Abstract
Central pontine myelinolysis and extrapontine myelinolysis are collectively called the osmotic demyelination syndromes. Despite being described in 1959, there are several aspects of the disorder that remain an enigma. Animal models and neuroimaging techniques have allowed us to understand the condition better. From being a universally fatal disorder that was diagnosed post mortem, increased awareness, neuroimaging techniques and supportive care have enabled us to make the diagnosis ante-mortem. This has also led to a significant drop in associated mortality. The aim of this review is to highlight the clinical spectrum, neuroimaging findings, and recent developments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adams et al., first described central pontine myelinolysis as a clinicopathological entity in 1959. Several outstanding reviews have been published subsequently on the disorder over the years. Although some authors call the spectrum of both central pontine myelinolysis and extra pontine myelinolysis collectively as osmotic demyelination syndromes, the original authors were very clear in their paper why they wanted to avoid the term demyelination. Adams et al., reasoned that in this hitherto peculiar disorder, the myelin loss was not associated with inflammation. They wanted to differentiate the pathology of this condition from multiple sclerosis and other neuroinflammatory disorders in which myelin loss was associated with inflammation. When they described the condition, the authors hypothesised the underlying cause to be either a toxin related or due to a nutritional deficiency [1]. For the purpose of this review and to avoid confusion, the author uses the terminology ‘osmotic demyelination syndrome’ (ODS) in relevant sections when there is need to encompass both central pontine and extrapontine myelinolysis.
Clinical presentation
With key developments since the original description, it has become clear that there is no classical presentation of osmotic demyelination syndromes. The presentation is multifaceted and diverse. It is important for the clinician to be aware of the distinct clinical presentations.
Asymptomatic
Since the original description of cases, it is now known from autopsy findings and clinical cases, that many are asymptomatic [2,3,4]. Asymptomatic central pontine myelinolysis was found in 21 out of 220 autopsies of consecutive patients with chronic liver disease [5]. A 12-year retrospective analysis involving review at autopsies of 3247 brains, revealed 15 cases of central pontine myelinolysis. This analysis suggested an overall incidence of 0.5% of the cases, emphasising that a large proportion of cases maybe asymptomatic if not the majority [6]. It remains to be seen whether asymptomatic cases represent a different pathophysiological mechanism as opposed to the vast majority of symptomatic cases that appear to be iatrogenic. The difference in prognosis between asymptomatic and iatrogenic cases is not known.
Acute encephalopathy
An initial encephalopathic stage is described in several cases of iatrogenic osmotic demyelination syndromes during electrolyte shifts.
Flaccid quadriparesis or quadriplegia
This phase is usually seen within the first 5 days of onset of symptoms. An initial phase of flaccid quadriparesis along with dysarthria and dysphagia can be seen. During this phase, the patient may be able to moves their eyes to command, suggestive of a ‘locked-in’ state. This is thought to be due to abrupt disruption of the corticospinal tracts and spinal shock. A lesion in the pons can explain these clinical features [1, 7].
Spastic quadriparesis or quadriplegia
By about the fifth day from the onset of symptoms, once the disruption in the corticospinal tracts gets firmly established, upper motor neuron signs may become prominent. The patient may have increased tone, brisk reflexes, clonus and positive Babinski sign [1, 7].
Pseudobulbar effect
Due to disruption of corticobulbar tracts within the pons, the patient may have difficulty with speech and swallowing [1].
Movement disorders
Various movement disorders are being increasingly being reported with osmotic demyelination syndromes especially when there is extrapontine myelinolysis. Due to basal ganglia involvement, symptoms like tremor, chorea, dystonia, ataxia, mutism and catatonia have been reported. Involuntary slow writhing and jerking movements of the anterior abdominal wall (known as belly dancer’s syndrome) occurring in conjunction with osmotic demyelination syndrome has also been reported (see Fig. 3) [8,9,10].
Death
When the syndrome was first described, the fatality was total and the cases all being diagnosed post-mortem. Death was reported usually by around day 13 following onset of symptoms. However, with improved awareness, intensive care access and neuroimaging, cases are now mostly detected ante-mortem and there has been a dramatic decline in mortality. This will be further discussed in the section on prognosis.
The ‘plastic revolution’
Since the description of cases by Adams et al., in their seminal paper published in 1959, there was been an explosion in cases reported worldwide [11, 12]. The location of the lesions is such that, it could not have been missed by pathologists had it occurred more frequently prior to 1959. It is thought that the increase in cases worldwide were down to the rampant use of intravenous fluids at the time, the so called ‘plastic revolution.’ The routine availability of serum electrolyte measurements may have also played a part. With the availability of this, sustained therapeutic interventions by clinicians to ‘normalise’ sodium levels using intravenous fluids may have contributed to the increased incidence of myelinolysis [8, 13, 14]. The author would like to coin this the ‘restless electrolyte correction syndrome’ amongst clinicians when there maybe the urge to correct electrolyte levels in situations where this may not be necessary.
Risk factors
Chronic alcoholism
Chronic alcoholism has consistently featured in association with osmotic demyelination syndromes in up to 40 percent of cases reported [8, 15]. The exact mechanism through which chronic alcoholism contributes to the syndrome remains to be elucidated. Possible explanations include disruption of sodium regulation, malnutrition, advent of hepatic cirrhosis and dysregulation of antidiuretic hormone (ADH) [8, 15].
Malnutrition
Malnutrition has also been commonly reported in association with central pontine myelinolysis, usually in conjunction with chronic alcoholism. The presence of Marchiafava-Bignami disease and Wernicke-Korsakoff syndrome in in up to 30% of autopsy specimens of patients with osmotic demyelination disorders suggests that nutritional deficiencies especially thiamine deficiency may have a role in the development of osmotic demyelination disorders. Adams et al., speculated a nutritional deficiency as the most likely cause for this disorder as their four canonical cases had underlying chronic alcoholism or malnutrition [1, 8].
Hyponatremia
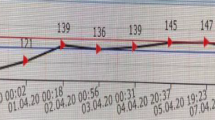
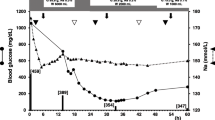
The association between rapid rises in serum sodium from baseline hyponatremia as a causative factor for central pontine myelinolysis was suggested by Norenberg et al. [16]. Subsequently, rapid correction of hyponatremia leading to experimentally induced central pontine myelinolysis was shown in an animal study involving 60 dogs. The dogs were rendered hyponatraemic by the administration of intramuscular vasopressin (antidiuretic hormone) and intraperitoneal administration of 2 litres of water. Amongst the animals that survived the sustained hyponatremia for at least 4 days, they were divided into four groups A, B, C and D based on the intervention carried out (i.e., uncorrected hyponatremia, hypertonic saline infusion in normal dogs, hyponatremia treated with water restriction and hyponatremia treated with hypertonic saline, respectively). Following autopsy, 50% (5/10) dogs with hyponatremia who underwent correction with hypertonic saline (Group D), were found to have autopsy findings consistent with myelinolysis [14].
A retrospective analysis of 1490 patients admitted with sodium of less than < 120 mEq/L underwent rapid correction in around 41% of the cases. The authors defined rapid correction as an increase of sodium by more than 8 mEq/L in a 24-h period. Amongst the patients who underwent rapid correction, approximately 1% developed osmotic demyelination syndrome [17].
Liver transplantation
Liver transplantation constitutes around 17% of cases reported of osmotic demyelination disorders since 1986. In a study involving 1730 consecutive liver transplant patients, about 8% had radiological documented central nervous system lesions consistent with central pontine myelinolysis [18].
Hypokalaemia
Hypokalaemia has been reported in association with osmotic demyelination syndromes. The very first canonical case described by Adams et al., was found to have hypokalaemia [14]. Several cases have been reported in literature since [7, 19, 20]. Association with hypokalaemia was also suggested in a literature review of osmotic demyelination syndrome. Out of 74 cases in which both serum potassium and sodium were measured at presentation, 89% of cases had documented hypokalaemia. The sodium pump (Na–K-ATPase) located in the cell membrane is responsible for transporting potassium into cells by exchanging sodium and is integral in regulation of cell volume. Reduced Na–K-ATPase activity during hypokalaemia may impact the ability of the cell membrane to preserve its volume against rapid changes in osmolality during correction of hyponatremia. This may lead to cell shrinkage and apoptosis. Hence there is a case for concurrent measurement and correction of electrolytes to reduce the impact of osmotic demyelination [7, 21].
Refeeding syndrome
Several clinical complications can occur during aggressive nutritional correction in malnourished patients due to rapid fluid and electrolyte shifts. This is collectively called refeeding syndrome. Deficiencies maybe seen in phosphate, magnesium, glucose, vitamins (especially thiamine) and sodium. Trying to replete the deficiencies quickly can be complicated by congestive heart failure, pulmonary oedema, cardiac arrhythmias, seizures and death [22, 23]. Osmotic demyelination syndrome has been reported in the context of refeeding syndrome [7, 24]. With rapid gradient shifts in osmoles associated with both refeeding syndrome and osmotic demyelination disorders, it remains to be seen whether osmotic demyelination syndrome is a central nervous system manifestation of refeeding syndrome [25]. Rapid electrolyte shifts may place a severe strain on the energy deprived glial cells in the brain. This can set off a cascade leading to glutamate receptor stimulation, opening up calcium channels, mitochondrial permeability and ultimately initiate apoptosis [26].
Others
Osmotic demyelination syndrome has also been reported in the context of burns. In a study of 139 burns patients that underwent autopsy over a 17-year period, 7% (n = 10) were found to have findings consistent with central pontine myelinolysis [27]. It has also been reported in hyperemesis gravidarum [12]. The syndrome has also been reported in the contexts of rapid shifts in serum glucose [28,29,30]. Other less common conditions in which osmotic demyelination disorders have been reported include autoimmune disorders (Sjögren's syndrome and systemic lupus erythematosus), HIV, acute intermittent porphyria, anaphylactic shock and cytomegalovirus hepatitis, brain tumours, Hodgkin’s disease, craniopharyngioma, renal disease, sepsis, Wilson’s disease, sickle cell disease, adrenal insufficiency, congestive heart failure, liver failure and chemotherapy [15, 26].
Pathogenesis
The exact mechanisms involved in causing osmotic demyelination syndromes in not known. Serum sodium is a key determinant of effective serum osmolality. Though the initial connection with electrolyte disturbances is usually attributed to Finlayson [31] or Tomlinson [32], it was Norenberg and colleagues who showed the association with hyponatremia using compelling evidence from a case series of 12 patients [16]. Laureno was successful in experimentally inducing myelinolysis using animal models that established rapid correction of hyponatremia as a key causative factor [14].
Osmolality is the concentration of a solution in terms of osmoles of solute per kilogram of solvent. Hence plasma osmolality alludes to the quantity of solute that is dissolved in 1 kilogram of plasma. Serum sodium is a key determinant of effective serum osmolality. In the equilibrium state, extracellular osmolality and intracellular osmolality remains the same. There is null net movement across the cell membrane. When serum sodium concentration drops, extracellular osmolality reduces as a result. As a consequence, water moves from the extracellular space into the intracellular compartment. Hence hypotonicity can cause the cell to swell and hypertonicity will lead to cell shrinkage as water moves from inside to outside. The development of symptoms will depend on the speed at which the change occurs and whether these overwhelm the brain’s adaptive mechanisms. One of the earliest defence mechanisms of the brain against hypotonicity that comes into play, is the shift of interstitial sodium rich fluid from the brain parenchyma, to the cerebrospinal fluid (CSF) and subsequently to systemic circulation through hydrostatic pressure. This measure serves to protect the brain from rapid oedema. Within the first hours of resultant hyponatremia, there is a significant decrease in the intracellular content of sodium, chloride, and potassium [8, 33].
As a late mechanism of brain adaptation to chronic hyponatremia, it has been shown in a rat model that after 4 days, brain electrolyte content reduced by 33%, 11%, and 17% for chloride, sodium, and potassium, respectively. However, the brain water content only increased by 0.6% [33, 34]. The loss of organic osmoles like myoinisotol, taurine and glutamate over the next day to the next few days, renders the cell isotonic compared to extracellular space and ensures maintenance of cell volume [8].
It is thought that rapid correction of established hyponatremia may disrupt the blood brain barrier, leading to accumulation of cytokines and complement factors. In experimental models, the astrocytes and oligodendroglia seem particularly susceptible to the osmotic stress [35].
These pathophysiological mechanisms provide an explanation for osmotic demyelination syndromes in the context of rapid correction of hyponatremia. However, the occurrence of the disorder in conditions where the serum sodium is normal suggest other important yet unknown mechanisms maybe at play.
Imaging
Conventional imaging (CT and MRI) may lag behind clinical manifestations but have allowed ante-mortem diagnosis and management of osmotic demyelination disorders. Though CT is less sensitive than MRI imaging in detecting early changes, occasionally a reduced attenuation within the pons may be seen (see Fig. 1) [7]. MRI imaging may show a symmetric signal intensity abnormality in the central pons with T2-weighted and FLAIR imaging (see Fig. 3). Early diagnosis of central pontine myelinolysis may be made with diffusion-weighted imaging (DWI) [36]. In a study looking at the outcome of patients with central pontine and extra pontine myelinolysis (n = 44) magnetic resonance imaging findings offered no prognostic significance. The extent of the pontine lesions seen on the scans did not co-relate with the severity of clinical findings during the acute phase of disease. Neither did the persistence of the pontine lesions seen on magnetic resonance imaging correlate with clinical improvement [37]. Another aspect worth stressing is that not all pontine lesions seen by neuroimaging represents central pontine myelinolysis and taking a clinical history is paramount [38]. Functional imaging studies in central pontine myelinolysis have shown hypermetabolism in the brainstem [26]. Fluorine‐18‐fuorodeoxyglucose (F‐18‐FDG) positron emission tomography/computed tomography (PET/CT) has shown showed localized uptake in the pons consistent with magnetic resonance imaging findings [39, 40]. Functional imaging may provide a vital role in the diagnosis and monitoring of patients with osmotic demyelination syndromes in the future (Fig. 4). These modalities need further investigation.
a, b Magnetic resonance imaging (MRI) Brain scans confirming the diagnosis of central pontine myelinolysis showing the increased T2 weighted signal in the central pons [7]
A case of Belly Dancer’s Syndrome Following Central Pontine and Extrapontine Myelinolysis. T2-weighted MRI Brain scans obtained 1 day after symptom onset (a) showed characteristic bilateral hyperintensities in the central pons (left panel) as well as bilaterally in the caudate nucleus and the putamen (right panel). The follow-up T2-weighted MRI scan 5 months later (b) demonstrated unchanged pontine signal alterations (left panel) but incomplete disappearance of basal ganglia lesions (right panel). Abnormal hyperintensities indicated by arrows [9]
18F-FDG PET/CT scan of a 51-year-old Caucasian female with symptoms of central pontine myelinolysis. Scan shows localized FDG uptake in the pons, with normal and symmetrical activity in the rest of the brain [40]. (Creative Commons Attribution-Non Commercial-ShareAlike License (CC BY-NC-SA))
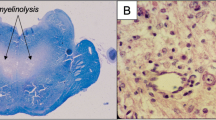
Histopathology
Autopsy findings show that central pontine myelinolysis predominantly involves the basis pontis. Histology shows evidence of demyelination, with sections stained for myelin usually showing a sharply demarcated pallor in the centre of basis pontis. The original authors described the loss of oligodendrocytes with sparing of axons and nerve cells except at the very center. Inflammation was absent [1, 2, 15]. Within a few years following the description of central pontine myelinolysis, it became apparent that similar lesions could also involve extrapontine sites like cerebellum, lateral geniculate body, external capsules, hippocampus, putamen, thalamus and caudate nucleus. Unusual sites include spinal cord, mamillary bodies, amygdala and subthalamic nucleus [15]. Subsequent animal models have undergone detailed microscopic evaluations and the findings are similar to autopsy findings in humans. Animal models have shown early opening of the blood brain barrier which may constitute the initial injury. Animal models have also suggested that microglial activity and consequent release of cytokines may accentuate myelin destruction [15]. See Fig. 5 for histopathology findings in a case of chronic asymptomatic central pontine myelinolysis with histological evidence of remyelination.
a Post-mortem image of the fresh pons and medulla, opened sagitally from the ventral aspect. A red, central, triangular region of softening is seen with preservation of the surrounding parenchyma. b Sagittal T1 and c Axial T2 ante-mortem MRI sequences. The pons includes a trident-shaped focus of high T2 signal. Cerebellar atrophy is also noted, in keeping with the history of alcoholism. d Hypercellular pontine tissue, reflecting astrocytic gliosis and perivascular and parenchymal accumulation of chronic inflammatory cells (scale bar = 200 μm). e Staining with luxol fast blue and cresyl violet revealed a sharply demarcated region of reduced staining of myelin in the central part of the base of the pons, with good preservation of neurons (scale bar = 200 μm). f, g There was reduced labelling of myelin with anti- PLP1 in the affected region of pons (scale bar = 200 μm). h Included within this region were many large-calibre but thinly myelinated axons (blue arrowhead), in contrast to the normally myelinated, large-calibre fibres in the adjacent pons (green arrowhead) (scale bar = 50 μm). Reproduced with kind permission from the author. (http://creativecommons.org/licenses/by/4.0/). [2]
Why the pons and the extrapontine regions?
Ever since the first description of the condition, scientists have found it very intriguing and peculiar, the distribution and localisation of the lesions. Several explanations have been put forward to explain this. One theory suggests the ‘grid’ like intertwining longitudinal and transverse fibres within the pontine basis is prone to myelinolysis when oedematous. This arrangement may severely impact mechanical flexibility during osmotic stress [13]. Another proposed hypothesis based on a rat model is the blood–brain barrier breakdown which results in oedema within the highly vascular gray matter regions involved. The resultant oedema could damage the neighbouring white matter tracts [41,42,43,44]. The vascular supply to the central pons may also be a crucial factor. The perforating branches of the basilar artery supplies the region. These vessels have a low pressure differential and leading to poor perfusion of the central pons which may be exacerbated by any metabolic rearrangements [26]. These hypotheses do not take into account the extrapontine involvement. The localisation and activity of Na+/K+-ATPase pump activity, the role of glutamate and other excitatory molecules in the context of osmotic stress needs to be explored further to clarify whether these mechanisms provide the ultimate induction to apoptotic cell death in osmotic demyelination syndromes [15, 26]. Functional imaging studies may provide more clues in the future.
Management
Most management strategies for osmotic demyelination syndromes are centred around sodium levels. In patients with established hyponatremia, cerebral adaptation during very severe hyponatremia (e.g., < 105 mEq/L) requires higher depletion of brain organic osmolytes. These organic osmolytes cannot be replenished quickly with rapid correction of sodium and hence patients are more likely to develop ODS after rapid correction. The management strategies can be discussed under prevention and treatment.
Prevention
In patients at risk for osmotic demyelination syndrome like chronic alcoholics, malnourished, chronic hyponatremia (when hyponatremia is present for 3 or more days) and patients with severe liver disease, rapid correction of sodium must be avoided. Unless there is a strong history to suggest water intoxication, if the duration of hyponatremia is not known, it would be best for the clinician to assume that this is chronic. The traditional consensus figure amongst neurologists is not to correct chronic hyponatremia in excess of 8 mmol/L/day. However, there are no randomized controlled trials to guide correction. These figures are largely derived from animal models and some observational studies in humans [8, 14, 15, 45]. It is important to bear in mind that meticulous correction of hyponatremia may not stop the occurrence of osmotic demyelination disorders [15]. Factors like unrecognized hypovolemia and other reversible causes of water retention may lead to inadvertent overcorrection of sodium despite careful monitoring of sodium levels [46].
Treatment
Patients who have confirmed osmotic demyelination syndrome clinically and radiologically should have intensive supportive therapy involving various specialists. These may include neurologists, intensive care specialists, physiotherapists, speech and language therapists (SALT) and dietitians. No clinical trials exist to guide treatment once the syndrome has established. Reinduction of hyponatremia using desmopressin has led to complete recovery in some cases with complete resolution of MRI lesions in one case when initiated within 24 h of the onset of symptoms [47, 48]. There is currently no evidence in re-lowering sodium levels 24 h after the onset of symptoms.
Plasmapheresis has been tried in cases with reports of good outcome. It is thought that plasmapheresis may reduce high molecular myelinotoxic substances thereby contributing to clinical improvement [49, 50]. Intravenous immunoglobulins (IVIG) have also been used in osmotic demyelination syndromes with reports of good outcomes. The clinical effect of IVIG in this situation is assumed to be caused by the reduction of myelinotoxic substances and the promotion of remyelination [51,52,53,54].
Animal models suggest myoinisotol administration improves survival and reduces myelinolysis after rapid correction of chronic hyponatremia. More studies are needed to evaluate the role of myoinisotol as a potential therapeutic agent [55].
It is not possible to overemphasise the importance of good supportive care for patients with confirmed osmotic demyelination syndrome. With aggressive supportive therapy, patients may survive with minimal neurological sequelae. Potential secondary complications need to be anticipated like aspiration pneumonia and respiratory paralysis with immediate ventilatory support at the advent of respiratory failure. With good supportive care, patients can have a favourable outcome [7, 56]
Patients with history of alcoholism or malnutrition may lack sufficient reserve supply of glucose to maintain Na–K-ATPase pump activity, the primary mechanism responsible for electron transport in the brain. Subclinical thiamine deficiency may exacerbate this problem [15, 26]. Hence thiamine should be considered in patients with history of chronic alcoholism or malnutrition.
Prognosis
Prognosis used to be considered poor and universally fatal. However, since the initial description of the conditions, the prognosis has continued to improve with patient mortality of only 7% of cases from 1990 onwards according to one study. From what used to be an autopsy diagnosed disorder, modern imaging techniques have ensured that the condition can be detected and managed early. There is also increased awareness of this potential complication with electrolyte imbalances especially around sodium [11]. Improved Intensive care access and early intubation at the advent of respiratory complications including arrest may also be a key factor involved in improved prognosis with less severe residual neurological sequelae [7, 11].
Discussion
Hyponatremia is seen in association with osmotic demyelination disorders in up to 40% of cases but it is not a universal finding in osmotic demyelination syndromes. The occurrence of the condition in other situations where serum sodium is normal, suggests that there are still further underdetermined aspects regarding the condition apart from rapid correction of hyponatremia. Focussing solely on serum sodium may mean neglecting the other 60% of situations where sodium may not play a predominant role in the development of the condition. It is likely that the etiology of osmotic demyelination syndrome is multifactorial and linked to neuronal osmotic stress [26]. Energy deprived states like chronic alcoholism and malnutrition appear to aggravate the risk.
Conclusion
The case of central pontine myelinolysis and other osmotic demyelination syndromes, is by no means open and shut. Improved awareness and supportive care has led to a dramatic shift in the prognosis with a sustained improvement in mortality figures over the years.
Key points
-
1.
Resist the urge to treat chronic hyponatremia
-
2.
Anticipate osmotic demyelination syndrome in patients with risk factors like chronic alcoholism, malnutrition and those undergoing rapid osmotic shifts.
-
3.
Once osmotic demyelination has occurred, consider reinduction of hyponatremia if within 24 h. Beyond 24 h, plasmapheresis and IVIG can be considered.
-
4.
Consider thiamine in all patients with history of alcoholism and malnutrition.
-
5.
Consider a multidisciplinary team approach with neurologist, intensivist, physiotherapist, dietitian, speech and language therapist.
References
Adams RD, Victor M, Mancall EL (1959) Central pontine myelinolysis: a hitherto undescribed disease occurring in alcoholic and malnourished patients. AMA Archi Neurol Psychiatry 81:154–172
Haynes HR, Gallagher PJ, Cordaro A, Likeman M, Love S (2018) A case of chronic asymptomatic central pontine myelinolysis with histological evidence of remyelination. Forensic Sci Med Pathol 14:106–108
Razvi SS, Leach JP (2006) Asymptomatic pontine myelinolysis. Eur J Neurol 13:1261–1263
Strub MU, Steck AJ, Fuhr P (1999) Asymptomatic central pontine myelinolysis. Neurology 53:914
Slager UT (1986) Central pontine myelinolysis and abnormalities in serum sodium. Clin Neuropathol 5:252–256
Newell KL, Kleinschmidt-DeMasters BK (1996) Central pontine myelinolysis at autopsy; a twelve year retrospective analysis. J Neurol Sci 142:134–139
Bose P, Kunnacherry A, Maliakal P (2011) Central pontine myelinolysis without hyponatraemia. J R Coll Physicians Edinb 41:211–214
Martin RJ (2004) Central pontine and extrapontine myelinolysis: the osmotic demyelination syndromes. J Neurol Neurosurg Psychiatry. 75(Suppl 3):22–28
Julia R, Lothar B, Wei-Chi L et al (2007) Belly dancer’s syndrome following central pontine and extrapontine myelinolysis. Mov Disord 22:892–894
Tan AH, Lim SY, Ng RX (2018) Osmotic demyelination syndrome with evolving movement disorders. JAMA Neurol. https://doi.org/10.1001/jamaneurol.2018.0983
Ranger AM, Chaudhary N, Avery M, Fraser D (2012) Central pontine and extrapontine myelinolysis in children: a review of 76 patients. J Child Neurol 27:1027–1037
Lampl C, Yazdi K (2002) Central pontine myelinolysis. Eur Neurol 47:3–10
Messert B, Orrison WW, Hawkins MJ, Quaglieri CE (1979) Central pontine myelinolysis. Considerations on etiology, diagnosis, and treatment. Neurology 29:147–160
Laureno R (1983) Central pontine myelinolysis following rapid correction of hyponatremia. Ann Neurol 13:232–242
Kleinschmidt-Demasters, B. K.; Rojiani, A. M.; Filley, C. M. Central and extrapontine myelinolysis: then...and now, J Neuropathol Exp Neurol. 2006, 65, 1–11.
Norenberg MD, Leslie KO, Robertson AS (1982) Association between rise in serum sodium and central pontine myelinolysis. Ann Neurol 11:128–135
George JC, Zafar W, Bucaloiu ID, Chang AR (2018) Risk Factors and outcomes of rapid correction of severe hyponatremia. Clin J Am Soc Nephrol 13:984–992
Bonham CA, Dominguez EA, Fukui MB et al (1998) Central nervous system lesions in liver transplant recipients: prospective assessment of indications for biopsy and implications for management. Transplantation 66:1596–1604
Shinde SV (2017) Central pontine myelinolysis associated with hypokalemia in a diabetic patient with sepsis. Neurology India 65:674–675
Abdulla MC, Jemshad A, Shameem A, Ram N (2017) Central pontine myelinolysis in Sjogren’s syndrome with hypokalemia. Int J Rheum Dis. 20:2168–2170
Lohr JW (1994) Osmotic demyelination syndrome following correction of hyponatremia: association with hypokalemia. Am J Med 96:408–413
Mehanna HM, Moledina J, Travis J (2008) Refeeding syndrome: what it is, and how to prevent and treat it. BMJ 336:1495–1498
Schnitker MA, Mattman PE, Bliss TL (1951) A clinical study of malnutrition in Japanese prisoners of war. Ann Intern Med 35:69–96
Patel AS, Matthews L, Bruce-Jones W (2008) Central pontine myelinolysis as a complication of refeeding syndrome in a patient with anorexia nervosa. J Neuropsychiatry Clin Neurosci 20:371–373
Bose P (2012) 061 Central pontine myelinolysis: a CNS manifestation of re-feeding syndrome? J Neurol Neurosurg Psychiatry 83:e1–e1
Ashrafian H, Davey P (2001) A review of the causes of central pontine myelinosis: yet another apoptotic illness? Eur J Neurol. 8:103–109
McKee AC, Winkelman MD, Banker BQ (1988) Central pontine myelinolysis in severely burned patients: relationship to serum hyperosmolality. Neurology 38:1211–1217
Donnelly H, Connor S, Quirk J (2016) Central pontine myelinolysis secondary to hyperglycaemia. Pract Neurol 16:493–495
Marsili L, Gallerini S, Bartalucci M, Marotti C, Marconi R (2018) Paroxysmal painful spasms associated with central pontine myelinolisis in the context of nonketotic hyperglycemia. J Neurol Sci 388:37–39
Pliquett RU, Noll A, Ibe R et al (2018) Hyperglycemia-related central pontine demyelinization after a binge-eating attack in a patient with type-2 diabetes: a case report. BMC Endocr Dis 18:18
Finlayson MH, Snider S, Oliva LA, Gault MH (1973) Cerebral and pontine myelinolysis. Two cases with fluid and electrolyte imbalance and hypotension. J Neurol Sci 18:399–409
Tomlinson BE, Pierides AM, Bradley WG (1976) Central pontine myelinolysis. Two cases with associated electrolyte disturbance. Q J Med 45:373–386
Gankam Kengne F, Decaux G (2018) Hyponatremia and the Brain. Kidney Int Rep 3:24–35
Verbalis JG, Drutarosky MD (1988) Adaptation to chronic hypoosmolality in rats. Kidney Int 34:351–360
Gankam-Kengne F, Couturier BS, Soupart A, Brion JP, Decaux G (2017) Osmotic stress-induced defective glial proteostasis contributes to brain demyelination after hyponatremia treatment. J Am Soc Nephrol 28:1802–1813
Ruzek KA, Campeau NG, Miller GM (2004) Early diagnosis of central pontine myelinolysis with diffusion-weighted imaging. Am J Neuroradiol 25:210–213
Menger H, Jorg J (1999) Outcome of central pontine and extrapontine myelinolysis (n = 44). J Neurol 246:700–705
Sener RN (1998) A false lesion in the center of the pons on magnetic resonance images. Comput Med Imaging Graph 22:413–416
Sivathapandi T, Simon S, Elangovan I (2017) Localized pontine uptake in fluorine-18-fuorodeoxyglucose positron emission tomography/computed tomography in a case of hyponatremia: a case report and review of literature. Indian J Nucl Med 32:333–335
Rønne F, Tfelt-Hansen PC, Rørdam L (2017) Central pontine myelinolysis and localized fluorodeoxyglucose uptake seen on f-FDG PET/CT. World J Nucl Med. 16:56–58
Kleinschmidt-DeMasters B, Norenberg M (1981) Rapid correction of hyponatremia causes demyelination: relation to central pontine myelinolysis. Science 211:1068–1070
Kleinschmidt-DeMasters BK, Norenberg MD (1982) Neuropathologic observations in electrolyte-induced myelinolysis in the rat. J Neuropathol Exp Neurol 41:67–80
Monteiro L (1971) Central pontine myelinolysis within the framework of a new histopathological syndrome with systematized topography. Report of an anatomo-clinical case. J Neurol Sci. 13:293–314
Powers JM, McKeever PE (1976) Central pontine myelinolysis. An ultrastructural and elemental study. J Neurol Sci 29:65–81
Sterns RH, Cappuccio JD, Silver SM, Cohen EP (1994) Neurologic sequelae after treatment of severe hyponatremia: a multicenter perspective. J Am Soc Nephrol 4:1522–1530
Mohmand HK, Issa D, Ahmad Z, Cappuccio JD, Kouides RW, Sterns RH (2007) Hypertonic saline for hyponatremia: risk of inadvertent overcorrection. Clin J Am Soc Nephrol 2:1110–1117
Soupart A, Ngassa M, Decaux G (1999) Therapeutic relowering of the serum sodium in a patient after excessive correction of hyponatremia. Clin Nephrol 51:383–386
Oya S, Tsutsumi K, Ueki K, Kirino T (2001) Reinduction of hyponatremia to treat central pontine myelinolysis. Neurology 57:1931–1932
Grimaldi D, Cavalleri F, Vallone S, Milanti G, Cortelli P (2005) Plasmapheresis improves the outcome of central pontine myelinolysis. J Neurol 252:734–735
Bibl D, Lampl C, Gabriel C, Jüngling G, Brock H, Köstler G (1999) Treatment of central pontine myelinolysis with therapeutic plasmapheresis. The Lancet 353:1155
Finsterer J, Engelmayer E, Trnka E, Stiskal M (2000) Immunoglobulins are effective in pontine myelinolysis. Clin Neuropharmacol 23:110–113
Escribano-Gascon AB, Casanova-Peno LI, Bartolome-Puras M, Porta-Etessam J (2008) Efficacy of intravenous immunoglobulins in central pontine myelinolysis. Neurologia 23:392–394
Patel M, Kaur M, Gupta S, Ayman M, Shapshak A (2018) Intravenous immunoglobulin use in treatment of central pontine myelinolysis: a case report (P1168). Neurology 90
Rodriguez M, Miller DJ, Lennon VA (1996) Immunoglobulins reactive with myelin basic protein promote CNS remyelination. Neurology 46:538–545
Silver SM, Schroeder BM, Sterns RH, Rojiani AM (2006) Myoinositol administration improves survival and reduces myelinolysis after rapid correction of chronic hyponatremia in rats. J Neuropathol Exp Neurol 65:37–44
Louis G, Megarbane B, Lavoue S et al (2012) Long-term outcome of patients hospitalized in intensive care units with central or extrapontine myelinolysis*. Crit Care Med 40:970–972
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
No conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bose, P. Central pontine myelinolysis and the osmotic demyelination syndromes: an open and shut case?. Acta Neurol Belg 121, 849–858 (2021). https://doi.org/10.1007/s13760-021-01634-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-021-01634-0