Abstract
Purpose
Two randomized controlled trials (RCTs) showed the non-inferiority of fidaxomicin compared with vancomycin for Clostridium difficile infection (CDI) treatment and its superiority regarding recurrence rate. The aim of this study was to evaluate fidaxomicin’s efficacy in clinical practice.
Methods
This single-center prospective cohort study included hospitalized patients treated with fidaxomicin for CDI. Demographic, clinical and biological data were collected. Primary outcome was efficacy of fidaxomicin (clinical cure, recurrence and global cure) at 10 weeks. Secondary outcome was efficacy among different subgroups.
Results
Ninety-nine patients were included: 42 severe CDI, 16 complicated CDI and 41 recurrent CDI. Rates of clinical cure, recurrence and global cure were 87, 15 and 59%, respectively. Subgroup analysis showed a higher recurrence rate for patients with recurrent CDI compared with first episode (8 vs. 26%; p = 0.04). Binary toxin was associated with severe/complicated CDI (80 vs. 50%; p < 0.01) and recurrence (32 vs. 7%; p < 0.01). Fidaxomicin was used as a first line for 83% of the patients with recurrence and for only 52% of first episodes even though 86% had recurrence’s risk factors.
Conclusion
Compared with RCTs, fidaxomicin in real world is used for patients with more severe and recurrent CDI, but clinical cure and recurrence rates were similar. Comparative studies are needed in these specific subgroups. Our data also illustrate clinicians’ difficulty to define a “patient at risk for recurrence” among the first episodes. Finally, we showed that binary toxin could be important in the screening for severity and recurrence risks.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Clostridium difficile infection (CDI) is a global public health challenge with increasing incidence and severity leading to prolonged hospital stay, readmissions and increased costs [1, 2]. It is now the most common cause of health care-associated infections in the United States [3]. In Europe, incidence rose from 4.1 to 7 CDI cases per 10,000 patient-days from 2008 to 2013 [4]. There is an increasing CDI-associated mortality, especially in complicated forms [5] and CDI was assessed as an independent risk factor for mortality with a 2.5-fold increase in 30-day mortality [6]. Finally, another study in Scotland showed that mortality increased with the number of recurrence [7]. Recurrences are associated with diminished quality of life, increased mortality and costs through additional treatment and hospitalization [8–10]. It usually occurs within 2 months [11] and the major identified risk factors are advanced age, severe underlying diseases, renal failure, previous CDI, severe CDI, continued use of antibiotics, anti-acid medication and PCR-ribotype 027 strain [12–14]. Binary toxin, a toxin that impairs actin cytoskeleton in epithelial cells and enhances adherence of bacteria, is linked with higher mortality [15] and recurrence [16]. Overall, 25% of patients experience recurrence after a first episode, this percentage increase to 45 and 65% after a second and third episode, respectively [17]. The management of these multiple aspects of C. difficile infection constitutes a major therapeutic challenge.
Before 2011, antibiotic treatment for CDI was limited to metronidazole and vancomycin. However, the increasing number of reported treatment failures, particularly with metronidazole, showed the need for new therapeutic molecules [18]. Fidaxomicin, a macrocyclic antibiotic, inhibits both sporulation and toxin production of C. difficile through RNA transcription inhibition [19, 20]. Its narrow spectrum is associated to minimal effects on normal colonic microbiota [21]. Two large randomized controlled trials (RCTs), including more than 1000 patients with a first episode or a first recurrence of CDI, showed that fidaxomicin was non-inferior to vancomycin on clinical cure rate but was associated with a lower recurrence rate at 6 weeks [22, 23]. The recent revision of European Guidelines for CDI treatment includes fidaxomicin first line for (1) first episode with recurrence’s risk factor and (2) recurrence. For severe/complicated CDI, vancomycin should be favored and no evidence supports the use of fidaxomicin in case of life-threatening CDI [24]. Nevertheless, the use of fidaxomicin in clinical practice is difficult because of conflicting indications (European Guidelines or official licensing), unclear definitions of risk factors for recurrence or severe/complicated CDI, lack of evidence in multiple recurrences or complicated CDI and a high economic cost [25, 26]. The aim of this prospective study was to assess efficacy of fidaxomicin for CDI treatment in clinical practice.
Methods
Fidaxomicin has been available in Lille university hospital since November 2012 with a nominative prescription. When infectious disease (ID) stewardship was requested, fidaxomicin was proposed for non-027 CDI, non-complicated CDI, recurrent CDI, first episode with concomitant antibiotics or at least 2 recurrence risk factors and as salvage therapy.
Study design and inclusion criteria
We conducted a single-center, prospective, observational, cohort study in a 2965-bed hospital, from September 1, 2013 to September 2015. All hospitalized patients, older than 18 years, with a confirmed diagnosis of CDI and treated with fidaxomicin for more than 2 days were included. Multiple inclusions for a single patient were allowed. The study protocol was approved by our Ethical Comity (DC 2014/147) and performed in accordance with the Declaration of Helsinki. All patients provided informed consent.
Patients were identified through nominative prescription by the Pharmacy department. A study investigator validated the inclusion, collected patient’s consent and inclusion parameters. Patients were followed-up to 10 weeks (W10) after inclusion with an infectious disease consultation or a phone interview.
Definitions and microbiology
Clostridium difficile infection was defined as diarrhea (more than 3 unformed stools for at least 2 consecutive days) associated with the presence of C. difficile PCR toxin B assessed by PCR (Xpert C. difficile/Epi; Cepheid, Sunnyvale, CA). Ribotype 027 and binary toxin gene were assessed on stool sample by PCR (Xpert C. difficile/Epi; Cepheid, Sunnyvale, CA).
CDI episode was considered as (1) severe in presence of at least one CDI-attributable criteria: temperature >38.5 °C, rigors, ascites, severe sepsis, white blood cell >15,000/mm3, serum creatinine level >1.5 baseline value, albumin <30 mg/L, serum lactate >2 mmol/L, colonic distension >6 cm and pseudomembranous colitis; (2) complicated in presence of at least one CDI-attributable criteria: ICU admission, colic ileus or toxic megacolon, septic shock, serum lactate >5 mmol/L, death or surgery.
Risk factors for recurrence were age >65 years, severe underlying disease including renal impairment, concomitant antibiotics and previous CDI history.
Clinical cure was defined by resolution of diarrhea (3 or less unformed stools for at least 2 consecutive days) with no need for CDI treatment 2 days after treatment completion. Recurrence was defined as a new episode of diarrhea (without evidence for another cause), associated with the presence of toxigenic C. difficile in stool and the need for CDI treatment within 8 weeks after the onset of the previous episode. Global cure was defined as clinical cure with no recurrence. Recurrence and global cure were assessed at W6 and W10 for patients with initial clinical cure. Before W10, patients who died or underwent another CDI treatment in the absence of recurrence were labeled early withdrawals and excluded from the analysis for recurrence or global cure.
The constructed cohort included patients with complicated CDI, severe sepsis or with more than one recurrence.
Clinical outcomes
Primary outcome evaluated efficacy of fidaxomicin, including clinical cure rate at the end of treatment, recurrence and global cure at W10. Secondary outcomes were (1) efficacy among subgroups (age, severity, prior CDI, concomitant antibiotic) and in the constructed cohort; (2) impact of binary toxin on clinical forms and outcomes, and (3) mortality rate.
Data collection
A standardized form was used to collect (1) demographic characteristics such as age, sex, activity of daily living (ADL) score, medical history, prior CDI episode, Charlson comorbidity index and current treatment; (2) characteristics of the current CDI episode, including prior and concomitant antibiotics, use of other anti-CDI treatment, PCR ribotype 027 strain, presence of binary toxin and severity criteria and risk factor for recurrence.
Statistical analysis
Data are presented as percentage (confidence interval 95%) or median (interquartile range, Q1–Q3). Categorical variables were compared using either Chi square test or Fisher’s exact test when appropriate with EpiData Software. A P value less than 0.05 was considered statistically significant.
Results
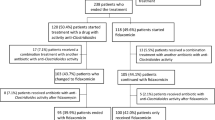
Ninety-nine episodes of fidaxomicin-treated CDI were included, representing 89 patients. Demographic and clinical characteristics of patients are summarized in Table 1. Figure 1 shows the follow-up of patients to W10 and outcomes. Eighty-six patients (87%) presented clinical cure at the end of treatment. Among the 13 patients with treatment failure, 5 had complicated CDI and 4 severe CDI. Seven experienced a first episode. Five patients died with one CDI-attributable death. The other 8 patients underwent additional anti CDI-treatment (4 fecal microbiota transplantations, 1 pulsed vancomycin regimen, 2 vancomycin/metronidazole combination therapy and 1 new fidaxomicin course). Among the 86 patients with clinical cure, 71 were assessed for recurrence and global cure. Fifteen patients were excluded from the W10 analysis because of death (13 patients) or fecal microbiota transplantations (2 patients). None of them presented criteria for recurrence. At W10, 13 patients (13/86; 15%) presented recurrence and 58 patients (58/99; 59%) achieved global cure. Recurrence occurred at a median time of 29 days [9-46] and 8 (9%) occurred before W6. Recurrences were complicated for 6 patients (4 deaths and 2 colectomies), 3 underwent fecal microbiota transplantation and 4 received a new fidaxomicin course.
Table 2 reports the clinical outcomes regarding patient subgroups. A higher recurrence rate was found for patients with at least one prior CDI episode (8 vs. 26%; p = 0.04). We also showed trends towards a lower rate of clinical cure and global cure rate for complicated CDI and higher recurrence rate for younger patients, complicated CDI and with concomitant antibiotic. Overall, mortality rate was at 22% (22 patients) but reached 44% for patients with complicated CDI. However, CDI-attributable mortality was measured at 5%. The 28 patients included in the constructed cohort presented a significantly lower global cure rate (41 vs. 66%; p = 0.04) and a trend toward a lower clinical cure rate with higher recurrence or mortality rates. The analysis of the 13 patients with a history of more than 2 recurrences showed that they all had severe underlying disease and at least 3 risk factors for recurrence. In this population, clinical cure rate was achieved for 9 patients (69%), and 33% had recurrence at W10. Finally, mortality rate reached 23% (3 patients).
Table 3 shows the outcome of 89 CDI episodes stratified on microbiological data (presence of ribotype 027 and binary toxin). Ten episodes could not be assessed because initial microbiological tests were performed in other centers. The presence of binary toxin was significantly associated with recurrence (32 vs. 7%; RR = 4.5 [95% CI 1.5 – 13.7]; p < 0.01) and with severe or complicated forms (80 vs. 50%; RR = 2.5 [95% CI 1.1–5.7]; p < 0.01). PCR-ribotype 027 positive was associated with severe or complicated CDI (100 vs. 54%; p < 0.01).
Analysis of fidaxomicin prescription showed that all patients received 200 mg bid for a median length of 10 days. Only 1 patient was given fidaxomicin in combination with another anti-CDI therapy. Overall, fidaxomicin prescription followed failure of other anti-CDI therapy for 35 (35%) patients. This rate increased to 75% for patients with a complicated episode. Fidaxomicin was used as the initial anti-CDI treatment for 30 patients with a first episode (52%) and for 34 patients with recurrences (83%). Eighty-six percent of patients with a first episode had at least one risk factor for recurrence.
Discussion
To our knowledge, this is the largest prospective cohort study assessing clinical outcomes of patients treated with fidaxomicin in real life. Our data showed a clinical cure at 87%, 15% of recurrence at W10 and a global cure rate at 59%. A significantly higher rate of recurrence was showed for patients with a previous CDI or in the presence of binary toxin. Patients with complicated CDI presented less clinical cure by the end of treatment and more recurrence at W10 but the difference did not reach a statistical significance.
This study showed major differences in population characteristics compared with RCTs [22, 23]. The main differences concerned recurrence, severity and concomitant antibiotic use, which are known to increase recurrence risk [14]. Indeed, 28% of our patients experienced a first recurrence and 13% had more than 1 recurrence compared with, respectively, 15 and 0% in RCTs [22, 23], 42% had severe CDI and 16% complicated CDI compared with, respectively, 36 and 0%. Finally, 57% of our patients received concomitant antibiotics compared with 27% in RCTs. Besides this accumulation of risk factors for recurrence, the increased follow-up period (10 weeks) could have potentially allowed the observation of more recurrences since median time for recurrence usually exceeds 4 weeks following the end of therapy [11]. Indeed, we showed a recurrence rate at 9% at W6 and 5 recurrences on 13 occurred after W6. That confirms the possible underestimation of recurrences in RCTs. Overall, our results confirm the low recurrence rate of fidaxomicin-treated CDI in clinical practice that is consistent with RCTs and retrospective cohorts on fidaxomicin [27–29]. A recent work by Feher et al. also showed in a real-world Spanish cohort that patients presented more complicated and recurrent ICD, with more concomitant antibiotic than in RCTs and found a recurrent rate at 16.7% [29].
In our study, the subgroup analysis showed a significantly higher recurrence rate in patients with previous CDI episode compared with patients with a first episode (26 vs. 8%; p = 0.04) and the 13 patients with more than 2 recurrences had a recurrence rate at 33%. These data strengthen the potential benefit of early prescription of fidaxomicin. Indeed, a recent English study found a larger reduction in recurrence and mortality when fidaxomicin was used as first-line treatment [30]. Very few data assessing fidaxomicin in multiple recurrences are available. Some prospective studies, on a small number of patients, reported successful treatment and a low rate of recurrence after fidaxomicin in this population [27, 31]. On the other hand, some authors describe clinical failures in fidaxomicin-treated patients with multiple recurrences [32, 33]. These discordant data confirm the need for large and comparative studies in this specific population to assess fidaxomicin interest.
Our study also showed a trend towards higher recurrent rate and lower clinical cure rate in patients with complicated CDI. The difference was not statistically significant probably because of the small number of patients. It is also possible that this population included more patients with a first CDI, reducing recurrence risk. This specific population had a mortality rate at 44%. Fidaxomicin is not recommended for the treatment of complicated CDI. Very few data are available and this population was excluded from the 2 RCTs [22, 23]. In our cohort, 16 patients had a complicated CDI and 75% received fidaxomicin after failure of another molecule. Complicated CDI are associated with poorer outcomes [14, 34] and the high mortality rate found in our cohort is consistent with the literature [35]. A recent study, comparing fidaxomicin efficacy between patients in critical care unit or in medical general floors, showed in multivariate analysis that severe/complicated infection was associated with a high probability of fidaxomicin failure [36]. We, lack large and comparative studies in this population to assess the benefit of fidaxomicin over other molecules or combinations. Finally, we constructed a cohort including patients with complicated or multiple CDI to observe the outcomes in all patients excluded from the RCTs [22, 23]. We found a significantly lower global cure rate at 10 weeks compared with the other group and a high mortality rate. Although the difference was not statistically significant, we observed a lower clinical cure rate and higher recurrence rate in this constructed cohort.
Our study showed a low global cure rate compared with RCTs (58 vs. 76%) [22, 23]. This is due to numerous early withdrawals with patients that could not be assessed at W10, mostly for death (13 patients) or fecal microbiota transplantation (2 patients) with no criteria for recurrence. Overall, mortality rate was at 22% with 5% of CDI-attributable mortality that is consistent with literature [37, 38]. This rate is also consistent with a US-real-world cohort on fidaxomicin [28] but not with two others that found a mortality rate below 5% with a similar rate of severe/complicated ICD [27, 29]. It is possible that patients in our cohort had more comorbidities or presented more infection with virulent strains such as ribotype-027 or binary toxin producers.
Indeed, as described in multiple publications, we found a significant association between PCR-ribotype 027 and the severity of the disease, even though it concerned only 9 patients [39]. Besides, the presence of binary toxin was also significantly associated with severe form (but not mortality) and recurrence rate. This is the first time that these associations are reported in patients receiving fidaxomicin. In the literature, the presence of binary toxin was associated with recurrence in one study from the United States including 69 patients on metronidazole or vancomycin [16]. However, the prevalence of binary toxin positive strains was considerably higher than in this study (74 vs. 29%, respectively). An association with mortality has been described in several European studies [40–42] but our study is the first to describe an association with recurrence.
Analysis of fidaxomicin prescription showed that 35% of the prescriptions followed failure of another anti-CDI treatment, as a salvage therapy. It concerned 75% of patients with complicated episode, which is concordant with the guidelines, since fidaxomicin is not recommended in this indication [24]. Half of patients with a first episode received fidaxomicin as salvage therapy, even though 86% had recurrence risk factors and 86% of patients with recurrent CDI received fidaxomicin as a first line therapy. Overall, it illustrates the difficulties to place fidaxomicin among first episode and to define recurrence risk factors. Clinicians seemed more confident with fidaxomicin’s benefit in recurrent CDI. This could be due to unawareness of the molecule and to cost issues. Nevertheless, several European or North American studies showed with analytic model the cost-effectiveness of fidaxomicin in first CDI with risk factor for recurrence or first recurrence [43–45].
Our study presents several limitations. First of all, this is a single-center study, therefore, limiting a potential extrapolation to other center or country. Although 99 patients were prospectively included in our cohort, we could not show significant differences in several subgroups that are known to be associated with poorer outcomes. This lack of power limits the interpretation of fidaxomicin’s effectiveness in specific subgroups and is increased by numerous early withdrawals (mostly because of a high mortality rate in this cohort) with only 71 analyzed episodes at W10. Inclusion of more patients might also have allowed us to perform multivariate analyses. Second, we did not include a comparative group that could have allowed us to suggest a potential benefit of fidaxomin in subgroups with poor outcomes. This study also presents microbiological limitation with detection of toxigenic C. difficile by molecular assay instead of culture and use of a “one step” diagnostic strategy in our center. Indeed, considering the low sensitivity of IEA in detecting toxin, the CDI diagnosis was retained with a strict definition of diarrhea (number and consistency using the Bristol stool chart) associated with a positive PCR toxin. We potentially have a risk to include patients with colonization and diarrhea of other causes and skew the results [46, 47]. Moreover, the presumptive identification of PCR-ribotype 027 was conducted using the Xpert C. difficile Epi assay that had been associated with false-positive results [48].
In conclusion, our study showed that CDI management in clinical practice involves many patients with severe and recurrent disease. Overall, fidaxomicin treatment was associated with similar clinical cure and recurrence rates at W10 than those described in RCTs. However, we showed a significantly higher recurrence rate for patients with 1 or more recurrence. This suggests a greater benefit of an early use of fidaxomicin and comparative studies are needed for treatment of patients with multiple recurrences. We also demonstrate the difficulties encountered by clinicians to prescribe fidaxomicin for a first CDI and the need for clear definitions of patients with a high risk of recurrence. Finally, we found an association between binary toxin and recurrence. This is described for the first time in Europe and needs to be further confirmed.
References
Lessa FC, Mu Y, Bamberg WM, et al. Burden of Clostridium difficile infection in the United States. N Engl J Med. 2015;372:825–34.
Wiegand PN, Nathwani D, Wilcox MH, Stephens J, Shelbaya A, Haider S. Clinical and economic burden of Clostridium difficile infection in Europe: a systematic review of healthcare-facility-acquired infection. J Hosp Infect. 2012;81:1–14.
Magill SS, Edwards JR, Bamberg W, et al. Multistate point-prevalence survey of health care-associated infections. N Engl J Med. 2014;370:1198–208.
Davies KA, Longshaw CM, Davis GL, et al. Underdiagnosis of Clostridium difficile across Europe: the European, multicentre, prospective, biannual, point-prevalence study of Clostridium difficile infection in hospitalised patients with diarrhoea (EUCLID). Lancet Infect Dis. 2014;14:1208–19.
Ferrer Márquez M, Hernández Martínez Á, Reina Duarte Á, Rosado Cobián R. Current status of the treatment of fulminant colitis. Cir Esp. 2015;93:276-82.
Hensgens MPM, Dekkers OM, Goorhuis A, LeCessie S, Kuijper EJ. Predicting a complicated course of Clostridium difficile infection at the bedside. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis. 2014;20:O301–8.
Taori SK, Wroe A, Poxton IR. Clostridium difficile infections in South East Scotland: mortality and recurrence in a region without PCR ribotype 027. J Med Microbiol. 2013;62:1468–77.
Le Monnier A, Duburcq A, Zahar J-R, et al. Hospital cost of Clostridium difficile infection including the contribution of recurrences in French acute-care hospitals. Infect: J Hosp; 2015.
Olsen MA, Yan Y, Reske KA, Zilberberg MD, Dubberke ER. Recurrent Clostridium difficile infection is associated with increased mortality. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis. 2015;21:164–70.
Sheitoyan-Pesant C, Abou Chakra CN, Pépin J, Marcil-Héguy A, Nault V, Valiquette L. Clinical and healthcare burden of multiple recurrences of Clostridium difficile infection. Clin Infect Dis Off Publ Infect Dis Soc Am. 2016;62:574–80.
Barbut F, Richard A, Hamadi K, Chomette V, Burghoffer B, Petit JC. Epidemiology of recurrences or reinfections of Clostridium difficile-associated diarrhea. J Clin Microbiol. 2000;38:2386–8.
Deshpande A, Pasupuleti V, Thota P, et al. Risk factors for recurrent Clostridium difficile infection: a systematic review and meta-analysis. Infect Control Hosp Epidemiol. 2015;36:452–60.
D’Agostino RB, Collins SH, Pencina KM, Kean Y, Gorbach S. Risk estimation for recurrent Clostridium difficile infection based on clinical factors. Clin Infect Dis Off Publ Infect Dis Soc Am. 2014;58:1386–93.
Abou Chakra CN, Pepin J, Sirard S, Valiquette L. Risk factors for recurrence, complications and mortality in Clostridium difficile infection: a systematic review. PLoS One. 2014;9:e98400.
Bacci S, Mølbak K, Kjeldsen MK, Olsen KEP. Binary toxin and death after Clostridium difficile infection. Emerg Infect Dis. 2011;17:976–82.
Stewart DB, Berg A, Hegarty J. Predicting recurrence of C. difficile colitis using bacterial virulence factors: binary toxin is the key. J Gastrointest Surg Off J Soc Surg Aliment Tract. 2013;17:118–24 (discussion 124–125).
Kelly CP. Can we identify patients at high risk of recurrent Clostridium difficile infection? Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis. 2012;18:21–7.
Zar FA, Bakkanagari SR, Moorthi KMLST, Davis MB. A comparison of vancomycin and metronidazole for the treatment of Clostridium difficile-associated diarrhea, stratified by disease severity. Clin Infect Dis Off Publ Infect Dis Soc Am. 2007;45:302–7.
Babakhani F, Bouillaut L, Gomez A, Sears P, Nguyen L, Sonenshein AL. Fidaxomicin inhibits spore production in Clostridium difficile. Clin Infect Dis Off Publ Infect Dis Soc Am. 2012;55:S162–9.
Babakhani F, Gomez A, Robert N, Sears P. Killing kinetics of fidaxomicin and its major metabolite, OP-1118, against Clostridium difficile. J Med Microbiol. 2011;60:1213–7.
Louie TJ, Cannon K, Byrne B, et al. Fidaxomicin preserves the intestinal microbiome during and after treatment of Clostridium difficile infection (CDI) and reduces both toxin reexpression and recurrence of CDI. Clin Infect Dis Off Publ Infect Dis Soc Am. 2012;55:S132–42.
Cornely OA, Crook DW, Esposito R, et al. Fidaxomicin versus vancomycin for infection with Clostridium difficile in Europe, Canada, and the USA: a double-blind, non-inferiority, randomised controlled trial. Lancet Infect Dis. 2012;12:281–9.
Louie TJ, Miller MA, Mullane KM, et al. Fidaxomicin versus vancomycin for Clostridium difficile infection. N Engl J Med. 2011;364:422–31.
Debast SB, Bauer MP, Kuijper EJ. Committee. European Society of Clinical Microbiology and Infectious Diseases: update of the treatment guidance document for Clostridium difficile infection. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis. 2014;20:1–26.
Khanafer N, Barbut F, Eckert C, et al. Factors predictive of severe Clostridium difficile infection depend on the definition used. Anaerobe. 2016;37:43–8.
Jacobson SM, Slain D. Evaluation of a bedside scoring system for predicting clinical cure and recurrence of Clostridium difficile infections. Am J Health Syst Pharm AJHP Off J Am Soc Health Syst Pharm. 2015;72:1871–5.
Eiland EH, Sawyer AJ, Massie NL. Fidaxomicin use and clinical outcomes for Clostridium difficile-associated diarrhea. Infect Dis Clin. Pract Baltim Md. 2015;23:32–5.
Vargo CA, Bauer KA, Mangino JE, Johnston JEW, Goff DA. An antimicrobial stewardship program’s real-world experience with fidaxomicin for treatment of Clostridium difficile infection: a case series. Pharmacotherapy. 2014;34:901-9.
Fehér C, Múñez Rubio E, Merino Amador P, et al. The efficacy of fidaxomicin in the treatment of Clostridium difficile infection in a real-world clinical setting: a Spanish multi-centre retrospective cohort. Eur J Clin Microbiol Infect Dis. 2016. [Epub ahead of print].
Goldenberg SD, Brown S, Edwards L, et al. The impact of the introduction of fidaxomicin on the management of Clostridium difficile infection in seven NHS secondary care hospitals in England: a series of local service evaluations. Eur J Clin Microbiol Infect Dis Off Publ Eur Soc Clin Microbiol. 2016;35:251–9.
Esmaily-Fard A, Tverdek FP, Crowther DM, Ghantoji SS, Adachi JA, Chemaly RF. The use of fidaxomicin for treatment of relapsed Clostridium difficile infections in patients with cancer. Pharmacotherapy. 2014;34:1220-5.
Orenstein R. Fidaxomicin failures in recurrent Clostridium difficile infection: a problem of timing. Clin Infect Dis Off Publ Infect Dis Soc Am. 2012;55:613–4.
Johnson S, Gerding DN. Fidaxomicin ‘chaser’ regimen following vancomycin for patients with multiple Clostridium difficile recurrences. Clin Infect Dis Off Publ Infect Dis Soc Am. 2013;56:309–10.
Hu MY, Katchar K, Kyne L, et al. Prospective derivation and validation of a clinical prediction rule for recurrent Clostridium difficile infection. Gastroenterology. 2009;136:1206–14.
Sailhamer EA, Carson K, Chang Y, et al. Fulminant Clostridium difficile colitis: patterns of care and predictors of mortality. Arch Surg. 2009;144:433–9 (discussion 439–440).
Penziner S, Dubrovskaya Y, Press R, Safdar A. Fidaxomicin therapy in critically ill patients with Clostridium difficile infection. Antimicrob Agents Chemother. 2015;59:1776–81.
van Kleef E, Green N, Goldenberg SD, et al. Excess length of stay and mortality due to Clostridium difficile infection: a multi-state modelling approach. J Hosp Infect. 2014;88:213–7.
Dubberke ER, Butler AM, Reske KA, et al. Attributable outcomes of endemic Clostridium difficile-associated disease in nonsurgical patients. Emerg Infect Dis. 2008;14:1031–8.
Pépin J, Valiquette L, Cossette B. Mortality attributable to nosocomial Clostridium difficile-associated disease during an epidemic caused by a hypervirulent strain in Quebec. CMAJ Can Med Assoc J J Assoc Med Can. 2005;173:1037–42.
Reigadas E, Alcalá L, Marín M, Martín A, Iglesias C, Bouza E. Role of binary toxin in the outcome of Clostridium difficile infection in a non-027 ribotype setting. Epidemiol Infect. 2016;144:268–73.
Pilate T, Verhaegen J, Van Ranst M, Saegeman V. Binary toxin and its clinical importance in Clostridium difficile infection, Belgium. Eur J Clin Microbiol Infect Dis Off Publ Eur Soc Clin Microbiol. 2016;35:1741–7.
Goldenberg SD, French GL. Lack of association of tcdC type and binary toxin status with disease severity and outcome in toxigenic Clostridium difficile. J Infect. 2011;62:355–62.
Watt M, McCrea C, Johal S, Posnett J, Nazir J. A cost-effectiveness and budget impact analysis of first-line fidaxomicin for patients with Clostridium difficile infection (CDI) in Germany. Infection. 2016;44:599–606.
Nathwani D, Cornely OA, Van Engen AK, Odufowora-Sita O, Retsa P, Odeyemi IAO. Cost-effectiveness analysis of fidaxomicin versus vancomycin in Clostridium difficile infection. J Antimicrob Chemother. 2014;69:2901–12.
Rubio-Terrés C, Cobo Reinoso J, Grau Cerrato S, et al. Economic assessment of fidaxomicin for the treatment of Clostridium difficile infection (CDI) in special populations (patients with cancer, concomitant antibiotic treatment or renal impairment) in Spain. Eur J Clin Microbiol Infect Dis Off Publ Eur Soc Clin Microbiol. 2015;34:2213–23.
Planche TD, Davies KA, Coen PG, et al. Differences in outcome according to Clostridium difficile testing method: a prospective multicentre diagnostic validation study of C difficile infection. Lancet Infect Dis. 2013;13:936–45.
Polage CR, Gyorke CE, Kennedy MA, et al. Overdiagnosis of Clostridium difficile infection in the molecular test era. JAMA Intern Med. 2015;175:1792–801.
Kok J, Wang Q, Thomas LC, Gilbert GL. Presumptive identification of Clostridium difficile strain 027/NAP1/BI on Cepheid Xpert: interpret with caution. J Clin Microbiol. 2011;49:3719–21.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors decline conflicts of interest regarding this work and did not receive external funding.
Additional information
Marie Pichenot and Rozenn Héquette-Ruz equally contributed to the study.
Rights and permissions
About this article
Cite this article
Pichenot, M., Héquette-Ruz, R., Le Guern, R. et al. Fidaxomicin for treatment of Clostridium difficile infection in clinical practice: a prospective cohort study in a French University Hospital. Infection 45, 425–431 (2017). https://doi.org/10.1007/s15010-017-0981-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-017-0981-8