Abstract
Purpose
Intraoperative cerebral aneurysm rupture (IOR) is a common phenomenon with a frequency of around 19%. Research regarding IOR lacks an analysis of its predictors.
Methods
We retrospectively examined all saccular aneurysms, in 198 patients with subarachnoid hemorrhage, surgically treated from 2013 to 2019. Operative reports, patient histories, blood test results, discharge summaries, and radiological data were reviewed. IOR was defined as any bleeding from the aneurysm during surgery, preceding putting a clip on its neck, regardless of how trivial.
Results
The frequency of IOR was 20.20%. Patients with IOR had higher aneurysm dome size (9.43 ± 8.39 mm vs. 4.96 ± 2.57 mm; p < 0.01). The presence of blood clot on the aneurysm dome was significantly associated with IOR (12.50% vs. 2.53%; p < 0.01). We also associated lamina terminalis fenestration during surgery (7.50% vs. 21.52%; p = 0.04) and multiple aneurysms (5.00% vs. 18.35%; p = 0.038) with a lower risk of IOR. Glucose blood levels were also elevated in patients with IOR (7.47 ± 2.78 mmol/l vs. 6.90 ± 2.22 mmol/l; p = 0.04). Multivariate analysis associated that urea blood levels (OR 0.55, 0.33 to 0.81, p < 0.01) and multiple aneurysms (OR 0.04, 0.00 to 0.37, p = 0.014) were protective factors against the occurrence of IOR.
Conclusion
Large dome size of an aneurysm, a blood clot on the aneurysm dome and elevated glucose blood levels can be IOR predictive. Lamina terminalis fenestration, the appearance of multiple aneurysms, and high urea blood levels may be associated with a lower risk of such an event.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intracranial aneurysm rupture is an unpredictable danger that may lead to an unfavorable outcome. Intraprocedural rupture is a well-known complication of intracranial aneurysm treatment that has been profoundly studied for coiling procedures, but there is less research on operative cerebral aneurysm treatment. Intraoperative rupture (IOR) is a much more common issue in comparison to endovascular methods—19% to 5%, respectively [1]. The most dangerous bleeding may be the effect of IOR occurring before proximal vascular control [2]. Despite larger sack size, location on an anterior communicating artery (ACoA) being independent predictors of IOR, many preoperative risk factors such as elevated systolic blood pressure, previous aneurysm rupture, temporary artery occlusion, blood glucose level, ventricular opening, modified Fischer grade, brain swelling, World Federation of Neurosurgical Societies (WFNS) scale, Glasgow Coma Scale (GCS) upon admission still need more research [3,4,5]. Possible causes of IOR also include craniotomy drilling vibration and dural opening transmural pressure changes [2]. When studying factors associated with IOR drugs taken before surgery and laboratory blood parameters results are often overlooked. This study aimed to seek new predictors of IOR with special attention of above mentioned.
Methods
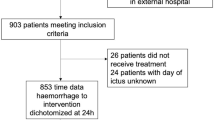
In this retrospective study, we analyzed patients with surgically treated, ruptured saccular cerebral aneurysms, hospitalized between January 2013 and July 2019 due to aneurysmal subarachnoid hemorrhage (SAH). A total of 198 patients have met the study inclusion criteria. All patients were operated by neurosurgeons working in the same center. All the neurosurgeons, who were main operators, were experts in field with at least 6 years of experience. SAH was diagnosed by assessing computed tomography (CT) scan performed upon admission. All patients were operated within 24 h after first symptoms of aneurysm rupture. The presence of IOR was determined based on operative records, which were written by neurosurgeons shortly after surgery. We additionally obtained factors such as aneurysm visual appearance, with special consideration of the presence of blood clot on the aneurysm dome, and whether the patient had lamina terminalis fenestration before putting clip on aneurysm neck (during obtaining access to aneurysm or directly after opening the dura mater). Aneurysm characteristics such as its number, location, dome, and neck size were obtained from an assessment of CT angiography on coronal and sagittal planes. Measurements were performed on dedicated workstation running IMPAX 6 Software (Agfa Healthcare nV, Belgium). From patients’ medical records, we also acquired data regarding medical history—diseases, current medication, and blood test results preceding surgery. On admission, patients were assessed with GCS, Hunt and Hess scale, modified Fischer grading scale, and WFNS scale. Upon discharge, patients were assessed using the modified Rankin Scale (mRS). The intraoperative rupture was defined as any bleeding from the aneurysm preceding putting a clip on its neck during surgery [6]. The study protocol was approved by the local bioethical committee and all patients gave informed consent. The database management and statistical analysis were performed with RStudio version 8.5 for Windows (RStudio, Inc, USA). We used the Shapiro–Wilk test to assess normality. For comparisons of continuous variables, we used the t test for normally distributed variables and Mann–Whitney U test for non-normally distributed variables. We used the χ2 test for dichotomized variables. We express continuous variables as mean ± standard deviation. To find factors independently associated with risk of IOR we employed logistic regression analysis, with and without adjustment for possible confounders. All significance tests are two-tailed and p value < 0.05 are considered statistically significant.
Results
Our study group consisted of 125 (63.13%) females. The mean age of patients was 55.68 ± 13.77 years. Most of the aneurysms were located on the middle cerebral artery (MCA) (54.04%), on ACoA (30.80%), and internal carotid artery (ICA) (6.06%) (Fig. 1). The average GCS score upon admission was 11.66 ± 4.71 and the average mRS score upon discharge was 3.02 ± 2.02. Most of the aneurysms were right-sided—84 (61.31%) and 53 (38.69%) remained left-sided, while 61 were located on a single ACoA. Multiple aneurysms were present in 31 (15.66%) cases. We established the frequency of IOR at 20.20%. The dome size of an aneurysm was observed to be increased in patients with IOR (9.43 ± 8.39 mm vs. 4.96 ± 2.57 mm; p < 0.01). Statistical analysis showed that the presence of blood clot on the aneurysm dome is significantly associated with IOR (12.50% vs. 2.53%; p < 0.01). We additionally observed that patients who had lamina terminalis fenestration during surgery are at a lower risk of IOR (7.50% vs. 21.52%; p = 0.04), as well as those with multiple aneurysms (5.00% vs. 18.35%; p = 0.038) (Table 1). We found no correlation between IOR and intake of anti-hypertensive and anti-diabetic drugs. (Table 2). In terms of blood test results upon admission, patients with longer activated partial thromboplastin time (APTT) (31.44 ± 5.73 s vs. 28.73 ± 4.56 s; p = 0.02) and prothrombin time (PT) through International Normalized Ratio (INR) (1.15 ± 0.47 vs. 1.03 ± 0.10; p = 0.05) had increased risk of IOR. Glucose blood levels were also higher in patients with IOR (7.47 ± 2.78 mmol/l vs. 6.90 ± 2.22 mmol/l; p = 0.04). APTT, INR and glucose above norms were not predictive for IOR. IOR was also associated with lower urea blood levels (4.18 ± 1.34 vs. 5.57 ± 3.53; p = 0.048). Multivariate analysis associated that urea blood levels (OR 0.55, 0.33–0.81, p < 0.01) and multiple aneurysms (0.04, 0.00–0.37, p = 0.014) were protective factors against the occurrence of IOR. Such analysis also revealed that APTT (1.18, 1.03–1.38, p = 0.026) was IOR predictive (Table 3). Rupture occurred the most (61.11%) when surgeon was dissecting cerebral structures to access to the aneurysm. Second most common moment was putting clip on aneurysm neck (22.22%), third—after dural opening (1.11%), and fourth was when dissecting the aneurysm from encasing tissues and vessels (5.56%).
Distribution of surgically clipped aneurysms’ rupture rates by location. ACA anterior cerebral artery, ACoA anterior communicating artery, ICA internal carotid artery, IOR intraoperative cerebral aneurysm rupture, MCA middle cerebral artery, PCoA posterior communicating artery, PICA posterior inferior cerebellar artery, VA vertebral artery
Discussion
The study group in our research consisted mostly of female patients. Articles by Chen et al., Krzyżewski et al. and the CARAT study [1, 3, 7] have explicitly shown that aneurysms occur more often in women than in men. Vast evidence supports our results that aneurysms mostly appear in anterior cerebral circulation with the dominance of MCA and ACoA [7]. ICA appeared to be the third most popular location of an aneurysm, which also appeared in research by Korja M et al. [8], that considered only ruptured aneurysms. Some studies show that ICA aneurysms or ACoA aneurysms are the most popular ones, but it may be dependent on the number of female patients in study group [1, 3]. One in five patients had an aneurysm rupture during the clipping procedure. IOR frequency varies in different studies from 3% to 19% [1, 3]. IOR present in 19% of patients was observed in the CARAT study, which observed 711 patients during clipping procedure due to SAH being in our opinion the most accurate estimation of IOR frequency among literature [1]. Chen S.F. et al. [3] study has compared IOR rates in patients with unruptured and ruptured aneurysms. In patients with unruptured aneurysms prior to surgery IOR rate was 0.57%, which is much lower than in the ruptured aneurysms IOR ratio of 9.6%. The first of the factors associated with the increased risk of IOR in our study was higher aneurysm dome size. Lakićević et al. [9] study shared an idea that aneurysm size may have an influence but that research could not prove such an association. CARAT study has also suggested that IOR is not associated with aneurysm size [1]. However, a pooled analysis of six prospective cohort studies conducted by Greving et al. [10] described aneurysm size as a predictor of overall aneurysm rupture. Similarly, irregular aneurysm shape, which is associated with aneurysm size, has been shown to increase the risk of IOR [11]. Additionally, according to a study by Zhu et al. [12], aneurysm size is independently associated with aneurysm wall enhancement that is considered a rupture risk factor. Our research has shown that the presence of a blood clot on the aneurysm dome significantly increases the risk of IOR. Experimental models have demonstrated that continuous exposure of the unorganized thrombus to the circulation can promote the recruitment of neutrophils and inflammatory cells [13, 14]. There is also evidence that the presence of thrombus in the aneurysm lumen is associated with the inflammation process in the aneurysm wall [15]. That leaves us with a question if IOR risk correlates with the inflammatory process beginning prior to SAH/during/after SAH. Lamina terminalis fenestration (LTF) appeared as another protective factor against the occurrence of IOR as well as the presence of multiple aneurysms. In our study LTF was performed after cranial and dural opening or at the beginning of aneurysm access cerebral dissection. All neurosurgeons in operative records described that performing LTF gave them better operating conditions and more procedural space. Neurosurgeons often perform LTF to create an additional way for cerebrospinal fluid to outflow and reduce intracranial pressure (ICP) which allows better operating conditions. To the best of our knowledge, there is no research assessing the lamina terminalis fenestration effect on IOR frequency. Although, LTF was associated with a better outcome in patients who underwent surgery due to SAH. This procedure was also associated with a lower risk of vasospasm [16]. Reducing the risk of vasospasm by performing LTF may influence outcome after SAH, because it was associated as one of the main contributors to SAH mortality and morbidity [17]. LTF has also been associated with a lower risk of hydrocephalus which may occur during SAH [18]. It may allow us to suggest that performing LTF can lead to improved functional outcomes [19]. Our study also associated IOR with multiple aneurysms putting them forward as a possible protective factor. Such association was also supported by the multivariate analysis result. A study conducted by Ho et al. [20] has also shown that patients with unruptured aneurysms were more likely to have multiple aneurysms in comparison to those with ruptured aneurysms. Such association was also supported by long-term study by Juvela et al. [21] which suggested that presence of multiple aneurysms does not elevate rupture risk. Study by Sai Kirian et al. [22] has shown that successful occlusion and similar outcomes can be achieved after both single and multiple aneurysms microsurgical clipping procedures. Patients with multiple aneurysms have also been studied for specific rupture risk factors. Researchers found out that aspect ratio and irregular shape of multiple aneurysms have been associated with a higher risk of aneurysm rupture [23]. Until now, there has been no evidence that the presence of multiple intracranial aneurysms may be a factor reducing the risk of IOR. There was evidence that multiplicity raises the risk of subarachnoid hemorrhage and endovascular treatment of one aneurysm may also trigger a formation of another aneurysm elsewhere [24]. We consider that association between multiple aneurysms and lower risk of IOR may be an effect of higher surgeon attention during multiple aneurysm microsurgery, being a possible high-risk scenario. What is more hemodynamic study of single patient with multiple aneurysms has shown that aneurysms affect each other’s flow rates which may affect rupture risks preoperatively and during surgery [25]. As it comes to drugs association with IOR, only two patients in our study had taken anticoagulants prior to SAH and both had consecutive IOR, but due to small sample size the statistical difference is likely to be spurious. A large randomized control trial on antithrombotic agents (anticoagulants included) influence on intracranial hemorrhage risk has proved such association [26]. On the other hand, Tarlov et al. [27] study has shared an idea that aneurysm rupture is not influenced by anticoagulants. Lack of such association in that research, as authors admitted, may have been caused by the small sample size and retrospective aspect of the study. Coagulation parameters by the mean of Activated Partial Thromboplastin Time (APTT) and International Normalized Ratio (INR) appeared to be higher in patients with IOR, although APTT and INR above normal levels—> 36.0 s and > 1.2, respectively—showed no relationship to IOR. Our multivariate analysis has also supported such a theory. INR elevation in aneurysm surgery had been previously studied by Can et al. [28] and provided us with an association of intracranial aneurysm rupture and higher INR values. APTT to the best of our knowledge has not been researched for impact on intracranial aneurysms, although a study on abdominal aortic aneurysms shows that APTT increases in patients admitted to ICU due to its rupture [29]. Such an effect on IOR is yet to be researched more profoundly. Despite not finding a link between IOR and anti-diabetic drugs, increased blood glucose levels were a factor that increased the risk of an IOR. Presence of glucose blood level above norm—over 5.8 mmol/L was not found significantly predictive for IOR. Hyperglycemia develops in one-third of SAH patients. Hyperglycemia is associated with a poor clinical condition on admission and is independently associated with poor outcome [30,31,32,33]. In American Guidelines for management of aneurysmal, SAH prevention of hyperglycemia is classified as probably indicated [19]. Hyperglycemia could be a secondary phenomenon to a transient stress reaction inflicted by the insult. Indeed, previous studies showed that the release of catecholamines and levels of glucose relates to the clinical magnitude of SAH [34]. Such associations are yet to be established for IOR. Strikingly, blood urea levels were found to be lower in patients with IOR. The multivariate analysis we performed has also exposed such association. This is the first study to connect urea and intracranial aneurysms, however, elevated serum urea levels were previously associated with calcification in intracranial arteries [35]. To the best of our knowledge, calcification has also been connected with higher aneurysm size which has been associated, as stated above, with increased risk of IOR [36]. Despite such association staying in contrary with our research, enteral urea dosage has also been reported to decrease ICP [37]. Managing increased ICP may decrease the risk of IOR, but such studies are yet to be performed [38]. As in both groups, mean urea levels were within normal range, the simplest association may be the fact that higher urea levels are associated with higher protein intake [39]. High-protein diet has been found to improve systemic microvascular health in patients with heart failure, while low-protein diet was found to increase inflammation and vascular calcification in rats [40, 41].
Several factors were identified to increase and decrease the risk of aneurysm rupture during the clipping procedure. Specifically, a large dome size of an aneurysm, a blood clot on the aneurysm dome and elevated glucose blood levels were found to be associated with IOR in our study. Performing lamina terminalis fenestration, the appearance of multiple aneurysms, and high urea blood levels may be associated with a lower risk of such an event. These parameters were available through imaging, patients’ data and, although further analysis and validation of these parameters is necessary, they could add to the surgeon’s ability to assess the rupture risk more accurately before or in surgery.
Limitations
Due to retrospective character of this study may present inferior level of evidence compared with prospective studies as it is a “chart-based study”. Our research was limited by the size of the study group. Further research should be performed on larger and more varied study groups. Factors like fluctuation of blood pressure, use of tranexamic acid, sharp or blunt dissection, transmural pressure gradient, multi-lobulated sac, number of previous bleeds, irregular shapes, pre-emptive trapping, or proximal control, use of pilot clip, presence of calcification or atherosclerosis were not possible to discuss and analyze due to retrospective character of the study. Missing data for different laboratory tests may have also influenced results of our study. Despite using operative reports to determine IOR, we would like to emphasize that those reports were standardized and high-quality with specific description of every part of surgery. Despite our limitations, this is the first study which analyzes such a wide spectrum of factors possibly influencing IOR frequency.
Data availability
No data and materials are going to be available publicly.
Code availability
Not applicable.
References
Elijovich L, Higashida RT, Lawton MT et al (2008) Predictors and outcomes of intraprocedural rupture in patients treated for ruptured intracranial aneurysms: The CARAT study. Stroke 39:1501–1506. https://doi.org/10.1161/STROKEAHA.107.504670
Park J, Son W, Park KS et al (2016) Intraoperative premature rupture of middle cerebral artery aneurysms: risk factors and sphenoid ridge proximation sign. J Neurosurg 125:1235–1241. https://doi.org/10.3171/2015.10.JNS151586
Chen SF, Kato Y, Kumar A et al (2016) Intraoperative rupture in the surgical treatment of patients with intracranial aneurysms. J Clin Neurosci 34:63–69. https://doi.org/10.1016/j.jocn.2016.01.045
Okazaki T, Hifumi T, Kawakita K et al (2018) Blood glucose Variability: a strong independent predictor of neurological outcomes in aneurysmal subarachnoid hemorrhage. J Intensive Care Med 33:189–195. https://doi.org/10.1177/0885066616669328
Leipzig TJ, Morgan J, Horner TG et al (2005) Analysis of intraoperative rupture in the surgical treatment of 1694 saccular aneurysms. Neurosurgery 56:455–466. https://doi.org/10.1227/01.NEU.0000154697.75300.C2
Sandalcioglu IE, Schoch B, Regel JP et al (2004) Does intraoperative aneurysm rupture influence outcome? Analysis of 169 patients. Clin Neurol Neurosurg 106:88–92. https://doi.org/10.1016/j.clineuro.2003.10.011
Krzyżewski RM, Kliś KM, Kucala R et al (2018) Intracranial aneurysm distribution and characteristics according to gender. Br J Neurosurg 32:541–543. https://doi.org/10.1080/02688697.2018.1518514
Korja M, Kivisaari R, Jahromi BR, Lehto H (2017) Size and location of ruptured intracranial aneurysms: consecutive series of 1993 hospital-admitted patients. J Neurosurg 127:748–753. https://doi.org/10.3171/2016.9.JNS161085
Lakicevic N, Vujotic L, Radulovic D et al (2015) Factors influencing intraoperative rupture of intracranial aneurysms. Turk Neurosurg. https://doi.org/10.5137/1019-5149.JTN.12966-14.2
Greving JP, Wermer MJH, Brown RD et al (2014) Development of the PHASES score for prediction of risk of rupture of intracranial aneurysms: a pooled analysis of six prospective cohort studies. Lancet Neurol 13:59–66. https://doi.org/10.1016/S1474-4422(13)70263-1
Goertz L, Hamisch C, Telentschak S et al (2018) impact of aneurysm shape on intraoperative rupture during clipping of ruptured intracranial aneurysms. World Neurosurg 118:e806–e812. https://doi.org/10.1016/j.wneu.2018.07.058
Zhu C, Wang X, Degnan AJ et al (2018) Wall enhancement of intracranial unruptured aneurysm is associated with increased rupture risk and traditional risk factors. Eur Radiol 28:5019–5026. https://doi.org/10.1007/s00330-018-5522-z
Marbacher S, Marjamaa J, Bradacova K et al (2014) Loss of mural cells leads to wall degeneration, aneurysm growth, and eventual rupture in a rat aneurysm model. Stroke 45:248–254. https://doi.org/10.1161/STROKEAHA.113.002745
Marbacher S, Frösén J, Marjamaa J et al (2014) Intraluminal cell transplantation prevents growth and rupture in a model of rupture-prone saccular aneurysms. Stroke 45:3684–3690. https://doi.org/10.1161/STROKEAHA.114.006600
Cebral J, Ollikainen E, Chung BJ et al (2017) Flow conditions in the intracranial aneurysm lumen are associated with inflammation and degenerative changes of the aneurysm wall. Am J Neuroradiol 38:119–126. https://doi.org/10.3174/ajnr.A4951
Andaluz N, Zuccarello M (2004) Fenestration of the lamina terminalis as a valuable adjunct in aneurysm surgery. Neurosurgery 55:1050–1057. https://doi.org/10.1227/01.NEU.0000140837.63105.78
Sozen T, Tsuchiyama R, Hasegawa Y et al (2011) Advances in Experimental Subarachnoid Hemorrhage. In: Feng H, Mao Y, Zhang JH (eds) Early Brain Injury or Cerebral Vasospasm. Springer Vienna, Vienna, pp 15–21
Schroeder HWS, Oertel J, Gaab MR (2008) Endoscopic treatment of cerebrospinal fluid pathway obstructions. Neurosurgery. https://doi.org/10.1227/01.NEU.0000249242.17805.E3
Connolly ES, Rabinstein AA, Carhuapoma JR et al (2012) Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the american heart association/american stroke association. Stroke 43:1711–1737
Ho AL, Lin N, Frerichs KU, Du R (2015) Intrinsic, transitional, and extrinsic morphological factors associated with rupture of intracranial aneurysms. Neurosurgery 77:433–441. https://doi.org/10.1227/NEU.0000000000000835
Juvela S, Poussa K, Lehto H, Porras M (2013) Natural history of unruptured intracranial aneurysms. Stroke 44:2414–2421. https://doi.org/10.1161/STROKEAHA.113.001838
Sai Kiran NA, Raj V, Sivaraju L et al (2020) Outcome of microsurgical clipping for multiple versus single intracranial aneurysms: a single-institution retrospective comparative cohort study. World Neurosurg 143:e590–e603. https://doi.org/10.1016/j.wneu.2020.08.019
Backes D, Vergouwen MDI, Velthuis BK et al (2014) Difference in aneurysm characteristics between ruptured and unruptured aneurysms in patients with multiple intracranial aneurysms. Stroke 45:1299–1303. https://doi.org/10.1161/STROKEAHA.113.004421
Ferns SP, Sprengers MES, van Rooij WJJ et al (2011) De novo aneurysm formation and growth of untreated aneurysms. Stroke 42:313–318. https://doi.org/10.1161/STROKEAHA.110.591594
Jou L, Britz DG (2016) Correlation between aneurysm size and hemodynamics in one individual with multiple small intracranial aneurysms. Cureus. https://doi.org/10.7759/cureus.683
Gulati S, Solheim O, Carlsen SM et al (2018) Risk of intracranial hemorrhage (rich) in users of oral antithrombotic drugs: nationwide pharmacoepidemiological study. PLoS ONE. https://doi.org/10.1371/journal.pone.0202575
Tarlov N, Norbash AM, Nguyen TN (2013) The safety of anticoagulation in patients with intracranial aneurysms. J Neurointerv Surg 5:405–409. https://doi.org/10.1136/neurintsurg-2012-010359
Can A, Castro VM, Dligach D et al (2018) Elevated international normalized ratio is associated with ruptured aneurysms. Stroke 49:2046–2052. https://doi.org/10.1161/STROKEAHA.118.022412
Gierek D, Cyzowski T, Kaczmarska A et al (2013) Okołooperacyjne czynniki prognostyczne u chorych z pękniętym tętniakiem aorty brzusznej leczonych na oddziale intensywnej terapii. Anestezjol Intens Ter 45:25–29. https://doi.org/10.5603/AIT.2013.0005
Dorhout Mees SM, van Dijk GW, Algra A et al (2003) Glucose levels and outcome after subarachnoid hemorrhage. Neurology 61:1132–1133. https://doi.org/10.1212/01.WNL.0000090466.68866.02
Juvela S, Siironen J, Kuhmonen J (2005) Hyperglycemia, excess weight, and history of hypertension as risk factors for poor outcome and cerebral infarction after aneurysmal subarachnoid hemorrhage. J Neurosurg 102:998–1003. https://doi.org/10.3171/jns.2005.102.6.0998
Lanzino G, Kassell NF, Germanson T et al (1993) Plasma glucose levels and outcome after aneurysmal subarachnoid hemorrhage. J Neurosurg 79:885–891. https://doi.org/10.3171/jns.1993.79.6.0885
Wartenberg KE, Schmidt JM, Claassen J et al (2006) Impact of medical complications on outcome after subarachnoid hemorrhage*. Crit Care Med 34:617–623. https://doi.org/10.1097/01.CCM.0000201903.46435.35
Kruyt ND, Biessels GJ, De Haan RJ et al (2009) Hyperglycemia and clinical outcome in aneurysmal subarachnoid hemorrhage: a meta-analysis. Stroke. https://doi.org/10.1161/STROKEAHA.108.529974
Chen XY, Lam WWM, Ho KN et al (2006) The frequency and determinants of calcification in intracranial arteries in Chinese patients who underwent computed tomography examinations. Cerebrovasc Dis 21:91–97. https://doi.org/10.1159/000090206
Kizilkilic O, Huseynov E, Kandemirli SG et al (2016) Detection of wall and neck calcification of unruptured intracranial aneurysms with flat-detector computed tomography. SAGE Publications, UK, In Interventional Neuroradiology, pp 293–298
Annoni F, Fontana V, Brimioulle S et al (2017) Early effects of enteral urea on intracranial pressure in patients with acute brain injury and hyponatremia. J Neurosurg Anesthesiol 29:400–405. https://doi.org/10.1097/ANA.0000000000000340
Brinker T, Seifert V, Stolke D (1990) Acute changes in the dynamics of the cerebrospinal fluid system during experimental subarachnoid hemorrhage. Neurosurgery. https://doi.org/10.1097/00006123-199009000-00005
Weiner ID, Mitch WE, Sands JM (2015) Urea and ammonia metabolism and the control of renal nitrogen excretion. Clin J Am Soc Nephrol 10:1444–1458. https://doi.org/10.2215/CJN.10311013
Yamada S, Tokumoto M, Tatsumoto N et al (2016) Very low protein diet enhances inflammation, malnutrition, and vascular calcification in uremic rats. Life Sci 146:117–123. https://doi.org/10.1016/j.lfs.2015.12.050
De LA, Dos SEM, Bello Moreira AS et al (2021) Dietary supplementation with whey protein improves systemic microvascular function in heart failure patients: a pilot study. Brazilian J Med Biol Res. https://doi.org/10.1590/1414-431x202010577
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation was done by KMK. Data collection and analysis were performed by MJF, MJB and KMK. The first draft of the manuscript was written by MJF and all authors commented on previous versions of the manuscript. Supervision of the article and guidance—Roger: MK, JP, KS, BMK. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical standards
Study has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments, with local ethics committee approval and informed consent obtained from patients about using their blinded data in medical research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Frączek, M.J., Błoński, M.J., Kliś, K.M. et al. Predictors of intraoperative intracranial aneurysm rupture in patients with subarachnoid hemorrhage: a retrospective analysis. Acta Neurol Belg 123, 1717–1724 (2023). https://doi.org/10.1007/s13760-022-02005-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-022-02005-z