Abstract
Purpose
To examine patterns of outpatient and community antibiotic use among adults in five European countries.
Methods
We used healthcare data of 28.8 million adults from six population-based ARITMO project databases to ascertain information on systemic antibiotic use in Denmark (2000–2008), the Netherlands (1999–2010), Italy (2000–2010), the UK (1996–2009), and Germany (2004–2008). We estimated overall, and age-group and sex specific antibiotic use as defined daily doses (DDD) per 1000 inhabitants per day. We computed annual age- and sex-standardized population prevalence of antibiotic use per 1000 persons-years (p-y) and the mean duration (in days) of antibiotic use.
Results
The overall antibiotic use varied from 8.7 DDD per 1000 inhabitants per day in the UK to 18.1 DDD in Denmark, representing a 2.1-fold geographical variation. In all countries, prescribing was relatively high among individuals aged 15–19 years; lower in those aged 20–50 years; and then increased steadily reaching 41.8 DDD per 1000 inhabitants per day in individuals ≥85 years in Denmark. After age- and sex-standardization, prevalence of antibiotic use varied threefold from 160.2/1000 p-y in the UK to 421.1/1000 p-y in Italy. The ratio of broad- to narrow-spectrum penicillin, cephalosporin, and macrolide use varied from 0.6 in Denmark to 120.2 in Italy. Women used more antibiotics than men did in all countries. Across countries, the mean duration of antibiotic use varied 1.3 to 21.1-fold for different antibiotics.
Conclusions
Antibiotic use is high in women and the elderly. Prescribing patterns vary substantially across European countries, both according to overall consumption, user prevalence, duration, and narrow- versus broad-spectrum antibiotics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Antibiotic resistance driven by selective pressure from both appropriate and inappropriate use of antibiotics is an evolving public health crisis and a potential threat to future healthcare delivery [1, 2]. The European Centre for Disease Control (ECDC) recently estimated that 25,000 deaths per year within Europe are directly related to antibiotic resistance [3]. Therefore, data on antibiotic use is vital to identify priority areas for interventions to optimize antibiotic use.
The European Surveillance of Antimicrobial Consumption Network (ESAC-Net) program has documented a 3.1-fold variation in antibiotic use between countries with the highest use [35.1 defined daily doses (DDD) per 1000 inhabitants per day in Greece] and the country with the lowest use (11.4 DDD per 1000 inhabitants per day in the Netherlands) in 2011 [4]. Striking geographical variation was observed not only for overall prescription but also for use of various specific antibiotic subgroups including quinolones, macrolides, penicillins, and cephalosporins [5, 6]. ESAC-net presents aggregated measures on antibiotic use according to DDD per 1000 inhabitants per day and as packages per 1000 inhabitants per day (PID) that are based on DDDs, which is a parameter that does not necessarily reflect the prescribed daily dose. Additionally, ESAC-net does not provide patient-level information, such as number of patients treated in the population, age and sex distribution, and duration of treatment, which is necessary to identify target groups for intervention to improve prudent use of antibiotics. Therefore, to fill this gap, we utilized data from the EU funded “Arrhythmogenic potential of drugs (ARITMO)” project (www.aritmo-project.org). For the overall antibiotics and for each antibiotic subgroup and chemical substance, separately, we measured and compared across five European Countries: (1) the volume (expressed as DDD per 1000 inhabitants per day) of antibiotics used in the community, (2) the annual population prevalence of antibiotic use; and (3) the mean duration of antibiotic use.
Methods
Data sources and setting
ARITMO is a collaborative project started in 2010 and funded by the European Commission under the VII Framework Programme (Grant agreement number: HEALTH 241679). The overall objective of ARITMO was to analyze the arrhythmogenic potential of antihistamines, antipsychotics and anti-infectives, including antibiotics. The ARITMO project combines anonymized electronic healthcare records data of about 30 million individuals from six population-based databases of five European countries. The databases included in the project are, the PHARMO research database from the Netherlands; Aarhus University Hospital (AUH) database from Denmark; the German Pharmacoepidemiological Research Database (GePaRD) from Germany; the health improvement network (THIN) database from the United Kingdom (UK); and the Health Search/Longitudinal Patients Database (HSD) and Emilia-Romagna regional database (ERD) from Italy. The HSD [7, 8] and THIN databases [9, 10] are general practice databases documenting clinical information and drug prescriptions. The information is gathered and transferred by selected and trained practitioners from all over Italy and the UK. The PHARMO and GePaRD are claims and record linkage databases collecting information on drug dispensing. The PHARMO database collects information from the entire population of 65 municipalities in the Netherlands, whereas GePaRD gathers information from four national statutory health insurance providers. The AUH and ERD are population-based record linkage registries and cover the entire population of the respective geographical regions of Denmark and Italy. Table 1 shows an overview of the contributing databases. Data from the individual databases were extracted locally using a common pre-specified data model and thereafter elaborated using a dedicated software Jerboa which allowed anonymization and aggregation of data [11]. Data were ultimately sent in encrypted format, for data protection reasons, to a central repository managed by the Department of Medical Informatics at Erasmus Medical Center in the Netherlands for further evaluation and analyses. All databases obeyed the European Union guidelines on the usage of medical data for research. The study was given approval by regulatory agencies or by scientific and ethical advisory boards of the databases where applicable. The whole process of data extraction, quality check and analyses when combining multiple databases has been in depth described elsewhere [12].
Study population and study period
We included all persons aged 15 years or above from the source population who were registered in the databases during the study period. The study duration varied across databases and ranged from 1996 through 2010, as summarized in Table 1. We defined the eligibility period for each patient as starting 1 year after the date of registration in the database and ending on the date of last supply of data, death, or December 31, 2010, whichever came first.
Data on antibiotic use
Data on outpatient and community antibiotic prescription and dispensation were collected from different databases and used as a proxy for antibiotic use. Data on antibiotic use were aggregated at the level of the active chemical substance, using the Anatomical Therapeutic Chemical (ATC) classification and the DDD measurement unit (WHO, version 2011) [13]. From each database we retrieved information on date of prescription or dispensing (if both dates were available we used the date of dispensing), total quantity of the active principle in each prescription, DDD-value, number of units per prescription, strength per unit, number of prescribed units per day (if available), and total number of DDD for each prescription/dispensing.
Statistical analysis
We computed volume of antibiotic use as DDDs per 1000 inhabitants per day. Inhabitants per day were calculated as: total person-days observed in each database divided by 1000. We computed sex and age-group stratified volume of antibiotic use for each database. To compare antibiotic use across the participating countries, we standardized the estimates to age and sex according to the EUR27 standard population for the year 2004 (http://epp.eurostat.ec.europa.eu/portal/page/portal/statistics/search_database).
Furthermore, we computed the annual age- and sex-standardized population prevalence of antibiotic use according to ATC 4th level (antibiotic subgroup) and ATC 5th level (antibiotic chemical substance). We presented annual prevalence per 1000 person-years calculated as the number of individuals who received at least one antibiotic prescription/dispensing divided by the total cumulated person time in the observation year and multiplied by 1000. We then repeated the analyses for broad- and narrow-spectrum antibiotics, separately. Broad spectrum antibiotics included broad-spectrum penicillins (ATC code: J01CR+J01CA), cephalosporins (ATC code: J01DC+J01DD), and macrolides (ATC code: all J01F except J01FA01). Narrow spectrum antibiotics included narrow-spectrum penicillins (ATC code: J01CE+J01CF), cephalosporins (ATC code: J01DB), and macrolides (ATC code: J01FA01). We also computed sex and age-group stratified annual prevalence of antibiotic use per 1000 person-years for each database. Additionally, we calculated the mean duration of antibiotic use per prescription/dispensing at the ATC 4th level and ATC 5th level. We calculated mean days of antibiotic use per prescription/dispensing by adding the total days of antibiotic exposure (ATC 4th level and ATC 5th level) divided by the total number of prescriptions retrieved.
Results
Volume of antibiotic use in the community
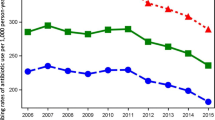
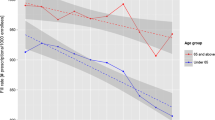
Antibiotic use ranged from 8.7 DDD per 1000 inhabitants per day in the UK to 18.1 DDD per 1000 inhabitants per day in Denmark, representing a 2.1-fold variation. The consumption was 9.4 DDD per 1000 inhabitants per day in the Netherlands, 13.7 DDD per 1000 inhabitants per day in Germany, and 13.9–16.7 DDD per 1000 inhabitants per day in Italy. The age- and sex-standardized annual use of antibiotics increased steadily over time in Denmark (from 10.3 to 14.4 DDD per 1000 inhabitants per day), the Netherlands (from 6.7 to 8.6 DDD per 1000 inhabitants per day), the UK (from 5.3 to 8.1 DDD per 1000 inhabitants per day), and Germany (from 11.2 to 11.6 DDD per 1000 inhabitants per day). In Italy antibiotic use increased up to 2006 (from 6.1 to 11.5 DDD per 1000 inhabitants per day) followed by a decrease (from 14.8 to 11.9 DDD per 1000 inhabitants per day in the ERD database, and from 12.9 to 11.5 DDD per 1000 inhabitants per day in the HSD database) (Fig. 1). In all countries, antibiotic use was relatively high among individuals aged 15–19 years, lower at a stable level among individuals aged 20–50 years, and then increased steadily with age (Table 4 in the “Appendix”). In particular, there was more than a 3.1-fold increase with age in Denmark, from 13.5 DDD per 1000 inhabitants per day in individuals aged 50–54 years to 41.8 DDD per 1000 inhabitants per day in individuals ≥85 years. The antibiotic use was substantially lower among the elderly in the other countries. Stratifying by sex revealed a higher antibiotic use among women compared to men in all age-groups, except among individuals older than 70 years in Italy where use was higher in men compared with women (Fig. 2).
Annual trends in the age- and sex-standardized antibiotic use as DDDs per 1000 inhabitants per day among participating countries. DDDs defined daily doses, DID DDD per 1000 inhabitants per day, AUH Aarhus University Hospital, ERD Emilia-Romagna regional database, HSD Health Search Database, GePaRD German Pharmacoepidemiological Research Database, THIN The Health improvement network
Volume of antibiotic use as DDDs per 1000 inhabitants per day by country and age-groups in women (left) and men (right). DDDs defined daily doses, DID DDD per 1000 inhabitants per day, AUH Aarhus University Hospital, ERD Emilia-Romagna regional database, HSD Health Search Database, GePaRD German Pharmacoepidemiological Research Database, THIN The Health improvement network
Population prevalence of antibiotic use
The age- and sex-standardized annual prevalence of antibiotic use varied from 160.2/1000 person-years in the UK to 421.1/1000 person-years in the Emilia-Romagna region of Italy, equivalent to a threefold variation (Table 2). The most frequently used subgroups were beta lactamase sensitive penicillins in Denmark (161.9/1000 person-years), penicillin combinations including beta lactamase inhibitors in Italy (77.1–94.7/1000 person-years), tetracycline in the Netherlands (52.9/1000 person-years), beta-lactamase resistant penicillins in the UK (34.2/1000 person-years), and macrolides in Germany (72.3/1000 person-years) (Fig. 3). Antibiotics used for intestinal infections (ATC code: A07AA) were relatively frequent in Italy (24.2–25.6/1000 person-years) while the prevalence accounted for less than 4/1000 person-years in the other countries.
Distribution of mean annual prevalence of antibiotic use at ATC group level 3 in the five participating countries. *Others: other J01 codes, A07AA, A02BD, J04AB, J04AC, J04AD, J04AK, J04AM, G01AA, R02AB. AUH Aarhus University Hospital, ERD Emilia-Romagna regional database, HSD Health Search Database, GePaRD German Pharmacoepidemiological Research Database, THIN The Health improvement network, UK the United Kingdom
The annual prevalence of individual chemical substances also varied widely among participating countries (Table 5 in the “Appendix”). Highest age- and sex-standardized prevalences were found for phenoxymethylpenicillin in Denmark (161.9/1000 person-years), amoxicillin with clavulanic acid in Italy (75.9–94.3/1000 person-years), doxycycline in the Netherlands (49.3/1000 person-years), amoxicillin in Germany (47.8/1000 person-years), and flucloxacillin in the UK (34.2/1000 person-years) (Table 5 in the “Appendix”). Dicloxacillin, sufamethizole, pivmecillinam, and pivampicillin were widely used in Denmark but not in the other countries or with a very low prevalence in the UK, respectively.
In Denmark and the UK narrow-spectrum penicillin, cephalosporin, and macrolides were more commonly prescribed than broad-spectrum penicillin, cephalosporin, and macrolides. Whereas in Germany, Italy and the Netherlands broad-spectrum penicillin, cephalosporin, and macrolides were more frequently prescribed than narrow-spectrum counterparts (Fig. 4). The ratio of broad- to narrow-spectrum penicillin, cephalosporin, and macrolides varied from 0.60 in Denmark to 102.18 in Italy (HSD). The ratio was 4.94 in Germany, 69.78 in the Emilia-Romagna region of Italy (ERD), and 3.99 in the Netherlands.
Annual prevalence of broad- and narrow-spectrum penicillin, cephalosporin, and macrolides use at ATC group level 3 in the five participating countries. AUH Aarhus University Hospital, ERD Emilia-Romagna regional database, HSD Health Search Database, GePaRD German Pharmacoepidemiological Research Database, THIN The Health improvement network, UK the United Kingdom
After stratifying by age and sex, we observed a relatively higher prevalence of antibiotic use in individuals aged 15–19 years. The annual prevalence was lower at a stable level in individuals aged 20–44 years and increased steadily with age in individuals over 45 years of age until 79 years in all countries, and varied thereafter (Fig. 5 in the “Appendix”). This pattern was similar for men and women, but annual prevalence was highest for women in all countries (Fig. 6 in the “Appendix”).
Duration of antibiotic treatment
Mean duration of antibiotic use varied for all antibiotic subgroups among the five countries (Table 3). The lowest variation in duration was observed for macrolides (J01FA) with a 1.3-fold variation between countries with the shortest and longest duration of use, respectively, (6.7 days in Germany versus 8.8 days in Denmark). In comparison, the greatest variation was a 21.1-fold variation in the duration of use of aminoglycosides other than streptomycin (J01GB) [2.3 days in Italy (HSD) versus 47.7 days in Denmark]. The duration of antibiotic use also varied greatly for individual antibiotic substances across the five participating countries (Table 6 in the “Appendix”).
Discussion
This population-based study of 28.8 million people covered by six databases of five European countries identified substantial variations in the use of antibiotics from 8.7 DDD per 1000 inhabitants per day in the UK to 18.1 DDD per 1000 inhabitants per day in Denmark. The overall use increased with age over 20 years in all countries but most markedly in Denmark. The overall age- and sex-standardized prevalence of antibiotic use varied from 160/1000 person-years in the UK to 421/1000 person-years in the Emilia-Romagna region of Italy with large variations in the use of individual antibiotic subgroups. Denmark and the UK prescribed more narrow-spectrum antibiotics whereas broad-spectrum penicillin, cephalosporin, and macrolides were used more frequently than narrow-spectrum counterparts in the Netherlands, Germany and mostly in Italy. Antibiotic use was relatively higher among women compared with men. Additionally, we observed substantial variation in the mean duration of antibiotic use among the participating countries.
The ESAC-Net project recently documented a 3.5 fold variation in antibiotic use among 26 European countries [14]. Our study extends these findings by including results for antibiotic subgroups and individual chemical substances and enhances comparability by providing age and sex standardized results. Additionally, we provide information on demographic characteristics of antibiotic users in the participating countries. Our finding of an increasing use with age in Denmark and the UK are of the same magnitude as observed in a previous study comparing antibiotic utilization in Denmark and Italy [15]. Additionally, a recent Swedish study reported higher antibiotic use among individuals aged ≥65 years old (556/1000 inhabitants) compared with individuals aged 40–65 years (339/1000 inhabitants) [16]. Other prior studies have also shown wide variations in community antibiotic use both between [14] and within [17] countries.
Higher antibiotic use in some settings does not necessarily indicate inappropriate prescribing but may relate to differences in disease occurrence. Differences in healthcare systems including the number of GPs in a country [18], antibiotic dosage regimens, guidelines, patient expectation and attitude toward taking medications, cultural and social factors, source of information available to the GPs, and knowledge of the GPs [19, 20] also play a role. For example, the longer duration of aminoglycosides use observed in Denmark despite its low overall consumption is likely because it is it is indicated for haematological cases for longer duration and as a prophylactic drug after intra-abdominal surgeries and prescribed for weeks [21]. The Social and Cultural Planning Office of The Netherlands have reported that countries with a more egalitarian society (The Netherlands, the UK, Scandinavia) have a much lower level of medication use than countries with a hierarchical society (France, Italy, Spain, Portugal, etc.) [22]. Thus, it is possible to reduce community antibiotic use, as the observed variations are explained by multiple factors rather than mere differences in disease incidence, severity, etiology, or different demographics [23–26]. For example, implementation of antibiotic stewardship program in Sweden significantly reduced the outpatient antibiotic use [27]. Similarly, the marked decrease in the antibiotic use in the Emilia-Romagna region of Italy as reported in our results might be the result of informative campaigns and adoption of effective treatment guidelines by the region.
Our study is a sub-study of the ARITMO project that combined electronic health records from five European countries to build a unique dataset to study several outcomes. The databases included in ARITMO are compliant with the anonymity, European directives, national data regulations and database governance rules. Local experts from each of the participating countries were involved in the project to maximize the efficiency and to deal effectively with methodological, cultural, ethical, governance and political issues of sharing data out of the country.
Our study extends prior studies by providing information on prescription prevalence and duration of antibiotic use. We used the ATC classification system and DDD measurement units, developed by the WHO collaborating center for drug statistics methodology. The DDD is the assumed average maintenance dose per day for a drug used for its main indication in adults [13] and only gives a rough estimate of the drug used. Thus, actual doses of drug may differ from DDD and are usually based on patient factors (age, weight, severity of disease etc.). This might have contributed to the observed variation across the countries. However, as Monnet et al. [28] reported the number of DDD may indicate the number of prescriptions for outpatients at the national level. We used reimbursement data, thereby excluding drugs that were sold over-the-counter, which may underestimate the actual use of drugs. However, a questionnaire survey among EU member states found that only 2–3 % of survey participants obtained antibiotics without a prescription [29], so we believe any underestimation is likely to be negligible. Caution should be taken when interpreting our findings because the results are based on sections of a population. However, we believe that the source population of most databases is representative of the whole population, except for the data from the Emilia-Romagna region of Italy. Results for Italy cannot be directly generalized due to substantial differences in regional prescribing patterns, and we assume that the results for Italy are underestimated due to the sale of antibiotics without prescription [30]. Finally, the slightly different time-frames of our available data should be kept in mind when comparing countries. To address this we provide the time-trends for each database and report standardized estimates.
In conclusion, this study observed considerable differences in the amount of antibiotic use and the user prevalence across Europe. Antibiotics are mostly prescribed to people younger than 20 years or older than 50 years, and to women. The ratio of broad- to narrow-spectrum penicillin, cephalosporin, and macrolides seems to be lowest in Denmark and the UK, and was high for Germany, the Netherlands, and to a much greater extent in Italy. Further population-based studies are warranted to understand the mechanism behind the differences in antibiotic use pattern. Understanding the determinants of antibiotic use may help to frame a targeted approach to reduce antibiotic use, which is urgently needed to halt the emerging antibiotic resistance.
References
The European Centre for Disease Prevention and Control (ECDC). Antimicrobial resistance surveillance in Europe: annual report of the European Antimicrobial Resistance Surveillance Network (EARS-Net). 2013. http://www.ecdc.europa.eu/en/publications/Publications/antimicrobial-resistance-surveillance-europe-2012.pdf. Accessed 21 Nov 2014.
World Health Organization 2014. Antimicrobial resistance: global report on surveillance. 2014. http://apps.who.int/iris/bitstream/10665/112642/1/9789241564748_eng.pdf?ua=1. Accessed 23 June 2014.
European Centre for Disease Prevention and Control. European Medicines Agency. The bacterial challenge: time to react. 2009. http://www.ecdc.europa.eu/en/publications/Publications/0909_TER_The_Bacterial_Challenge_Time_to_React.pdf. Accessed 20 Jan 2014.
European Centre for Disease Prevention and Control. Surveillance of antimicrobial consumption in Europe 2011. Stockholm: ECDC; 2014. http://www.ecdc.europa.eu/en/publications/Publications/antimicrobial-consumption-europe-surveillance-2011.pdf. Accessed 21 Nov 2014.
Versporten A, Coenen S, Adriaenssens N, Muller A, Minalu G, Faes C, et al. European Surveillance of Antimicrobial Consumption (ESAC): outpatient cephalosporin use in Europe (1997–2009). J Antimicrob Chemother. 2011;66:vi25–35.
Coenen S, Adriaenssens N, Versporten A, Muller A, Minalu G, Faes C, et al. European Surveillance of Antimicrobial Consumption (ESAC): outpatient use of tetracyclines, sulphonamides and trimethoprim, and other antibacterials in Europe (1997–2009). J Antimicrob Chemother. 2011;66:vi57–70.
Sacchetti E, Trifiro G, Caputi A, Turrina C, Spina E, Cricelli C, et al. Risk of stroke with typical and atypical anti-psychotics: a retrospective cohort study including unexposed subjects. J Psychopharmacol. 2008;22:39–46.
Mazzaglia G, Mantovani LG, Sturkenboom MC, Filippi A, Trifiro G, Cricelli C, et al. Patterns of persistence with antihypertensive medications in newly diagnosed hypertensive patients in Italy: a retrospective cohort study in primary care. J Hypertens. 2005;23:2093–100.
Bourke A, Dattani H, Robinson M. Feasibility study and methodology to create a quality-evaluated database of primary care data. Inform Prim Care. 2004;12:171–7.
Grant RL, Drennan VM, Rait G, Petersen I, Iliffe S. First diagnosis and management of incontinence in older people with and without dementia in primary care: a cohort study using the health improvement network primary care database. PLoS Med. 2013;10(8):e1001505.
Coloma PM, Schuemie MJ, Trifiro G, Gini R, Herings R, Hippisley-Cox J, et al. Combining electronic healthcare databases in Europe to allow for large-scale drug safety monitoring: the EU-ADR Project. Pharmacoepidemiol Drug Saf. 2011;20(1):1–11.
Trifiro G, Coloma PM, Rijnbeek PR, Romio S, Mosseveld B, Weibel D, et al. Combining multiple healthcare databases for postmarketing drug and vaccine safety surveillance: why and how? J Intern Med. 2014;275(6):551–61.
WHO Collaborating Centre for Drug Statistics Methodology. Anatomical Therapeutic Chemical (ATC) Classification System: Guidelines for ATC Classification and DDD Assignment 2011. http://www.whocc.no/filearchive/publications/2011guidelines.pdf. Accessed 14 Oct 2013.
Weist K, ESAC-Net participants and the Antimicrobial Resistance and Healthcare-associated Infections (ARHAI) programme at ECDC. ECDC publishes its first data on antimicrobial consumption in Europe. Euro Surveill. 2013;7:20419.
Vaccheri A, Bjerrum L, Resi D, Bergman U, Montanaro N. Antibiotic prescribing in general practice: striking differences between Italy (Ravenna) and Denmark (Funen). J Antimicrob Chemother. 2002;50:989–97.
Ternhag A, Hellman J. More on U.S. outpatient antibiotic prescribing, 2010. N Engl J Med. 2013;369:1175.
Huttner B, Harbarth S. Variations in outpatient antimicrobial use between and within countries: an ongoing mystery. Infection. 2010;38:1–2.
Veninga CC, Lundborg CS, Lagerlov P, Hummers-Pradier E, Denig P, Haaijer-Ruskamp FM. Treatment of uncomplicated urinary tract infections: exploring differences in adherence to guidelines between three European countries. Drug Education Project Group. Ann Pharmacother. 2000;34:19–26.
Cadieux G, Tamblyn R, Dauphinee D, Libman M. Predictors of inappropriate antibiotic prescribing among primary care physicians. CMAJ. 2007;177:877–83.
Wang KY, Seed P, Schofield P, Ibrahim S, Ashworth M. Which practices are high antibiotic prescribers? A cross-sectional analysis. Br J Gen Pract. 2009;59:e315–20.
Habib G, Hoen B, Tornos P, Thuny F, Prendergast B, Vilacosta I, et al. Guidelines on the prevention, diagnosis, and treatment of infective endocarditis (new version 2009): the Task Force on the Prevention, Diagnosis, and Treatment of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and the International Society of Chemotherapy (ISC) for Infection and Cancer. Eur Heart J. 2009;30(19):2369–413.
Hulscher ME, van der Meer JW, Grol RP. Antibiotic use: how to improve it? Int J Med Microbiol. 2010;300(6):351–6.
Zhang Y, Steinman MA, Kaplan CM. Geographic variation in outpatient antibiotic prescribing among older adults. Arch Intern Med. 2012;172(19):1465–71.
Harbarth S, Albrich W, Brun-Buisson C. Outpatient antibiotic use and prevalence of antibiotic-resistant pneumococci in France and Germany: a sociocultural perspective. Emerg Infect Dis. 2002;8(12):1460–7.
Butler CC, Hood K, Verheij T, Little P, Melbye H, Nuttall J, et al. Variation in antibiotic prescribing and its impact on recovery in patients with acute cough in primary care: prospective study in 13 countries. BMJ. 2009;338:b2242.
Boggon R, Hubbard R, Smeeth L, Gulliford M, Cassell J, Eaton S, et al. Variability of antibiotic prescribing in patients with chronic obstructive pulmonary disease exacerbations: a cohort study. BMC Pulm Med. 2013;13:32.
Molstad S, Erntell M, Hanberger H, Melander E, Norman C, Skoog G, et al. Sustained reduction of antibiotic use and low bacterial resistance: 10-year follow-up of the Swedish Strama programme. Lancet Infect Dis. 2008;8(2):125–32.
Monnet DL, Molstad S, Cars O. Defined daily doses of antimicrobials reflect antimicrobial prescriptions in ambulatory care. J Antimicrob Chemother. 2004;53(6):1109–11.
Safrany N, Monnet DL. Antibiotics obtained without a prescription in Europe. Lancet Infect Dis. 2012;12(3):182–3.
Napolitano F, Izzo MT, Di Giuseppe G, Angelillo IF. Public knowledge, attitudes, and experience regarding the use of antibiotics in Italy. PLoS One. 2013;8(12):e84177.
Acknowledgments
The current study is part of the EU-funded ARITMO study which aims to assess the utilisation and arrhythmogenic potential of antiinfectives, antihistamines and antipsychotics. ARITMO is a Research and Development project funded by the Health Area of the European Commission under the VII Framework Program (FP7/2007–2013) under Grant agreement no. 241679-the ARITMO project.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
See Tables 4, 5, 6, 7 and Figs. 5, 6, 7.
Overall volume of antibiotics as DDDs per 1000 inhabitants per day by country and sex. DDDs defined daily doses, DID DDD per 1000 inhabitants per day, AUH Aarhus University Hospital, ERD Emilia-Romagnia regional database, GePaRD German Pharmacoepidemiological Research Database, THIN The Health improvement network
Rights and permissions
About this article
Cite this article
Mor, A., Frøslev, T., Thomsen, R.W. et al. Antibiotic use varies substantially among adults: a cross-national study from five European Countries in the ARITMO project. Infection 43, 453–472 (2015). https://doi.org/10.1007/s15010-015-0768-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-015-0768-8