Abstract
There is a growing interest in functional movement disorders (FMD). However, epidemiological data from large cohorts of patients with FMD are scarce and come mainly from General Neurology and Movement Disorders Clinics. Recently, specialized FMD clinics have been developed and epidemiological data from such clinics may provide useful information. We aimed to describe the clinical and sociodemographic features of patients diagnosed with FMD at our specialized FMD clinic. A standardized form was used to extract data from electronic records from the first-100 consecutive patients who were evaluated and diagnosed with FMD at our clinic from 2017 to 2019. Mean age was 40.88 ± (14.02) years, 63% females. Most patients were within working-age range, but only 16% were working at the time of consultation. Mean disease duration was 3.74 ± 5.73 years and was longer among men. The most common FMD were gait disturbance (42%), tremor (22%) and dystonia (15%). A precipitating event (mainly physical) was reported by 74%. The onset was mostly acute (83%) and the clinical course fluctuating (62%). Pain (64%) and fatigue (44%) were common comorbidities. Potential joint-hypermobility was present in 21%, mostly women (90%) and related to the presence of dystonia. FMD affects men and women mostly in working-age. Gait disturbance was the most common diagnosis, possibly because it causes a higher level of disability that may lead to consultation in a specialized clinic. Non-motor symptoms (pain and fatigue) were frequent in this cohort. Further data from specialized units may contribute to both understanding and management of FMD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Functional movement disorders (FMD) are a common presenting complaint to neurology clinics. They are among the broad spectrum of Functional neurological disorders (FND) and encompass a wide variety of clinical manifestations [1]. The prevalence of FND is estimated to be about 16% in new patients referred to neurology outpatient clinics [2], but varies largely depending on the cohort, and “medically unexplained symptoms” can affect up to 60% of patients seeking a neurology consultation [3]. FMD account for 1.5% of all patients seen in neurology clinics and range between 2 and 20% of patients referred to movement disorder outpatient clinics [4]. The only descriptive study from a Neurology hospitalization facility in Spain reported that 1% of patients admitted in the last 10 years received a diagnosis of FND [5].
Although they are common and disabling disorders, they have been surprisingly neglected for years. However, over the past two decades, clinical and scientific interest has revived and the number of scientific publications has increased exponentially. FMD are more frequent in women according to most studies (60–75%) [3]. A recent study described a cohort of 196 patients with FMD and reported that functional dystonia was significantly more frequent in women (47.5 vs. 20.3%, p < 0.001) and there was a trend for higher frequency of functional gait disorder in men [6]. With respect to functional parkinsonism, prevalence has been described to be similar in both sexes [7]. Although the mean age of onset ranges from 37 to 50 years [4], FMD appear in all age groups, including children [8] and the elderly [9]. According to the literature, functional tremor is the most common presentation of FMD [7, 10] accounting for at least half of the patients, followed by dystonia and myoclonus [4] and the presentation is often combined.
The majority of published FMD epidemiological data comes from general neurology services in outpatient [2, 11], hospital settings [5], psychiatry consultations, neurophysiology consultations [12] or movement disorder clinics [6, 13, 14]. The diagnosis of these disorders is challenging due, in part, to recent changes in criteria, variability in the terminology used, and the need to make a diagnosis based on positive clinical signs since ancillary tests are not diagnostic [15]. In recent years, specialized FMD clinics have been developed in some countries and the epidemiological data from these centers, still scarce, may provide useful information [13, 16,17,18].
This study aims to describe the clinical and sociodemographic features of patients diagnosed with FMD at the only specialized FMD clinic in Spain.
Methods
The first 100 consecutive patients evaluated and diagnosed with FMD at our specialized FMD clinic, set in a private medical center in Spain, were included. All patients included were evaluated and diagnosed from Jan 2017 to Dec 2019 by a movement disorders specialist (IP) and fulfilled criteria for clinically definite phenotype-specific diagnosis for FMD [19]. We included patients with comorbidity with another neurological disorder as long as their FMD met the previous diagnostic criteria. We excluded referred patients who after assessment and complementary tests had a diagnosis other than FMD.
The study was approved by the local Ethics Committee. Data were collected in a standardized manner by a neurologist specialized in FMD (IP) in an electronic medical record system during the first consultation and retrospectively extracted from the medical record to be incorporated into the database. Demographic information on age, sex, work situation, education, type and clinical characteristics of FMD, precipitating factors and associated symptoms were included. Professions were classified following the International Standard Classifications of Occupations (ISCO-08) [20]. For purposes of this study, precipitating factors were defined as those occurring within the 3 months prior to the onset of the FMD, including neurological diseases. This three-month time window was arbitrarily defined, following that established in previous studies for reasons of comparability [17]. When FMD occurred in the setting of a neurological disease after the three months temporal window, the comorbidity was recorded, but the neurological disease was not regarded as a physical precipitant. Clinical data recorded in the medical history suggesting potential joint hypermobility (e.g., diagnosis of Ehlers Danlos Syndrome or prior history of two or more recurrent joint luxations/subluxations) was also included.
We analyzed the data by descriptive statistics using means, standard deviation (SD), variances and percentages. Chi-squared (χ2) test and Fisher’s exact test were used to compare the frequencies between groups and Student’s t test or non-parametric tests (Mann–Whitney–Wilcoxon test) according to sample characteristics to compare means. We considered all p values < 0.05 as statistically significant. Data were analyzed using R software (3.6.2 version).
Results
Demographic characteristics are summarized in Table 1. Most patients were referred by their treating neurologists from all over the country (15 different regions) and one from Portugal, 16% were self-referred. The majority of them (63%) were female and mean age at first visit was 40.88 ± 14.02 years. Disease duration at first consultation was approximately 4 years (3.74 ± 5.73 years). Ninety percent were within the working-age range (18–64 years old), but only 16% were working at the time of consultation. Twenty per cent of them had been granted some type of disability. More than one-third (36%) had a university degree. Professions varied greatly and scientific and intellectual professionals (20%) were the most frequent.
FMD and related clinical features are summarized in Table 2. The most common FMD was gait disturbance (42%), followed by tremor (22%) and dystonia (15%). We often found a combination with other FMD (19%), other FND (34%) or other non-neurological functional disorder (such as irritable bowel syndrome or functional cough) (9%). Comorbidity with another neurological disease was present in 22% of the patients.
A total of 74 patients reported a physical or psychological precipitating event within three months prior to onset of the FMD. Of these, 59 (80%) reported a physical event. The most frequent among them were physical injury in 14 (23%) patients, neurological disorder in 12 (20%), surgical intervention or invasive procedure in 9 (15%) and pain without specific injury in 7 (11%). The neurological disorders considered as physical precipitants (reported up to three months prior to the onset of FMD) were: peripheral facial palsy (n = 3), migraine episode (n = 3), Miller Fisher Syndrome (n = 1), Parkinson’s disease onset (n = 1), ruptured vermian lipoma (n = 1), trigeminal neuralgia (n = 1), peripheral nerve palsy (n = 1) and demyelinating peripheral neuropathy (n = 1). In seven patients, the FMD started after a mild infection (most commonly acute gastroenteritis or flu-like symptoms), and in three patients after an adverse event related to medication. Peripheral vertigo and syncope were reported by five patients and two presented worsening of chronic non-neurological disease. We found no association between the type of physical event and the type of FMD, but in fixed limb dystonia (n = 7), we found a higher frequency in women (86%) and previous physical injury affecting the limb that developed fixed dystonia in 5 (71%), with chronic local pain in 6 (86%) of them. Psychological relevant events prior to the onset of FMD (including personal, familiar and work related difficulties) were reported by 15 patients (20%).
Time from precipitating event to onset of FMD was: within one day in 26 (35%) patients, between one day and one week in 14 (19%) patients, between one week and one month in 18 (24%) patients and between one month and three months in 9 (12%) patients. Seven patients could not specify the exact time interval even though the precipitating event occurred within the first three months. Three patients reported a physical injury, followed by chronic pain prior the onset, but they were not included because the FMD started about a year later.
The onset of the FMD was acute (within one day) in most patients (83%) and 62% exhibited a fluctuating clinical course (characterized by frequent exacerbations and attenuation of symptoms). Fifteen patients (15%) presented periods of complete remission over the course of the disease. We found that both generalized and/or localized pain in the affected limb (64%) and fatigue (44%) were frequently reported comorbidities. Clinical features in the medical history suggesting potential joint hypermobility were present in 21% of patients, mostly women (n = 19 (90%) vs. men n = 2 (9%), χ2 = 7.18, p = 0.0074) and related to the presence of dystonia (47% of patients with dystonia vs 16% among the rest of FMD, χ2 = 5.31, p = 0.0212), especially in those with fixed limb dystonia (71% of patients with fixed limb dystonia vs 17% among the rest of FMD, χ2 = 8.50, p = 0.0035).
As for psychiatric comorbidity, 55% had been assessed by a psychiatrist and 34% by a psychologist prior to the first consultation in our unit. A total of 59% were on antidepressants or anxiolytic medications at the time of the first assessment. Nearly a third of the whole cohort (34%) had been diagnosed with a psychiatric condition, most frequently depression (n = 20, 59%, including major depression, dysthymia, and adjustment depressive disorder) and anxiety (n = 7, 21%, including generalized anxiety disorder, and panic attacks). None of them referred a previous diagnosis of personality disorder.
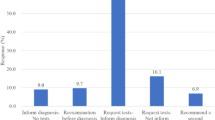
When analyzing our cohort by gender, we found that women were overrepresented (63%), and they tended to be younger than men, at both onset of the FMD (t = 1.93, p = 0.057), and the first evaluation (t = 2.33, p = 0.022). When considering only patients under 18 years old (n = 12), men were still underrepresented (n = 2, 17%), but this gender difference disappeared in patients over 50 years old (48% were women and 52% were men). Men tended to have longer symptoms duration at the time of the first visit compared to women (mean 3.1 vs. 4.7 years) although this difference did not reach statistical significance (W = 1421, p = 0.07). We found a higher educational level among women (42% women vs. 28% men had a university degree), but the result was not statistically significant and no difference in working situation. The most frequent FMD in both sexes was gait disorder, followed by tremor and dystonia [Fig. 1]. No significant differences were found in movement phenotypes between women and men. Additional clinical features can be found in Fig. 2. Overall, women tended to report a precipitating factor more frequently than men (69 vs. 31%) mostly physical, but this trend did not reach statistical significance (χ2 = 3.36, p = 0.067). We found no difference in the frequency of reported emotional precipitating factor prior to onset of the FMD between genders. There were no differences between women and men regarding the diagnosis of psychiatric comorbidity prior to the first consultation in our unit.
Discussion
In this study, we describe the demographic and clinical characteristics of 100 consecutive patients with FMD specifically referred to the only Functional Movement Disorder Unit in Spain. Similar to previous studies, we found that women were clearly overrepresented [3], but interestingly, this difference vanished in the subgroup of patients over 50 years old. This had been published in patients with non-epileptic seizures [21], but has been only recently acknowledged in patients with FMD [6].
Although some clinical and demographic features reported in our cohort are in line with previous cohorts of patients with FMD, it has particular characteristics and we found some differences with the existing literature. For instance, functional gait disturbance represented almost half of our patients, differing from most published cohorts where tremor is the most common phenotype, followed by dystonia [4, 7, 10]. We hypothesize that this may be due to a severity selection bias. Gait disturbances are very disabling and have an impact in day-to-day life due to mobility impairment. In fact, 90% of patients with gait disorders in our sample were unemployed or on sick leave. A recent study also described patients with functional gait disorder as having worse physical functioning than those with functional tremor and functional myoclonus [22]. Our results are similar to other patient cohorts from specialized FMD clinics where gait disturbance was also widely overrepresented, suggesting that this FMD subtype may be more susceptible to be referred to a specialized FMD clinic [16, 18].
We found a high frequency of precipitating factors, mostly physical, while life events or psychological triggers were less commonly reported. These findings are in line with other publications. A systematic review described the presence of physical precipitants in 37% of patients [23], although it has been reported to be as high as 80% [17]. These differences may be due to recall bias or methodological differences such as time threshold (set to 3 months prior to FMD onset in our cohort). It should also be noted that any significant physical trauma can also be a psychologically significant life event, such as a traffic accident, making it difficult to differentiate between the two. It is also important to take into account that alexithymia, defined as the inability to identify and describe emotions, is common in patients with FMD [24] and this may also influence the reporting of emotional events in the first consultation. We did not find a greater report of psychological triggers among women, unlike what has been previously reported in other studies [6] nor a greater rate of psychiatric comorbidity diagnosis at first consultation in our Unit.
Non-motor symptoms are common in patients with FMD. Pain seems to play an important role in our cohort as it is present in the majority of patients. The adaptation of movement to pain is a physiological reaction. However, it has been proposed that this normal adaptation can lead to a distortion of incoming sensory information through negative reinforcement mechanisms and supported by excessive self-monitoring, distorted expectations and avoidance maneuvers. Pain has been proposed to underlie chronic dysfunction in FMD [25], and is associated with a worse prognosis [13, 26].
Longer symptoms duration has also been associated with poor prognosis [14, 27]. In our sample, the average time to specialized consultation was almost 4 years, similarly to that reported in a clinic in Switzerland and somewhat less than in other specific FMD clinics [16]. Men had a longer symptoms duration compared to women, suggesting this may be a gender bias and that perhaps physicians still show greater reluctance in diagnosing men with a FND.
We found that 21% of patients in our cohort had clinical features suggestive of joint hypermobility, especially those with fixed limb dystonia. This prevalence is higher than the 10–15% seen in the general population [28]. It has been hypothesized that abnormal range of joint mobility can lead to physical injury, chronic pain and maladaptive maneuvers, and thus join hypermobility may be a relevant factor in the pathophysiology of fixed dystonia [28]. However, the small sample size and the fact that we did not use a standardized questionnaire and scale to diagnose joint hypermobility syndrome, are limiting factors and thus entail caution in interpreting our results. However, our findings suggest that future research should investigate joint hypermobility syndromes as potential predisposing factors for FMD.
Finally, it should be noted that the majority of our patients were in working-age and had a high-unemployment rate, supporting recent evidence that FND generates greater disability and financial costs to healthcare/welfare systems [2, 3]. Referrals to our clinic from 15 different regions in Spain and one from Portugal highlights the need to seek specialized assistance among this patient population.
We acknowledge limitations in our study. Data were collected in a standardized manner and extracted into a database retrospectively. Data were based on patient self-report and clinical letters from previous specialists and there may be recall biases, especially regarding precipitating factors or onset times. No specific questionnaires or scales were used to measure psychiatric comorbidity or hypermobility as already mentioned.
Finally, we have tried to minimize biases by including consecutive patients, but our sample probably does not represent the general population in Spain due to an economic selection bias. Our specialized clinic is in a private hospital while the predominant health care system in Spain is public. Therefore, it is likely that more severe, disabling and long-standing cases with the financial means to invest in seeking help are overrepresented in our cohort. Also, most patients in our cohort had a secondary or university degree and a specialized job. Although this is also likely to be related to a selection bias, our cohort exemplifies that all strata of occupations and educational attainment are represented in the spectrum of FND, in contrast to historically established views where lower social and education levels are more prevalent [29].
In conclusion, our cohort’s data suggests that FMD are frequent and disabling and affect all population strata universally, in terms of gender, age, educational background and profession. Interest in these disorders has been revived in recent decades resulting in the creation of specialized clinics. Clinical and demographic data from specialized units may lead to more homogeneous and thoroughly evaluated cohorts and thus helps to further our understanding and management of these enigmatic disorders.
References
Hallett M (2016) Functional (psychogenic) movement disorders—clinical presentations. Parkinsonism Relat Disord. 22(Suppl 1):S149–S152
Stone J, Carson A, Duncan R, Roberts R, Warlow C, Hibberd C, Coleman R, Cull R, Murray G, Pelosi A, Cavanagh J, Matthews K, Goldbeck R, Smyth R, Walker J, Sharpe M (2010) Who is referred to neurology clinics?–The diagnoses made in 3781 new patients. Clin Neurol Neurosurg 112(9):747–751
Carson A, Lehn A (2016) Epidemiology. Handb Clin Neurol 139:47–60
Factor SA, Podskalny GD, Molho ES (1995) Psychogenic movement disorders: frequency, clinical profile, and characteristics. J Neurol Neurosurg Psychiatry 59(4):406–412
De la Cruz-Cosme C, Barbieri G, Avanesi-Molina E, Romero-Acebal M (2011) Psychogenic pathology in the neurology unit. A review of the hospital admissions over the last 10 years in a third-level service. Rev Neurol. 53(11):649–656
Baizabal-Carvallo JF, Jankovic J (2019) Gender differences in functional movement disorders. Mov Disord Clin Pract 7(2):182–187 (Published 2019 Dec 24)
Bhatia KP, Schneider SA (2007) Psychogenic tremor and related disorders. J Neurol 254(5):569–574
Harris SR (2019) Psychogenic movement disorders in children and adolescents: an update. Eur J Pediatr 178(4):581–585
Dehoust MC, Schulz H, Härter M, Volkert J, Sehner S, Drabik A, Wegscheider K, Canuto A, Weber K, Crawford M, Quirk A, Grassi L, DaRonch C, Munoz M, Ausin B, Santos-Olmo A, Shalev A, Rotenstein O, Hershkowitz Y, Strehle J, Wittchen HU, Andreas S (2017) Prevalence and correlates of somatoform disorders in the elderly: results of a European study. Int J Methods Psychiatr Res 26(1):e1550
Schwingenschuh P, Deuschl G (2016) Functional tremor. Handb Clin Neurol 139:229–233
Park JE (2018) Clinical characteristics of functional movement disorders: a cclinic-based study. Tremor Other Hyperkinet Mov (NY) 8:504
Garcin B (2018) Motor functional neurological disorders: an update. Rev Neurol (Paris) 174(4):203–211
Glass SP, Matin N, Williams B, Mello J, Stephen CD, Young SS, Callahan J, LaFrance WC Jr, Perez DL (2018) Neuropsychiatric factors linked to adherence and short-term outcome in a U.S. functional neurological disorders clinic: a retrospective cohort study. J Neuropsychiatry Clin Neurosci. 30(2):152–159
Thomas M, Vuong KD, Jankovic J (2006) Long-term prognosis of patients with psychogenic movement disorders. Parkinsonism Relat Disord 12(6):382–387
Espay AJ, Aybek S, Carson A, Edwards MJ, Goldstein LH, Hallett M, LaFaver K, LaFrance WC Jr, Lang AE, Nicholson T, Nielsen G, Reuber M, Voon V, Stone J, Morgante F (2018) Current concepts in diagnosis and treatment of functional neurological disorders. JAMA Neurol 75(9):1132–1141
Aybek S, Lidstone SC, Nielsen G, MacGillivray L, Bassetti CL, Lang AE, Edwards MJ (2020) What is the role of a specialist assessment clinic for FND? Lessons from Three National Referral Centers. J Neuropsychiatry Clin Neurosci. 32(1):79–84
Pareés I, Kojovic M, Pires C, Rubio-Agusti I, Saifee TA, Sadnicka A, Kassavetis P, Macerollo A, Bhatia KP, Carson A, Stone J, Edwards MJ (2014) Physical precipitating factors in functional movement disorders. J Neurol Sci 338(1–2):174–177
Jacob AE, Smith CA, Jablonski ME, Roach AR, Paper KM, Kaelin DL, Stretz-Thurmond D, LaFaver K (2018) Multidisciplinary clinic for functional movement disorders (FMD): 1-year experience from a single centre. J Neurol Neurosurg Psychiatry 89(9):1011–1012
Espay AJ, Lang AE (2015) Phenotype-specific diagnosis of functional (psychogenic) movement disorders. Curr Neurol Neurosci Rep 15(6):32
International Standard Classification of Occupations (2012) ISCO-08. International Labour Office, Geneva
Duncan R, Oto M, Martin E, Pelosi A (2006) Late onset psychogenic nonepileptic attacks. Neurology 66(11):1644–1647
Gelauff JM, Rosmalen JGM, Gardien J, Stone J, Tijssen MAJ (2020) Shared demographics and comorbidities in different functional motor disorders. Parkinsonism Relat Disord 70:1–6
Stone J, Carson A, Aditya H, Prescott R, Zaubi M, Warlow C, Sharpe M (2009) The role of physical injury in motor and sensory conversion symptoms: a systematic and narrative review. J Psychosom Res 66(5):383–390
Demartini B, Petrochilos P, Ricciardi L, Price G, Edwards MJ, Joyce E (2014) The role of alexithymia in the development of functional motor symptoms (conversion disorder). J Neurol Neurosurg Psychiatry 85(10):1132–1137
Edwards MJ, Adams RA, Brown H, Pareés I, Friston KJ (2012) A Bayesian account of ‘hysteria.’ Brain 135(Pt 11):3495–3512
Stone J, Carson A, Duncan R, Coleman R, Roberts R, Warlow C, Hibberd C, Murray G, Cull R, Pelosi A, Cavanagh J, Matthews K, Goldbeck R, Smyth R, Walker J, Macmahon AD, Sharpe M (2009) Symptoms ‘unexplained by organic disease’ in 1144 new neurology out-patients: how often does the diagnosis change at follow-up? Brain 132(Pt 10):2878–2888
Gelauff J, Stone J, Edwards M, Carson A (2014) The prognosis of functional (psychogenic) motor symptoms: a systematic review. J Neurol Neurosurg Psychiatry 85(2):220–226
Kassavetis P, Batla A, Pareés I, Saifee TA, Schrag A, Cordivari C, Bhatia KP, Edwards MJ (2012) Joint hypermobility syndrome: a risk factor for fixed dystonia? Mov Disord 27(8):1070
Tasca C, Rapetti M, Carta MG, Fadda B (2012) Women and hysteria in the history of mental health. Clin Pract Epidemiol Ment Health 8:110–119
Acknowledgements
We would like to acknowledge all our patients and their families for placing their trust in us and making this project possible.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Celia Delgado, Monica Kurtis and Isabel Pareés. The first draft of the manuscript was written by Celia Delgado and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest. C.D. has received travel expenses to attend scientific meetings from Alter and Bial. M.M.K. has received honoraria for talks from Bial and International Parkinsonism and Movement Disorder Society, and travel expenses to attend scientific meetings from Boston Scientific; she is currently participating in a Michael J. Fox Grant. I.P. has received travel expenses to attend scientific meetings from Neuroaxpharm and International Parkinsonism and Movement Disorder Society and honoraria for speaking at meetings from Allergan, and International Parkinsonism and Movement Disorders Society.
Ethical approval
This study was approved by the Ruber International Hospital Clinical Research Ethics Committee and has therefore been performed in accordance with the ethical standards laid down in the 1964 declaration of Helsinki and its later amendments. All the data obtained were anonymized. Informed patient consent was not necessary for this work. We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this work is consistent with those guidelines.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Delgado, C., Kurtis, M., Martin, B. et al. Clinical and demographic characteristics of patients with functional movement disorders: a consecutive cohort study from a specialized clinic. Acta Neurol Belg 122, 97–103 (2022). https://doi.org/10.1007/s13760-021-01648-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-021-01648-8