Abstract
Migraine is considered an underdiagnosed disease in general population. Different studies show a higher prevalence in neurologists. However, there are few studies about its prevalence in doctors of other specialties, where it could also be superior than in general population. Our aim was to define migraine lifetime prevalence among doctors according to three parameters (previous diagnosis, self-diagnosis and positivity of a screening test). Single-center, descriptive, cross-sectional study based on online surveys with collection of sociodemographic and clinical variables, addressed to doctors of a tertiary hospital. Participants who reported 5 or more headaches throughout their lives were considered “headache sufferers” and were divided in different groups according to their position (specialists or trainees) and their specialty (medical, medical-surgical and surgical or specialties with no direct contact with the patient). The Spanish validated version of the Migraine Screen Questionnaire (MS-Q) was used as screening test. There were 217 participants (response rate of 29%), 72% were women and 56% trainees, mean age 34 years (SD10). 77% were “headache sufferers” Among all participants, migraine lifetime prevalence according to diagnosis by another physician was 15.2%, self-diagnosis 38.2% and positivity of the MS-Q 20.3%; those categories were not mutually exclusive Greater but not statistically significant coexistence of self-diagnosis and positive MS-Q was seen in specialists compared to trainees and in medical specialties. Migraine prevalence among doctors in a tertiary care hospital was higher than in general population, according to all three parameters analyzed. Self-diagnosis was the highest which could reflect an overdiagnosis; further studies are needed to determine this possibility.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Among the eight chronic illnesses that affect over 10% of the world’s population [1], migraine is the main cause of years lived with disability of all neurological diseases [2]. Its diagnosis is clinical, according to the criteria established by the International Headache Society (IHS) [3]. Its prevalence varies in different studies, between 10 and 16% worldwide [4, 5] and the 1-year prevalence in Spain is 8% [6]. This prevalence is higher in women and in people aged 20–50 years.
Despite its high prevalence, migraine is considered an underdiagnosed disease, with a medical diagnosis in less than half of those who suffer from it [7]. With the aim of improving migraine detection in general population, some screening tests have been developed, like the ID Migraine Screener [8] and the Migraine Screen Questionnaire (MS-Q) [9]. Low medical consultation is considered one of the main factors contributing to migraine underdiagnosis [7]. Moreover, in a previous study, Viana et al. reported that, despite consulting for their headache, patients only achieved a correct migraine diagnosis in 8% of the cases when consulting with general practitioners and 35% when consulting with specialists [10]. Moreover, it has been calculated that only a third of the patients who suffer from it receives optimal treatment [11].
Different studies have shown higher migraine prevalence in neurologists and headache specialists [12,13,14], which may be explained by a deeper knowledge on the disease that could help them reach a migraine self-diagnosis, without needing another doctor’s confirmation [15]. Those fewer studies that have evaluated migraine prevalence in other specialties, most of them focused on primary care doctors, have shown a similar prevalence to that of the general population [16,17,18,19].
However, to the best of our knowledge, there are no studies that have compared migraine prevalence in doctors from different specialties. Thanks to their medical training and their familiarity with migraine, a higher prevalence could be expected in doctors responsible for the diagnosis and/or treatment of this disease, as observed in neurologists.
According to this, we hypothesize that the prevalence in doctors from different specialties would be higher than the one in the general population. The main objective of our study was to estimate migraine prevalence in doctors of a tertiary hospital according to three parameters: previously diagnosed by another doctor (PD), self-diagnosis (SM) and positivity of the Spanish validated screening test, the Migraine Screen Questionnaire (positive MS-Q). These parameters were not mutually exclusive and each participant could have a migraine diagnosis made by him-/herself and by another physician. Likewise, we evaluated the possible impact of different sociodemographic and clinical items on this prevalence.
Methods
We conducted a descriptive, cross-sectional study, with data collection from surveys addressed to all doctors of a tertiary hospital in Madrid, Spain (see Supplementary file).
The survey was developed with the digital platform Google forms and then sent to the doctors’ institutional electronic mail. When designing the survey all relevant questions had to be answered to conclude the process so there were no missing data.
The study was approved by the Ethics Committee and hospital’s Medical Direction on April 4th 2019 (reference number 3718).
The recruitment period started on May 2019 and finished on September 2019.
Each survey included 6 initial questions about sociodemographic features and 18 about the clinical aspects of the headache. There were single-choice and multiple-choice questions (see Supplementary material). Questions numbered 16–20 corresponded to the items included in the MS-Q. A positive MS-Q was considered when the participant answers positively to 4 or more of any of these five questions.
The sample included doctors from different specialties working at that moment in the hospital. We classified participants in groups according to their specialty and position (specialists and trainees) and we determined migraine prevalence in the general sample and in the different subgroups according to PD, SM and positive MS-Q. We also analyzed the coexistence of SM and positive MS-Q in the different subgroups.
The different specialties were clustered in three groups: one of “medical specialties” including Allergology, Gastroenterology, Cardiology, Endocrinology, Hematology, Family Medicine, Critical Care Medicine, Internal Medicine, Nephrology, Pneumology, Neurology, Oncology, Psychiatry and Rheumatology; another with “surgical or medical-surgical specialties” including Anesthesiology, General Surgery, Oral and Maxillofacial Surgery, Traumatology, Dermatology, Neurosurgery, Ophthalmology, Otorhinolaryngology and Urology; and one with those specialties with “no direct contact with patients” including Clinical Analysis, Anatomical Pathology, Clinical Pharmacology, Immunology, Preventive Medicine, Microbiology and Radiology.
The required sample size was beforehand estimated in 220 participants. To reach statistical significance, statistical power was set at 0.80 and alpha error ≤ 0.05. Migraine prevalence in doctors of different specialties was assumed to be within that previously reported in the general population (approximately 15%) and the one described in neurologists (over 30%).
A descriptive analysis of the characteristics of both groups was performed: for the nominal variables, the sample size (N) and the percentage (%) per group were shown, and a χ2 test or the Fisher exact test was performed. For continuous variables: means and standard deviations (SD) are shown for variables with normal distribution, and median and interquartile range (IQR) for variables that do not have a normal distribution. Likewise, a t-test for independent variables and equal variance test or Wilcoxon rank tests were performed according to whether or not they followed assumptions (normal distribution and homoscedasticity). Normal distribution was checked by the Shapiro–Wilk test. Homoscedasticity was checked by Levene test. A multiple logistic regression was performed to predict the independent contribution of different factors. For this model, variables that in the descriptive had shown a p ≤ 0.1 were included. Multicollinearity was checked before making the models. A p value ≤ 0.05 was considered statistically significant. All statistical analysis was performed using the statistical package STATA SE version 14.1 (StataCrop, College Station, TX, USA).
Regression models were estimated with STATA software. In our case, there was no collinearity problem.
Results
Descriptive analysis of the participants
There were 217 doctors who answered the survey from a total possible number of participants of 744, being the participation rate of 29%. Mean age was 34 years (SD 10) and mean number of working years was 9.8 (SD 11). 50 participants (23%) reported having suffered less than 5 headaches throughout their lives.
Of the 744 physicians working in the hospital, 60% were women. The proportion of women in our sample was 72% (156/217). 279 out of the 744 doctors in our hospitals were trainees (38%) and in our sample they represented a 56%. Considering an alpha risk of 0.05 and beta risk of 0.2 in a bilateral contrast hypotheses, both sex and work position distribution were considered representative of the doctors’ population in the hospital (≥ 133 women and ≥ 58 trainees).
Regarding the different groups of specialties, a total of 155 participants were included in the group of “medical specialties”, 37 in the group of “medical-surgical and surgical specialties” and 25 in the group with “no direct contact with patients”. “Headache sufferers”, defined as those with ≥ 5 headaches throughout their lives, were 119/155 (76.77%), 30/37 (81%) and 18/25 (72%), respectively. A total of 24 neurologists participated in the survey, 16 of whom (66.67%) were “headache sufferers”.
122 out of 217 (56%) were trainees and among them, 82 (67.2%) were “headache sufferers”. Of the 95 specialists participating in our study, 75 (78.9%) have had ≥ 5 headaches throughout their lives, as they are necessary to consider a migraine diagnosis according to ICHD-3 criteria [3].
Migraine prevalence according to PD, SM and positive MS-Q
Figure 1 shows a schematic representation of the study sample. 167/217 participants (77%) were considered “headache sufferers”. Of those, 45/167 (27%) had consulted another doctor about their headaches and 33 of those 45 (73.3%) had received a previous diagnosis of migraine (PD estimated prevalence 33/217 (15.2%)). When asked about the type of headache they thought they suffered, 83 participants answered migraine (prevalence according to SM 83/217 (38.2%)). 44 participants had a positive screening test determined by a score \(\ge\) 4 in MS-Q (prevalence of 44/217 (20.2%) according to positive MS-Q).
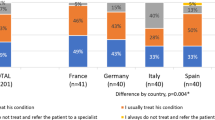
Migraine prevalence according to different specialties and work position
Migraine prevalence in the different subgroups was analyzed and is shown in Table 1.
Migraine prevalence according to work position (specialists or trainees) is shown in Table 2. Among residents with headache, 25/82 (30.5%) consulted another doctor in relation with their headache; while in the specialists group, this percentage was lower (20/75, 26.6%).
We studied the coexistence of SM and positive MS-Q in the different groups of the sample. According to specialties, 26/119 (21.8%) of the participants in the group of “medical specialties” presented SM and positive MS-Q, while this proportion was 5/30 (16.7%) in the participants of the group “surgical and medical-surgical” and 6/18 (3.3%) in group of specialists with “no direct treat with patients”. Regarding work position, 18/82 (21.9%) of the trainees and 29/75 (38.7%) of the specialists had both SM and positive MS-Q. However, these differences observed in SM and MS-Q coexistence between specialty groups and work position did not reach statistical significance (p = 0.086 and p = 0.083, respectively).
Among the 24 neurologists, 14 (58.3%) had a SM, though only 5 (20.8%) had a positive MS-Q.
Clinical items related to SM and PD
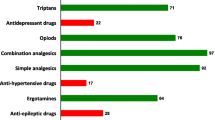
We observed a statistically significant relation (p < 0.01) between SM and multiple clinical characteristics: duration of headache > 4 h and < 3 days, phonophobia and photophobia, avoidance of routine physical activity, unilateral headache, pulsating quality, nausea and/or vomit and aura (see Table 3).
Subsequently, we performed a multivariate logistic regression model with all those characteristics, in which 4 of the variables showed a narrow association with migraine SM: unilateral pain (OR 3.76, p = 0.012), nausea and/or vomits (OR 4.19, p = 0.009), phonophobia or photophobia (OR 9.74, p < 0.001) and aura (OR 5.98, p < 0.001).
We also found statistically significant relations between PD and pulsating quality (p = 0.023), phonophobia and photophobia (p = 0.007) and aura (p = 0.005) (see Table 4).
Discussion
In our study, we estimated a migraine prevalence among doctors in a tertiary care hospital in Spain between 15.2% and 38.2%, according to three different parameters. Coexistence between self-diagnosis and a positive screening test was higher in specialists than in trainees and also in medical specialties than in surgical or with no direct contact with patients.
Migraine prevalence according to PD (15.2%) was the lowest. This prevalence is similar to the one described in the general population and possibly reflects the underdiagnosis of the disease, in relation to low consultation rates to other doctors. In our sample, only 27% of the participants consulted another physician, but there was a high proportion of migraine among them (73.3%). This could be related to the mean age of the participants, according to migraine distribution [20] and/or to the disabling nature of the disease that may lead patients with migraine to consult more frequently than those with other types of headache. Unfortunately, we did not determine the intensity and/or frequency of headaches in our participants.
The percentages of medical consultation for headache were higher in previous studies (64% in patients with migraine, 45% in patients with tensional headaches [21] and 43% in a sample of hospital workers [22]. According to Edmeads et al., the main reasons for medical consultation were search for treatment, preoccupation of a severe underlying etiology and the boredom of living with headache [21]. Another study has also highlighted uncertainty of diagnosis as a main feature to refer the patient to a neurologist [23]. It is possible that the participants’ formation and previous knowledge of the disease has allowed them to reach an easier self-diagnosis without seeking for an external confirmation, regardless of pain-related disability.
In contrast with our hypothesis, a previous study by Bartolini et al. compared migraine diagnostic delay assessed by ID-migraine among a group of hospital workers to the delay in general population; they found it took more years for hospital workers to reach a diagnosis. Moreover, there were no differences when comparing doctors or nurses, who are presumed to have clinical experience with the matter, and administratives or other workers with no such experience [24].
On the other hand, our study shows that trainees consult more often about their migraine which could suggest an increased insecurity about the self-diagnosis and treatment of their headache. Indeed, we found a higher coexistence of SM and positive MS-Q in specialists than in trainees. In relation to this, a previous German study found that younger doctors with fewer years of practice would use less preventive treatment than indicated in clinical guidelines, due to fear of side-effects, low intensity of migraine attacks and a sufficient effect of acute medication [25].
Migraine prevalence according to a positive MS-Q was 20.2% in our whole sample, which contrasts with the 38.2% calculated by self-diagnosis. This would be the first study trying to analyze migraine prevalence in doctors of different specialties with this tool, even though it would be close to the estimated prevalence range for doctors in other studies [17,18,19]. Likewise, according to our work, 58.3% of the neurologists reported a self-diagnosis of migraine while only 20.8% had a positive MS-Q. Both percentages are within the range of migraine prevalence in neurologists in different studies (27.6% and 71%) [13,14,15]. Recently, Evers et al. established a higher migraine prevalence according to SM in neurologists (43%) than in primary care doctors (19.3%), being the latter similar to the one in general population [26].
MS-Q, unlike other screening tests, is completely based in IHS migraine diagnostic criteria. It has a sensitivity and specificity over 0.8 and has a validated Spanish version.
Therefore, the difference in these two ways of analyzing migraine prevalence, being MS-Q a sensitive and validated tool for migraine screening, could be explained by an overdiagnosis among neurologists. Unfortunately, we could not properly evaluate this hypothesis as we did not conduct a medical interview with the participants to confirm the diagnosis. However, we found an older mean age in those neurologists who stated a self-diagnosis of migraine. Different studies on migraine in the eldest describe lower unilateral pain, less association with nausea and/or vomiting, less photophobia and phonophobia, higher coexistence of autonomic signs (mouth dryness, pallor…) and coexistence of aura [27,28,29]. For this reason, certain migraine diagnostic characteristics, included in the MS-Q screening test, could have been attenuated or even disappeared over the years in these participants, not reaching the positivity threshold for the MS-Q (false-negative).
Our study also showed a higher prevalence of migraine in specialists than in trainees according to both SM and positive MS-Q. Not only age and time with the disease could have affected the difference in migraine prevalence, but also working experience could be reflected in these results. Indeed, we also observed a higher coexistence of SM and positive MS-Q in participants of the group of “medical specialties” than in the other two groups. Therefore, it is probable that our findings reflect that “medical specialists” are more familiar with frequent diseases in the general population, such as migraine, as they spend more time evaluating patients and taking medical histories in outpatient consultations, hospitalization or emergency department.
On the other side, the lower migraine prevalence in participants of the group of specialties with “no usual direct treat with patients” compared to the other two subgroups could be explained by the lower number of participants within this subgroup (selection bias) or a true lower prevalence related to external factors (less changing work routines, less pressure derived from direct patient attention). As previously mentioned, we cannot discard either some degree of overdiagnosis in the other two groups, which can explain the higher prevalence according to SM than to MS-Q.
To our knowledge, there are no previous studies that have tried to evaluate migraine prevalence according to working experience, except for a study that determined a lower prevalence of migraine amongst residents according to SM [12].
Among clinical parameters that were more frequently related to SM and PD, we found similar results to other studies of migraine diagnosis in doctors [18]. This is not an unexpected finding, because some of the characteristics used by our participants to establish SM and PD, such as unilaterality or aggravation with physical activity, are key clinical criteria for migraine diagnosis and help to distinguish this disease from other primary headaches such as tension-type headache or trigeminal autonomic cephalalgias. For example, Viana et al. also observed that unilateral pain and vomiting helped the patients determine their headache was actually migraine [10].
Our study has some limitations. First, the methodology was based on an online survey, which prevented us from carrying out a medical evaluation of the participants to confirm the data. In this survey, and with the purpose of shortening it, we used a screening test that, despite being validated in our language, is less accurate than the ICHD-3 criteria. As reported in previous studies, the diagnostic criteria used to achieve migraine prevalence may induce variations. For instance according to the meta-analysis of migraine prevalence in university students conducted by Wang et al., a higher prevalence was found when the ICHD-3 criteria were used [30]. Besides, the size of the sample was modest to achieve statistical significance when analyzing different subgroups, such as specialties or work position, with an imbalance regarding the number of participants in each group. The response rate was not very high and this could have overestimated migraine prevalence; it is also possible that we faced a selection bias, as doctors who suffer from headache could have felt more motivated to answer the survey, and could have led to higher migraine prevalence in the sample regardless of the parameter analyzed [15]. Last, the possible influence of medications, frequency of headaches or other factors related to migraine chronification could not be analyzed due to the sample size.
As far as we know, ours is the first study that has tried to estimate migraine prevalence in doctors of different specialties and working position, regarding three parameters (previous diagnosis of migraine, self-diagnosis or positivity of MS-Q). It is also the first work comparing the accuracy of migraine self-diagnosis according to a positive screening test (MS-Q).
We found a higher migraine prevalence in doctors than the one reported in the general population regardless the parameter analyzed. Given the different prevalences depending on the parameter considered (previous diagnosis of migraine, self-diagnosis or positivity of a screening test) and being self-diagnosis the highest of the three, we cannot rule out an overdiagnosis in doctors, along with an underdiagnosis in the general population according to previous reports.
Moreover, our work showed that some clinical items and factors, such as the type of specialty or work position of the physician, could be related to a higher prevalence of migraine. These findings could be useful for future prevalence studies and might also help the development of more accurate screening tools for migraine diagnosis in both general population and subgroups with a former knowledge of the disease.
References
GBD 2015 Disease and Injury Incidence and Prevalence Collaborators (2016) Global, regional and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 388(10053):1545–1602
Steiner TJ, Stovner LJ, Birbeck GL (2013) Migraine: the seventh disabler. Cephalalgia 33(5):289–290
Headache Classification Committee of the International Headache Society (IHS) (2018) The International Classification of Headache Disorders, 3rd edition. Cephalalgia 38(1):1–211
Stewart WF, Lipton RB, Celentano DD et al (1992) Prevalence of migraine headache in the United States. Relation to age, income, race, and other sociodemographic factors. JAMA 267(1):64–69
Honkasalo M, Kaprio J, Heikkilä K et al (1993) A population-based survey of headache and migraine in 22,809 adults. Headache 33(8):403–412
Roy R, Sánchez-Rodríguez E, Galán S et al (2019) Factors associated with migraine in the general population of Spain: results from the European Health Survey 2014. Pain Med 20(3):555–563
Lipton RB, Diamond S, Reed M et al (2001) Migraine diagnosis and treatment: results from the American migraine study II. Headache 41(7):638–645
Lipton RB, Dodick D, Sadovsky R et al (2003) A self-administered screener for migraine in primary care the ID Migraine TM validation study. Neurology 61(3):375–382
Láinez MJA, Domínguez M, Rejas J et al (2005) Development and validation of the Migraine Screen Questionnaire (MS-Q). Headache 45(10):1328–1338
Viana M, Khaliq F, Zecca C et al (2020) Poor patient awareness and frequent misdiagnosis of migraine: findings from a large transcontinental cohort. Eur J Neurol 27(3):536–541
Lipton RB, Scher AI, Kolodner K et al (2002) Migraine in the United States: epidemiology and patterns of health care use. Neurology 58(6):885–894
Brockmann N, Evers S (2010) Migraine in neurologists and headache specialists. Headache 50(1):138–140
Alstadhaug KB, Hernandez A, Næss H et al (2012) Migraine among Norwegian neurologists. Headache 52(9):1369–1376
Lu SR, Wang SJ, Fuh JL (2006) The practice pattern of migraine management among neurologists in Taiwan. Cephalalgia 26(3):310–313
Yeh WZ, Blizzard L, Taylor BV (2018) What is the actual prevalence of migraine? Brain behav 8(6):e00950. https://doi.org/10.1002/brb3.950
Hettiarachchi J, Lipton RB, Dodick D et al (2012) A self administered screener for migraine in primary care. Neurology 61(3):375–382
Evans RW, Evans RE, Kell HJ (2010) A survey of family doctors on the likeability of migraine and other common diseases and their prevalence of migraine. Cephalalgia 30(5):620–623
Waters WE (1975) Migraine in general practitioners. Brit J prev soc med 29:48–52
Dalsgaard-Nielsen T, Ulrich J (1973) Prevalence and heredity of migraine and migrainoid headaches among 461 Danish doctors. Headache 12(4):168–172
Bigal ME, Liberman JN, Lipton RB (2006) Age-dependent prevalence and clinical features of migraine. Neurology 67(2):246–251
Edmeads J, Findlay H, Tugwell P et al (1992) Impact of migraine and tension-type headache on life-style, consulting behaviour, and medication use: a Canadian Population Survey. Can J Neurol Sci 20(2):131–137
Viticchi G, Falsetti L, Pettinari P et al (2014) Headache in a population of hospital workers. Neurol Sci 35(Suppl 1):157–158
Bekkelund SI, Salvesen R (2006) Is uncertain diagnosis a more frequent reason for referring migraine patients to neurologist than other headache syndromes? Eur J Neurol 13(12):1370–1373
Bartolini M, Viticchi G, Falsetti L et al (2014) Migraine in health workers: working in a hospital can be considered an advantage? Neurol Sci 35:27–29
Hansen LC, Gaul C, Pogatzki-Zahn E, Baron R, Gierthmühlen J (2020) Do doctors treat themselves differently than their patients? Study on the self-treatment of migraine among German neurologists and pain specialists. Cephalalgia 40(8):788–796
Evers S, Brockmann N, Summ O et al (2020) Primary headache and migraine in headache specialists—does personal history of doctors matter? Cephalalgia 40(1):96–106
Bordini CA, Bigal ME (2006) Migraine in the Elderly: a comparison with migraine in young adults. Headache 46(2):312–316
Wijeratne T, Tang M (2009) Prevalence of migraine in the elderly: a narrated review. Neuroepidemiology 52(1–2):104–110
Starling AJ (2018) Diagnosis and management of headache in older adults. Mayo Clin Proc 93(2):252–262
Wang X, Zhou HB, Sun JM et al (2016) The prevalence of migraine in university students: a systematic review and meta-analysis. Eur J Neurol 23(3):464–475
Acknowledgements
We would like to thank all the doctors who agreed to participate in our study.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
Study concept and design: Sonia Quintas and Inés Muro. Analysis and interpretation of data: Lorena Vega, Inés Muro and Sonia Quintas. Drafting of the manuscript: Inés Muro. Critical revision of the manuscript for important intellectual content: Sonia Quintas, Ana Beatriz Gago-Veiga and Jose Vivancos. Statistical analysis: Lorena Vega and Miguel Ruiz. Study supervision: Sonia Quintas, Ana Beatriz Gago-Veiga and Jose Vivancos.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Ethics approval
The study was approved by the Ethics Committee and hospital’s Medical Direction on April 4th 2019 (reference number 3718).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Muro, I., Gago-Veiga, A.B., Vivancos, J. et al. Are doctors accurate when diagnosing themselves with migraine? A study on migraine prevalence among doctors in a tertiary care hospital. Acta Neurol Belg 121, 1045–1051 (2021). https://doi.org/10.1007/s13760-021-01727-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-021-01727-w