Abstract
Stroke is the leading cause of disability and one of the most common reasons of death around the world. Information is not sufficient on the palliative care (PC) needs of stroke patients and factors affecting their prognosis. In this study, we have investigated the demographics and comorbidities of stroke patients followed-up in a PC center (PCC), and the factors efficient on their prognosis. Medical records of 132 patients followed-up in PCC with stroke diagnosis between years 2016 and 2017 were reviewed retrospectively. Patients diagnosed with stroke were grouped as ischemic stroke, intracerebral hematoma (ICH) and subarachnoid hemorrhage (SAH). Age, gender, PCC hospitalization period (LOS), Glasgow Coma Scale, comorbidities such as percutaneous endoscopic gastrostomy, tracheostomy, pressure ulcer (PU), and discharge status (home, intensive care unit, exitus) have been compared for the patients included in the study. While average age was 72.41 ± 16.03 and hospitalization period was 35.47 ± 36.13 days, 92 patients (69.7%) were diagnosed with ischemic stroke, 20 patients (15.2%) with ICH, and 20 patients (15.2%) were diagnosed with SAH. The rate of exitus in patients diagnosed with ischemic stroke was significantly higher than patients diagnosed with ICH and SAH (p = 0.02), and hypertension rate was higher in patients with ischemic stroke than patients diagnosed with SAH (p = 0.007). The age of patients with exitus were found to be significantly higher (p = 0.001). Length of stay (LOS) in PC was determined to be significantly higher in patients with tracheostomy and patients diagnosed with ICH compared to patients with SAH. Furthermore, PU rate was significantly higher in patients diagnosed with ICH than patients with SAH (p = 0.007). Patients who experienced stroke and their families need comprehensive palliative care for psychosocial support, determination of patient-focused care objectives, and symptom management. There is a need for studies on larger populations to eliminate prognostic uncertainties and provide successful symptom management in patients following stroke.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Palliative care (PC) is defined as a clinical approach that targets to improve the quality of life in patients and families facing a life-threatening disease [1]. While the WHO defined PC first in 1986 as a practice for end of life patients when the curative approaches are exhausted, it became an application that also support the family along with therapeutic approaches from the beginning of diagnosis, but independent from the diagnosis and prognosis of the patient. In addition, scope of palliative care has broadened, and patients that have dementia, Parkinson’s, stroke, and motor neuron diagnoses that have longer life spans and lower mortality rates also began benefiting from palliative care. Neurological diseases constitute the disease group with the highest need for palliative care among non-cancer diseases [2]. While the role of PC is recognized for oncologic and chronic progressive neuromuscular diseases, it still protects its uncertainty for stroke patients [3, 4].
Stroke is an important public health issue and it is known to constitute 10% of all deaths [5]. In recent years, it has been observed that the incidence of stroke has decreased with the better control of vascular risk factors that are important in stroke, and that mortality also decreased with the developments in acute stroke care [6]. Despite these developments, 1-year mortality is reported between 20–40% for stroke [5, 7]. Stroke is a sudden and unexpected condition, and while curative treatment is provided for a small part of stroke patients, it results in death for those remaining and causes serious disabilities in most of the survivors [8, 9]. For this reason, there is need for a comprehensive care to increase the quality of life for patients after stroke for providing control of pain and other symptoms, and managing physical, social, psychological or moral needs of patients and families [10].
In both acute and chronic periods of stroke, particularly patients undergoing sequelae after stroke and their families, face potentially life-changing decisions. Although stroke results in high levels of mortality and morbidity, very little is known on the quality, scope and timing of palliative care services presented to this patient group, and how to provide these services [11, 12]. In this study, we have grouped the stroke patients followed-up in palliative care as ischemic stroke, ICH and SAH. We have examined the effect of demographics and comorbidities on the prognosis and PC hospitalization period.
Materials and methods
The study was approved by Ankara Numune Training and Research Hospital Ethics Committee (dated 26.6.2018 and approval no: E-18-2080). All procedures have been applied in accordance with the principles of the Declaration of Helsinki.
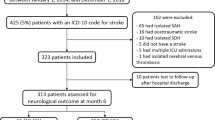
Ulus State Hospital PCC is an institution that also provides follow-ups for patients in addition to cancer patients, and when necessary, support is received from neurosurgeons, general surgeons, internal disease, cardiology, chest disease, and infectious diseases specialists, plastic and reconstructive surgeons, and physical therapy and rehabilitation specialists under the responsibility of anaesthesia and reanimation specialists. In addition to medical treatments of patients for such symptoms as pain, agitation, delirium, nausea, vomiting, etc., patients are provided nutrition, wound care, and physiotherapies by a multidisciplinary team. Besides, patients and their families receive provided moral support by psychologists and spiritual care specialists. In this study files of 132 patients, who were followed-up in Ankara Ulus Public Hospital PCC between the dates January 1, 2015 and December 31, 2017 with stroke diagnosis, have been reviewed retrospectively. Patients with incomplete patient file records, 1-day hospitalization period and repeated hospitalizations in PCC have been excluded from the study. Patients diagnosed with stroke were grouped as ischemic stroke, ICH and SAH. Age, gender, PCC hospitalization period (LOS in PCC), Glasgow Coma Scale (GCS), chronic diseases such as cardiac disease (CD), hypertension (HT) and diabetes mellitus (DM), comorbidities such as percutaneous endoscpic gastrostomy (PEG), tracheostomy and pressure ulcer (PU), and discharge status (home, intensive care unit, exitus) have been compared for the patients included in the study.
Statistical analysis
MS-Excel 2003 and IBM SPSS Statistics 23.0 (IBM Corp. Released 2015. IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp.) programs were used for statistical analysis and calculations. In the analysis of data, n % was used for categorical variables, and mean ± standard deviation was used for numeric variables. Kolmogorov–Smirnov normality test was performed for numeric variables to undergo statistical tests, and it was observed that variables did not show normal distribution. For this reason, non-parametric statistical methods were used in this study. Accordingly, Mann–Whitney U test was performed while examining differences between two independent groups (e.g., gender) with regard to numeric variables (e.g., GCS score). Kruskal–Wallis test was used while examining differences among more than two independent groups (e.g., discharge status) with regard to numeric variables (e.g., number of hospitalization days). The relation between two independent numeric variables was interpreted with Spearman’s Rho, and the relation between two independent categorical variables was interpreted with Chi-square analysis, and p < 0.05 was assumed to indicate significant difference.
Results
Nineteen patients who had incomplete patient file records, hospitalization period of 1 day and below, and repeated hospitalizations in PCC have been excluded from the study. A total of 132 patients, 58 (43.9%) of whom were female and 74 (56.1%) were male, have been included in the study. Average age was 72.41 ± 16.03 and LOS in PCC 35.47 ± 36.13 days, and average GCS points were determined as 9.89 ± 2.66. While the number of patients with discharge status exitus was 27 (20.5%), the number of patients transferred to intensive care unit (ICU) was 28 (21.2%), and the number of patients who were discharged to go home was 77 (58.3%). Ischemic stroke was observed in the highest rate (69.7%) as 92 of 132 patients included in the study had ischemic stroke, and the number of patients diagnosed with ICH and SAH was 20. Top accompanying chronic systemic disease was observed to be HT in 60 (45.5%) patients, and it was followed by DM in 32 (24.2%) patients and CD in 27 (20.5%) patients. Nine patients (6.8%) had oral nutrition, 79 patients (59.8%) had PEG feeding, 42 patients (31.8%) had tracheostomy, and 39 patients (29.5%) had PU (Table 1.).
The effect of age, LOS in PCC and GCS on prognosis (exitus, ICU and discharged to go home) has been determined to possess statistically significant difference upon examination. It was observed that the age of exitus patients was significantly higher than patients who were discharged to go home (81.04 ± 12.34 and 68.88 ± 16.51, p = 0.001), and LOS in PCC was significantly longer in patients who were discharged to go home compared to patients transferred to ICU (39.13 ± 38.50 and 23.46 ± 22.16, p = 0.035) (Table 2.).
Considering their discharge status, it was determined that patients with ischemic stroke had higher exitus, and patients with ICH had higher discharge rate for going home. While ICU transfer rate was low in ICH patients, it was observed more in patients with ischemic stroke and SAH (p = 0.022) (Table 3).
Considering the factors affecting LOS in PCC (Table 4), the number of hospitalization days in patients diagnosed with ICH was significantly higher than patients with SAH (48.35 ± 30.88 and 23.15 ± 15.62, p = 0.023), and it was observed that tracheostomy caused statistically longer LOS in PCC (p = 0.004). (Table 4).
The relation between diagnosis and comorbidity is shown in Table 5. Rate of HT was determined higher in ischemic stroke patients (n = 49, 53.3%) compared to patients with SAH (n = 3, 15.0%), and it was determined to be statistically significant (p = 0.007). PU sub-diagnosis was determined to be significantly higher in patients diagnosed with ICH compared to patients with SAK sub-diagnosis (p = 0.007) (Table 5).
Discussion
According to the update of cardiac disease and stroke statistics on 2014, more than 5% of all deaths in USA was related with stroke, and 73% of these deaths were diagnosed as ischemic stroke and 16% as intracerebral hemorrhage (ICH) [13]. Studies have reported that PC need is high for stroke patients, and that rehabilitation period should also be integrated with PC starting from acute period [14]. However, studies on stroke patients performed with PC is quite limited [15, 16]. Our study is the first study performed in Turkey on this subject. The most common diagnosis of stroke patients followed-up in PC was ischemic stroke (69.7%), and it was followed by ICH (15.2%) and SAH (15.2%). While more than half of stroke patients was discharged to go home (n:77, 58.3%), 27 (20.5%) patients have died, and 28(21.2%) patients were transferred to intensive care. In their study, Chen et al. established 1-year mortality rate as 17.6% in patients with the age range of 45–65, and as 80.2% in patients above the age of 65 [17].
Stroke is one of the leading reasons of long-term disability, although disease severity and course was quite variable in stroke patients [18]. Since more than half of our patients were discharged to go home in this study, PC support is extremely important for the acceptance of disability condition by the patient and family, and for increasing quality of life on the remaining part of life. Creutzfeldt et al. [16] have emphasized the necessity of PC for improving the quality of life of patients by the recognition and treatment of disturbing symptoms developed after ischemic stroke and ICH. In this study where we analyse the factors efficient on prognosis, we have determined ischemic stroke and age negatively affect prognosis, and that patients with ischemic stroke and advanced age experienced higher rate of exitus. Moreover, we have determined that the rate of being discharged to go home was higher in patients diagnosed with ICH, and patients diagnosed with ischemic stroke and SAH has higher ICU transfer rate. According to National Vital Statistics Report, in-hospital mortality increases with age in stroke patients [19]. It has been observed in other studies that age affects prognosis negatively, and mortality increases in stroke patients with advanced age [20, 21]. However, the effect of ischemic stroke and ICH on prognosis has been determined to be different in these studies. While Alonso et al [20] reported poor prognosis in patients with ICH diagnosis, Pham et al [22] have reported ischemic stroke had higher mortality compared to ICH and SAH.
Among a total of 132 patients followed-up in PC, 92 (69.7%) were diagnosed with ischemic stroke, and LOS in PCC was significantly higher in patients with ICH diagnosis. Furthermore, we have determined discharge rate to be higher and ICU transfer to be significantly lower in patients with ICH diagnosis. In compliance with our study, Koton et al. have reported the highest rate of ischemic stroke was among stroke patients, and longer hospitalization period was present in patients with ICH diagnosis in their study [23]. In another study, it has been reported that PC application extends hospitalization period in ischemic stroke patients while decreasing hospitalization period in patients with ICH and SAH, however, ischemic stroke patients had shorter hospitalization period compared to ICH and SAH considering average hospitalization period [24]. They attributed this to high rate of mild ischemic stroke, and the fact that majority of patients followed-up in PC had non-fatal ischemic stroke.
Pham et al. [22] have reported that mortality was higher in ischemic stroke and prognosis was better in hemorrhage, and systemic diseases such as DM and HT increased mortality. Yang Wang and colleagues have shown that comorbidity is an important indicator of long-term mortality in ischemic stroke patients [25]. In compliance with literature, we have determined in our study that HT rate was significantly higher in ischemic stroke patients compared to SAH patients, and we have considered that this was effective on the higher mortality rate in ischemic stroke patients. It was shown in previous studies that the possibility of PU development was higher in chronic diseases such as stroke and patients above age 65, and that it extended hospitalization period [26, 27]. In our study, we consider that low mortality, but high PU rate in patients diagnosed with ICH may be one of the factors extending hospitalization period.
In a study performed on stroke patients, it has been reported that mechanical ventilation (MV) and tracheostomy requirement was higher in hemorrhagic stroke, and mortality was high in patients requiring mechanical ventilation [28, 29]. Studies have suggested that early tracheostomy is associated with shorter ventilation period, lower intensive care complications, lower mortality and increased home discharge rate [30, 31]. Among patients we have followed-up in PCC, 42 patients (31.8%) had tracheostomy, and the hospitalization period of patients with tracheostomy was significantly higher than other patients (p = 0.004). We think that time to discharge is extended due to training on care and nutrition for patients undergoing tracheostomy, PEG, PU throughout their follow-up in PCC.
In conclusion, patients who have experienced stroke and their families need comprehensive palliative care for psychosocial support, determination of patient-focused care objectives, and symptom management. The use of palliative care is increased for stroke patients in our day, and treatments that sustain life should be viewed as an important support for patients and families, rather than an alternative to other stroke treatments. There is a need for studies on larger populations to eliminate prognostic uncertainties and provide successful symptom management in patients following stroke.
References
World Health Organization (WHO) WHO Definition of Palliative Care. http://www.who.int/cancer/palliative/definition/en/. Accessed 2 Jul 2018
Boersma I et al (2014) Palliative care and neurology: time for a paradigm shift. Neurology 83(6):561–567
Holloway RG et al (2014) Palliative and end-of-life care in stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 45(6):1887–1916
Lorenzl S et al (2013) Palliative treatment of chronic neurologic disorders. Handb Clin Neurol 118:133–139
Mozaffarian D et al (2015) Heart disease and stroke statistics-2015 update: a report from the American Heart Association. Circulation 131(4):e29–e322
Koton S et al (2014) Stroke incidence and mortality trends in US communities, 1987 to 2011. JAMA 312(3):259–268
Hankey GJ et al (2000) Five-year survival after first-ever stroke and related prognostic factors in the Perth Community Stroke Study. Stroke 31(9):2080–2086
Robinson MT, Holloway RG (2017) Palliative care in neurology. Mayo Clin Proc 92(10):1592–1601
Creutzfeldt CJ, Longstreth WT, Holloway RG (2015) Predicting decline and survival in severe acute brain injury: the fourth trajectory. BMJ 351:h3904
Lindsay MP et al (2014) Canadian stroke best practice recommendations. Heart and Stroke Foundation, Ottawa. http://www.strokebestpractices.ca. Accessed 27 Jul 2014
Gardiner C et al (2013) Provision of palliative and end-of-life care in stroke units: a qualitative study. Palliat Med 27(9):855–860
Stevens T et al (2007) Palliative care in stroke: a critical review of the literature. Palliat Med 21(4):323–331
Go AS et al (2014) Heart disease and stroke statistics-2014 update: a report from the American Heart Association. Circulation 129(3):e28–e292
Burton CR et al (2010) The palliative care needs of acute stroke patients: a prospective study of hospital admissions. Age Ageing 39(5):554–559
Blacquiere D et al (2013) Satisfaction with palliative care after stroke: a prospective cohort study. Stroke 44(9):2617–2619
Creutzfeldt CJ, Holloway RG, Walker M (2012) Symptomatic and palliative care for stroke survivors. J Gen Intern Med 27(7):853–860
Chen HF, Li CY, Lee SP, Kwok YT, Chu YT (2014) Improving the one-year mortality of stroke patients: an 18-year observation in a teaching hospital. Tohoku J Exp Med 232(1):47–54
Roberts SE et al (2015) Mortality following stroke, the weekend effect and related factors: record linkage study. PLoS One 10(6):e0131836
Heron M (2016) Deaths: leading causes for 2013. Natl Vital Stat Rep 65(2):1–95
Alonso A et al (2015) Outcome predictors of acute stroke patients in need of intensive care treatment. Cerebrovasc Dis 40(1–2):10–17
Abanto C et al (2013) Predictors of functional outcome among stroke patients in Lima, Peru. J Stroke Cerebrovasc Dis 22(7):1156–1162
Pham TM et al (2007) Mortality and risk factors for stroke and its subtypes in a cohort study in Japan. Prev Med 44(6):526–530
Koton S et al (2010) Derivation and validation of the prolonged length of stay score in acute stroke patients. Neurology 74(19):1511–1516
Singh T et al (2017) Palliative care for hospitalized patients with stroke: results from the 2010 to 2012 national inpatient sample. Stroke 48(9):2534–2540
Wang Y et al (2003) A prediction model of 1-year mortality for acute ischemic stroke patients. Arch Phys Med Rehabil 84(7):1006–1011
Lyder CH et al (2012) Hospital-acquired pressure ulcers: results from the national Medicare Patient Safety Monitoring System study. J Am Geriatr Soc 60(9):1603–1608
Allman RM (1998) The impact of pressure ulcers on health care costs and mortality. Adv Wound Care 11(3 Suppl):2
Holloway RG et al (2005) Prognosis and decision making in severe stroke. JAMA 294(6):725–733
Roch A et al (2003) Long-term outcome in intensive care unit survivors after mechanical ventilation for intracerebral hemorrhage. Crit Care Med 31(11):2651–2656
Bosel J et al (2012) Benefits of early tracheostomy in ventilated stroke patients? Current evidence and study protocol of the randomized pilot trial SETPOINT (Stroke-related Early Tracheostomy vs. Prolonged Orotracheal Intubation in Neurocritical care Trial). Int J Stroke 7(2):173–182
Pan CX et al (2015) Impact of a palliative care program on tracheostomy utilization in a community hospital. J Palliat Med 18(12):1070–1073
Funding
No funding sources.
Author information
Authors and Affiliations
Contributions
GS, DA and KK collected and integrated the data. GS and KK conceived and designed the study. GS, DA and KK analyzed the data, wrote and reviewed the paper, and were responsible for statistical analysis. All authors approved the final version of this paper for publication.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the Medical Ethical Committee at the Ankara Numune Training and Research Hospital (dated 26.6.2018 and approval no: E-18-2080) and the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Saricam, G., Akdogan, D. & Kahveci, K. Palliative care after stroke. Acta Neurol Belg 119, 69–75 (2019). https://doi.org/10.1007/s13760-018-1047-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-018-1047-0