogam S, Li L, Haines K, Piso K, Baronas V, Yan JM, So SS, Klumpp K, Nájera I. In vivo emergence of a novel mutant L159F/L320F in the NS5B polymerase confers low-level resistance to the HCV polymerase inhibitors mericitabine and sofosbuvir. J Infect Dis. 2014;209:668–75. https://doi.org/10.1093/infdis/jit562.
Sulkowski MS, Eron JJ, Wyles D, Trinh R, Lalezari J, Wang C, Slim J, Bhatti L, Gathe J, Ruane PJ, Elion R, Bredeek F, Brennan R, Blick G, Khatri A, Gibbons K, Hu YB, Fredrick L, Schnell G, Pilot-Matias T, Tripathi R, Da Silva-Tillmann B, McGovern B, Campbell AL, Podsadecki T. Ombitasvir, paritaprevir co-dosed with ritonavir, dasabuvir, and ribavirin for hepatitis C in patients co-infected with HIV-1: a randomized trial. JAMA. 2015;313:1223–31.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to this paper with conception and design of the study, literature review and analysis, drafting and critical revision and editing, and final approval of the final version.
Corresponding author
Ethics declarations
Conflict of interest
No potential conflicts of interest. No financial support.
Rights and permissions
About this article
Cite this article
Sagnelli, E., Starace, M., Minichini, C. et al. Resistance detection and re-treatment options in hepatitis C virus-related chronic liver diseases after DAA-treatment failure. Infection 46, 761–783 (2018). https://doi.org/10.1007/s15010-018-1188-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-018-1188-3